Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Posterior Pericardial Window and a Single Pleural Drain: A Dual Defence Against Post-CABG Pericardial Effusion and Atrial Fibrillation
Authors Ranjan R , Kapetanakis S, Chandrasekaran V, Kaba RA, Momin AU
Received 17 February 2025
Accepted for publication 13 April 2025
Published 15 April 2025 Volume 2025:21 Pages 481—487
DOI https://doi.org/10.2147/TCRM.S521874
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Redoy Ranjan,1,2 Stamatis Kapetanakis,3 Venkatachalam Chandrasekaran,1 Riyaz A Kaba,4 Aziz U Momin1
1Department of Cardiac Surgery, St George’s University Hospitals NHS Foundation Trust, London, UK; 2Department of Cardiac Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh; 3Department of Cardiology, St Thomas’ Hospital, London, UK; 4Department of Cardiology, St George’s University Hospitals NHS Foundation Trust, London, UK
Correspondence: Aziz U Momin, Department of Cardiac Surgery, St George’s University Hospitals NHS Foundation Trust, London, UK, Tel +447956336739, Email [email protected]
Background: Postoperative new atrial fibrillation (POAF) commonly occurs after coronary artery bypass graft (CABG) and is often associated with postoperative pericardial effusion. We aimed to investigate the effectiveness of a posterior pericardial window (PPW) with a single left pleural drain in reducing post-CABG pericardial effusion and atrial fibrillation without mediastinal chest drains.
Methods: This descriptive observational study evaluated age and sex-adjusted isolated elective on-pump CABG patients into two groups: PPW with only left pleural chest drains and control (routine multiple mediastinal and pleural chest drains. We performed continuous telemonitoring for 96 hours after surgery to assess heart rhythm, followed by daily electrocardiograms. Bedside echocardiography was conducted on postoperative day 4 to check for pericardial effusion.
Results: This study evaluated age and sex-adjusted 250 CABG patients, with male predominance (80%) and identical comorbidities between study groups. We found similar age (61.5 ± 7.5 vs 62.6 ± 6.2, P =0.40) and male sex (86.9% vs 74.8%, P =0.13) between the PPW and control groups. Additionally, the sociodemographic and intraoperative variables were the same across the study groups (P > 0.05). The occurrence of > 1cm pericardial effusions (0.8% vs 14.1%, P < 0.001) and postoperative AF (6.9% vs 19.3%, P =0.002) occurrence was significantly lower in the PPW compared to the control group.
Conclusion: Despite similar clinical and operative profiles, a posterior pericardial window with a single left pleural drain effectively reduces pericardial effusion and the incidence of postoperative AF following CABG surgery.
Keywords: pericardiotomy, pericardial window, atrial fibrillation, coronary artery bypass graft
Introduction
Atrial fibrillation (AF) is a frequent complication after coronary artery bypass graft surgery (CABG), occurring in 20–40% of cases, usually within the first week and peaking on the second postoperative day.1,2 Despite technical advancements, the higher prevalence of post-CABG new AF (POAF) may be due to the increasing age and left atrial enlargement of the population undergoing revascularisation.2,3 Post-CABG atrial fibrillation was previously considered benign, but recent evidence shows it is independently associated with increased in-hospital and long-term mortality.4 The POAF occurrence is associated with early postoperative complications specifically haemodynamic instability, prolonged inotropic support, extended ventilation or re-intubation, use of intra-aortic balloon pump, and reoperation for bleeding.2–4
Cardiac arrhythmias necessitate a trigger and a susceptible substrate, including structural remodelling, atrial fibrosis, apoptosis, increased oxidative stress, and metabolic changes following CABG.1,5 Numerous studies suggest that b-blockers,6 antiarrhythmics,6 and the concept of “upstream” therapies7 may protect against postoperative new onset of AF. Upstream therapies, including renin-angiotensin-aldosterone system inhibitors, statins, and omega-3 fatty acids, may help prevent POAF by reducing inflammation, oxidative stress, and structural remodelling, modifying the atrial substrate, and intervening in specific mechanisms of AF.7,8 Additionally, pericardial effusions are a known post-CABG complication, and previous reports suggest a link between pericardial effusions and AF following CABG.9 Post-CABG pericardial effusion can trigger AF by causing mechanical irritation, inflammation, and increased atrial pressure, which induces atrial stretch and disrupts electrical conduction, promoting ectopic activity and re-entry circuits.10,11 Additionally, inflammatory cytokines contribute to atrial remodelling, increasing AF susceptibility in post-CABG patients. Insofar as existing literature found, effective post-CABG mediastinal drainage techniques include traditional chest tubes, Blake drains, and active suction systems.12–14 Although Blake drains offer less tissue trauma, conventional mediastinal chest drain tubes ensure efficient blood evacuation, preventing tamponade.14,15 Further, active suction systems, like vacuum-assisted drainage, enhance fluid removal from the pericardial and pleural cavities. However, proper positioning and timely removal of the drain tubes optimise post-CABG recovery and reduce complications.16,17
Creating a posterior pericardial window during CABG surgery may help prevent pericardial effusion and reduce the incidence of new-onset atrial fibrillation.9,17 We evaluated the effectiveness of this posterior pericardial window technique with single left pleural drains in reducing postoperative AF and pericardial collections by optimising mediastinal drainage compared to standard subxiphoid mediastinal and pleural drains.
Materials and Methods
This descriptive observational study recruited 250 age- and sex-adjusted isolated elective on-pump coronary artery bypass graft (ON-CABG) patients in a multi-surgeon practice at the King’s College Hospital and St George’s Hospital, London, UK. The study participants were divided into two groups: the posterior pericardial window with only left pleural chest drains (Case [PPW], n=115), while the second group received routine mediastinal and pleural chest drains (Control, n=135). We utilised purposive sampling techniques to included IHD patients who had undergone a first-time CABG surgery and had no history of atrial fibrillation (AF), other arrhythmias, or use of antiarrhythmic medications. Patients with a permanent pacemaker, valvular heart disease, acute coronary syndrome in the past month, renal dysfunction, or inflammatory diseases affecting the pericardium were excluded. All patients were administered routine statins prior to the operation. The primary endpoint was the development of postoperative AF during a hospital stay. Secondary endpoints were the presence of pericardial effusion on the fourth postoperative day and postoperative bleeding events. The ethics committee of the St George’s University Hospital NHS Foundation Trust reviewed the study and exempted ethical approval as this cohort was recruited as part of Service Evaluation and Improvement under the National Research Ethics Service, as well as part of the patient’s routine care under the adult NICOR (National Institute for Cardiovascular Outcomes Research) UK database. However, informed consent was obtained from all study participants. This research was conducted according to the Declaration of Helsinki, and the collected data were encrypted to ensure confidentiality.
Study Procedure
All included patients were seen at least one month before surgery in a pre-assessment clinic and the day before surgery, published elsewhere.3 At this juncture, a comprehensive preoperative history and examination were undertaken. All patients had their preoperative left ventricular function assessed during cardiac catheterisation. All operations were performed with standard anaesthetic and perfusion protocols under standard cardiopulmonary bypass (CPB) with extracorporeal circulation. A low-voltage diathermy was used to create a posterior pericardial window; a 4 cm cruciate incision was made parallel and posterior to the left phrenic nerve following the completion of distal coronary anastomoses. In the posterior pericardial window group, only left pleural chest drains were used until the right pleura was open and mediastinal chest drains were avoided. However, the control group had one anterior mediastinal chest drain (no drains behind the heart) and pleural drains as appropriate. After the routine reversal of heparin, we aimed to achieve an ACT time comparable to pre-heparinisation status after weaning from CPB to exclude the bias. The chest was closed, and drains were inserted with continuous suction (−5 kPA). According to the protocol described elsewhere,3 the drains for both groups were removed on the first day after the operation unless there was significant mediastinal bleeding, pneumothorax, or anything other than minimal drainage output for two consecutive hours.
Postoperative Management
This study was conducted following the National Health Services (NHS) Trust guidelines, and postoperatively, both groups of patients were treated utilising similar post-CABG protocols described elsewhere.3 Four days after CABG surgery, all subjects underwent 2D transthoracic echocardiography (TTE), blinded to the treatment groups, and conducted by the same operator. The echocardiography aimed to evaluate left ventricular function left atrial dimensions, and the presence of pericardial effusion. Any pericardial effusion greater than 1 cm was classified as significant. Late-onset effusions and cases of tamponade were documented and treated based on clinical requirements. Both groups received prophylactic beta-blockade during the first four days unless contraindicated by persistent hypotension or bradycardia. All patients were closely monitored for early clinical signs of pericardial effusion and tamponade. The study participants were monitored for 96 hours postoperatively using telemetry to observe for arrhythmias such as AF, confirmed by a standard 12-lead electrocardiogram. According to arterial blood gas analysis findings, a persistent arrhythmia (greater than 30 minutes) was treated with correction of serum potassium (K+) to ≥4.5 mmol/l and 20 mmol/l of Mg (magnesium) if needed. If the arrhythmia persisted, patients were commenced on Amiodarone. All other medical causes of AF were ruled out and treated. Patients were followed until discharge, and heart rhythm was assessed with daily electrocardiograms and 6-hourly clinical examinations for their hospital stay (beyond the first four days of continuous telemetry).
Statistical Analysis
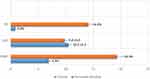
We utilised SPSS (Statistical Package for the Social Sciences) version 28.0 software (IBM SPSS Inc., NY, USA) for statistical analysis. Continuous data was expressed using the mean and standard deviation. Baseline and outcome variables between the case (pericardial window) and control groups were compared using Pearson’s chi-square or Fisher’s exact test for dichotomous data, as appropriate. A 3D bar chart and clustered bar chart illustrated operative and early postoperative outcomes, as applicable. The unpaired t-test was used for continuous variables with a normal distribution to compare the means of two independent groups. A P-value of less than 0.05 was considered to be statistically significant.
Results
This study evaluated age and sex-adjusted 250 isolated elective CABG patients, predominantly male (80%). We found that age (61.5 ±7.5 vs 62.6 ±6.2, P =0.40) and male sex (86.9% vs 74.8%, P =0.13) were similar between pericardial window (PW) and control groups. Additionally, there were no significant (P >0.05) differences between the study groups in diabetes, hypertension, CCS functional class, severity of CAD, previous MI, and left ventricular function (Table 1). Additionally, the number of distal coronary anastomoses (3.15 ±0.25 vs 2.85 ±.50, P =0.06), mean aortic cross-clamp time (41.2 ±28.5 vs 49.8 ±27.5, P =0.15), ventilation time (6.1 ±4.5 vs 5.7 ± 7.0, P=0.70) and total blood loss (895 ±502 mL vs 966 ±515 mL, P =0.40) were similar between the two groups (Figure 1).
 |
Table 1 Baseline Characteristics of the Study Population (N= 250) |
Although the length of hospital stay was similar (9.8 ±3.5 vs 10.5 ±2.5, P= 0.38), postoperative new AF (POAF) (19.3% vs 6.9%, P =0.002) and pericardial effusion (14.1% vs 0.8%, P <0.001) were significantly lower among the pericardial window group than the control population (Figure 2). There was no need to re-explore the bleeding in our cohort, and one mortality in each group was due to low cardiac output syndrome and suffered ventricular fibrillation arrest on postoperative days 6 and 20, respectively.
Discussion
We found post-CABG new-onset AF and pericardial effusion (>1cm) significantly lower among the pericardial window group than in the control sample despite similar clinical and operative profiles.
The pathogenesis of post-CABG AF is multifactorial, and pericardial effusion is an established and possibly avoidable trigger for postoperative new-onset AF.4,9,10 The exact mechanism for this association can only be speculated, which might be tissue ischemia due to diastolic compromise and possible intrapericardial oxidative stress and release of inflammatory mediators implicated in the pathogenesis of postoperative AF.5,10,18 Previous studies have suggested that the beneficial effect of posterior pericardiotomy on atrial fibrillation is driven by the more efficient drainage of potential postoperative effusions.8,19 Further, the use of mediastinal drains and their position could influence arrhythmias due to the direct contact of the silicon tube with the heart and its effect on patient comfort,5,19 which is why we avoided mediastinal drains utilising the pericardial window.
Despite the non-randomised nature of the study, there were no significant differences in established AF risk factors, such as age, obesity, and severity of coronary artery disease,20–22 between the posterior pericardiotomy and control groups, representing the robustness of the study findings. Nevertheless, the absence of a mediastinal drain may have increased the burden on the single pleural drain, leading to prolonged fluid accumulation in the chest cavity and subsequent risks of atelectasis and infection, leading to extended hospital stays and costs.23,24 However, we observed similar hospital stay durations between the study groups, likely due to the reduced incidence of atrial fibrillation, a common cause of delayed discharge.
Study Limitations
Despite the robustness of the study findings, the observational nature and small sample size are limitations that need to be acknowledged. However, age and sex-matched study populations with identical profiles mitigate the risk of selection and outcome bias. Although no specific thresholds for LA size were identified as being associated with postoperative AF in the UK population, the absence of detailed LA size data was a limitation of the study. Moreover, although the peak incidence of AF cases is observed on POD (postoperative days) 2 and 3, brief asymptomatic AF episodes may occur after POD 4, when telemonitoring is stopped. Daily ECGs and 6-hourly clinical examinations may not have detected these episodes. Further, the lack of details on AF episodes and data on the pro-BNP level also limits the findings, though these aspects were beyond the scope of our study objectives. While we observed a significant beneficial effect of the posterior pericardial window on postoperative AF, the underlying pathophysiological mechanism remains speculative. Further, this finding represents an association, not causation, and determining causality is beyond the scope of this study. Despite current findings contributing to the growing evidence supporting the benefits of a posterior pericardial window following CABG surgery, further large-scale studies with long-term follow-up data, particularly randomised controlled trials, may shed light on validating and strengthening the robustness of the results.
Conclusion
A posterior pericardial window is safe and effective following on-pump CABG, allowing for satisfactory mediastinum drainage preventing >1cm pericardial effusion, even without using a mediastinal drain, ultimately decreasing the incidence of POAF. We recommend further studies to evaluate how reducing early POAF following CABG affects long-term stroke risk and hospital readmissions.
Data Sharing Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions. The lead author Mr Aziz Momin had full access to all of the data in this study and took complete responsibility for the integrity of the data and the accuracy of the data analysis.
Patient and Public Involvement
Patients and the public were not involved in the design, conduct, reporting, or dissemination plans of this research.
Acknowledgments
We utilised the datasets from the Department of Cardiothoracic Surgery, King’s College Hospital, London, and we are grateful to Jatin Desai, Mansour T Sharabiani, and Ann-Marie R Howell for their kind cooperation.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare no conflict of interest in publication this paper.
References
1. Banach M, Kourliouros A, Reinhart KM, et al. Postoperative atrial fibrillation - what do we really know? Curr Vasc Pharmacol. 2010;8:553–572. doi:10.2174/157016110791330807
2. Kumar A, Ranjan R, Adhikary AB. Prevalence of postoperative atrial fibrillation following off-pump coronary artery bypass graft surgery in elderly patients. Cureus. 2023;15(2):e34499. doi:10.7759/cureus.34499
3. Momin AU, Sharabiani MT, Kapetanakis S, et al. Posterior pericardial window with single pleural drain prevents pericardial effusion and reduces atrial fibrillation after coronary artery BypassSurgery. J Heart Surg Treat. 2014;1(1):1–8.
4. Attaran S, Shaw M, Bond L, Pullan MD, Fabri BM. Atrial fibrillation postcardiac surgery: a common but a morbid complication. Interact Cardiovasc Thorac Surg. 2011;12:772–777. doi:10.1510/icvts.2010.243782
5. Kourliouros A, Yin X, Didangelos A, et al. Substrate modifications precede the development of atrial fibrillation after cardiac surgery: a proteomic study. Ann Thorac Surg. 2011;92:104–110. doi:10.1016/j.athoracsur.2011.03.071
6. Koniari I, Apostolakis E, Rogkakou C, Baikoussis NG, Dougenis D. Pharmacologic prophylaxis for atrial fibrillation following cardiac surgery: a systematic review. J Cardiothorac Surg. 2010;5:121. doi:10.1186/1749-8090-5-121
7. Kourliouros A, Savelieva I, Jahangiri M, Camm AJ. Atrial fibrillation: upstream therapies. In: Yusuf S, Cairns J, Camm AJ, Fallen EL, Gersh BJ, editors. Evidence-Based Cardiology. London: BMJ Books; 2009:568–580.
8. Savelieva I, Kakouros N, Kourliouros A, Camm AJ. Upstream therapies for management of atrial fibrillation: review of clinical evidence and implications for European Society of Cardiology guidelines. Part II: secondary prevention. Europace. 2011;13(5):610–625. doi:10.1093/europace/eur023
9. Farsak B, Gunaydin S, Tokmakoglu H, Kandemir O, Yorgancioglu C, Zorlutuna Y. Posterior pericardiotomy reduces the incidence of supra-ventricular arrhythmias and pericardial effusion after coronary artery bypass grafting. Eur J Cardiothorac Surg. 2002;22:278–281. doi:10.1016/S1010-7940(02)00259-2
10. Gaudino M, Di Franco A, Rong LQ, et al. Pericardial effusion provoking atrial fibrillation after cardiac surgery: JACC review topic of the week. J Am Coll Cardiol. 2022;79(25):2529–2539. doi:10.1016/j.jacc.2022.04.029
11. Kathrotia A, Hindupur MR. Massive purulent pericardial effusion presenting as atrial fibrillation with rapid rate: case report and review of the literature. Am J Case Rep. 2014;15:504–507. doi:10.12659/AJCR.889851
12. Bjessmo S, Hylander S, Vedin J, Mohlkert D, Ivert T. Comparison of three different chest drainages after coronary artery bypass surgery--a randomised trial in 150 patients. Eur J Cardiothorac Surg. 2007;31(3):372–375. doi:10.1016/j.ejcts.2006.12.027
13. Barozzi L, Biagio LS, Meneguzzi M, Courvoisier DS, Walpoth BH, Faggian G. Novel, digital, chest drainage system in cardiac surgery. J Card Surg. 2020;35(7):1492–1497. doi:10.1111/jocs.14629
14. Sakopoulos AG, Hurwitz AS, Suda RW, Goodwin JN. Efficacy of Blake drains for mediastinal and pleural drainage following cardiac operations. J Card Surg. 2005;20(6):574–577. doi:10.1111/j.1540-8191.2005.00138.x
15. Roberts N, Boehm M, Bates M, Braidley PC, Cooper GJ, Spyt TJ. Two-center prospective randomized controlled trial of Blake versus Portex drains after cardiac surgery. J Thorac Cardiovasc Surg. 2006;132(5):1042–1046. doi:10.1016/j.jtcvs.2006.06.031
16. Gomes DSO, Silva EJA, Silva JSE, Barbosa HCM, Guimarães AR, Cordeiro ALL. Impact of drains positioning on pulmonary function after coronary artery bypass grafting: an observational study. Braz J Anesthesiol. 2022;72(1):83–87. doi:10.1016/j.bjane.2021.06.010
17. Abdelaziz A, Hafez AH, Elaraby A, et al. Posterior pericardiotomy for the prevention of atrial fibrillation after cardiac surgery: a systematic review and meta-analysis of 25 randomised controlled trials. EuroIntervention. 2023;19(4):e305–e17. doi:10.4244/EIJ-D-22-00948
18. Kourliouros A, Karastergiou K, Nowell J, et al. Protective effect of epicardial adiponectin on atrial fibrillation following cardiac surgery. Eur J Cardiothorac Surg. 2011;39:228–232. doi:10.1016/j.ejcts.2010.05.006
19. Arbatli H, Demirsoy E, Aytekin S, et al. The role of posterior pericardiotomy on the incidence of atrial fibrillation after coronary revascularization. J Cardiovasc Surg. 2003;44:713–717.
20. Kumar A, Ranjan R, Adhikary AB. Postoperative atrial fibrillation following off-pump coronary artery bypass graft surgery: elderly versus young patients. Cureus. 2023;15(5):e39232. doi:10.7759/cureus.39232
21. Ranjan R, Adhikary D, Mandal S, Saha SK, Hasan K, Adhikary AB. Performance of EuroSCORE II and logistic EuroSCORE in Bangladeshi population undergoing off-pump coronary artery bypass surgery: a prospective cohort study. JRSM Cardiovasc Dis. 2019;8:2048004019862125. doi:10.1177/2048004019862125
22. Ranjan R, Adhikary AB. SYNTAX score and coronary artery bypass graft surgery in Bangladesh. Asian Cardiovasc Thorac Ann. 2019;27(7):542–547. doi:10.1177/0218492319869787
23. Brookes JDL, Williams M, Mathew M, Yan T, Bannon P. Pleural effusion post coronary artery bypass surgery: associations and complications. J Thorac Dis. 2021;13(2):1083–1089. doi:10.21037/jtd-20-2082
24. Brims FJ, Davies MG, Elia A, Griffiths MJ. The effects of pleural fluid drainage on respiratory function in mechanically ventilated patients after cardiac surgery. BMJ Open Respir Res. 2015;2(1):e000080. doi:10.1136/bmjresp-2015-000080
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.