Back to Journals » Journal of Pain Research » Volume 18
Postoperative Sore Throat After Tracheal Intubation: An Updated Narrative Review and Call for Action
Authors Chen Z , Zuo Z, Zhang L, Gong M, Ye Y, Jin Y , Zhao X
Received 1 October 2024
Accepted for publication 10 April 2025
Published 6 May 2025 Volume 2025:18 Pages 2285—2306
DOI https://doi.org/10.2147/JPR.S498933
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Zheping Chen,1,2,* Zhenxiang Zuo,3,4,* Le Zhang,2,4 Moxuan Gong,2,5 Yuyang Ye,2,4 Yanwu Jin,2,4,6 Xin Zhao2,4
1Shanghai Key Laboratory of Anesthesiology and Brain Functional Modulation, Translational Research Institute of Brain and Brain-Like Intelligence, Clinical Research Center for Anesthesiology and Perioperative Medicine, Department of Anesthesiology and Perioperative Medicine, Shanghai Fourth People’s Hospital, School of Medicine, Tongji University, Shanghai, 200434, People’s Republic of China; 2Department of Anesthesiology, The Second Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, 250033, People’s Republic of China; 3Department of Gastroenterology, The Second Hospital, Cheeloo College of Medicine, Shandong University, Jinan, Shandong, 250033, People’s Republic of China; 4The Second Clinical College, Shandong University, Jinan, Shandong, 250033, People’s Republic of China; 5Department of Pain, Shanghai Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, Shanghai, 200041, People’s Republic of China; 6Department of Anesthesiology and Perioperative Medicine, Shandong Public Health Clinical Center, Shandong University, Jinan, Shandong, 250100, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanwu Jin; Xin Zhao, Department of Anesthesiology, The Second Hospital, Cheeloo College of Medicine, Shandong University, 247 Bei Yuan Street, Jinan, Shandong, 250033, People’s Republic of China, Tel +86-17660085535 ; +86-17660085551, Email [email protected]; [email protected]
Background: Postoperative sore throat (POST) represents a common airway complication closely related to endotracheal tube (ETT), exhibiting a higher incidence following tracheal intubation compared to other airway apparatuses. Nevertheless, considering its mild and self-limiting character, POST is often overlooked. This study provides an updated narrative review on the latest perspectives regarding POST, including a comprehensive summary of its mechanisms, risk factors, clinical assessment methods, prevention and treatment strategies. Additionally, directions for future research are proposed.
Methods: A comprehensive search was conducted using keywords such as “postoperative sore throat” and “tracheal intubation” in PubMed, Web of Science, and Cochrane databases from their inception to October 2024. Two groups of reviewers independently performed data search and cleaning after standard training. To address gaps in knowledge or potential biases, the literature was thoroughly screened based on established criteria, and a comprehensive synthesis, analysis, and summary of the relevant findings was conducted.
Results: The precise cause of POST remains unknown, and its potential mechanism is believed to involve secondary inflammation triggered by irritation, mechanical trauma, tracheal intubation, and cuff inflation. The risk factors for POST encompass preoperative, intraoperative, and postoperative factors. Currently, effective prevention methods for POST consist of pharmacological interventions, non-pharmacological interventions, and traditional Chinese medicine (TCM) therapy. In terms of pharmacological interventions, non-steroidal anti-inflammatory drugs (NSAIDs) and steroid can effectively prevent the occurrence of POST through their anti-inflammatory properties. However, given the unavoidable side effects of medications, non-pharmacological interventions and non-invasive methods may offer greater benefits for POST and related hoarseness. For example, proficient and gentle intubation techniques can prevent mechanical injury caused by repeated intubation attempts. Currently, several studies have demonstrated the potential role of TCM in managing POST. Nonetheless, the precise mechanisms underlying its effects remain to be elucidated, and the available clinical evidence is still limited.
Conclusion: Given that POST is prevalent following tracheal intubation but frequently overlooked, we advocate heightened awareness of its occurrence and progression, and recommend integrating the prevention and management of POST into routine clinical practice.
Keywords: postoperative sore throat, tracheal intubation, risk factor, prevention
Introduction
Postoperative sore throat (POST) pertains to the throat pain or discomfort endured by patients after surgical operations carried out under general anesthesia (GA) or local anesthesia involving oral tracheal intubation or oropharyngeal airway.1,2 POST is a common postoperative complication that frequently emerges following extubation of endotracheal tube (ETT) in patients undergoing GA.2,3 Current research has demonstrated that the incidence of POST following GA varies from 12.1% to 70%.1,4 Notably, POST may occur in more severe forms in patients undergoing head or neck surgery or when placed in the prone position.1,4,5 The condition encompasses diverse disorders that occur in the early postoperative stage, such as pharyngitis, laryngitis, tracheitis, cough, hoarseness, and dysphagia.2 Previous clinical studies have primarily defined POST and hoarseness as endpoints.6 Patients frequently report POST following tracheal intubation, which may be accompanied by hoarseness.7–10 The incidence of these two complications is particularly elevated in cases involving prolonged surgical duration or improper intubation techniques. POST can prolong patients’ hospital stays, delay postoperative recovery, and potentially increase associated medical expenses.11,12 Consequently, POST has emerged as a critical perioperative concern that anesthesiologists must address.
In most cases, POST can heal by itself and is often overlooked in clinical practice.13,14 However, POST can cause a tonic spasm of the pharyngeal muscles. In severe cases, aspiration pneumonia may occur, significantly affecting the recovery of patients after anesthesia and the satisfaction of hospitalized patients.15–17 This is particularly evident after tracheal intubation, especially double-lumen tracheal intubation.18,19 Previous studies have demonstrated a significantly higher prevalence of POST following outpatient surgery with ETTs compared to patients with laryngeal masks (45.4% vs 17.5%).4
Mechanical injury, inflammatory responses, and procedural factors during tracheal intubation are associated with the occurrence of POST, but the precise molecular biological mechanisms remain incompletely understood.2,12 For example, the detailed cascade of inflammatory mediators involved in the progression of POST remains obscure. At present, numerous prevention and treatment approaches have been proposed to minimize POST (Figure 1 and Supplement Table 1). However, their efficacy and safety are still controversial. Owing to demographic variations among previous studies, such as differences in gender, age, and comorbidities, as well as inconsistencies in the details of preventive strategies—particularly the timing of drug administration—controversial results have been reported.1,20 This heterogeneity presents significant challenges in interpreting the clinical endpoints for preventing POST.
Considering the high incidence of POST after tracheal intubation, this review focuses on the occurrence mechanism of POST, the evaluation of POST, the risk factors, the current prevention and treatment methods, and future research trends. Given that POST has a high prevalence following endotracheal intubation and is frequently overlooked, this review emphasizes the importance of preventive measures and treatment of POST after tracheal intubation to improve medical care and promote enhanced recovery after surgery (ERAS).
Methodology
To ensure the inclusion of all potentially relevant articles, POST following tracheal intubation was discussed by reviewing published literature from PUBMED, Web of Science, and Cochrane. The keywords included “postoperative sore throat” and “tracheal intubation”. Two groups of reviewers independently performed data search and cleaning after standard training. The articles that met the following criteria were included: (1) the studies were written in English; (2) the studies focused on POST after tracheal intubation; and (3) the document type was original article, meta-analysis, or literature review.
Anatomical and Physiological Aspects of the Larynx and Pharynx
The larynx and pharynx are critical components of the respiratory system, with their structural and functional characteristics significantly influencing POST following tracheal intubation. The larynx is composed of several cartilages. The vocal cords, situated within the larynx, serve as the primary structures for sound production.21 In addition, the mucous membrane lining the larynx is richly vascularized and innervated, rendering it susceptible to irritation. The pharynx is anatomically divided into the nasopharynx, oropharynx, and laryngopharynx, each serving distinct functions in swallowing and respiration.21,22 The pharyngeal walls comprise muscular layers and smooth muscle that coordinate the mechanics of swallowing while providing a conduit for airflow.21,22
During the tracheal intubation process, the mucous membrane and neural structures of the larynx may sustain direct injury, resulting in a localized inflammatory response and subsequent pain. The vocal cords may also receive minor mechanical damage, leading to POST or hoarseness.23,24 Consequently, the larynx and pharynx are particularly vulnerable to injury and stimulation during intubation due to their anatomical and physiological characteristics, thereby contributing to the occurrence of POST.12,23
Development and Mechanism of POST After Tracheal Intubation
POST is primarily caused by injury to the supraglottic structures (possibly induced by laryngoscope insertion) and injury to the subglottic structures (possibly caused by tracheal intubation or cuffs).25,26 At present, the precise cause of POST remains unknown, and its potential mechanism is believed to involve secondary inflammation triggered by irritation, mechanical trauma, tracheal intubation, and cuff inflation.8,12 The current research findings indicate that the mechanisms of POST after tracheal intubation can be categorized into the following several major aspects.
The primary mechanism underlying POST following tracheal intubation is the stimulation induced by the ETT. During the tracheal intubation process, the insertion of the laryngoscope, such as the Macintosh laryngoscope, can cause mechanical injury to the pharyngeal area (Figure 2).27–30 The procedure of inserting an ETT can stimulate the glottis and the posterior pharyngeal wall, resulting in mucosal damage.31–33 Additionally, tracheal extubation procedures may also affect POST, as the extraction force during the removal of the tracheal intubation stylet, the duration of extubation, and coughing during extubation may cause injury.34–36 Moreover, the occurrence of POST may also be affected by the size, material of the ETT, and the pressure of the tracheal catheter cuff.37–42
 |
Figure 2 The process of tracheal intubation. |
In addition to tracheal intubation procedures, certain surgical operations can lead to direct injuries to laryngeal tissues, such as mucosal rupture and vascular rupture, thereby triggering inflammatory responses and pain and accelerating the occurrence of POST.43,44 During thyroid surgery, traction may cause repeated movement of the ETT, resulting in laryngeal edema. During the surgery, the ETT can be compressed, elevating the pressure of the cuff and the probability of inflammation, thereby expediting the occurrence of POST.45–47
Some recent studies have reported that drugs associated with GA may contribute to the occurrence of POST. Some anesthetic drugs may, through neurally mediated mechanisms, give rise to excitement and inflammatory responses, resulting in POST. For instance, low concentrations of nitrous oxide can stimulate the laryngeal sensory nerves, increase the pressure of the tracheal intubation cuff, and induce pain and discomfort.48 In addition, irritation caused by desflurane may result in coughing and POST.49,50 Fentanyl and other analgesic drugs might enhance the inflammatory response by acting on immune cells and inflammatory mediators.51
In summary, the mechanism of POST is complex and involves multiple aspects.52 POST typically results from a combination of various factors.52 Hence, targeted treatment and prevention for the relevant mechanisms have been proposed.
Risks Factors of POST After Tracheal Intubation
Several high-quality meta-analyses and clinical studies have conducted in-depth investigations into the risk factors of POST after tracheal intubation.1,4,20,23,40,50,53–62 The risk factors were summarized, which can primarily be classified into preoperative, intraoperative, and postoperative factors (Figure 3).
 |
Figure 3 Risk factors of POST after tracheal Intubation. Abbreviations: POST, Postoperative sore throat. Notes: Created in BioRender. Chen, Z (2024) BioRender.com/w63m753. |
Gender is a major determinant of POST. The incidence of POST following surgery in women is approximately 4%–11% higher compared to that in men. This could be attributed to the physiological characteristics of women. For instance, the laryngeal structure of women is narrower than that of men, thereby making them more vulnerable to the stimulation and injury caused by surgical procedures and tracheal intubation, increasing the occurrence of POST.63 Moreover, gender may also have an impact on the severity and duration of POST. This observation is highly likely to be correlated with the physiological traits and physiological cycles of women. For example, estrogen levels in women decline during menstruation, which may exacerbate the occurrence and severity of POST. The menstrual cycle of women is accompanied by significant hormonal fluctuations, inducing mood changes and leading to premenstrual syndrome (PMS), influencing the pain tolerance threshold.64 Furthermore, women react differently to opioid and non-opioid analgesics and typically require higher doses than men.65,66
Multiple studies have reported that the duration of anesthesia is also associated with POST, with prolonged anesthesia increasing the incidence of POST. Research has demonstrated that with an anesthesia duration of over 4 hours, cellulose within the tracheal lumen gradually seeps out and triggers a series of adverse reactions, such as submucosal congestion and the release of inflammatory substances, causing extensive damage to the laryngeal and airway epithelium.53,56,57,67,68
Among numerous risk factors, the utilization of succinylcholine remains controversial. Considering that succinylcholine can induce significant muscle fasciculation and striated muscle pain, succinylcholine was believed to heighten the risk of POST.4,69 Nevertheless, the outcomes of several studies remain inconclusive. Other studies reported that under standardized airway management, succinylcholine does not augment the risk of POST.70,71
Clinical Assessment of POST After Tracheal Intubation
In order to assess the occurrence and severity of POST, a series of scales have been adopted in the existing studies for evaluation (Table 1).
 |
Table 1 Clinical Assessment Scales of POST After Tracheal Intubation |
One commonly used scale is the Visual Analog Scale (VAS), which is prevalently acknowledged and employed approach for evaluating pain intensities in patients encountering POST. It offers a distinct and measurable means to assess the severity of POST by enabling individuals to denote their degree of discomfort on a scale spanning from 0 (signifying no sore throat) to 10 (representing the most severe throat discomfort conceivable).72
Another important tool is the Numeric Rating Scale (NRS), where patients rate their pain on a numerical scale, typically ranging from 0 (signifying no sore throat) to 10 (representing the utmost severe throat discomfort conceivable).73 In some studies, the NRS score is categorized into four levels—none, mild, moderate, and severe—to more precisely describe the severity of POST.
In addition to the VAS score, another commonly utilized rating scale within the domain of POST research is employed to assess the severity of this condition. This alternative scale classifies POST into diverse grades based on the extent of throat pain. Grade I indicates the absence of throat pain, while Grade II suggests mild discomfort during swallowing. Progressing in severity, Grade III represents continuous throat pain that deteriorates upon swallowing, and Grade IV indicates intense throat pain that impedes eating and demands rescue medication.18,73,74
In the research of Calabrese et al8 and Tazeh-Kand et al,75 a verbal scale, namely the Throat Pain Scale (TPS), was used as a supplement to the VAS scale to evaluate POST. TPS: 0 no throat pain; 1 mild (less than the common cold); 2 moderate (similar to the common cold); and 3 severe (more than the common cold).8,76,77
In addition to the assessment methods, the timing and duration of the evaluation hold paramount significance. Given that swallowing movements may enhance the incidence and severity of POST, certain studies have separately evaluated POST in the non-swallowing resting state and the swallowing state, yielding more objective and dependable outcomes.78 In clinical research, the follow-up and evaluation period of POST is mainly restricted to within 3 days after the surgery.18,79 POST is more prevalent within 6 hours after the surgery, and its incidence and severity gradually decline as time progresses.74 Thus, POST should be evaluated at multiple time points after the surgery.
Non-Pharmacological Prevention and Treatment of POST After Tracheal Intubation
Size and Type of ETT
The size and type of ETT can profoundly impact the incidence of POST. In airway management, the appropriate size and type of ETT should be selected, as a smaller ETT can mitigate the occurrence of POST. Specifically, for female patients, a 6.0 mm ETT is generally preferred over a 7.0 mm ETT; for male patients, a 7.0 mm ETT results in a lower POST occurrence compared to an 8.0 mm ETT.38,39,80–84 For double-lumen tubes (DLT), airway complications such as POST can be mitigated by selecting a DLT in which the inner diameters of the trachea and bronchus measured on the chest CT slice match the outer diameters of the tracheal and bronchial cuffs when inflated.85 Furthermore, the incidence of POST was significantly lower with the reinforced DLT made of silicone compared to that of the common DLT made of polyvinyl chloride (PVC).86
Cuff Pressure and Cuff Shape of ETT
A series of studies have been conducted to investigate the effects of cuff pressure on POST. Inflated endotracheal intubation cuffs can mitigate the risk of reflux and aspiration. However, excessive cuff pressure and prolonged hyperventilation may result in ischemic necrosis of the mucosa and elevate the risk of POST.1,87–89 Ryu et al90 indicated that maintaining the cuff pressure at approximately 25 cm H2O during thyroid surgery could prevent the occurrence of POST. In contrast, Lee et al55 reported that the cuff pressure should be restricted to 17 cm H2O. The discrepancy in results may be attributed to the different populations and surgical procedures. In some surgeries, increased airway pressure and cuff pressure are observed due to surgical procedures and body positions, such as pneumoperitoneum and the Trendelenburg position in gynecological surgeries.41 Hence, Zhu et al40 proposed a method for continuous monitoring of the cuff pressure to control the occurrence of POST.
In addition to the cuff pressure of the ETT, the shape of the ETT cuff also influences POST. A prior study demonstrated that tapered cuffs were associated with a lower incidence of POST than traditional cylindrical cuffs and simultaneously reduced the incidence of postoperative hoarseness.42 During anterior cervical surgery, the tapered cuff mitigates elevated pressure on the tracheal intubation cuff that may result from surgical procedures.91 Furthermore, when the head and neck are extended during intubation, the pressure exerted by a tapered cuff is significantly lower compared to that of a cylindrical cuff.92
Two-Handed Jaw Thrust
The two-handed jaw thrust maneuver elevates the epiglottis and the base of the tongue away from the posterior pharyngeal wall and enlarges the laryngeal aperture, thereby effectively reducing the damage during intubation.32 Several studies have demonstrated that the two-handed jaw thrust can effectively decrease the incidence and severity of POST within 24 hours after surgery in patients with ETT or DLT.32,33,93 Moreover, the study by Yang et al93 also indicates that the two-handed jaw thrust is more effective compared to the one-handed jaw thrust.
Thermal Softening
Thermal softening, achieved by heating, reduces the hardness of both ETT and DLT, effectively minimizing airway trauma during intubation. This approach was initially applied to DLT by Seo et al18 in 2016, revealing that DLT thermally softened at 40°C for 10 minutes could lower the incidence of postoperative POST and vocal cord injury. Several subsequent studies indicated that this method was also applicable to ETT and could also alleviate the related POST after DLT intubation in patients with SARS-CoV-2 infection and smokers.77,94,95 Similar to thermal softening, cold steam and ice cubes can decrease the occurrence of POST during the early postoperative stage; however, further studies are required to confirm these findings.96
180° Rotation
The intubation process of DLT is challenging due to requiring a 90° rotation after its tip passes through the vocal cords to achieve a complete position. However, this procedure might increase the risk of glottic injury and raise the incidence of POST. Therefore, Seo et al97 proposed a method of rotating 180° while passing through the glottis, which can effectively alleviate potential airway injuries. Rotating the DLT by 180° rather than 90° reduces the average intubation angle between DLT and the proximal trachea from an average of 66.6 ± 5.9 to merely 15.8 ± 5.9 degrees, leading to a decreased incidence of POST.98
Pharmacological Prevention and Treatment of POST After Tracheal Intubation
NSAIDs
The pharmacological attributes of nonsteroidal anti-inflammatory drugs (NSAIDs) include anti-inflammatory and analgesic effects. Previous research has investigated the impacts of several NSAIDs on POST, including benzydamine hydrochloride, flurbiprofen, ketoprofen,99 and others. Several clinical studies and meta-analyses have demonstrated the effectiveness of benzydamine hydrochloride in preventing POST, and its application has been recommended by a recent international Delphi-based consensus.11,45,100–104 Benzydamine hydrochloride not only inhibits the synthesis of inflammatory mediators but also exhibits analgesic and local anesthetic effects.101 Flurbiprofen is equally efficacious in preventing postoperative sore throat, which can be administered subglottically or orally.7,8 However, the efficacy of diclofenac in POST significantly varies between different routes of administration. Studies have demonstrated that diclofenac patches are more effective than intravenous administration for POST.105,106
Steroid
A meta-analysis conducted by Zhang et al107 revealed that corticosteroids may lower the incidence of postoperative POST and hoarseness. Furthermore, another meta-analysis indicated that corticosteroids were superior to lidocaine.108 Several subsequent clinical studies have confirmed the efficacy of corticosteroids for POST, such as inhaled fluticasone propionate,75 budesonide spray,109 betamethasone gel,110 etc. In addition, the meta-analysis conducted by Zhao et al111 indicated that dexamethasone can reduce POST one hour after surgery. Both 2 mg/kg and 8 mg intravenous (IV) dexamethasone have shown promising potential in preventing POST.72,112,113 However, corticosteroids are known to have significant side effects, especially when administered in high doses. Currently, further research is still necessary to ascertain their safety.
NMDA Receptor Antagonists
N-methyl-D-aspartic acid (NMDA) receptor antagonists have been extensively studied in recent years due to their favorable analgesic and anesthetic effects. Canbay et al114 investigated the influence of ketamine gargle (40 mg of ketamine dissolved in 30 mL of normal saline) on POST in 46 patients undergoing tracheal intubation under GA, revealing positive effects in preventing POST due to EET intubation. For DLT intubation, a higher dose of esketamine gargle (50 mg dissolved in 30 mL of normal saline) was found to alleviate POST and hemodynamic fluctuations associated with intubation.73 However, IV administration of a low dose of ketamine does not prevent EET-related POST.115 Another NMDA receptor antagonist, magnesium, has also demonstrated considerable potential for the prevention of POST. Several studies have shown that preoperative oral administration of lozenges containing 610 mg magnesium citrate or 250 mg magnesium gargles is effective for POST.116,117
Local Anesthetics
A growing number of studies have investigated the role of local anesthetics (LA) such as lidocaine in preventing POST. The study conducted by Soltani et al118 indicates that both inflating the ETT cuff with lidocaine or IV lidocaine can effectively reduce postoperative cough and POST, which is consistent with other studies.83,119–122 Moreover, lidocaine spray on the laryngeal structure has also shown efficacy in preventing POST.123,124 Early research findings revealed that lidocaine spray may increase the occurrence of POST rather than prevent it, which may be attributed to the function of the additives in the lidocaine spray rather than lidocaine itself.125 The application of 5% EMLA (lidocaine-prilocaine) cream on the ETT cuff can equally reduce the incidence and severity of POST, cough, and hoarseness in adults after GA in the early postoperative stage.76
Ultrasound-Guided Block of the Internal Branch of the Superior Laryngeal Nerve
The superior laryngeal nerve (SLN) is a branch of the vagus nerve, and its internal branch governs the sensation of the larynx above the glottis and the laryngeal mucosa. Ultrasound-guided block of the internal branch of the superior laryngeal nerve (US-guided iSLNB) can be achieved by administering local anesthetics such as lidocaine, ropivacaine, and bupivacaine around the superior laryngeal nerve. This technique provides efficient laryngeal anesthesia for awake endotracheal intubation and pain management. While US-guided iSLNB is classified as a peripheral nerve block (PNB), its efficacy relies on the pharmacological properties of the LA used, representing a pharmacologically driven intervention. Several previous studies have investigated the efficacy of US-guided iSLNB at different timings, such as preoperatively and postoperatively, in reducing ETT-related POST; the results demonstrated that the incidence of POST could be mitigated.78,126,127 Our previous study found that preoperative US-guided iSLNB, similar to the postoperative US-guided iSLNB, could alleviate DLT-related POST.74,128 Our other recent study showed that the use of dexmedetomidine combined with ropivacaine for US-guided iSLNB significantly reduced the incidence of POST.129 Although this approach has been proven effective for POST, this nerve block remains an invasive operation that inevitably causes damage.130 Anesthesiologists need to carefully weigh the benefits and risks.
α2-Adrenergic Receptor Agonists
Dexmedetomidine is an agonist of the α2-adrenergic receptor and is extensively utilized for sedation or adjunctive analgesia in the clinical setting. A meta-analysis conducted by Liu et al131 revealed that the intravenous injection of dexmedetomidine exerts a positive impact on preventing POST. In contrast to the systemic application of dexmedetomidine, the combination of intratracheal dexmedetomidine and ropivacaine significantly decreases the incidence and severity of POST, reduces the consumption of opioids, and stabilizes hemodynamics.132 Additionally, combining dexmedetomidine with the lidocaine gargle can effectively lower the VAS score associated with postoperative POST.133 Conversely, oral administration of clonidine exacerbates POST.134 Currently, studies on the systemic and local application of clonidine in POST are lacking.
Others
In addition to the aforementioned medications, a number of drug studies have recently been conducted to observe their efficacy on POST, including sodium azulene sulfonate gargle,135 Strepsils® tablets,136 chewing gum,137 and so on. Azulene, a chamomile extract, has anti-inflammatory effects, and sodium azulene sulfonate has been used in the treatment of gastritis and pharyngitis.138 Strepsils® tablets contain a variety of active ingredients, such as bactericidal ingredients and local anesthetics, which have antibacterial and pain-relieving effects and have been found to improve oral inflammatory diseases and oral mucosal damage in several previous studies.136 Chewing gum can promote saliva secretion by regulating the neurally mediated saliva reflex, and a variety of bioactive substances in saliva have the effect of lubricating and protecting the throat mucosa, which can reduce damage during tracheal intubation.139
Traditional Chinese Medicine Therapy of POST After Tracheal Intubation
Traditional Chinese Medicine
Licorice is a traditional Chinese medicine (TCM) that exhibits functions such as heat-clearing and detoxification, phlegm-eliminating, and cough-relieving. Glycyrrhizic acid, the primary constituent of licorice, exhibits a wide range of pharmacological properties, such as inhibiting inflammatory mediator release and alleviating pharyngeal edema associated with inflammation.140 The effect of licorice on POST has been extensively explored in previous studies. The meta-analysis carried out by Singh et al141 and Kuriyama et al142 suggested that licorice, similar to steroids and magnesium, is the most efficacious in preventing POST. Compared to rinsing the sugar-water gargle, licorice can halve the incidence rate of POST.140,143
Acupuncture Point Stimulation
Acupuncture point stimulation is a TCM technique. Some preclinical studies have conducted in-depth research on its mechanism and discovered that it can exert anti-inflammatory properties by activating specific signaling pathways.144,145 Jau et al146 conducted a meta-analysis to explore the potential of acupuncture stimulation in preventing POST, indicating that acupuncture stimulation could reduce the incidence of POST and demonstrated favorable safety. Similar outcomes were also found in several clinical investigations.147,148 Nevertheless, additional studies are required to elucidate the mechanism of acupuncture point stimulation in the prevention of ETT-related POST.
Innovative Technologies for the Assessment and Monitoring of POST
With advancements in medical technology and artificial intelligence (AI), machine learning (ML) has been employed to predict postoperative complications and inform anesthesia management during the perioperative period. Currently, machine learning can be employed to evaluate postoperative delirium (POD), acute kidney injury (AKI), and other complications.149,150 Additionally, ML has been developed within the realm of pain management to classify and quantify acute postoperative pain.151–153 Facial recognition technology may also serve as a tool for assessing pain levels during surgery.154,155 A prior study demonstrated that, in POST, the neural network (NN) outperformed extreme gradient boosting (XGBoost) and random forest (RF), achieving an area under the curve (AUC) of 0.81.156 Additionally, the advent of wearable devices facilitates real-time monitoring of postoperative pain intensity, which holds potential applications in POST.157
POST and Hoarseness
Hoarseness is defined as an alteration in voice quality, typically manifested as a rough, low-pitched, or monotone sound.158,159 This condition is generally associated with vocal cord dysfunction. During intubation, the placement of the endotracheal tube may induce direct mechanical stimulation, compression, or trauma to the vocal cords.160–162 Furthermore, variations in tracheal pressure, airflow dynamics, and localized inflammatory responses following prolonged intubation can further aggravate vocal cord injury.160
Research has demonstrated a significant correlation between POST and hoarseness.163 The onset of POST is frequently associated with inflammation and edema of the laryngeal tissues, which can disrupt the normal vibration of the vocal cords, resulting in hoarseness.164 This underscores the potential importance of managing POST to prevent subsequent hoarseness. Consequently, strategies aimed at preventing or managing POST may also prove effective in addressing postoperative hoarseness.8,72,110
Controversies
There is an ongoing debate regarding the efficacy of some interventions in preventing POST. A key factor contributing to this controversy is the heterogeneity of research samples.1,4,53,165 Different populations, including children, adults, and the elderly, exhibit varying tolerances to ETTs due to differences in their laryngeal physiological and anatomical structures and functions.166,167 At the baseline characteristics of the patients, pre-existing conditions such as chronic respiratory diseases and prior surgical history can influence the effectiveness of POST prevention, which are often overlooked.53,129,162 Preoperative psychological factors, including anxiety, depression, and sleep quality, have also been increasingly recognized as significant determinants of clinical outcomes.129,168,169 Moreover, variations in control group settings across studies, such as the use of blank controls versus alternative interventions, may complicate the interpretation of results. Considering that most significant POST studies have been single-center trials with varying conditions, future multi-center studies with larger sample sizes are required to validate the efficacy of these interventions.
Potential Conflict of Interest Bias
In this review, we systematically analyzed the funding sources of the included studies and found that the majority were predominantly supported by intramural departmental sources, such as hospitals, with only a minority receiving funding from government or non-profit organizations (Table 2). Additionally, in some studies, researchers reported that specific new equipment, such as ETT, was funded by companies.170,171 Despite these findings, none of the articles explicitly disclosed potential conflicts of interest that might influence study outcomes.
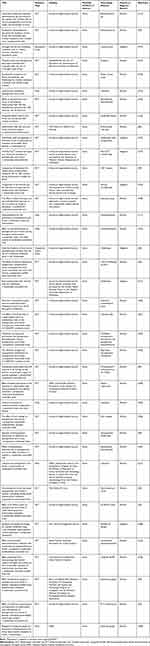 |
Table 2 Funding Sources and Related Information for Included Studies with Conflicts of Interest |
Given that the involvement of pharmaceutical companies in sponsoring trials or reviews may raise concerns about bias in result reporting, particularly in systematic reviews and meta-analyses where the inclusion or exclusion of certain studies can affect overall conclusions, we observed that only a limited number of systematic reviews and meta-analyses received funding from intramural departmental sources or the government.175,189
Future Research Trends
Currently, several preventive measures have been developed to reduce POST (Table 3). Undoubtedly, considering the side effects of drugs, non-pharmacological treatments offer superior prospects and safety. A previous meta-analysis revealed that providing non-pharmacological treatment prior to intubation was the most effective in reducing POST.190 Based on the relevant literature, several issues have been identified that urgently require attention.
 |
Table 3 Potential Prevention and Treatment of POST After Tracheal Intubation |
Firstly, new intervention measures are being developed to prevent POST, but their safety and efficacy require further verification. New advances in POST prevention methods, such as new endotracheal intubation technology and new cuff pressure monitoring devices, have greatly reduced the occurrence of POST. Secondly, the specific mechanism underlying POST requires further exploration, and the functional mechanisms of various drugs and intervention approaches remain elusive. Thirdly, the assessment methods for POST are simplistic, lacking objective assessment criteria and large-sample and multi-center clinical studies. Finally, while a specific variable was controlled in clinical research to assess its impact on POST, these methods are often employed in conjunction in actual clinical practice. For instance, the efficacy of US-guided iSLNB relies not only on the function of LA but also on the administration of PNB. Adjuncts such as corticosteroids can be incorporated into cuff pressure monitoring to enhance therapeutic outcomes; similarly, combining multiple agents, such as paracetamol and dexamethasone, could prove beneficial. Therefore, further studies are warranted to evaluate the advantages of combination therapy and to identify the most appropriate regimens for different patient populations, thereby optimizing clinical practice.
Conclusion
This review updates the prevailing viewpoints and elaborates on the mechanisms, risk factors, assessment approaches, and preventive measures related to POST after tracheal intubation. POST is a self-limiting disorder that is often disregarded; however, its incidence remains high and significantly affects postoperative recovery. Due to the unavoidable side effects of medications, some non-medicinal and non-invasive methods may be more beneficial for POST and related hoarseness. Resolving the existing controversies surrounding POST is essential for the development of comprehensive guidelines and consensus, which will aid in the prevention of POST and enhance patient quality of recovery and satisfaction. In line with the notions of ERAS and comfortable medical care, we advocate heightened awareness of its occurrence and progression, and recommend integrating the prevention and management of POST into routine clinical practice.
Acknowledgments
The authors thank all the research assistants for their time and efforts in this review. We thank biorender (www.biorender.com) for expert assistance in Figure 3. The authors also thank Home for Researchers editorial team (www.home-for-researchers.com) for language editing service.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by 2023 Qilu medical characteristics undergraduate education teaching research project-Shandong University (No. qlyxjy-202367) and Shandong Provincial Natural Science Foundation (ZR2022QH328).
Disclosure
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
1. El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a systematic review. Anaesthesia. 2016;71(6):706–717. doi:10.1111/anae.13438
2. McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia. 1999;54(5):444–453. doi:10.1046/j.1365-2044.1999.00780.x
3. Scuderi PE. Postoperative sore throat: more answers than questions. Anesthesia Analg. 2010;111(4):831–832. doi:10.1213/ANE.0b013e3181ee85c7
4. Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth. 2002;88(4):582–584. doi:10.1093/bja/88.4.582
5. Luo D, Su Y, Pang Y. Effects of ultrasound-guided stellate ganglion block on postoperative sore throat and postoperative sleep disturbance after lumbar spine surgery: a randomized controlled trial. BMC Anesthesiol. 2023;23(1):343. doi:10.1186/s12871-023-02301-y
6. Bennett MH, Isert PR, Cumming RG. Postoperative sore throat and hoarseness following tracheal intubation using air or saline to inflate the cuff--a randomized controlled trial. Anaesthesia Intensive Care. 2000;28(4):408–413. doi:10.1177/0310057x0002800409
7. Muderris T, Tezcan G, Sancak M, Gul F, Ugur G. Oral flurbiprofen spray for postoperative sore throat and hoarseness: a prospective, randomized, double-blind, placebo-controlled study. Minerva Anestesiol. 2019;85(1):21–27. doi:10.23736/s0375-9393.18.12703-9
8. Calabrese M, Arlotta G, Antoniucci ME, et al. Flurbiprofen in the subglottic space to prevent postoperative sore throat after cardiac surgery: a randomized double-blind study. J Clinical Anesthesia. 2024;95:111418. doi:10.1016/j.jclinane.2024.111418
9. Shui W, Hu W, Ma W, et al. The effects of video double-lumen tubes on intubation complications in patients undergoing thoracic surgery: a randomised controlled study. Eur J Anaesthesiol. 2024;41(4):305–313. doi:10.1097/eja.0000000000001959
10. Zhou H, Fei Y, Zhang Y, Quan X, Yi J. Individualized rotation of left double lumen endobronchial tube to improve placement success rate: a randomized controlled trial. Respir Res. 2024;25(1):184. doi:10.1186/s12931-024-02799-x
11. Kuriyama A, Aga M, Maeda H. Topical benzydamine hydrochloride for prevention of postoperative sore throat in adults undergoing tracheal intubation for elective surgery: a systematic review and meta-analysis. Anaesthesia. 2018;73(7):889–900. doi:10.1111/anae.14224
12. Mazzotta E, Soghomonyan S, Hu L-Q. Postoperative sore throat: prophylaxis and treatment. Front Pharmacol. 2023;14:1284071. doi:10.3389/fphar.2023.1284071
13. Oo S, Chia RHX, Li Y, et al. Bronchial rupture following endobronchial blocker placement: a case report of a rare, unfortunate complication. BMC Anesthesiol. 2021;21(1):208. doi:10.1186/s12871-021-01430-6
14. Flexman AM, Duggan LV. Maux de gorge postopératoires: effet secondaire inéluctable ou désagrément évitable? Canadian J Anesthesia. 2019;66(9):1009–1013. doi:10.1007/s12630-019-01397-6
15. Tong D, Chung F, Wong D. Predictive factors in global and anesthesia satisfaction in ambulatory surgical patients. Anesthesiology. 1997;87(4):856–864. doi:10.1097/00000542-199710000-00020
16. Hailu S, Shiferaw A, Regasa T, Getahun YA, Mossie A, Besha A. Incidence of Postoperative Sore Throat and Associated Factors Among Pediatric Patients Undergoing Surgery Under General Anesthesia at Hawassa University Comprehensive Specialized Hospital, a Prospective Cohort Study. International Journal of General Medicine. 2023;16:589–598. doi:10.2147/ijgm.S397519
17. Lee JH, Kim SB, Lee W, et al. Effects of topical dexamethasone in postoperative sore throat. Korean J Anesthesiol. 2017;70(1):58–63. doi:10.4097/kjae.2017.70.1.58
18. Seo JH, Cho CW, Hong DM, Jeon Y, Bahk JH. The effects of thermal softening of double-lumen endobronchial tubes on postoperative sore throat, hoarseness and vocal cord injuries: a prospective double-blind randomized trial. Br J Anaesth. 2016;116(2):282–288. doi:10.1093/bja/aev414
19. Mourisse J, Liesveld J, Verhagen A, et al. Efficiency, efficacy, and safety of EZ-blocker compared with left-sided double-lumen tube for one-lung ventilation. Anesthesiology. 2013;118(3):550–561. doi:10.1097/ALN.0b013e3182834f2d
20. Mitobe Y, Yamaguchi Y, Baba Y, et al. A Literature Review of Factors Related to Postoperative Sore Throat. J Clin Medicine Res. 2022;14(2):88–94. doi:10.14740/jocmr4665
21. Strohl KP, Butler JP, Malhotra A. Mechanical properties of the upper airway. Compr Physiol. 2012;2(3):1853–1872. doi:10.1002/cphy.c110053
22. Sahin-Yilmaz A, Naclerio RM. Anatomy and physiology of the upper airway. Proc Am Thorac Soc. 2011;8(1):31–39. doi:10.1513/pats.201007-050RN
23. Obsa MS, Adem AO, Bancha B, et al. Global incidence and risk factors of post-operative sore throat among patients who underwent surgery: a systematic review and meta-analysis. Review. Int J Surg Open. 2022;47:
24. Donner MW, Bosma JF, Robertson DL. Anatomy and physiology of the pharynx. Gastrointestinal Radiol. 1985;10(3):196–212.
25. Puyo CA, Peruzzi D, Earhart A, et al. Endotracheal tube-induced sore throat pain and inflammation is coupled to the release of mitochondrial DNA. Molecular Pain. 2017;13:1744806917731696. doi:10.1177/1744806917731696
26. Levin PD, Chrysostomos C, Ibarra CA, et al. Causes of sore throat after intubation: a prospective observational study of multiple anesthesia variables. Minerva Anestesiol. 2017;83(6):582–589. doi:10.23736/s0375-9393.17.11419-7
27. Tachibana N, Niiyama Y, Yamakage M. Less postoperative sore throat after nasotracheal intubation using a fiberoptic bronchoscope than using a Macintosh laryngoscope: a double-blind, randomized, controlled study. J Clinical Anesthesia. 2017;39:113–117. doi:10.1016/j.jclinane.2016.10.026
28. Aqil M, Khan MU, Mansoor S, Mansoor S, Khokhar RS, Narejo AS. Incidence and severity of postoperative sore throat: a randomized comparison of Glidescope with Macintosh laryngoscope. BMC Anesthesiol. 2017;17(1):127. doi:10.1186/s12871-017-0421-4
29. Kapadia AA, Shafiq F, Raza A. Post operative sore throat: comparison between Macintosh versus Video Laryngoscope in patients intubated by trainee anaesthetists - A Randomised Control Trial. Pakistan J Med Sci. 2021;37(3):764–769. doi:10.12669/pjms.37.3.3365
30. Cirilla II DJ, Ngo J, Vaisman V, et al. Does the incidence of sore throat postoperatively increase with the use of a traditional intubation blade or the GlideScope? J Clinical Anesthesia. 2015;27(8):646–651. doi:10.1016/j.jclinane.2015.06.005
31. Kim H, Kim JE, Kim Y, Hong SW, Jung H. Slow advancement of the endotracheal tube during fiberoptic-guided tracheal intubation reduces the severity of postoperative sore throat. Sci Rep. 2023;13(1):7709. doi:10.1038/s41598-023-34879-1
32. Huh H, Go DY, Cho JE, Park J, Lee J, Kim HC. Influence of two-handed jaw thrust during tracheal intubation on postoperative sore throat: a prospective randomised study. J Int Med Res. 2021;49(2):300060520961237. doi:10.1177/0300060520961237
33. Park JJ, Huh H, Yoon SZ, et al. Two-handed jaw thrust decreases postoperative sore throat in patients undergoing double-lumen endobronchial intubation: a randomised study. Eur J Anaesthesiol. 2020;37(2):105–112. doi:10.1097/eja.0000000000001149
34. Sakkanan NV, Elakkumanan LB. Extubation Parameters and Postoperative Sore Throat. Anesthesia Analg. 2020;130(2):e42–e43. doi:10.1213/ane.0000000000004549
35. Kusunoki T, Sawai T, Komasawa N, Shimoyama Y, Minami T. Correlation between extraction force during tracheal intubation stylet removal and postoperative sore throat. J Clinical Anesthesia. 2016;33:37–40. doi:10.1016/j.jclinane.2015.12.024
36. Minogue SC, Ralph J, Lampa MJ. Laryngotracheal topicalization with lidocaine before intubation decreases the incidence of coughing on emergence from general anesthesia. Anesthesia Analg. 2004;99(4):1253–1257. doi:10.1213/01.Ane.0000132779.27085.52
37. Wang C, Yan X, Gao C, et al. Effect of continuous measurement and adjustment of endotracheal tube cuff pressure on postoperative sore throat in patients undergoing gynecological laparoscopic surgery: a randomized controlled trial. J Clin Monitoring Comput. 2024;2024:1. doi:10.1007/s10877-024-01173-y
38. Christiansen P, Pedersen CH, Selter H, et al. How Does Tube Size Affect Patients’ Experiences of Postoperative Sore Throat and Hoarseness? A Randomised Controlled Blinded Study. J Clin Med. 2021;10(24):5846. doi:10.3390/jcm10245846
39. Hu B, Bao R, Wang X, et al. The size of endotracheal tube and sore throat after surgery: a systematic review and meta-analysis. PLoS One. 2013;8(10):e74467. doi:10.1371/journal.pone.0074467
40. Zhu G, Wang X, Cao X, et al. The effect of different endotracheal tube cuff pressure monitoring systems on postoperative sore throat in patients undergoing tracheal intubation: a randomized clinical trial. BMC Anesthesiol. 2024;24(1):115. doi:10.1186/s12871-024-02499-5
41. Geng G, Hu J, Huang S. The effect of endotracheal tube cuff pressure change during gynecological laparoscopic surgery on postoperative sore throat: a control study. J Clin Monitoring Comput. 2015;29(1):141–144. doi:10.1007/s10877-014-9578-2
42. Chang JE, Kim H, Han SH, Lee JM, Ji S, Hwang JY. Effect of Endotracheal Tube Cuff Shape on Postoperative Sore Throat After Endotracheal Intubation. Anesthesia Analg. 2017;125(4):1240–1245. doi:10.1213/ane.0000000000001933
43. Okui A, Konomi U, Watanabe Y. Complaints and Complications of Microlaryngoscopic Surgery. J Voice. 2020;34(6):949–955. doi:10.1016/j.jvoice.2019.05.006
44. Borna R, McCleary S, Wang L, et al. Effect of Throat Pack Placement on the Incidence of Sore Throat and Postoperative Nausea and Vomiting in Septorhinoplasty Patients: a Randomized Controlled Trial. Aesthetic Surg J. 2022;42(7):743–748. doi:10.1093/asj/sjab410
45. Kim D, Jeong H, Kwon J, et al. The effect of benzydamine hydrochloride on preventing postoperative sore throat after total thyroidectomy: a randomized-controlled trial. Can J Anaesthesia. 2019;66(8):934–942. doi:10.1007/s12630-019-01371-2
46. Sanabria A, Betancourt C, Chiesa-Estomba C, et al. Locoregional strategies to decrease postoperative pain and neck discomfort after open thyroidectomy: a scoping review. Head Neck. 2023;45(7):1841–1855. doi:10.1002/hed.27392
47. Jung TH, Rho JH, Hwang JH, Lee JH, Cha SC, Woo SC. The effect of the humidifier on sore throat and cough after thyroidectomy. Korean J Anesthesiol. 2011;61(6):470–474. doi:10.4097/kjae.2011.61.6.470
48. Braz JR, Volney A, Navarro LH, Braz LG, Nakamura G. Does sealing endotracheal tube cuff pressure diminish the frequency of postoperative laryngotracheal complaints after nitrous oxide anesthesia? J Clinical Anesthesia. 2004;16(5):320–325. doi:10.1016/j.jclinane.2004.03.001
49. White PF, Tang J, Wender RH, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesthesia Analg. 2009;109(2):387–393. doi:10.1213/ane.0b013e3181adc21a
50. Park JH, Lee YC, Lee J, Kim S, Kim HC. Influence of intraoperative sevoflurane or desflurane on postoperative sore throat: a prospective randomized study. J Anesthesia. 2019;33(2):209–215. doi:10.1007/s00540-018-2600-y
51. Huang C, Huang Q, Shen Y, Liu K, Wu J. General anaesthesia with double-lumen intubation compared to opioid-sparing strategies with laryngeal mask for thoracoscopic surgery: a randomised trial. Anaesth Crit Care Pain Med. 2022;41(3):101083. doi:10.1016/j.accpm.2022.101083
52. McCarthy DT. Postoperative sore throat: a multifactorial problem. Br J Anaesth. 2012;108(6):1037–1038. doi:10.1093/bja/aes155
53. Jiang J, Wang Z, Xu Q, Chen Q, Lu W. Development of a nomogram for prediction of postoperative sore throat in patients under general anaesthesia: a single-centre, prospective, observational study. BMJ open. 2022;12(5):e059084. doi:10.1136/bmjopen-2021-059084
54. Jensen PJ, Hommelgaard P, Søndergaard P, Eriksen S. Sore throat after operation: influence of tracheal intubation, intracuff pressure and type of cuff. Br J Anaesth. 1982;54(4):453–457. doi:10.1093/bja/54.4.453
55. Lee JY, Sim WS, Kim ES, et al. Incidence and risk factors of postoperative sore throat after endotracheal intubation in Korean patients. J Int Med Res. 2017;45(2):744–752. doi:10.1177/0300060516687227
56. Bekele Z, Melese Z. Incidence and risk factors for postoperative sore throat after general anesthesia with endotracheal intubation: prospective cohort study. Ann Med Surg. 2023;85(6):2356–2361. doi:10.1097/ms9.0000000000000786
57. Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: a prospective evaluation. Eur J Anaesthesiol. 2005;22(4):307–311. doi:10.1017/s0265021505000529
58. Loeser EA, Bennett GM, Orr DL, Stanley TH. Reduction of postoperative sore throat with new endotracheal tube cuffs. Anesthesiology. 1980;52(3):257–259. doi:10.1097/00000542-198003000-00011
59. Clayton-Smith A, Bennett K, Alston RP, et al. A Comparison of the Efficacy and Adverse Effects of Double-Lumen Endobronchial Tubes and Bronchial Blockers in Thoracic Surgery: a Systematic Review and Meta-analysis of Randomized Controlled Trials. J Cardiothoracic Vascular Anesthesia. 2015;29(4):955–966. doi:10.1053/j.jvca.2014.11.017
60. Zheng ZP, Tang SL, Fu SL, et al. Identifying the Risk Factors for Postoperative Sore Throat After Endotracheal Intubation for Oral and Maxillofacial Surgery. Therapeut Clinical Risk Manage. 2023;19:163–170. doi:10.2147/tcrm.S396687
61. Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB. Postoperative throat complaints after tracheal intubation. Br J Anaesth. 1994;73(6):786–787. doi:10.1093/bja/73.6.786
62. Tadesse MA, Alimawu AA, Kebede FS, Alemu EA, Matrisch L, Waktasu DO. Effectiveness of preoperative ketamine gargle to reduce postoperative sore throat in adult patients undergoing surgery with endotracheal tube; systematic review and meta-analysis of randomized control trials. BMC Anesthesiol. 2024;24(1):449. doi:10.1186/s12871-024-02837-7
63. Myles PS, Hunt JO, Moloney JT. Postoperative ‘minor’ complications. Comparison between men and women. Anaesthesia. 1997;52(4):300–306. doi:10.1111/j.1365-2044.1997.89-az0091.x
64. Riley III JL, Robinson ME, Wise EA, Price D. A meta-analytic review of pain perception across the menstrual cycle. Pain. 1999;81(3):225–235. doi:10.1016/s0304-3959(98)00258-9
65. Dahan A, Sarton E, Teppema L, Olievier C. Sex-related differences in the influence of morphine on ventilatory control in humans. Anesthesiology. 1998;88(4):903–913. doi:10.1097/00000542-199804000-00009
66. Gear RW, Miaskowski C, Gordon NC, Paul SM, Heller PH, Levine JD. Kappa-opioids produce significantly greater analgesia in women than in men. Nat Med. 1996;2(11):1248–1250. doi:10.1038/nm1196-1248
67. Zhou Z, Gao L, Lv Z, et al. Prediction of Postoperative Sore Throat in Patients After Day-case Surgery With General Anesthesia: a Retrospective Study. J Perianesthesia Nurs. 2024;2024:2. doi:10.1016/j.jopan.2024.03.022
68. Teshome D, Fenta E, Mekete G, et al. Prevalence and factors associated with postoperative sore throat in Ethiopia: a systemic review and meta-analysis, 2023. Preventive Med Rep. 2024;45:102818. doi:10.1016/j.pmedr.2024.102818
69. Capan LM, Bruce DL, Patel KP, Turndorf H. Succinylcholine-induced postoperative sore throat. Anesthesiology. 1983;59(3):202–206.
70. Mencke T, Knoll H, Schreiber JU, et al. Rocuronium is not associated with more vocal cord injuries than succinylcholine after rapid-sequence induction: a randomized, prospective, controlled trial. Anesthesia Analg. 2006;102(3):943–949. doi:10.1213/01.ane.0000194509.03916.02
71. Jøorgensen LN, Weber M, Pedersen A, Münster M. No increased incidence of postoperative sore throat after administration of suxamethonium in endotracheal anaesthesia. Acta anaesthesiologica Scandinavica. 1987;31(8):768–770. doi:10.1111/j.1399-6576.1987.tb02661.x
72. Park SH, Han SH, Do SH, Kim JW, Rhee KY, Kim JH. Prophylactic dexamethasone decreases the incidence of sore throat and hoarseness after tracheal extubation with a double-lumen endobronchial tube. Anesthesia Analg. 2008;107(6):1814–1818. doi:10.1213/ane.0b013e318185d093
73. Liang J, Liu J, Qiu Z, et al. Effect of Esketamine Gargle on Postoperative Sore Throat in Patients Undergoing Double-Lumen Endobronchial Intubation: a Randomised Controlled Trial. Drug Des Devel Ther. 2023;17:3139–3149. doi:10.2147/dddt.S430077
74. Chen Z, Jin Y, Lu G, Jin Y, Feng C, Zhao X. Preoperative Ultrasound-Guided Internal Branch Block of Superior Laryngeal Nerve Reduces Postoperative Sore Throat Caused by Double Lumen Endotracheal Intubation: a Randomized Trial. Anesthesia Analg. 2023;137(6):1270–1278. doi:10.1213/ane.0000000000006534
75. Tazeh-Kand NF, Eslami B, Mohammadian K. Inhaled fluticasone propionate reduces postoperative sore throat, cough, and hoarseness. Anesthesia Analg. 2010;111(4):895–898. doi:10.1213/ANE.0b013e3181c8a5a2
76. Murugaiyan A, Sahoo AK, Rao PB, Misra S. Effect of 5% EMLA Cream on Postoperative Sore Throat in Adults Following General Endotracheal Anesthesia: a Randomized Placebo-Controlled Study. Anesthesia Analg. 2023;136(2):338–345. doi:10.1213/ane.0000000000006269
77. Yan W, Cai J, Zhu C, et al. Effect of thermal softening of double-lumen endobronchial tubes on postoperative sore throat in patients with prior SARS-CoV-2 infection: a randomized controlled trial. BMC Anesthesiol. 2023;23(1):403. doi:10.1186/s12871-023-02363-y
78. Bao Y, Xiong J, Wang H, Zhang Y, Zhong Q, Wang G. Ultrasound-Guided Block of the Internal Branch of the Superior Laryngeal Nerve Reduces Postoperative Sore Throat Caused by Suspension Laryngoscopic Surgery: a Prospective Randomized Trial. Fronti Surg. 2022;9:829811. doi:10.3389/fsurg.2022.829811
79. Nakanishi T, Sento Y, Kamimura Y, et al. Combined use of the ProSeal laryngeal mask airway and a bronchial blocker vs. a double-lumen endobronchial tube in thoracoscopic surgery: a randomized controlled trial. J Clinical Anesthesia. 2023;88:111136. doi:10.1016/j.jclinane.2023.111136
80. Jaensson M, Gupta A, Nilsson U. Gender differences in sore throat and hoarseness following endotracheal tube or laryngeal mask airway: a prospective study. BMC Anesthesiol. 2014;14:56. doi:10.1186/1471-2253-14-56
81. Cho HY, Yang SM, Jung CW, et al. A randomised controlled trial of 7.5-mm and 7.0-mm tracheal tubes vs. 6.5-mm and 6.0-mm tracheal tubes for men and women during laparoscopic surgery. Anaesthesia. 2022;77(1):54–58. doi:10.1111/anae.15568
82. Jaensson M, Olowsson LL, Nilsson U. Endotracheal tube size and sore throat following surgery: a randomized-controlled study. Acta anaesthesiologica Scandinavica. 2010;54(2):147–153. doi:10.1111/j.1399-6576.2009.02166.x
83. Xu YJ, Wang SL, Ren Y, Zhu Y, Tan ZM. A smaller endotracheal tube combined with intravenous lidocaine decreases post-operative sore throat - a randomized controlled trial. Acta anaesthesiologica Scandinavica. 2012;56(10):1314–1320. doi:10.1111/j.1399-6576.2012.02768.x
84. Karmali S, Rose P. Tracheal tube size in adults undergoing elective surgery - a narrative review. Anaesthesia. 2020;75(11):1529–1539. doi:10.1111/anae.15041
85. Cui G, Zhao L, Chi C, Liang S, Liu Z. The feasibility and accuracy of the method for selecting the optimal size of double-lumen tube in thoracic surgery: a prospective, randomized controlled trial. Sci Rep. 2024;14(1):17539. doi:10.1038/s41598-024-68349-z
86. Jeon J, Lee K, Ahn G, Lee J, Hwang W. Comparison of postoperative sore throat and hoarseness between two types of double-lumen endobronchial tubes: a randomized controlled trial. J Cardiothoracic Vascular Anesthesia. 2015;29(1):121–125. doi:10.1053/j.jvca.2014.05.028
87. Veld BA, Rettig TCD, De Heij N, De Vries J, Wolfs JFC, Arts MP. Maintaining endotracheal tube cuff pressure at 20 mmHg during anterior cervical spine surgery to prevent dysphagia: a double-blind randomized controlled trial. Eur Spine J. 2019;28(2):353–361. doi:10.1007/s00586-018-5798-3
88. Liu J, Zhang X, Gong W, et al. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesthesia Analg. 2010;111(5):1133–1137. doi:10.1213/ANE.0b013e3181f2ecc7
89. Ratnaraj J, Todorov A, McHugh T, Cheng MA, Lauryssen C. Effects of decreasing endotracheal tube cuff pressures during neck retraction for anterior cervical spine surgery. J Neurosurg. 2002;97(2 Suppl):176–179. doi:10.3171/spi.2002.97.2.0176
90. Ryu JH, Han SS, Do SH, Lee JM, Lee SC, Choi ES. Effect of adjusted cuff pressure of endotracheal tube during thyroidectomy on postoperative airway complications: prospective, randomized, and controlled trial. World J Surg. 2013;37(4):786–791. doi:10.1007/s00268-013-1908-x
91. Li YS, Tan EC, Tsai YJ, et al. A Tapered Cuff Tracheal Tube Decreases the Need for Cuff Pressure Adjustment After Surgical Retraction During Anterior Cervical Spine Surgery: a Randomized Controlled, Double-Blind Trial. Front Med. 2022;9:920726. doi:10.3389/fmed.2022.920726
92. Seol G, Jin J, Oh J, Byun SH, Jeon Y. Pressure changes in tapered and cylindrical shaped cuff after extension of head and neck: a randomized controlled trial. World J Clin Cases. 2022;10(31):11419–11426. doi:10.12998/wjcc.v10.i31.11419
93. Yang SM, Kim H, Chang JE, Min SW, Lee JM, Hwang JY. A comparison of single-handed chin lift and two-handed jaw thrust for tracheal intubation using a lightwand. J Anesthesia. 2017;31(1):5–10. doi:10.1007/s00540-016-2276-0
94. Yu JH, Paik HS, Ryu HG, Lee H. Effects of thermal softening of endotracheal tubes on postoperative sore throat: a randomized double-blinded trial. Acta anaesthesiologica Scandinavica. 2021;65(2):213–219. doi:10.1111/aas.13705
95. Bi X, Wen J, Chen Q, Zhang X. Effects of Thermal Softening of Double-Lumen Endobronchial Tubes on the Prevention of Postoperative Sore Throat in Smokers: a Randomized Controlled Trial. J Cardiothoracic Vascular Anesthesia. 2022;36(8 Pt B):3109–3113. doi:10.1053/j.jvca.2022.04.017
96. Şahbaz M, Khorshid L. The Effect of Cold Vapor and Ice Cube Absorption in the Early Postoperative Period on Sore Throat and Hoarseness Induced by Intubation. J Perianesthesia Nurs. 2020;35(5):518–524. doi:10.1016/j.jopan.2019.12.007
97. Seo JH, Kwon TK, Jeon Y, Hong DM, Kim HJ, Bahk JH. Comparison of techniques for double-lumen endobronchial intubation: 90° or 180° rotation during advancement through the glottis. Br J Anaesth. 2013;111(5):812–817. doi:10.1093/bja/aet203
98. Cameron RB, Peacock WJ, Chang XG, Shin JS, Hoftman N. Double lumen endobronchial tube intubation: lessons learned from anatomy. BMC Anesthesiol. 2024;24(1):150. doi:10.1186/s12871-024-02517-6
99. Ozaki M, Minami K, Sata T, Shigematsu A. Transdermal ketoprofen mitigates the severity of postoperative sore throat: [Le kétoprofène transdermique réduit le mal de gorge postopératoire]. Can J Anaesthesia. 2001;48(11):1080–1083. doi:10.1007/bf03020373
100. Passali D, Barat V, Cadevall O, et al. International Delphi-based consensus on the appropriate use and effect of Benzydamine hydrochloride in the treatment of sore throat. BMC Primary Care. 2022;23(1):296. doi:10.1186/s12875-022-01901-w
101. Chen C-Y, Kuo C-J, Lee Y-W, Lam F, Tam K-W. Le chlorhydrate de benzydamine pour les maux de gorge postopératoires: une méta-analyse d’études randomisées contrôlées. Canadian J Anesthesia. 2014;61(3):220–228. doi:10.1007/s12630-013-0080-y
102. Hung N-K, Wu C-T, Chan S-M, et al. Effect on postoperative sore throat of spraying the endotracheal tube cuff with benzydamine hydrochloride, 10% lidocaine, and 2% lidocaine. Anesthesia Analg. 2010;111(4):882–886. doi:10.1213/ANE.0b013e3181d4854e
103. Huang Y-S, Hung N-K, Lee M-S, et al. The effectiveness of benzydamine hydrochloride spraying on the endotracheal tube cuff or oral mucosa for postoperative sore throat. Anesthesia Analg. 2010;111(4):887–891. doi:10.1213/ANE.0b013e3181e6d82a
104. Agarwal A, Nath SS, Goswami D, Gupta D, Dhiraaj S, Singh PK. An evaluation of the efficacy of aspirin and benzydamine hydrochloride gargle for attenuating postoperative sore throat: a prospective, randomized, single-blind study. Anesthesia Analg. 2006;103(4):1001–1003. doi:10.1213/01.ane.0000231637.28427.00
105. Rahimi M, Makarem J. Effects of diclofenac epolamine patch on postoperative sore throat in parturients after cesarean delivery under endotracheal general anesthesia. Acta Anaesthesiol Taiwanica. 2009;47(1):17–21. doi:10.1016/s1875-4597(09)60015-1
106. Thang’a P, Kamya D, Mung’ayi V. Effects of intravenous diclofenac on postoperative sore throat in patients undergoing laparoscopic surgery at Aga Khan University Hospital, Nairobi: a prospective, randomized, double blind controlled trial. Afr Health Sci. 2014;13(4):999–1006. doi:10.4314/ahs.v13i4.20
107. Zhang W, Zhao G, Li L, Zhao P. Prophylactic Administration of Corticosteroids for Preventing Postoperative Complications Related to Tracheal Intubation: a Systematic Review and Meta-Analysis of 18 Randomized Controlled Trials. Clin Drug Invest. 2016;36(4):255–265. doi:10.1007/s40261-015-0369-4
108. Kuriyama A, Maeda H, Sun R, Aga M. Topical application of corticosteroids to tracheal tubes to prevent postoperative sore throat in adults undergoing tracheal intubation: a systematic review and meta-analysis. Anaesthesia. 2018;73(12):1546–1556. doi:10.1111/anae.14273
109. Hintong T, Chongvisal S, Pipanmekaporn T, Unchiti K. A Randomized Comparison of Effects of Budesonide Spray and K-Y Gel as an Endotracheal Tube Cuff Lubricant on Incidence of Postoperative Sore Throat. J Perianesthesia Nurs. 2023;38(4):585–589. doi:10.1016/j.jopan.2022.10.003
110. Sumathi PA, Shenoy T, Ambareesha M, Krishna HM. Controlled comparison between betamethasone gel and lidocaine jelly applied over tracheal tube to reduce postoperative sore throat, cough, and hoarseness of voice. Br J Anaesth. 2008;100(2):215–218. doi:10.1093/bja/aem341
111. Zhao X, Cao X, Li Q. Dexamethasone for the prevention of postoperative sore throat: a systematic review and meta-analysis. J Clinical Anesthesia. 2015;27(1):45–50. doi:10.1016/j.jclinane.2014.06.014
112. Thomas S, Beevi S. La dexaméthasone réduit la sévérité du mal de gorge postopératoire. Canadian J Anesthesia. 2007;54(11):897–901. doi:10.1007/bf03026793
113. Subedi A, Tripathi M, Pokharel K, Khatiwada S. Effect of Intravenous Lidocaine, Dexamethasone, and Their Combination on Postoperative Sore Throat: a Randomized Controlled Trial. Anesthesia Analg. 2019;129(1):220–225. doi:10.1213/ane.0000000000003842
114. Canbay O, Celebi N, Sahin A, Celiker V, Ozgen S, Aypar U. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth. 2008;100(4):490–493. doi:10.1093/bja/aen023
115. Park SY, Kim SH, Noh JI, et al. The effect of intravenous low dose ketamine for reducing postoperative sore throat. Korean J Anesthesiol. 2010;59(1):22–26. doi:10.4097/kjae.2010.59.1.22
116. Bhanwra A, Palta S, Saroa R, Saxena P, Bhanwra S, Jain A. Role of preoperative zinc, magnesium and budesonide gargles in Postoperative Sore Throat (POST) - a randomised control trial. BMC Anesthesiol. 2024;24(1):164. doi:10.1186/s12871-024-02534-5
117. Borazan H, Kececioglu A, Okesli S, Otelcioglu S. Oral magnesium lozenge reduces postoperative sore throat: a randomized, prospective, placebo-controlled study. Anesthesiology. 2012;117(3):512–518. doi:10.1097/ALN.0b013e3182639d5f
118. Soltani H-A, Aghadavoudi O. The effect of different lidocaine application methods on postoperative cough and sore throat. J Clinical Anesthesia. 2002;14(1):15–18. doi:10.1016/s0952-8180(01)00344-0
119. Navarro RM, Baughman VL. Lidocaine in the endotracheal tube cuff reduces postoperative sore throat. J Clinical Anesthesia. 1997;9(5):394–397. doi:10.1016/s0952-8180(97)00068-8
120. Tanaka Y, Nakayama T, Nishimori M, Tsujimura Y, Kawaguchi M, Sato Y. Lidocaine for preventing postoperative sore throat. Cochrane Database Syst Rev. 2015;2015(7):Cd004081. doi:10.1002/14651858.CD004081.pub3
121. Li H, Yue Y, Qu Y, Mu D. Lidocaine for postoperative sore throat: a meta-analysis of randomized controlled trials. Minerva Anestesiol. 2020;86(5):546–553. doi:10.23736/s0375-9393.20.14170-1
122. Yang SS, Wang -N-N, Postonogova T, et al. Intravenous lidocaine to prevent postoperative airway complications in adults: a systematic review and meta-analysis. Br J Anaesth. 2020;124(3):314–323. doi:10.1016/j.bja.2019.11.033
123. Maruyama K, Sakai H, Miyazawa H, et al. Laryngotracheal application of lidocaine spray increases the incidence of postoperative sore throat after total intravenous anesthesia. J Anesthesia. 2004;18(4):237–240. doi:10.1007/s00540-004-0264-2
124. Ishida K, Maruyama Y, Yoshiyama Y, et al. Alkalized lidocaine in a tapered cuff suppresses endotracheal tube-induced hemodynamic changes: a randomized controlled trial. J Anesthesia. 2023;37(5):726–733. doi:10.1007/s00540-023-03224-1
125. Hara K, Maruyama K. Effect of additives in lidocaine spray on postoperative sore throat, hoarseness and dysphagia after total intravenous anaesthesia. Acta anaesthesiologica Scandinavica. 2005;49(4):463–467. doi:10.1111/j.1399-6576.2005.00632.x
126. Zhipeng L, Meiyi H, Meirong W, et al. Ultrasound-guided internal branch of superior laryngeal nerve block on postoperative sore throat: a randomized controlled trial. PLoS One. 2020;15(11):e0241834. doi:10.1371/journal.pone.0241834
127. Zhou Y, Chen B, Xiong Y, Yu X. The Efficacy of Ultrasound-Guided Superior Laryngeal Nerve Block as an Adjuvant to General Anesthesia during Suspension Laryngoscopy Vocal Cord Polypectomy. Evid Complementary Alternative Medicine. 2022;2022:1594829. doi:10.1155/2022/1594829
128. Wang J, Chai B, Zhang Y, Zheng L, Geng P, Zhan L. Effect of postoperative ultrasound-guided internal superior laryngeal nerve block on sore throat after intubation of double-lumen bronchial tube: a randomized controlled double-blind trial. BMC Anesthesiol. 2022;22(1):276. doi:10.1186/s12871-022-01819-x
129. Chen Z, Zhang L, Lu G, et al. Effects of Dexmedetomidine as an Adjuvant in Preoperative Ultrasound-Guided Internal Branch of Superior Laryngeal Nerve Block on Postoperative Sore Throat and Hemodynamics in Patients With Double-Lumen Endotracheal Intubation: a Randomized Controlled Trial. Journal of Pain Research. 2025;18:229–241. doi:10.2147/jpr.S498538
130. Malta SM, Bilotta F, Nozari A. Is it Safe to Use Ultrasound-Guided Superior Laryngeal Nerve Block for the Prevention of Postoperative Sore Throat After Double Lumen Endotracheal Intubation? Anesthesia Analg. 2024;138(1):e1–e2. doi:10.1213/ane.0000000000006732
131. Liu Y, Ai D, Wang X. Efficacy of perioperative intravenous dexmedetomidine administration for the prevention of postoperative sore throat: a meta-analysis. J Int Med Res. 2021;49(5):3000605211017686. doi:10.1177/03000605211017686
132. Niu J, Hu R, Yang N, et al. Effect of intratracheal dexmedetomidine combined with ropivacaine on postoperative sore throat: a prospective randomised double-blinded controlled trial. BMC Anesthesiol. 2022;22(1):144. doi:10.1186/s12871-022-01694-6
133. Abedzadeh E, Modir H, Pazooki S, Barsari FZ, Almasi-Hashiani A. Comparison of adding magnesium sulfate, dexmedetomidine and ondansetron to lidocaine for gargling before laryngoscopy and endotracheal intubation to prevent sore throat: a randomized clinical trial. Med Gas Res. 2024;14(2):54–60. doi:10.4103/2045-9912.372664
134. Maruyama K, Yamada T, Hara K. Effect of clonidine premedication on postoperative sore throat and hoarseness after total intravenous anesthesia. J Anesthesia. 2006;20(4):327–330. doi:10.1007/s00540-006-0421-x
135. Ogata J, Minami K, Horishita T, et al. Gargling with sodium azulene sulfonate reduces the postoperative sore throat after intubation of the trachea. Anesthesia Analg. 2005;101(1):290–293. doi:10.1213/01.Ane.0000156565.60082.7c
136. Ebneshahidi A, Mohseni M. Strepsils® tablets reduce sore throat and hoarseness after tracheal intubation. Anesthesia Analg. 2010;111(4):892–894. doi:10.1213/ANE.0b013e3181d00c60
137. Zou S, Guo L, Xu C, et al. Effect of chewing gum of different weights before surgery on sore throat after total thyroidectomy: a randomized controlled trial. World J Surg. 2024;48(1):130–137. doi:10.1002/wjs.12025
138. Sakai H, Misawa M. Effect of sodium azulene sulfonate on capsaicin-induced pharyngitis in rats. Basic Clin Physiol Pharmacol. 2005;96(1):54–59. doi:10.1111/j.1742-7843.2005.pto960108.x
139. Wang T, Wang Q, Zhou H, Huang S. Effects of Preoperative Gum Chewing on Sore Throat After General Anesthesia With a Supraglottic Airway Device: a Randomized Controlled Trial. Anesthesia Analg. 2020;131(6):1864–1871. doi:10.1213/ane.0000000000004664
140. Ruetzler K, Fleck M, Nabecker S, et al. A randomized, double-blind comparison of licorice versus sugar-water gargle for prevention of postoperative sore throat and postextubation coughing. Anesthesia Analg. 2013;117(3):614–621. doi:10.1213/ANE.0b013e318299a650
141. Singh NP, Makkar JK, Cappellani RB, Sinha A, Lakshminarasimhachar A, Singh PM. Efficacité des agents topiques pour la prévention des maux de gorge postopératoires après une intubation avec tube endotrachéal simple lumière: une méta-analyse bayésienne en réseau. Canadian J Anesthesia. 2020;67(11):1624–1642. doi:10.1007/s12630-020-01792-4
142. Kuriyama A, Maeda H. Topical application of licorice for prevention of postoperative sore throat in adults: a systematic review and meta-analysis. J Clinical Anesthesia. 2019;54:25–32. doi:10.1016/j.jclinane.2018.10.025
143. Agarwal A, Gupta D, Yadav G, Goyal P, Singh PK, Singh U. An evaluation of the efficacy of licorice gargle for attenuating postoperative sore throat: a prospective, randomized, single-blind study. Anesthesia Analg. 2009;109(1):77–81. doi:10.1213/ane.0b013e3181a6ad47
144. Liu S, Wang Z, Su Y, et al. A neuroanatomical basis for electroacupuncture to drive the vagal–adrenal axis. Nature. 2021;598(7882):7882):641–645. doi:10.1038/s41586-021-04001-4
145. Torres-Rosas R, Yehia G, Peña G, et al. Dopamine mediates vagal modulation of the immune system by electroacupuncture. Nat Med. 2014;20(3):291–295. doi:10.1038/nm.3479
146. Jau P-Y, Chang S-C. The effectiveness of acupuncture point stimulation for the prevention of postoperative sore throat: a meta-analysis. Medicine. 2022;101(28):e29653. doi:10.1097/md.0000000000029653
147. Esmaeili S, Alizadeh R, Shoar S, Naderan M, Shoar N. Acupuncture in preventing postoperative anaesthesia-related sore throat: a comparison with no acupuncture. Acupuncture Med. 2013;31(3):272–275. doi:10.1136/acupmed-2012-010249
148. Park HS, Kim KS, Min HK, Kim DW. Prevention of postoperative sore throat using capsicum plaster applied at the Korean hand acupuncture point. Anaesthesia. 2004;59(7):647–651. doi:10.1111/j.1365-2044.2004.03739.x
149. Fliegenschmidt J, Hulde N, Preising MG, et al. Artificial intelligence predicts delirium following cardiac surgery: a case study. J Clinical Anesthesia. 2021;75:110473. doi:10.1016/j.jclinane.2021.110473
150. Xue B, Li D, Lu C, et al. Use of Machine Learning to Develop and Evaluate Models Using Preoperative and Intraoperative Data to Identify Risks of Postoperative Complications. JAMA Netw Open. 2021;4(3):e212240. doi:10.1001/jamanetworkopen.2021.2240
151. Harland T, Hadanny A, Pilitsis JG. Machine Learning and Pain Outcomes. Neurosurgery Clinics North America. 2022;33(3):351–358. doi:10.1016/j.nec.2022.02.012
152. Rashidi P, Edwards DA, Tighe PJ. Primer on machine learning: utilization of large data set analyses to individualize pain management. Curr Opin Anaesthesiol. 2019;32(5):653–660. doi:10.1097/aco.0000000000000779
153. Nagireddi JN, Vyas AK, Sanapati MR, Soin A, Manchikanti L. The Analysis of Pain Research through the Lens of Artificial Intelligence and Machine Learning. Pain Physician. 2022;25(2):E211–e243.
154. Dawes TR, Eden-Green B, Rosten C, et al. Objectively measuring pain using facial expression: is the technology finally ready? Pain Management. 2018;8(2):105–113. doi:10.2217/pmt-2017-0049
155. Hassan T, Seus D, Wollenberg J, et al. Automatic Detection of Pain from Facial Expressions: a Survey. IEEE Transact Pattern Analysis Machine Intelligence. 2021;43(6):1815–1831. doi:10.1109/tpami.2019.2958341
156. Zhou Q, Liu X, Yun H, et al. Leveraging artificial intelligence to identify high-risk patients for postoperative sore throat: an observational study. Biomolecules Biomed. 2024;24(3):593–605. doi:10.17305/bb.2023.9519
157. Chen J, Abbod M, Shieh J-S. Pain and Stress Detection Using Wearable Sensors and Devices—A Review. Sensors. 2021;21(4):1030. doi:10.3390/s21041030
158. Stachler RJ, Francis DO, Schwartz SR, et al. Clinical Practice Guideline: hoarseness (Dysphonia) (Update). Otolaryngology. 2018;158(1_suppl):S1–S42. doi:10.1177/0194599817751030
159. Reiter R, Hoffmann TK, Pickhard A, Brosch S. Hoarseness-causes and treatments. Deutsches Arzteblatt International. 2015;112(19):329–337. doi:10.3238/arztebl.2015.0329
160. Jones MW, Catling S, Evans E, Green DH, Green JR. Hoarseness after tracheal intubation. Anaesthesia. 1992;47(3):213–216. doi:10.1111/j.1365-2044.1992.tb02121.x
161. Yamanaka H, Hayashi Y, Watanabe Y, Uematu H, Mashimo T. Prolonged hoarseness and arytenoid cartilage dislocation after tracheal intubation. Br J Anaesth. 2009;103(3):452–455. doi:10.1093/bja/aep169
162. Brodsky MB, Akst LM, Jedlanek E, et al. Laryngeal Injury and Upper Airway Symptoms After Endotracheal Intubation During Surgery: a Systematic Review and Meta-analysis. Anesthesia Analg. 2021;132(4):1023–1032. doi:10.1213/ane.0000000000005276
163. Jaensson M, Gupta A, Nilsson UG. Gender differences in risk factors for airway symptoms following tracheal intubation. Acta anaesthesiologica Scandinavica. 2012;56(10):1306–1313. doi:10.1111/j.1399-6576.2012.02771.x
164. Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology. 2003;98(5):1049–1056. doi:10.1097/00000542-200305000-00005
165. Lautenbacher S, Peters JH, Heesen M, Scheel J, Kunz M. Age changes in pain perception: a systematic-review and meta-analysis of age effects on pain and tolerance thresholds. Neurosci Biobehav Rev. 2017;75:104–113. doi:10.1016/j.neubiorev.2017.01.039
166. Di Cicco M, Kantar A, Masini B, Nuzzi G, Ragazzo V, Peroni D. Structural and functional development in airways throughout childhood: children are not small adults. Pediatric Pulmonol. 2021;56(1):240–251. doi:10.1002/ppul.25169
167. Pohunek P. Development, structure and function of the upper airways. Paediatric Respirat Reviews. 2004;5(1):2–8. doi:10.1016/j.prrv.2003.09.002
168. Levett DZH, Grimmett C. Psychological factors, prehabilitation and surgical outcomes: evidence and future directions. Anaesthesia. 2019;74(S1):36–42. doi:10.1111/anae.14507
169. Ten Noever de Brauw GV, Aalders MB, Kerkhoffs G, Zuiderbaan HA, Keijser LCM, Benner JL. The mind matters: psychological factors influence subjective outcomes following unicompartmental knee arthroplasty—A prospective study. Knee Surg Sports Traumato Arthroscopy. 2025;33(1):239–251. doi:10.1002/ksa.12275
170. Wasem S, Lazarus M, Hain J, et al. Comparison of the Airtraq and the Macintosh laryngoscope for double-lumen tube intubation: a randomised clinical trial. Eur J Anaesthesiol. 2013;30(4):180–186. doi:10.1097/EJA.0b013e32835fe574
171. Turkstra TP, Cusano F, Fridfinnson JA, Batohi P, Rachinsky M. Early Endotracheal Tube Insertion with the GlideScope: a Randomized Controlled Trial. Anesthesia Analg. 2016;122(3):753–757. doi:10.1213/ane.0000000000001147
172. Bouvet L, Stoian A, Jacquot-Laperrière S, Allaouchiche B, Chassard D, Boselli E. Lésions laryngées et conditions d’intubation avec ou sans relaxation musculaire: une étude d’équivalence. Canadian J Anesthesia. 2008;55(10):674–684. doi:10.1007/bf03017743
173. Chia -Y-Y, Lee S-W, Liu K. Propofol causes less postoperative pharyngeal morbidity than thiopental after the use of a laryngeal mask airway. Anesthesia Analg. 2008;106(1):123–126. doi:10.1213/01.ane.0000297292.84620.2c
174. Teoh WH, Shah MK, Sia AT. Randomised comparison of Pentax AirwayScope and Glidescope for tracheal intubation in patients with normal airway anatomy. Anaesthesia. 2009;64(10):1125–1129. doi:10.1111/j.1365-2044.2009.06032.x
175. Tanaka Y, Nakayama T, Nishimori M, Sato Y, Furuya H. Lidocaine for preventing postoperative sore throat. Cochrane Database Syst Rev. 2009;2009(3):Cd004081. doi:10.1002/14651858.CD004081.pub2
176. Andersen LH, Rovsing L, Olsen KS. GlideScope videolaryngoscope vs. Macintosh direct laryngoscope for intubation of morbidly obese patients: a randomized trial. Acta anaesthesiologica Scandinavica. 2011;55(9):1090–1097. doi:10.1111/j.1399-6576.2011.02498.x
177. Turkstra TP, Smitheram AK, Alabdulhadi O, Youssef H, Jones PM. La sonde trachéale Flex-Tip™ ne réduit pas les maux de gorge postopératoires: une étude randomisée contrôlée. Canadian J Anesthesia. 2011;58(12):1090–1096. doi:10.1007/s12630-011-9592-5
178. D’Aragon F, Beaudet N, Gagnon V, Martin R, Sansoucy Y. Effets de la lidocaïne vaporisée et de la lidocaïne alcalinisée dans le ballonnet sur la survenue de toux au moment de l’extubation: une étude randomisée contrôlée à double insu. Canadian J Anesthesia. 2013;60(4):370–376. doi:10.1007/s12630-013-9896-8
179. Lam F, Lin YC, Tsai HC, Chen TL, Tam KW, Chen CY. Effect of Intracuff Lidocaine on Postoperative Sore Throat and the Emergence Phenomenon: a Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS One. 2015;10(8):e0136184. doi:10.1371/journal.pone.0136184
180. Yang HL, Liu FC, Tsai SC, Tsay PK, Lin HT, Liu HE. Ketorolac Tromethamine Spray Prevents Postendotracheal-Intubation-Induced Sore Throat after General Anesthesia. Biomed Res Int. 2016;2016:4582439. doi:10.1155/2016/4582439
181. Lee J, Lee YC, Son JD, Lee JY, Kim HC. The effect of lidocaine jelly on a taper-shaped cuff of an endotracheal tube on the postoperative sore throat: a prospective randomized study: a CONSORT compliant article. Medicine. 2017;96(37):e8094. doi:10.1097/md.0000000000008094
182. Lee J, Park HP, Jeong MH, Kim HC. Combined intraoperative paracetamol and preoperative dexamethasone reduces postoperative sore throat: a prospective randomized study. J Anesthesia. 2017;31(6):869–877. doi:10.1007/s00540-017-2411-6
183. Park JH, Lee YC, Lee J, Kim H, Kim HC. The influence of high-dose intraoperative remifentanil on postoperative sore throat: a prospective randomized study: a CONSORT compliant article. Medicine. 2018;97(50):e13510. doi:10.1097/md.0000000000013510
184. Fang P, Zong Z, Lu Y, Han X, Liu X. Effect of topical ropivacaine on the response to endotracheal tube during emergence from general anesthesia: a prospective randomized double-blind controlled study. BMC Anesthesiol. 2018;18(1):134. doi:10.1186/s12871-018-0601-x
185. Liao AH, Yeoh SR, Lin YC, Lam F, Chen TL, Chen CY. Lidocaine lubricants for intubation-related complications: a systematic review and meta-analysis. Canad J Anaesthes. 2019;66(10):1221–1239. doi:10.1007/s12630-019-01408-6
186. Farhang B, Grondin L. The Effect of Zinc Lozenge on Postoperative Sore Throat: a Prospective Randomized, Double-Blinded, Placebo-Controlled Study. Anesthesia Analg. 2018;126(1):78–83. doi:10.1213/ane.0000000000002494
187. Yhim HB, Yoon SH, Jang YE, et al. Effects of benzydamine hydrochloride on postoperative sore throat after extubation in children: a randomized controlled trial. BMC Anesthesiol. 2020;20(1):77. doi:10.1186/s12871-020-00995-y
188. Oxenham O, Pairaudeau C, Moody T, Mendonca C. Standard and flexible tip bougie for tracheal intubation using a non-channelled hyperangulated videolaryngoscope: a randomised comparison. Anaesthesia. 2022;77(12):1368–1375. doi:10.1111/anae.15854
189. Fu S, Miao M, Bian J, Fu Y, Zhang J, Sun M. Preoperative Ketamine Gargle for Prevention of Postoperative Sore Throat After Tracheal Intubation in Adults: a Meta-Analysis. Pain Res Manag. 2025;2025(1):7622696. doi:10.1155/prm/7622696
190. Senol Celik S, Chalkias A, Sariköse S, et al. Effect of peri-intubation non-pharmacological interventions on postoperative laryngeal symptoms: a systematic review with meta-analysis and meta-regression. Intensive Critical Care Nursing. 2024;84:103728. doi:10.1016/j.iccn.2024.103728
191. Chen GC, Lo KL, Wu ZF, et al. Comparison of the incidence and severity of postoperative sore throat and subglottic airway injury with cylindrical versus tapered cuff endotracheal tubes in women undergoing surgery for breast cancer: a randomized controlled trial. BMC Anesthesiol. 2025;25(1):181. doi:10.1186/s12871-025-03040-y
192. Guan X, Tian Y, Yang J, et al. The application of reinforced endotracheal tubes with pressure indicators in preventing postoperative airway-related complications in neurosurgical patients: a randomized controlled study. BMC Anesthesiol. 2025;25(1):90. doi:10.1186/s12871-025-02967
193. Fu CH, Sung CH Effects of GlideScope, pentax airway scope, and macintosh blade on the incidence of postoperative sore throat: a cohort study of 9,881 patients. BMC Anesthesiol. 2024;24(1):409. doi:10.1186/s12871-024-02798-x
194. Shan T, Zhang H, Zhou X, et al. Effect of different head position during tracheal intubation on postoperative sore throat: a randomized clinical trial. Annals of Medicine. 2025;57(1). doi:10.1080/07853890.2025.2464943):2464943.
195. Shui W, Hu W, Ma W, et al. The effects of video double-lumen tubes on intubation complications in patients undergoing thoracic surgery: a randomised controlled study. Eur J Anaesthesiol. 2024;41(4):305–313. doi:10.1097/EJA.0000000000001959
196. Tao D, Zhang G, Zheng X, et al. Feasibility study of intubation in lateral position using viva-sight double-lumen tube combined with video laryngoscope in patients undergoing pulmonary lobectomy. Asian J Surg. 2024;47(1):373–379. doi:10.1016/j.asjsur.2023.08.199
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


