Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Positive Collaboration in Rehabilitation Nursing Enhances Fall Efficacy and Confidence in Elderly Patients with Cerebral Infarction
Authors Luo F, Xu W, Xu Y, Lou L, Xu C
Received 21 January 2025
Accepted for publication 17 May 2025
Published 27 May 2025 Volume 2025:21 Pages 793—805
DOI https://doi.org/10.2147/TCRM.S518683
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Fang Luo,1 Wenyao Xu,2 Yaqin Xu,3 Lingdi Lou,1 Chunyan Xu3
1Department of Rehabilitation Medicine - Cerebrovascular Accident Rehabilitation Ward, Zhejiang Provincial People’s Hospital, Hangzhou, Zhejiang, 310024, People’s Republic of China; 2Convalescence Zone 1, Air Force Hangzhou Special Service Convalescence Center, Hangzhou, Zhejiang Province, 310007, People’s Republic of China; 3Department 5 of Geriatrics, Zhejiang Provincial People’s Hospital, Hangzhou, Zhejiang, 310007, People’s Republic of China
Correspondence: Chunyan Xu, Email [email protected]
Background: Cerebral infarction is a prevalent disabling condition among the elderly, often leading to limb dysfunction and psychological challenges that significantly impair quality of life. Traditional nursing approaches have primarily focused on physical rehabilitation; however, growing evidence highlights the importance of psychological factors—such as emotional well-being and rehabilitation confidence—in influencing recovery outcomes. Positive collaboration in rehabilitation nursing, which involves coordinated efforts among patients, healthcare providers, and family members, has emerged as a holistic approach to enhance both physical and psychological recovery.
Objective: To analyze the effects of positive collaboration concept rehabilitation nursing on elderly patients with cerebral infarction, focusing on fall efficacy and rehabilitation confidence.
Methods: A retrospective analysis was conducted on clinical data from 106 elderly patients with cerebral infarction, admitted from October 2022 to April 2024. Patients were divided into a control group (n=53, receiving routine care) and an observation group (n=53, receiving positive collaboration rehabilitation nursing). Neurological function (NIHSS), negative emotions (SAS, SDS), fall efficacy (MFES), activities of daily living (ADL), quality of life (SS-QOL), rehabilitation confidence (CaSM), and nursing satisfaction (NSNS) were compared between the two groups.
Results: The observation group showed significantly lower NIHSS scores at 2 weeks and 1 month post-intervention (P< 0.05). Both groups demonstrated reduced SAS and SDS scores, with the observation group showing greater improvement (P< 0.05). A higher proportion of patients in the observation group (56.60%) showed excellent fall efficacy compared to the control group (37.74%) (P< 0.05). The observation group also had greater improvements in ADL, SS-QOL, and rehabilitation confidence, with higher patient satisfaction (90.57% vs 71.70%, P< 0.05).
Conclusion: Positive collaboration rehabilitation nursing significantly improves neurological function, emotional well-being, fall efficacy, and quality of life in elderly patients with cerebral infarction. This approach increases patient and family satisfaction, highlighting the potential benefits of integrating collaborative care into clinical practice.
Keywords: cerebral infarction, elderly, positive collaboration concept rehabilitation nursing, fall efficacy, rehabilitation confidence, satisfaction, effect, impact
Introduction
Cerebral infarction is a common cerebrovascular disease, primarily characterized by localized insufficient blood flow to the brain, leading to ischemic damage to brain tissue.1 The elderly population is particularly vulnerable to cerebral infarction, with higher incidence and disability rates due to factors such as vascular sclerosis, metabolic decline, and the presence of chronic underlying diseases.2 According to relevant studies,3 patients with cerebral infarction often experience neurological dysfunction, increased negative emotions, and decreased quality of life after the acute phase. Therefore, optimizing rehabilitation nursing strategies to promote neurological recovery, improve quality of life, and enhance rehabilitation confidence is an essential issue in clinical nursing practice. Traditional routine nursing interventions primarily focus on disease treatment and basic nursing, which, although helpful in alleviating the patient’s condition to some extent, tend to neglect psychological factors such as the patient’s emotional state, daily living abilities, fall efficacy, and rehabilitation confidence.4,5 Addressing this issue, exploring innovative nursing models has become particularly necessary.
In recent years, rehabilitation nursing based on the positive collaboration concept has gained widespread attention in clinical practice. This nursing philosophy emphasizes proactive interaction and collaboration among nurses, patients, and their families, aiming to mobilize the patient’s subjective initiative and stimulate their rehabilitation potential through systematic and personalized nursing interventions, thus achieving multidimensional functional recovery.6 Studies7,8 have shown that positive collaboration concept rehabilitation nursing can promote both physical and psychological recovery through a combination of psychological intervention, functional training, and social support. However, research on the effects of positive collaboration concept rehabilitation nursing for elderly patients with cerebral infarction is still limited. Thus, this study retrospectively analyzes the clinical data of 106 elderly patients with cerebral infarction in our hospital and compares the differences in the intervention effects between routine nursing care and positive collaboration concept rehabilitation nursing. The goal is to provide scientific evidence for optimizing rehabilitation nursing models for cerebral infarction patients and contribute new ideas and practical experience for improving patient satisfaction and quality of life.
Materials and Methods
Basic Information
A retrospective analysis was conducted on the clinical data of 106 elderly patients with cerebral infarction admitted to our hospital from October 2022 to April 2024. Inclusion criteria: (1) patients who meet the clinical diagnostic criteria for cerebral infarction and have been confirmed by imaging examinations; (2) age ≥ 65 years, with no gender restriction; (3) first onset of disease; (4) all received basic treatment and are currently in the recovery phase with stable condition; (5) no significant speech disorders or severe cognitive dysfunction, able to understand and cooperate with nursing interventions; (6) patients and their families were informed about the study and signed the informed consent form. Exclusion criteria: (1) occurrence of adverse events such as falls, pressure injuries, etc., prior to inclusion; (2) severe communication or cognitive impairment and/or mental abnormalities; (3) severe organ function abnormalities; (4) serious complications of cerebral infarction such as arrhythmia or myocardial infarction; (5) malignant tumor diseases; (6) combined with other cardiovascular and cerebrovascular diseases; (7) immunological, hematological diseases, and/or severe infections; (8) recent participation in other interventional nursing studies or receiving special medications or treatments that might interfere with the study results; (9) inability to fully cooperate with the study for various reasons and/or incomplete clinical data. The patients were divided into two groups based on the nursing interventions they received: a control group (n=53, receiving routine nursing interventions) and an observation group (n=53, receiving active cooperative rehabilitation nursing intervention in addition to routine nursing). This study was approved by the Medical Ethics Committee of Zhejiang Provincial People’s Hospital (Approval No. NCZ24-HL0017), and the study process strictly adhered to the ethical guidelines of the Helsinki Declaration.
Nursing Methods
Control Group
The control group received routine nursing interventions, which mainly included the following aspects: (1) Condition Observation and Assessment: Regular monitoring of the patient’s neurological symptoms, including limb function, speech disorders, etc., to assess changes in the condition and promptly report any abnormalities. (2) Basic Care: Basic daily care such as oral care, skin care, and position management. Due to the patients’ long bed rest periods, comfortable positioning and appropriate nursing measures were provided to prevent complications like pressure ulcers and lung infections. (3) Nutritional Support and Diet Management: A diet plan was developed based on the patient’s nutritional status to ensure adequate energy and nutrient intake. For patients with swallowing difficulties, appropriate dietary adjustments were made, such as liquid or soft food, to meet the patients’ nutritional needs. (4) Rehabilitation Training: After the neurological function stabilized, patients were arranged for basic rehabilitation training, including limb function training, speech training, and swallowing training (Figure 1).
 |
Figure 1 The flow chart of the study. |
Observation Group
The observation group received active cooperative rehabilitation nursing intervention in addition to routine care. Specific measures were as follows: (1) Establishment of a Rehabilitation Nursing Team: A rehabilitation nursing team was formed, consisting of one attending physician, one rehabilitation doctor, one head nurse, and four responsible nurses. The team members collaboratively learned the concept and methods of the active cooperative rehabilitation philosophy, analyzed the rehabilitation care needs of elderly patients with cerebral infarction, and developed a rehabilitation care plan based on the analysis results. The attending physician was responsible for evaluating the quality of rehabilitation care, the rehabilitation doctor provided the rehabilitation plan, the head nurse supervised the nursing process, and the responsible nurses implemented the care plan. (2) Establishment of the Active Cooperative Rehabilitation Philosophy: After admission, the responsible nurse actively introduced the concept of the active cooperative philosophy to the patient, informing them that they would be the main subject in the rehabilitation care, with the care implemented based on their needs and willingness. The patient was guided to join the rehabilitation care team and engage in a collaborative model of care. (3) Rehabilitation Care Based on the Active Cooperative Philosophy: ① Patient Participation and Self-Management Ability Improvement: A. Patient Education and Information Transfer: Nursing staff used various forms such as health education pamphlets and videos to provide the patient and their family with relevant knowledge about cerebral infarction, including its causes, treatment methods, rehabilitation goals, and lifestyle adjustments, to help the patient understand their condition and rehabilitation process. By enhancing the patient’s disease awareness, active participation in treatment and rehabilitation was promoted. B. Personalized Rehabilitation Plan Development: Based on each patient’s specific condition, functional recovery, and psychological state, nursing staff collaborated with the patient to create a personalized rehabilitation plan. Small goals were set to help the patient build confidence as they progressively achieved them, enhancing self-management ability. C. Encouraging Patient Participation in Rehabilitation Activities: Nursing staff designed practical rehabilitation tasks based on the patient’s interests and abilities and encouraged the patient to actively participate. ② Emotional Regulation and Psychological Support: A. Psychological Counseling and Emotional Management: Nursing staff built trust and communicated deeply with the patient to understand their psychological needs, helping them accurately perceive the illness and adjust negative emotions through warm, patient communication. Regular emotional management activities, such as relaxation training and meditation exercises, were conducted to alleviate the patient’s anxiety and depression. B. Positive Encouragement and Confidence in Rehabilitation: Through positive reinforcement and psychological support, patients were encouraged to maintain a positive attitude and strengthen their confidence in the rehabilitation process. Nursing staff used specific examples to help patients set small goals and foster self-confidence as these goals were achieved. At every stage of the patient’s recovery, appropriate affirmation and encouragement were provided to ensure the patient remained confident in their rehabilitation. ③ Fall Efficacy and Daily Living Ability Training: A. Enhancing Fall Efficacy: Nursing staff developed personalized balance training plans based on the patient’s functional status. Functional training and daily activity guidance were used to help the patient increase their awareness of fall risks. Training content included sitting, standing, gait training, and common fall prevention techniques, such as correct rising methods and walking precautions. B. Daily Living Ability Training: Specific training included tasks like washing, dressing, eating, and toileting. Through one-on-one guidance and training, nursing staff helped the patient improve their self-care abilities and reduce dependence on others. For patients with swallowing difficulties, professional swallowing training was provided to help restore normal swallowing function. ④ Family Support and Cooperation: A. Family Member Education and Involvement: Nursing staff regularly communicated with the patient’s family, providing knowledge on cerebral infarction care and helping family members understand the patient’s rehabilitation needs. By educating the family, confidence in patient care was enhanced, and family members learned how to cooperate with the nursing team to reduce the patient’s burden and anxiety. Family members were encouraged to participate in the rehabilitation activities, such as assisting the patient with simple physical activities or engaging in the patient’s psychological counseling process. B. Establishment of a Support System: Nursing staff helped the patient and family establish a support system, encouraging the family to provide more care and support in daily life. Through active family support, patients felt more secure and cared for, which helped improve their confidence in rehabilitation and enhanced treatment compliance. (4) Nursing Assessment and Adjustment: During the nursing process, regular assessments were made regarding the patient’s rehabilitation progress. Based on the patient’s actual condition, nursing staff would adjust rehabilitation goals as necessary. Through regular assessments and feedback, the nursing team ensured that each patient received the most appropriate interventions to maximize the rehabilitation outcomes. Both groups were assessed after one month of continuous intervention.
Observation Indicators
Neurological Function
Before the intervention, 2 weeks post-intervention, and 1 month post-intervention, the National Institutes of Health Stroke Scale (NIHSS, Cronbach’s α = 0.894, validity = 0.857)9 was used to assess the neurological function of the patients. The scale ranges from 0 to 42 points, with higher scores correlating with more severe neurological impairment.
Negative Emotional Status
Before the intervention and post-intervention, the Self-Rating Anxiety Scale (SAS, Cronbach’s α = 0.862, validity = 0.831)10 and Self-Rating Depression Scale (SDS, Cronbach’s α = 0.879, validity = 0.846)11 were used to assess the negative emotional status of the patients. The maximum score for both scales is 100, with a cutoff of 50 for SAS and 53 for SDS. The scores are positively correlated with the patients’ negative emotions.
Falls Efficacy
Before and after the intervention, the Modified Falls Efficacy Scale (MFES, Cronbach’s α = 0.911, validity = 0.876)12 was used to assess the patients’ belief in their ability to avoid falling during daily activities such as dressing, bathing, and walking. The scale includes 14 items, rated on a 0–10 scale, with the total score being the average of individual scores. The scores were categorized into three levels: low efficacy (0–4), moderate efficacy (5–9), and high efficacy (10).
Activities of Daily Living
Before and after the intervention, the Activities of Daily Living Scale (ADL, Cronbach’s α = 0.786, validity = 0.751)13 was used to assess the patients’ ability to perform daily activities. The scale includes 10 items with a total score of 100, and the scores are positively correlated with the patient’s ability to perform daily activities.
Quality of Life
Before and after the intervention, the Stroke-Specific Quality of Life Scale (SS-QOL, Cronbach’s α = 0.813, validity = 0.795)14 was used to assess the patients’ quality of life. The scale consists of 12 dimensions and 49 items, with a total score of 245. The scores are positively correlated with the patient’s quality of life.
Rehabilitation Confidence
Before and after the intervention, the Stroke Rehabilitation Confidence Measure (CaSM, Cronbach’s α = 0.882, validity = 0.839)15 was used to assess the patient’s confidence in rehabilitation. The scale includes three dimensions: self-confidence (9 items, 0–27 points), positive attitude (8 items, 0–24 points), and social confidence (10 items, 0–30 points). It consists of 27 items, each rated on a 0–3 scale, with scores positively correlated with the patient’s rehabilitation confidence.
Nursing Satisfaction
After the intervention, the Newcastle Nursing Service Satisfaction Scale (NSNS, Cronbach’s α = 0.846, validity = 0.829)16 was used to evaluate satisfaction. The scale consists of 19 items, scored using a Likert 5-point scale. The scores are positively correlated with satisfaction. The total satisfaction rate = (number of very satisfied + number of satisfied) / total number of cases × 100%.
Statistical Analysis
The charting software used was GraphPad Prism 8; statistical analysis was performed using SPSS 22.0 software. For count data, percentages were presented and analyzed using the chi-square test. For measurement data ( ) were presented. Independent sample t-tests were used for comparisons between two groups, paired t-tests for within-group comparisons, and repeated measures ANOVA for comparisons at different time points. A p-value of <0.05 was considered statistically significant.
) were presented. Independent sample t-tests were used for comparisons between two groups, paired t-tests for within-group comparisons, and repeated measures ANOVA for comparisons at different time points. A p-value of <0.05 was considered statistically significant.
Results
Comparison of Baseline Data
There were no significant differences in gender, age, hemiplegic side, comorbidities, and educational level between the two groups (P > 0.05), making them comparable (Table 1).
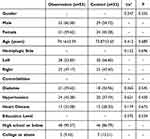 |
Neurological Function Comparison
The NIHSS scores showed significant differences between groups (F=6.876), time points (F=8.412), and interaction (F=7.474) (P < 0.05). Within groups: both groups showed lower NIHSS scores at 2 weeks and 1 month post-intervention compared to pre-intervention (P < 0.05). Between groups: no significant difference in NIHSS scores before the intervention (P > 0.05), but the observation group had significantly lower scores than the control group at 2 weeks and 1 month post-intervention (P < 0.05) (Figure 2).
Negative Emotional Status Comparison
Both the SAS and SDS scores decreased post-intervention, with a larger change in the observation group (P < 0.05) (Table 2).
 |
Comparison of Fall Efficacy
In the control group of 53 patients, 15 had low fall efficacy, 18 had moderate fall efficacy, and 20 had excellent fall efficacy. In the observation group of 53 patients, 9 had low fall efficacy, 14 had moderate fall efficacy, and 30 had excellent fall efficacy. The observation group (56.60%) had a higher proportion of excellent fall efficacy compared to the control group (37.74%) (P < 0.05) (Figure 3).
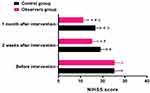 |
Figure 3 Comparison of Fall Efficacy [n (%)]. Note: Compared with the control group, *P < 0.05. |
Comparison of Activities of Daily Living and Quality of Life
After the intervention, the ADL score and SS-QOL score in the observation group were significantly higher than those before the intervention, with a greater change observed in the observation group (P < 0.05) (Table 3).
 |
Table 3 Comparison of Activities of Daily Living and Quality of Life ( |
Comparison of Rehabilitation Confidence
After the intervention, the self-confidence, positive attitude, and social confidence scores of both groups increased compared to before the intervention, with a greater change observed in the observation group (P < 0.05) (Table 4).
 |
Comparison of Satisfaction
In the control group of 53 patients, 13 were very satisfied, 25 were satisfied, 10 were neutral, and 5 were dissatisfied. In the observation group of 53 patients, 23 were very satisfied, 25 were satisfied, 4 were neutral, and 1 was dissatisfied. The observation group (90.57%) had a higher satisfaction rate compared to the control group (71.70%) (P < 0.05) (Figure 4).
 |
Figure 4 Comparison of Satisfaction [n (%)]. Note: Compared with the control group, *P < 0.05. |
Discussion
Cooperative care rehabilitation, as an emerging nursing concept, emphasizes active interaction and joint participation between patients, the nursing team, and family members.17 The goal is to enhance patients’ subjective initiative and improve their sense of self-efficacy, thereby improving rehabilitation outcomes.18 The core of this concept is to position the patient as an active participant in the rehabilitation process, rather than solely relying on passive nursing interventions. It focuses on collaboration, consensus, and joint efforts between the patient and the nursing team.19 This collaborative framework fosters a sense of ownership in patients, which enhances motivation and promotes consistent participation in rehabilitation exercises. Additionally, the inclusion of family members creates a continuous support network, ensuring that rehabilitation strategies extend beyond the clinical setting into the patient’s home environment.
Neurofunctional recovery is one of the key objectives in the rehabilitation treatment of cerebral infarction. Common neurological deficits in patients with cerebral infarction include hemiplegia, speech disorders, and cognitive impairment, which severely affect the patients’ independence and quality of life.20,21 The results of this study show that the NIHSS scores of patients in the observation group (who received cooperative care rehabilitation) were significantly lower than those in the control group at both 2 weeks and 1 month after intervention (P < 0.05). This finding aligns with previous studies,22,23 suggesting that cooperative care rehabilitation can effectively promote neurofunctional recovery in patients with cerebral infarction. The mechanism likely involves increased patient engagement in targeted therapeutic activities, facilitated by collaborative goal-setting and real-time feedback from both caregivers and family, thus accelerating neuroplastic adaptation and recovery.
The core of cooperative care rehabilitation is the positive interaction and collaboration between patients, nursing staff, and family members. The nursing process not only focuses on the patient’s physiological condition but also addresses their psychological needs and social support. By enhancing communication between patients and the nursing team, patients can fully understand their condition and rehabilitation goals, which increases their sense of participation and control. Furthermore, cooperative care rehabilitation emphasizes individualized rehabilitation plans, tailored to the patient’s specific condition, which helps improve their motor function and cognitive abilities, thereby promoting neurofunctional recovery. This individualized approach is reinforced by frequent two-way feedback, enabling nurses to dynamically adjust interventions based on patient response and preferences, thus enhancing both effectiveness and adherence.
A study24 indicated that patients with cerebral infarction often face significant negative emotions such as anxiety, depression, and feelings of helplessness, which not only affect their quality of life but also hinder their rehabilitation. The results of this study show that the observation group had significantly lower SAS and SDS scores after intervention compared to the control group (P < 0.05), suggesting that the cooperative care rehabilitation model effectively alleviates negative emotions in patients. This may be closely related to the high emphasis on psychological health in the cooperative care rehabilitation model. In this model, nurses establish trust relationships, listen to the psychological needs of patients, and provide necessary psychological support, helping to reduce anxiety, depression, and other emotional reactions. Additionally, through communication with patients and their families, nurses help patients understand the disease process correctly, thus reducing fear and uncertainty about the illness. Research25 suggests that enhancing the psychosocial support network of patients can not only improve their emotional state but also increase their participation and compliance in the rehabilitation process. By cultivating emotional resilience and buffering stress through empathetic communication and education, the collaborative model contributes to a more positive psychological environment conducive to healing.
Fall efficacy is an important indicator of a patient’s confidence and physical ability and is a crucial aspect of the rehabilitation process for patients with cerebral infarction. After a cerebral infarction, patients face a high risk of falls due to impaired limb motor function and reduced balance ability, which further affects their quality of life and independence.26 The results of this study show that the observation group (56.60%) had a higher proportion of excellent fall efficacy compared to the control group (37.74%) (P < 0.05), indicating that cooperative care rehabilitation has a positive effect on improving physical activity ability and reducing fall fear. Cooperative care rehabilitation is not just about the recovery of physiological function; it also emphasizes the positive transformation of the patient’s mindset. During the nursing process, nurses develop appropriate balance training and exercise rehabilitation plans based on the patient’s specific condition, helping them gradually recover motor function and increase physical stability. At the same time, through psychological interventions, the fear of falling is alleviated, and patients’ confidence in their ability to move is strengthened. These dual approaches—physical training supported by emotional coaching—synergistically improve the patient’s actual mobility and perceived control over their environment, both of which are critical for reducing fall-related anxiety. By improving fall efficacy, patients can participate more confidently in daily activities, thereby promoting their overall physical and mental recovery.
Activities of daily living and quality of life are important comprehensive indicators for assessing the rehabilitation outcomes of patients with cerebral infarction.27 The results of this study show that the ADL and SS-QOL scores in the observation group after intervention were significantly higher than those in the control group (P < 0.05). This indicates that cooperative care rehabilitation can not only promote physical recovery but also effectively improve patients’ quality of life. The cooperative care rehabilitation model addresses the holistic needs of patients. It not only promotes physical rehabilitation through functional training but also helps patients restore their normal life rhythm and social roles through psychological support. By enhancing patients’ confidence in self-rehabilitation, nurses help patients adapt to their post-disease life both psychologically and behaviorally, gradually recovering their ability to take care of themselves and interact socially. Meanwhile, nurses regularly assess patients’ activities of daily living during the nursing process and adjust care plans based on patients’ recovery progress to ensure smooth rehabilitation. The continuous feedback loop between nurses, patients, and caregivers facilitates timely intervention when challenges arise, supporting uninterrupted functional gains and maintenance of independence.
Rehabilitation confidence is the intrinsic motivation for patients’ participation in the rehabilitation process and directly affects the outcomes of rehabilitation.28 The results of this study show that the self-confidence, positive attitude, and social confidence scores in the observation group after intervention were significantly higher than those in the control group (P < 0.05). This result is likely related to the respect and encouragement emphasized in the cooperative care rehabilitation model. In this model, nurses build close cooperative relationships with patients and their families, allowing them to promptly understand patients’ emotional fluctuations and psychological needs. Through timely encouragement, comfort, and support, nurses help patients build confidence in overcoming their illness. Positive reinforcement, goal achievement tracking, and shared success stories during the rehabilitation journey play an essential role in fostering a growth mindset and optimism, both of which drive further engagement and perseverance. By continuously receiving positive feedback during the rehabilitation process, patients’ rehabilitation confidence is strengthened, providing strong support for maintaining a positive attitude during long-term rehabilitation.
Patient satisfaction with nursing care is a subjective evaluation of the quality-of-care services, and it is an important indicator for assessing the effectiveness of nursing. The results of this study show that the satisfaction rate in the observation group (90.57%) was significantly higher than that in the control group (71.70%) (P < 0.05). This indicates that the cooperative care rehabilitation model can significantly improve patients’ overall satisfaction with nursing services. The cooperative care rehabilitation model has unique advantages in improving patients’ nursing experience. First, by establishing closer relationships with patients and their families, nurses help patients feel warmer and more cared for during rehabilitation. Second, nurses provide personalized care based on patients’ individual needs, making patients feel valued and respected. This nursing model not only improves patients’ physiological condition but also enhances their psychological health and overall treatment experience, ultimately increasing patient satisfaction. When patients perceive themselves as active, respected collaborators in their care journey, their trust in the healthcare team improves, thereby enhancing the therapeutic alliance and contributing to overall satisfaction.
The cooperative care rehabilitation model, while showing promising results, may have broader applicability across different patient populations. The findings from this study suggest that the collaborative approach, which emphasizes active patient involvement and family participation, can be beneficial not only for elderly patients with cerebral infarction but also for those recovering from other neurological conditions or major surgeries. Furthermore, the individualized nature of the rehabilitation plan can be adapted to suit diverse clinical settings and patient demographics, including those with varying levels of cognitive function, comorbidities, and socio-cultural backgrounds. The extended involvement of caregivers and family members may also help address the unique needs of patients from different familial and social environments. Future research should explore the model’s applicability and effectiveness in other patient groups to strengthen the evidence base and broaden its clinical utility.
Implications for Practice
The results of this study show that the cooperative care rehabilitation model has significant effects on improving neurofunctional recovery, alleviating negative emotions, enhancing fall efficacy, improving activities of daily living, increasing quality of life, and boosting rehabilitation confidence in elderly patients with cerebral infarction. By strengthening the interaction and cooperation between patients, nursing staff, and family members, this nursing model can effectively promote both physical and mental recovery, improve the quality of life, and increase nursing satisfaction. Therefore, the cooperative care rehabilitation model is worth widely applying in clinical nursing for elderly patients with cerebral infarction and provides valuable insights for rehabilitation care in other diseases.
Limitations
Despite the valuable insights provided by this study, several limitations must be acknowledged. First, this was a single-center retrospective analysis with a relatively small sample size, which may limit the generalizability of the findings. Large-scale, multi-center studies are essential to improve the robustness and reliability of results and enhance external validity. Second, the study timeframe was designed to evaluate the short-term effects of the cooperative care rehabilitation model; however, a longer observation period would be necessary to capture long-term physiological and psychological outcomes more comprehensively. Future research should incorporate extended follow-up durations to generate stronger and more informative data on the sustained benefits and potential drawbacks of the intervention. Additionally, certain confounding factors—such as varying levels of family involvement, individual patient motivation, and differences in nurse-patient communication—could not be fully controlled and may have contributed to the observed effects. Future prospective, randomized studies are warranted to minimize the impact of these variables and further validate our findings. In the revised manuscript, we have explicitly acknowledged these limitations to provide transparency and guide future research directions.
Conclusion
The findings of this study demonstrate that the cooperative care rehabilitation model, which emphasizes collaboration among patients, nursing staff, and family members, has a significant positive impact on the rehabilitation outcomes of elderly patients with cerebral infarction. The model effectively promoted neurofunctional recovery, reduced negative emotions, enhanced fall efficacy, and improved overall quality of life and self-rehabilitation confidence. Additionally, the cooperative approach fostered improved patient satisfaction with nursing care. These results suggest that incorporating cooperative care rehabilitation into clinical practice can lead to better holistic rehabilitation for patients, addressing both their physical and psychological needs. Future studies with larger cohorts and extended timelines are recommended to further validate these findings and explore the broader applicability of this model to diverse patient populations and settings.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Liu Y, Yin YY, Lu QL, et al. Clinical analysis of dual enhanced antiplatelet therapy after cerebrovascular intervention for reducing the risk of cerebral infarction recurrence. Zhonghua Yu Fang Yi Xue Za Zhi. 2024;58(7):1062–1068. doi:10.3760/cma.j.cn112150-20240115-00054 Wolof
2. Zhai GJ, Xu Y, Yang XY, et al. Related factors of internal border-zone infarcts in patients with symptomatic chronic internal carotid artery occlusion. Zhonghua Yi Xue Za Zhi. 2022;102(37):2950–2955. doi:10.3760/cma.j.cn112137-20220106-00043 Danish
3. Erbguth F. Acute stroke treatment in old age. Z Gerontol Geriatr. 2020;53(1):59–74. doi:10.1007/s00391-019-01655-8 Slovak
4. Xiong HL, Li Z-X, Lu X, et al. Impact of early refined nursing program on prognosis of middle-aged and elderly patients with cognitive dysfunction combined with cerebral infarction. World J Psychiatry. 2024;14(7):1034–1042. doi:10.5498/wjp.v14.i7.1034
5. Li WW, Li M, Guo X-J, et al. Application of a hospital-community-family trinity rehabilitation nursing model combined with motor imagery therapy in patients with cerebral infarction. World J Clin Cases. 2023;11(3):621–628. doi:10.12998/wjcc.v11.i3.621
6. Xue LL, Zhang JZ, Shen HX, et al. The application of rapid rehabilitation model of multidisciplinary cooperation in cesarean section and the evaluation of health economics. Zhonghua Yi Xue Za Zhi. 2019;99(42):3335–3339. doi:10.3760/cma.j.issn.0376-2491.2019.42.012 Danish
7. Wu KJ. Multidisciplinary cooperation strengthens individualized management of breast cancer in pregnancy. Zhonghua Wai Ke Za Zhi. 2020;58(2):95–98. doi:10.3760/cma.j.issn.0529-5815.2020.02.004 Hawaiian
8. He YS, Liu G-H, Zhang Y-H, et al. Effect of parent-child cooperative music therapy on children with autism spectrum disorder and their mothers: a prospective randomized controlled study. Zhongguo Dang Dai Er Ke Za Zhi. 2022;24(5):472–481. doi:10.7499/j.issn.1008-8830.2201105 Xhosa
9. Zhu FJ, Fan SL, Liu GX, et al. Effect of early rehabilitation training on motor function and neural function of patients with brainstem hemorrhage after body-oriented individualized surgery. Zhonghua Yi Xue Za Zhi. 2023;103(45):3670–3675. doi:10.3760/cma.j.cn112137-20231012-00722 Danish
10. Shi MQ, Zhang WX, Ni TY, et al. Analysis of factors for anxiety and anxiety tendency in tinnitus patients. Zhonghua Yi Xue Za Zhi. 2024;104(36):3392–3396. doi:10.3760/cma.j.cn112137-20240623-01395 Danish
11. He M, Lai YQ, Zhang XW, et al. Characteristics and correlated factors of preoperative sleep disorders in cardiac surgical patients. Zhonghua Yi Xue Za Zhi. 2024;104(40):3745–3750. doi:10.3760/cma.j.cn112137-20240410-00839 Danish
12. Uriah SS, Oguzor UC, Atata CT, et al. Fear of falling and its relationship with quality of life in the elderly attending a family medicine clinic in South-South Nigeria. West Afr J Med. 2023;40(12 Suppl 1):S23–s24.
13. Liu HL, Song YN, Wang XX, et al. Effects of whole-course multimodal analgesia on postoperative pain and rapid recovery in elderly patients with urological tumors. Zhonghua Yi Xue Za Zhi. 2023;103(41):3245–3251. doi:10.3760/cma.j.cn112137-20230725-00089 Danish
14. Yan H, Wang W, Wang S, et al. Clinical effects of debulking surgery combined with neoadjuvant chemotherapy in treating ovarian cancer and its influence on tumor markers and immune function. Pak J Med Sci. 2024;40(11):2475–2479. doi:10.12669/pjms.40.11.9337
15. Horne JC, Lincoln NB, Logan PA. Measurement of confidence: the development and psychometric evaluation of a stroke-specific, measure of confidence. Clin Rehabil. 2017;31(11):1529–1537. doi:10.1177/0269215517705424
16. Karadaş A, Ergün S, Kaynak S. Relationship between missed nursing care and patients’ trust in nurses and satisfaction with care: a cross-sectional study. Nurs Health Sci. 2024;26(3):e13149. doi:10.1111/nhs.13149
17. Frewer-Graumann S, Teichmüller AK. Enhancement of hospice philosophy and palliative care competence in nursing homes for seniors through cooperation with an outpatient hospice care service: a practical example. Z Gerontol Geriatr. 2021;54(1):13–19. doi:10.1007/s00391-020-01803-5 Slovak
18. Froschauer S, Muth T, Bredow L, et al. Care atlas rheumatology: approaches and concepts for improving care in outpatient rheumatology. Z Rheumatol. 2021;80(9):819–826. doi:10.1007/s00393-021-01072-6
19. Friedrich AC, Czwikla J, Schulz M, et al. Medical care with or without cooperative agreements? A cross-sectional study in nursing homes in Bremen and lower saxony. Z Evid Fortbild Qual Gesundhwes. 2023;177:57–64. doi:10.1016/j.zefq.2022.11.011 Swedish
20. Zhang J, Luo Z, Zeng Y. Predictive modeling of early neurological deterioration in patients with acute ischemic stroke. World Neurosurg. 2024;191:58–67. doi:10.1016/j.wneu.2024.08.017
21. Hu J, Gao S-Q, Wang J, et al. Analysis on disease burden and direct medical cost of Xueshuan Xinmaining Tablets in patients with cerebral infarction and coronary heart disease. Zhongguo Zhong Yao Za Zhi. 2021;46(9):2309–2316. doi:10.19540/j.cnki.cjcmm.20210128.502 Catalan
22. Zhu FX, Ye Q. Effect of medical care linkage-continuous management mode in patients with posterior circulation cerebral infarction undergoing endovascular interventional therapy. World J Clin Cases. 2022;10(29):10478–10486. doi:10.12998/wjcc.v10.i29.10478
23. Chen QQ, Lin F-M, Chen D-H, et al. Analysis of mental health status and related factors in patients with acute cerebral infarction. World J Psychiatry. 2023;13(10):793–802. doi:10.5498/wjp.v13.i10.793
24. Sun Y, Ren T, Ji X. Influence of hyperbaric oxygen therapy-specialized care on limb motor function and mental state of cerebral infarction patients with hemiplegia. Technol Health Care. 2024;32(3):1967–1976. doi:10.3233/THC-231643
25. Mao Y, Tao X, Zhang G, et al. Effect of music therapy on negative psychology, sleep, and quality of life in elderly patients recovering from cerebral infarction with depression and anxiety: a retrospective analysis. Noise Health. 2024;26(122):430–435. doi:10.4103/nah.nah_84_24
26. Sjöholm H, Hägg S, Nyberg L, et al. Exploring possible risk factors for time to first fall and 6-month fall incidence in persons with acute stroke. SAGE Open Med. 2022;10:20503121221088093. doi:10.1177/20503121221088093
27. Liu Y, Qu M, Wang N, et al. Effects of an evidence-based nursing intervention on neurological function and serum inflammatory cytokines in patients with acute cerebral infarction: a randomized controlled trial. Restor Neurol Neurosci. 2021;39(2):129–137. doi:10.3233/RNN-201080
28. Chen Y, Zhang Q, You N, et al. Analysis of influencing factors of neurological function recovery and cerebral hemorrhage transformation after intravenous thrombolysis in patients with acute ischemic stroke. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2020;32(11):1340–1345. doi:10.3760/cma.j.cn121430-20200713-00517 Dutch
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.







