Back to Journals » Drug Design, Development and Therapy » Volume 19
Potential Application of Origanum majorana Stabilized Silver Nanoparticles for Coating of Urinary Catheter
Authors Al Rugaie O , Abdulbaqi MR, Danial AW, Mohammed HA , Alsharidah M, Tawfeek HM , Abdellatif AA
Received 14 December 2024
Accepted for publication 27 March 2025
Published 15 April 2025 Volume 2025:19 Pages 2941—2957
DOI https://doi.org/10.2147/DDDT.S512320
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Solomon Tadesse Zeleke
Osamah Al Rugaie,1 Mustafa R Abdulbaqi,2 Amal W Danial,3 Hamdoon A Mohammed,4 Mansour Alsharidah,5 Hesham M Tawfeek,6 Ahmed AH Abdellatif7
1Department of Biology and Immunology, College of Medicine, Qassim University, Buraydah, Saudi Arabia; 2Department of Pharmaceutics, College of Pharmacy, Al-Naji University, Al-Naji, Iraq; 3Botany and Microbiology Department, Faculty of Science, Assiut University, Assiut, Egypt; 4Department of Medicinal Chemistry and Pharmacognosy, College of Pharmacy, Qassim University, Al Qassim, 51452, Saudi Arabia; 5Department of Physiology, College of Medicine, Qassim University, Buraydah, 51452, Saudi Arabia; 6Department of Industrial Pharmacy, Faculty of Pharmacy, Assiut University, Assiut, 71526, Egypt; 7Department of Pharmaceutics, College of Pharmacy, Qassim University, Buraydah, 51452, Saudi Arabia
Correspondence: Ahmed AH Abdellatif, Email [email protected]
Introduction: Urinary tract infections related to catheters are one of the most common urinary infections and can affect patient outcomes. Hence, coating urinary catheters is an important issue against several resistant bacterial pathogens that can form a resistant biofilm. This study examined the antibacterial and antibiofilm properties of the coated catheter with green silver nanoparticles (AgNPs) made from Origanum majorana.
Methods: Aloe Vera, Ocimum basilicum, Matricaria chamomilla, Foeniculum vulgare, Glycyrrhiza glabra, Origanum majorana, Urtica urens, Salvia Rosmarinus, and Salvia officinalis hydro-alcoholic extracts were prepared and tested for their antibacterial activities utilizing the agar well diffusion technique. Furthermore, O. majorana extract was tested against biofilm formation using a microtiter plate assay. UPLC-ESI-Q-TOF was used for the profiling and tentative identification of biological compounds in the O. majorana extract. O. majorana was used to prepare AgNPs-MARJ, which were characterized for their size, charge, and shape. Further, AgNPs-MARJ were used to coat two types of urinary catheters. The coated catheters were tested for their resistance to bacterial biofilm formation and compared with non-coated catheters.
Results and Discussion: Initial antimicrobial screening tests showed that O. majorana extracts presented a significant (p< 0.05; ANOVA/Tukey) antibacterial activity against the studied species of bacteria compared to the other plant extracts. O. majorana extract showed MIC value of 35.0 mg/mL for E. coli, Pseudomonas aeruginosa and K. pneumoniae and displayed the highest antibiofilm activity at 100 mg/mL. LC-MS analysis tentatively identified the presence of quinic acid and flavonoid-based constituents like apigenin which contribute to the antibiofilm activity. AgNPs-MARJ were efficiently prepared with a size and charge of 111.5 nm and − 19.66 mV, respectively. The coated urinary catheters showed a significant (p< 0.05) decrease in Pseudomonas aeruginosa biofilm formation compared to control non-coated catheters.
Conclusion: AgNPs-MARJ offer promising prospects for addressing biofilm-related challenges in urinary tract-related catheter infections.
Keywords: Origanum majorana, silver nanoparticles, urinary catheters, antibiofilm activity, plant extract
Introduction
Hospitals address incontinence and urine retention via catheters. Urinary tract infections can result from catheter surface bacterial colonization. Common catheter-associated bacteria include E. coli, K. pneumoniae, and E. faecalis. These organisms can form catheter biofilms, complicating therapy and increasing morbidity and healthcare costs.1 The produced biofilm provides a strong resistance to any delivered antibiotics. In this context, strenuous efforts have been directed to minimize the accumulation of bacteria on the surface of urinary catheters especially those used for long term therapy. The use of antibacterial coating agents such as silver sulfadiazine or antibiotics to prevent bacterial growth and catheter infections is a traditional method for bacterial catheter colonization. These conventional methods have several limitations,such as they help germs to grow and become antimicrobial-resistant.1,2 In addition to other materials like antimicrobial peptides used for retardation of bacterial growth, they demonstrated potential toxicity, lower coating properties and high initial cost.3,4 Nanomaterials play a crucial role in controlling nosocomial infections via effective coating and releasing of components which can disrupt the formed resistant biofilm. Furthermore, they can be efficiently engineered to form an efficient coat, decrease bacterial adhesion to the catheter surface as well as be biocompatible. Different nanomaterials have been investigated for their efficiency for catheter coating and bacterial colonization growth retardation such as silver nanoparticles, gold nanoparticles, copper nanoparticles, and zinc-doped copper oxide nanoparticles.3–6
Among the metal nanoparticles, silver nanoparticles (AgNPs) showed a potent broad spectrum of antibacterial and anti-fungal properties, in addition, AgNPs can resist bacterial colonization in several ways.4,5 It was also demonstrated that AgNPs could be used as efficient coating nanomaterials for different surfaces like catheters, titanium implants, textiles, and water membranes.5–7
Natural products offer a wide range of biological molecules which have been shown to have many biological properties as well as being easily obtained via simple extraction procedures. The extracted materials could be used as alternatives to the chemically synthesized antibacterial agents. Origanum majorana offers antibiofilm activity on medical devices, such as catheters and implants. Coating O. majorana-based extract into the design of medical devices could possibly diminish biofilm formation and diminish the probability of device-related infections.8–10 Among various essential oils that may be useful as antibacterial agents is the O. majorana oil which belongs to the Lamiaceae family.11,12 O. marjorana is characterized also by the presence of a variety of volatile secondary metabolites, especially carvacrol which represents 81.5% of O. majorana essential oils. Carvacrol is traditionally used to treat different conditions like asthma, rheumatism, dizziness, gastrointestinal disorders, and migraine.13,14 The antimicrobial action of O. majorana essential oil relies on the hydrophobic property of the oil which facilitates easy penetration into the bacterial cell membrane. Further, it can also penetrate the cell interior to interact with intracellular sites vital for bacterial activities.15–17 Other researchers explained their role in inhibition of glucosyl transferase enzyme activity, which is responsible for bacteria adhesion to its sites.18
It is well known that plant extracts obtained from different sources are powerful materials for green synthesis of metallic NPs, especially AgNPs.19,20 It has been reported that AgNPs were prepared within higher stability and optimum particle size without the use of chemically reducing agents.21,22 Not only an environment friendly method but, also, it is straightforward and cheap. The prepared AgNPs obtained from plant sources have many physical, chemical, and biological purposes like antibacterial, anti-viral, anti-inflammatory, anti-platelet, and anti-fungal.22,23 Our previous study has shown the coating of urinary catheters using AgNPs stabilized with certain cellulosic polymers.24 Even though the study revealed promising results, however, the use of polymers in terms of industry might be expensive and not economic. Combining the antibiofilm and antibacterial activities of O. majorana extract and AgNPs could provide a synergistic effect to retard and control bacterial colonization and biofilm formation in urinary catheters.
The present study aimed to evaluate the antimicrobial and antibiofilm activity of AgNPs coated with O. majorana, AgNPs-MARJ, prepared utilizing a green approach using O. majorana leaf extract. This was followed by coating of two types of urinary Foley catheters and investigating the effect of coating on the retardation of biofilm formation caused by P. aeruginosa. Briefly, different plants materials were extracted and tested for their antibacterial effect against different Gram-positive and Gram-negative bacterial strains using the agar well diffusion method to find the MIC in vitro of every plant extract. Further, the antibiofilm activity was conducted using microtiter plate assay for the best extract showing the highest antimicrobial activity. LC-MS was used to identify some of the important components of O. majorana. AgNPs were prepared using O. majorana extract and characterized for their size, charge, and morphology. The prepared AgNPs-MARJ were used to coat two types of urinary Foley catheters. The resistance of coated urinary catheters to bacterial biofilm formation was investigated and compared to non-coated catheters.
Materials and Methods
Plant Materials and Preparation of the Plant Extracts
The plant materials were obtained for the local market from Buraydah, Qassim, Saudi Arabia, and authenticated by Dr. Hamdoon Mohammed, the pharmacognosist at the Faculty of Pharmacy, Qassim University, Saudi Arabia. A voucher sample of the plants was stored at the same department under the numbers OPP-136 to OPP-144, for the Aloe vera, Ocimum basilicum, Matricaria chamomilla, Foeniculum vulgare, Glycyrrhiza glabra, Origanum majorana, Urtica urens, Salvia rosmarinus, and Salvia officinalis. The plants are widely available in local herbalist shops and are not classified as endangered or extinct. Therefore, no institutional or additional approvals were required to conduct this research in accordance with local regulations. Plant materials were ground into small pieces before being subjected to extraction with hydroalcoholic solution (30% water in pure ethanol). The dried plant materials (100 g) were macerated with the hydroalcoholic solvent overnight under continuous agitation to facilitate the plant constituent extraction. The extracts were then filtrated using cellulose Whatman 7.0 cm2 filter paper and dried under reduced pressure and stored in the freezer for further phytochemical analysis and biological applications.25
Tested Microorganisms
The following microbial cultures were used in this study: Bacillus subtilis, Escherichia coli, Staphylococcus aureus, Serratia marcescens, Klebsiella pneumoniae and Pseudomonas aeruginosa. All these microorganisms are involved in human and animal diseases or frequently reported from contaminated soil, water, and food substances. All isolates were isolated from different sources in human bodies (urine, sputum, or stool) at Assiut University Hospital, Assiut, Egypt. These isolates were preliminary identified using Gram stain, morphological and physiological characters, and by using specific media.
Inoculum Preparation
For inoculum preparation, bacteria cultures were cultured in nutrient agar medium over night at 37 ±2 °C, then diluted with sterilized nutrient broth to obtain 108 CFU/mL using 0.5 McFarland standard (BioMerieux, Paris, France).
Screening for the Antimicrobial Potential Activity
The agar well-diffusion method was used to screen the antibacterial activity of all hydro-alcoholic extracts of medicinal plants used. Nutrient agar plates prepared according to the manufacturer’s instruction were autoclaved and dispensed into sterile 10 cm2 Petri dish. Further, 0.1 mL of diluted inoculum (105 CFU/mL) of test organism was spread on nutrient agar plates using sterilized glass spreader. Sterile cork borer was used to make 6-mm wells on nutrient agar plates (4 wells/plate) and filled with 50 μL of plant extract. DMSO (Sigma-Aldrich, St. Louis, MO, USA) was used as a negative control and chloramphenicol (20 μg/mL) (Sigma-Aldrich, St. Louis, MO, USA) was used as a positive control. DMSO was the negative control because it is often used as a solvent to dissolve test compounds that are not water-soluble and it has minimal or no antimicrobial activity at low concentrations, making it a suitable negative control. This ensures that any observed effects in the experiment are due to the test compound itself and not the solvent. Chloramphenicol (20 μg/mL) is the positive control because it is a broad-spectrum antibiotic that inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit and it is used as a positive control to confirm that the bacterial strain is susceptible to antibiotic treatment. This ensures the experimental setup is functional and capable of detecting inhibitory effects when present.
Then, the plates were incubated aerobically at 37 °C, overnight. All tests were performed in triplicate.26 The antimicrobial screening was determined by measuring the size of clear zone of inhibition across the diameter of the well (mm). Zone of inhibition measuring more than 7 mm implies that the organism is susceptible to the tested plant extract.27,28 The extracts that showed antimicrobial activity were further tested to determine the minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) for each of the tested organisms.
Determination of MIC and MBC
The double-fold micro-dilution method29 was used according to the Clinical and Laboratory Standards Institute. Samples of 100 µL of plant extract were prepared starting with the original concentration used in the screening experiment, with various concentrations of two-fold serial dilution of each of the most effective extracts. One milliter of the standard inoculum (5 × 105 bacterial cells/mL) of each of isolate was dispersed with a 20 mL nutrient agar medium (NA) plate, and after solidification, 50 μL of each concentration were put in the agar well (0.5 cm2 diameter). The plates were incubated at 30 °C for 24–48 h, the minimum inhibitory concentration (MIC) was expressed as the lowest concentration that inhibits the visible growth of each strain.30 To evaluate the MBC, the concentrations that showed complete inhibition of the microbial growth were streaked onto agar plates and incubated under the same conditions as previously mentioned. The complete inhibition of microbial growth on the agar surface at the lowest concentrations was defined as the MBC.31
Quantitative Assessment of Anti-Biofilm Formation by the Microtiter Plate Method (MTP)
The antibiofilm activity of the crude extract of organum against biofilm produced by S. mutans and B. subtilis, S. aureus, K. pneumoniae, P. aeruginosa, E. coli and S. marcescens was assessed according to the method described by Yimgang et al32 using a 96-well microtiter plate with some modifications. A single colony from the nutrient agar (NA) medium overnight bacterial culture was incubated at 37 °C for 24 h, then 1 mL was transferred to 100 mL poly beta-hydroxybutyric acid (BHIB) supplemented with 4% sucrose and 100 µL of single strength nutrient broth were distributed in the wells of 96 microtiter plate. Aliquots of 100 µL of each extract (100 mg/mL) were transferred to the first well of each row, and then two-fold serial dilutions was carried out up to the tenth columns from which 100 µL aliquots were discarded. The last 2 columns (11th and 12th) represent 2 controls for biofilm formation level of untreated bacterial isolates. The plate was then incubated at 37 °C for 24 h. After incubation, the content of each well was carefully discarded and washed three times with 200 μL of PBS (pH 7.3) to remove the non-adherent bacterial cells, then the plate was left to air dry at room temperature. Crystal violet 2% (200 μL) was used to stain the formed bacterial biofilm for 15 min at room temperature, and the plates were then washed three times with distilled water to remove the excess stain. Next, 200 μL of methanol was added to each well for 30 min to resolubilize the adhered biofilm. The optical density (OD) of stained biofilm at λmax of 600 nm was measured using the microtiter plate reader (BioTek EPOCH, Highland Park, Winooski, VT, USA).31,33
Qualitative Detection of Anti-Biofilm Formation by the Test Tube Method (TM)
Overnight bacterial cultures were prepared using BHIB and then 1 mL transferred to 100 mL BHIB supplemented with 4% sucrose and 1 mL of these broths were distributed in clean sterilized test tubes. Aliquots of 100 µL of each extract (100 mg/mL) were transferred to the first test tube and then two-fold serial dilutions was carried out up to tube number 6 from which 100 µL aliquots were discarded. The last tube represents control for biofilm formation level of untreated bacterial isolates. The tubes were then incubated at 37 °C for 24 h. After incubation, tubes were washed gently three times with sterile saline, and then dried at room temperature. Three milliters of crystal violet solution (0.1% w/v) were added to each tube, then the tubes were left at room temperature for 15 min, followed by removing of crystal violet solution and three times gentle washing with deionized water. Biofilm formation was detected by the appearance of visible violet color on the walls and the bottoms of the test tubes.34,35
LC-MS/MS Analysis of the Plant Extract
LC-MS analysis was carried out on a Shimadzu Exion-LC (Shimadzu, Kyoto, Japan) connected to a TurboIon-Spray SCIEX-X500R-QTOF (SCIEX, Framingham, MA, USA). Analytical grade solvents were used for dissolving the extract and to prepare the mobile phase systems. In addition, the plant extract was dissolved in DMSO in a concentration of 0.5 mg/mL, 5 min centrifuged (5,000 rpm), passed through a Millipore 0.2 m filter paper, and placed in a vial for autosampler. The injection volume was adjusted to 3.0 µL. The analysis was carried out at the capillary voltage of −4,000 V, nebulizer gas of 2.0 bar, nitrogen flow of 8 L/min, and dry temperature of 200 °C. The mass sensitivity was adjusted at 50,000 FSR, the mass precision was 1 ppm, and the TOF recurrence was adjusted at a rate up to 20 kHz. Chromatographic separation with the gradient elution method was applied using an RP-C18 column (2.1 mm I.D., 100 mm length, and 3 µm particle size) from GL-Science (Japan). The parameters of the separation were adjusted as follows: flow rate of 0.35 mL/min for 30 min of running. Formic acid (0.1%) and pure acetonitrile were used as the mobile phases A and B, respectively. The gradient system was composed of 0.1% formic acid in water (A) and acetonitrile (B); for the first 4 min, the system was composed of 96% of system (A) and 4% of system (B). The ratio of acetonitrile (B) was increased to 6% in 10 min, 7% in 12 min, 8% in 15 min, 13% in 18 min, 15% in 23 min, 20% in 25 min, and 28% in 27 min, and maintained until 30 min. The annotation processes were based on several analysis outcomes, including the molecular weight of the compounds, their fragmentation pattern compared to the literature, the suggestions of the machine library, and the reported constituents of O. majorana.
Preparation of Silver Nanoparticles Coated with O. majorana
Silver nitrate 17 mg was added to a 100 mL of extract and left on a hot plate (WiseStir, MSH-30A, Korea) with stirring for about 30 min. Further, with the color change to deep red, the solution is set aside to cool and filtered to remove the formed AgNP big particles. Finally, the produced AgNPs were centrifuged (HERMLE Z 200 A Centrifuge, Germany) at 7000 rpm for 10 min and stored in the fridge for further investigations.36,37 The produced AgNPs-MARJ were characterized for size and zeta potentials using a Malvern zetasizer nano (Malvern, UK).38,39 Furthermore, the shape of the produced AgNPs-MARJ was identified using transmission electron microscope (TEM) (JEM-1230; Joel Japan, Tokyo, Japan).23,24,40 Stability of the prepared NPs was checked after storage of AgNPs-MARJ at room temperature for one month, followed by measuring their size and charge and comparing them with the initial values.
Coating of Urinary Catheter with AgNPs-MARJ
Two different urinary catheters were used in this study, the first is a latex Foley balloon catheter model, silicone coated, and the second type is a silicone Foley balloon catheter model, all silicone.
Coating of Urinary Catheters
Catheters were sliced into small pieces of approximately 2 cm2 length and soaked in the AgNPs-MARJ solution containing 15 µg/mL AgNPs with stirring overnight as mentioned previously.24,41 Further, they are washed twice with distilled water and dried at ambient conditions of laboratory for 24 h and stored in closed container for further investigation.
Antibiofilm Efficacy for Coated Urinary Catheters
A pathogenic bacterial species, P. aeruginosa was investigated in this study. Generally, coated and non-coated (negative control) catheters were incubated in the investigated bacterial suspension overnight. Then, bacterial adhesion to the surface of the catheters was determined by staining 2 cm2 of the catheter with methyl violet and measuring the intensity of the biofilm calorimetrically as previously described.
Statistical Analysis
The data were compiled in MS Office Excel 365. Statistical analysis was done using SPSS version 21 software package (SPSS Statistics for Windows, Version 28.0; SPSS Inc., Chicago, IL, USA). ANOVA, and Student ‘t’ tests were performed. A p-value less than <0.05 was statistically significant.
Results
Results from the aforementioned studies and experiments are presented in the following sections. The obtained results are novel and matching the aims of the study. Briefly, the results begin through the evaluation of the antibacterial activity of the obtained plants extracts and their pronounced antibacterial and antibiofilm effect especially with O. majorana. These are followed by detailed chemical analysis of the O. majorana extract using LC-MS and green synthesis of AgNPs and their characterizations. Finally, coating of urinary catheters with the prepared AgNPs and their antibiofilm activity toward one of the most prevalent and harmful bacterial species responsible for urinary tract infections.
Evaluation of Antimicrobial Activity
Results from the agar well diffusion method showed that only O. majorana leaves' hydro-alcoholic extract had strong antibacterial activity against the studied species of bacteria compared to the other investigated extracts as shown in Table 1.42
The initial screening test showed that O. majorana extract showed a significant (p<0.05; ANOVA/Tukey) antibacterial activity against the studied species of bacteria compared to the other investigated extracts as shown in Table 1.
 |
Table 1 Sensitivity of the Investigated Bacterial Species to Different Types of the Investigated Extracts Shown as Inhibition Zone (mm) |
Susceptibility of Bacterial Strains to O. majorana Extract
In this experiment, the zone of inhibition was measured, and the data are presented in Table 2. The results showed that the O. majorana leaf extract was efficiently suppressing the growth of the studied strains. The crude extract recorded the highest zone of inhibition against Gram-positive strains (S. aureus) and Gram-negative strains (K. pneumoniae and S. marcescens). In the case of B. subtilis, the extracts showed minimal to moderate inhibitory effects, with some extracts leading to notable inhibition zones. E. coli exhibited similar patterns, with certain extracts demonstrating higher inhibitory activity. P. aeruginosa, S. marcescens, S. aureus, and K. pneumoniae also displayed varying degrees of sensitivity to the extracts, highlighting the diversity of antibacterial effects across different bacterial species.43,44
 |
Table 2 Minimal Inhibitory Concentration (MIC) of O. marjorana Leaves Hydro-Alcoholic Extract (mg/mL) Against Tested Organisms |
Determination of MIC and MBC
The tested antimicrobial substances were further evaluated for its MIC and MBC using the microdilution assay, as shown in Tables 2 and 3. The MIC value was found to be 35.0 mg/mL for the studied organisms with zones of inhibition of 13±0.4, 15±0.4 and 20.0±0.4 mm for S. aureus, K. pneumoniae and S. marcescens; respectively using O. majorana extract. Zones of bacterial growth inhibition for E. coli and P. aeruginosa was found to be 10.0±0.8 and 10.0±0.5 mm, respectively as shown in Table 2. MIC is generally regarded as the most basic laboratory measurement of the activity of an antimicrobial agent against an organism. MBC values were in the range of 35–17.5 mg/mL for O. majorana extract as depicted in Table 3. Results of MIC and MBC measurements showed strong antibacterial activity of O. majorana extracts against the tested Gram-positive and Gram-negative bacteria, with largest inhibition zones and the lowest MIC values (35.0 and 17.5 mg/mL) against both B. subtilis and S. aureus, a Gram-positive bacterium, and S. marcescens, P. aeruginosa and K. pneumoniae, a Gram-negative bacterium with largest inhibition zones and the lowest MIC values (35.0 mg/mL), and mild antibacterial activity was detected against both of E. coli, Gram-negative bacteria, with MIC value of (35.0 mg/mL). Least activity was exhibited against the rest of tested microorganisms, with the smallest inhibition zones and MIC value of (35.0 mg/mL). In agreement with our results, Ramos et al, reported that the methanolic extract of O. majorana was active against S. aureus, E. faecalis, and E. coli.45 In contrast to our results, a study reported that O. majorana showed a strong growth inhibition effect against E. coli, S. enteritidis, S. aureus, and B. cereus.46
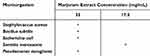 |
Table 3 Minimum Bacteria Concentration (MBC) of O. marjorana Leaves Hydro-Alcoholic Extract (mg/mL) Against Tested Organisms by the Agar Well Diffusion Method |
Effect of O. majorana Extract on Biofilm Formation
The effect of O. majorana extract on the biofilm formation of bacterial isolates was qualitatively and quantitatively tested. The presence of violet visible film lining the walls and bottoms of the Wassermann tubes indicates biofilm production (Figure 1). The quantification of anti-biofilm activity was performed using a microtiter plate assay. The data were expressed in terms of the average OD values at 600 nm. In this experiment, bacterial biofilms were exposed to multiple concentrations (35, 17.5, 8.75, 4.375, 2.18, 1.095 mg/mL) of the O. majorana extract for 48 h. O. majorana extract showed the highest anti-biofilm activity at a concentration of 100 mg/mL (Figure 2). The results of the tube method (TM) revealed that the extract has high anti-biofilm activity at different concentrations.
 |
Figure 1 The 96-well microtiter plate assay depicted the O. marjorana hydro-alcoholic extract on the biofilm formation of K. pneumoniae and P. aeruginosa. |
Phytochemical Profiling of O. marjorana Extract
The LC-MS-based constituent profiling of O. marjorana was conducted to identify the plant constituents from the cultivated species of the plant in Egypt and to understand the possible interactions and mechanisms underlying the antimicrobial activity of the plant. The LC-MS analysis of the plant extract leads to the tentative identification of 31 compounds among tens of the peaks demonstrated in the LC chromatogram. The tentative nomination of the compounds has been carried out using the mass fragmentation patterns and the library identification based on the high-resolution mass of these compounds. All the identified compounds were of a polyphenolic nature, either phenolic acids or flavonoids. Among the compounds listed in Table 4 sixteen compounds were identified as phenolic acids, and fifteen compounds were found to be flavonoids in nature. In addition, most of the identified flavonoids were in glycosidal forms, and part of their identification was attributed to the presence of their aglycon mass fragments in the MS/MS chromatogram. For instance, the presence of mass fragment m/z 269 in the chromatogram of apiin (RT 10.26, m/z 563 [M–H]–) was assigned to the aglycon apigenin after detaching the apiosyl-glucoside mass unit. In a similar way, apigenin-O-glucuronide, luteolin-O-glycoside, kaempferol-O-sambubioside, kaempferitrin, kaempferol-O-glucuronide, rutin, and luteolin-O-rutinoside were identified based on the presence of the mass fragments of apigenin (m/z 270), luteolin (m/z 285), kaempferol (m/z 284), and quercetin (m/z 301) in their MS/MS chromatogram. The overall phytochemical analysis of the plant indicated its enrichment with polyphenolic compounds, especially the phenolic acids and flavonoid glycosides.
 |
Table 4 LC-MS Analysis of O. marjorana Hydro-Alcoholic Extract |
The AgNPs-MARJ were formed with a faint brown color (Figure 3A). The size and PDI of the prepared AgNPs-MARJ was recorded using DLS as 111.5±12.6 and 0.43±0.02, respectively. In addition, they have a zeta potential value of −19.66±3.22 (Figure 3B). TEM image showed a round to oval nanoparticles with a size ranging from 50–150 nm (Figure 3C). Upon storage of AgNPs-MARJ at room temperature, it was found that there is no significant difference was found between the measured initial size and charge and that obtained after one-month storage at room temperature.
Two types of catheters have been investigated in this study. Type I (Figure 3D), surface coated, silicone coated latex Foley catheter, and type II (Figure 3E), fully coated silicone Foley catheter. The two types of catheters were subjected to coating with AgNPs-MARJ (Figure 3F). The catheters showed formation of an AgNPs-MARJ layer on the surfaces of type I (Figure 3G) and type II (Figure 3H).
The effect of AgNPs-MARJ coating and resistance to biofilm formation into the investigated unrainy catheters was tested using the tube assay method. It was clear that the silicone coated Foley catheter showed a lower percentage of bacterial biofilm formation compared to the latex type Foley catheter. AgNPs-MARJ coated catheters showed 36.6±2.5 and 43.6±3.5% biofilm formation for latex Foley catheter and silicone coated Foley catheter, respectively as shown in (Figure 4). Both the investigated catheters showed a significant (p<0.05) decrease in biofilm formation compared to control non-coated catheters. Furthermore, the investigated catheters did not show any significant difference (p>0.05) in percentage of P. aeruginosa biofilm formation (Figure 4).
Discussion
Plant materials contain numerous valuable components which show different medical and chemical activities. Herein in this study, different plant materials were extracted using the maceration technique. Such a method is simple and the cheapest method for extraction. In addition, it is widely used for extraction of leaves derived plant components, but it takes a relatively long time.60
O. majorana extract has been widely studied for its strong antibacterial properties, often showing significant activity compared to other investigated herbal extracts. O. majorana extract contains various bioactive compounds, including monoterpenes, phenolic acids, and flavonoids, which contribute to its pronounced antibacterial activity. Studies have shown that O. majorana extract is effective against a range of bacteria, including both Gram-positive and Gram-negative strains. It has been investigated that the hydro-alcoholic extract of O. majorana stem exhibited strong antibacterial activity against food spoilage bacteria such as B. cereus.61 The antibacterial activity of O. majorana extract is attributed to its ability to disrupt bacterial cell membranes, inhibit enzyme activity, and interfere with bacterial DNA synthesis.61,62 Due to its strong antibacterial properties, O. majorana extract is used as a natural preservative in food products to prevent spoilage and extend their shelf life. Its effectiveness against biofilms and resistant pathogenic bacteria makes it also valuable component in medical and dental treatments.61,63,64
LC-MS analysis revealed the presence of several phenolic acids and flavonoids, along with their corresponding glycosides, which contributed to the plant antimicrobial and antibiofilm activities. In addition, the presence of the listed compounds in Table 4 might be also reflected the potential antioxidant health benefits of the plant and its extract. Compounds like flavonoids, tannins, and essential oils from plants exhibit anti-biofilm properties by interfering with quorum sensing, disrupting the extracellular polymeric substance (EPS), and inhibiting bacterial adhesion to surface like catheter walls. In addition, the presence of these compounds, which are known for their metal-reducing ability,48,65 in the plant extract might be underlying one of their potential mechanisms to inhibit microbial growth by inhibiting the metal-based microbial enzymes, the mechanism which is known for several antimicrobial agents such as lactoferrin.66 The flavonoids have been also reported to inhibit the topoisomerase enzymes including DNA gyrase, the responsible enzymes for the DNA replication in the prokaryotes, which might also highlight the plant antimicrobial activity owing to its flavonoid contents.58 Polyphenols have been also reported to inhibit the microbial growth via preventing the microbial cell envelope synthesis by the inhibition of bacterial-type II fatty acid synthase.67
In that context, quinic acid (RT 2.48), has been reported for its antibiofilm activity against P. aeruginosa biofilms and enhances the antibiofilm activity of some antibiotics such as ciprofloxacin.68 The antimicrobial effect of quinic acid is related to the compound ability to modulate ribosome functions and aminoacyl-tRNA synthesis, alters glycerophospholipid and fatty acid levels, and messes with the oxidative phosphorylation pathway. This may help to explain why quinic acid interferes with membrane fluidity.69 Similarly, ferulic acid, dihydroxy ferulic acid, coumaric acid, arbutin, and chlorogenic acid have exerted inhibition to different microbial biofilms.70
The LC-MS analysis also revealed the presence of several antimicrobial and antibiofilm flavonoid-based constituents in O. marjorana hydro-alcoholic extract (Table 4). These flavonoids includes apigenin derivatives such as apiin, vicenin-2, and apigenin-O-glucuronide, which according to literature induced substantial antimicrobial and antibiofilm activities, specifically against S. aureus and E. coli microbial pathogens.71 Moreover, apigenin have been reported to affect the adherence and biofilm formation through changing the surface characteristics of S. aureus mutants pathogen.72 In addition to the presence of a mixture of luteolin, kaempferol, and quercetin derivatives, which usually detected in the several anti-inactive and anti-biofilm plants.73–75 The overall LC-MS profiling results supported the present anti-microbial and antibiofilm findings of O. marjorana extract and its beneficial effect on synthesis of AgNPs and further coating of urinary catheters to fight bacterial colonization.
In the case of AgNPs-MARJ, O. marjorana was adsorbed onto the surface of AgNPs via the carbonyl groups of the contained compounds. The obtained negative charge of the prepared AgNPs-MARJ proved the effective O. marjorana coating layer around the produced AgNPs. Hence, better particle stability and this could eventually provide good adherence to catheter wall. In general, the measured particle size by TEM was smaller than that obtained by DLS, as TEM only showed the particle’s metal core. At the same time, DLS assesses the hydrodynamic particle size.24 Furthermore, the Marjoram coating effect on the surface of NPs reduced particle diffusivity and increased particle size as assessed by DLS.76
One of the most prevalent causes of urinary tract infections is the use of the urinary catheters especially those used for the long term. The catheter-associated urinary tract infections can range from few bacterial growths to high microbial colonization during patient hospitalization. In addition, growth of highly resistant bacterial species like E. coli, K. pneumoniae and P. aeruginosa can form resistant biofilm.77,78 The significance of catheter-associated urinary tract infections is presented in the future patient’s outcome. From these outcomes is an overuse of antibiotics, long hospitalization time, higher healthcare expenditures, and the overuse of antibiotics, as well as higher mortality rates.79–81 In this study, K. pneumoniae was chosen as it often contributes significantly to catheter-associated urinary tract infections through cross-transmission.82 It was also found in many studies that K. pneumoniae is second most prevalent pathogen following E. coli among Enterobacteriaceae in urinary tract infections.82,83 Colonization of K. pneumoniae produces high levels of extended-spectrum β-lactamase (ESBL), which causes resistance to most antibiotics. Furthermore, highly resistant species of K. pneumoniae showed a significant resistance to carbapenems.84 P. aeruginosa was also chosen as another important Gram-negative anaerobic bacteria which contributes to nosocomial urinary tract infections and is reported to be a significant biofilm producer.78
Coating of urinary catheters with antimicrobial agents derived from biological sources could be beneficial compared with conventional chemical compounds like antibiotics. Hence, they are considered safer, and they have also different components with many biological activities which could act synergistically to retard bacterial colonization and biofilm formation. It was reported by Mohanta et al that AgNPs synthesized from plant extracts exhibited significantly greater antibacterial activity that that prepared from other sources like bacteria, fungi, algae, etc. The authors also pointed out that the plant derived AgNPs could be more superior than the chemically synthesized one in terms of self-coating and stabilization as well as exhibiting their own antibacterial activity.85 Goda et al have demonstrated the effect of AgNPs prepared using Pomegranate rind extract on the retardation of biofilm colonization in urinary catheters. AgNPs coated catheters significantly inhibited the colonization of catheters by certain antibiotic-resistant clinical Gram-positive and Gram-negative bacterial strains. However, the coating solution contains chloroform which is an organic solvent, and its residue remaining after coating is still an issue.86 Lethongkam et al, similarly, studied the effect of AgNPs produced from Eucalyptus camaldulensis leaves on the prevention of biofilm formation in urinary catheters. Even though they have obtained promising results, they utilized a complex method that depends on coating and reduction of silver nitrate solution as well as the long time of the used process which persist for 5 days.87 Divya et al have shown the promising effect of AgNPs for bacterial growth and biofilm retardation in urinary catheters. The results exhibit that the coating of synthesized AgNPs on catheters effectively inhibited the growth and biofilm formation of urinary tract infection causing pathogens. However, the processes of bacterial isolation, screening, and identification is harsh, expensive, and time consuming.88 Our last investigation in this field has demonstrated the effect of AgNPs stabilized with certain polymeric materials to retard biofilm formation. Data obtained in this study delineated the useful use of AgNPs coated with ethyl cellulose and PVP as potential antibacterial and anti-biofilm catheter coating agents to prevent the development of urinary tract infections caused by E. coli. However, in this study, AgNPs were prepared via chemical method, reduction of silver nitrate, and focused on E. coli bacterial strains.24
Fully coated silicone catheter showed a lower percentage of biofilm formation compared to silicone coated latex Foley catheter that could be possibly due to the inner and outer coating of catheter with silicone which potentially decreases the adhesion of bacteria into the inner wall of catheter.
The anti-biofilm activity observed after coating the urinary catheters could be attributed to the dual effect of both AgNPs as well as the O. marjorana extract components which acts synergistically to retard biofilm formation. As depicted from LC-MS, O. marjorana extract contained valuable antibacterial and anti-biofilm compounds like quinic acid and flavonoids such as apigenin which all contribute to the anti-biofilm activity and good adherence to catheter wall. It has been found that AgNPs are considered one most excellent tool for avoiding catheter-associated microbial infections due to their pronounced antibacterial activities.89 AgNPs released silver ions which can target certain cell component like proteins and unsaturated fatty acids, thus followed by inactivation of certain enzymes and proteins associated with the bacterial cell wall.90,91 After that, the bacterial membrane becomes permeable with enhanced fluidity character followed by overall disruption of cell wall and altering membrane integrity.92 This is followed by easy internalization of AgNPs, they could interact with bacterial DNA causing disturbance and accumulation into the cytoplasm of damaged bacteria, leading to leakage of cellular components and bacterial death.93 It has been also stated that the inhibition of biofilm formation by AgNPs could be possibly attributed to the inhibitory effect on what is called exopolysaccharides, a prerequisite for biofilm formation.94 Park et al95 showed that the biosorption could be responsible for the inhibition of biofilm formation against P. aeruginosa induced by AgNPs. Similar results were also found by Mohanta et al,96 who demonstrated that AgNPs prepared using different phytoconstituents present in some Indian plants have a significant inhibitory effect on biofilm formed from either P. aeruginosa or E. coli at low concentrations. The authors also delineated that the complex biofilm signaling mechanism could also be associated with cell survival. It cannot be also neglected the role of O. marjorana as it has a pronounced antibacterial and anti-biofilm activities as shown in our study and previously reported.97 So, the combined synergistic effect could be responsible also for the observed anti-biofilm activity. Similarly, Mohanta et al,96 who demonstrated the antibacterial properties and antibiofilm activity of AgNPs prepared using leaf extracts of Semecarpus anacardium, Glochidion lanceolarium, and Bridelia retusa. From our perspective, the obtained findings correlate with the results and research objectives. In addition, they are relevant to the study objectives. Beginning from the plant extraction, screening for antibacterial action and biofilm study, green synthesis of AgNPs-MARJ and characterization, coating of urinary catheters, and finally their anti-biofilm activity after catheter coating. The significant reduction in the biofilm formation with the investigated two types of urinary catheters produced with P. aeruginosa which contribute significantly to catheter-associated urinary tract infections is considered a good and promising target of our study. In addition, a one-step coating process, based on a simple, straightforward technique and economic, saving time and effort, can give promising results on biofilm retardation. However, further study should be conducted to minimize and determine the optimum coating layer for more reduction in biofilm formation and with other bacterial strains.
Conclusion
O. marjorana hydro-alcoholic extract was efficiently prepared and revealed that it contains a more valuable compounds which contributed to its antibacterial and anti-biofilm activities as obtained from LC-MS analysis compared to the other investigated extracts. Antibacterial AgNPs from plant sources offer a natural alternative to synthetic antimicrobials. The included compounds in the extract showed a promising role as an efficient reducing and coating agents to prepare stabilized AgNPs-MARJ with reasonable size and charge. Coating of urinary catheters was performed simply and straight forward with the prepared AgNPs-MARJ. Such coating offers a significant reduction in biofilm formation caused by P. aeruginosa which contribute significantly to catheter-associated urinary tract infections. The synergistic effect of both AgNPs and O. marjorana extract formed around the NPs contributed to the antibiofilm activity against the tested bacteria. It could be concluded that AgNPs-MARJ is a promising tool for urinary catheter coating to control the related unrainy tract nosocomial infections. Hence, they could improve urinary tract interventions, patient outcomes, and catheter-related infections by combining nanotechnology and plant-based resources to overcome standard antibacterial approaches.
Technology Challenges Issues
Despite the synthesis of efficient stabilized AgNPs-MARJ for urinary catheter coatings, however, there are certain technological challenges which should be considered. Some of these challenges relay on the optimization of coating process factors which contribute to formation of efficient coating layer on the catheter wall on both sides. As well as technology transfer from small scale to large scale production. In addition to, utilizing an in vivo model to study the effect of AgNPs-MARJ under a urine flowing condition.
Future Prospects
Nanoparticles and natural extracts can disclose novel antibacterial agents and promote novel formulations. Future perspectives include widening the angle to study the effect of these nanomaterials in different medical disorders like wounds as well as extending the market and potential impact.
Funding
The authors extend their appreciation to the Deputyship for Research & Innovation, Ministry of Education, Saudi Arabia, for funding this research work through project number QU-IF-1-4-1. The authors also thank Qassim University for the technical support.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Swidan NS, Hashem YA, Elkhatib WF, Yassien MA. Antibiofilm activity of green synthesized silver nanoparticles against biofilm associated enterococcal urinary pathogens. Sci Rep. 2022;12(1):3869. doi:10.1038/s41598-022-07831-y
2. Francis AL, Namasivayam SKR, Priyanka S. Antimicrobial activity of herbal biomass derived metabolites fabricated wound dressing material against microbial strains causing skin infection. S Afr J Bot. 2024;175:142–157. doi:10.1016/j.sajb.2024.09.058
3. Al-Subaiyel A, Abdellatif AAH. Eco-friendly synthesis of silver nanoparticles by Trigonella foenum-graecum: formulations, characterizations, and application in wound healing. Drug Dev Ind Pharm. 2024;50(11):927–937. doi:10.1080/03639045.2024.2431934
4. Kim JS, Kuk E, Yu KN, et al. Antimicrobial effects of silver nanoparticles. Nanomed Nanotechnol, Biol Med. 2007;3(1):95–101. doi:10.1016/j.nano.2006.12.001
5. Yassin MA, Elkhooly TA, Elsherbiny SM, Reicha FM, Shokeir AA. Facile coating of urinary catheter with bio–inspired antibacterial coating. Heliyon. 2019;5(12):e02986. doi:10.1016/j.heliyon.2019.e02986
6. Elshaer S, Shaaban MI. Antibiofilm activity of biosynthesized silver and copper nanoparticles using Streptomyces S29. AMB Express. 2023;13(1):139. doi:10.1186/s13568-023-01647-3
7. Kerekes EB, Vidacs A, Tako M, et al. Anti-biofilm effect of selected essential oils and main components on mono- and polymicrobic bacterial cultures. Microorganisms. 2019;7(9):345. doi:10.3390/microorganisms7090345
8. Kerekes EB, Deak E, Tako M, et al. Anti-biofilm forming and anti-quorum sensing activity of selected essential oils and their main components on food-related micro-organisms. J Appl Microbiol. 2013;115(4):933–942. doi:10.1111/jam.12289
9. Kaskatepe B, Aslan Erdem S, Ozturk S, et al. Antifungal and anti-virulent activity of Origanum majorana L. essential oil on Candida albicans and in vivo toxicity in the Galleria mellonella larval model. Molecules. 2022;27(3). doi:10.3390/molecules27030663
10. Mouhoub A, Guendouz A, El Alaoui-Talibi Z, Ibnsouda Koraichi S, Delattre C, El Modafar C. Elaboration and general evaluation of chitosan-based films containing terpene alcohols-rich essential oils. World J Microbiol Biotechnol. 2023;39(6):146. doi:10.1007/s11274-023-03597-1
11. Busatta C, Vidal R, Popiolski A, et al. Application of Origanum majorana L. essential oil as an antimicrobial agent in sausage. Food Microbiol. 2008;25(1):207–211. doi:10.1016/j.fm.2007.07.003
12. Mohamed HM, Mansour HA. Incorporating essential oils of marjoram and rosemary in the formulation of beef patties manufactured with mechanically deboned poultry meat to improve the lipid stability and sensory attributes. LWT-Food Sci Technol. 2012;45(1):79–87. doi:10.1016/j.lwt.2011.07.031
13. Abdel-Massih R, Abraham A. Extracts of Rosmarinus officinalis, Rheum rhaponticum, and Origanum majorana exhibit significant anti-staphylococcal activity. Inter JPharma Sci Res. 2014;5(3):819.
14. Dorman HD, Deans SG. Chemical composition, antimicrobial and in vitro antioxidant properties of monarda citriodora var. citriodora, myristica fragrans, Origanum vulgare ssp. hirtum, pelargonium sp. and thymus zygis oils. JEssential Oil Res. 2004;16(2):145–150. doi:10.1080/10412905.2004.9698679
15. Mathlouthi N, Bouzaienne T, Oueslati I, et al. Use of rosemary, oregano, and a commercial blend of essential oils in broiler chickens: in vitro antimicrobial activities and effects on growth performance. J Anim Sci. 2012;90(3):813–823. doi:10.2527/jas.2010-3646
16. Cristani M, D’Arrigo M, Mandalari G, et al. Interaction of four monoterpenes contained in essential oils with model membranes: implications for their antibacterial activity. J Agricul Food Chem. 2007;55(15):6300–6308. doi:10.1021/jf070094x
17. Abdelhai MF, Shabaan RH, Kamal NM, Elemary EA, Abd-Elhalim BT, Hassan EA. Copper nanoparticles biosynthesis by Stevia rebaudiana extract: biocompatibility and antimicrobial application. AMB Express. 2024;14(1):59. doi:10.1186/s13568-024-01707-2
18. Tsai P-J, Tsai T-H, Ho S-C. In vitro inhibitory effects of rosemary extracts on growth and glucosyltransferase activity of Streptococcus sobrinus. Food Chem. 2007;105(1):311–316. doi:10.1016/j.foodchem.2006.11.051
19. Abdellatif AAH, Mostafa MAH, Khojah HMJ, et al. Utilizing Ziziphus spina-christi for eco-friendly synthesis of silver nanoparticles: antimicrobial activity and promising application in wound healing. Nanotechnol Rev. 2024;13(1). doi:10.1515/ntrev-2024-0112
20. Ali E, Abu-Hussien SH, Hesham E, et al. Compatibility and antimicrobial activity of silver nanoparticles synthesized using Lycopersicon esculentum peels. AMB Express. 2024;14(1):120. doi:10.1186/s13568-024-01774-5
21. Abdellatif AAH, Abdelfattah A, Younis MA, Aldalaan SM, Tawfeek HM. Chitosan-capped silver nanoparticles with potent and selective intrinsic activity against the breast cancer cells. Nanotechnol Rev. 2023;12(1). doi:10.1515/ntrev-2022-0546
22. Beyene HD, Werkneh AA, Bezabh HK, Ambaye TG. Synthesis paradigm and applications of silver nanoparticles (AgNPs), a review. Sustain Mater Technol. 2017;13:18–23. doi:10.1016/j.susmat.2017.08.001
23. Abdellatif AAH, Alturki HNH, Tawfeek HM. Different cellulosic polymers for synthesizing silver nanoparticles with antioxidant and antibacterial activities. Sci Rep. 2021;11(1):84. doi:10.1038/s41598-020-79834-6
24. Rugaie OA, Abdellatif AAH, El-Mokhtar MA, et al. Retardation of bacterial biofilm formation by coating urinary catheters with metal nanoparticle-stabilized polymers. Microorganisms. 2022;10(7). doi:10.3390/microorganisms10071297
25. Mohammed HA, Said R, Abbas MM, et al. Phytochemical, biological, and computational investigations of Ephedra alata decne. Growing in salinity conditions of Arabian Peninsula. Sci Rep. 2024;14(1):21987. doi:10.1038/s41598-024-69607-w
26. NBH-B E, Abdelkefi M, Aissa RB, Chaabouni MM. Antibacterial screening of Origanum majorana L. oil from Tunisia. J Essent Oil Res. 2001;13(4):295–297. doi:10.1080/10412905.2001.9699698
27. Walker JF, Santos P, Schmidt CA, Bittencourt T, Guimarães AG. Antimicrobial activity of Marjoram (Origanum Majorana) essential oil against the multidrug‐resistant salmonella enterica serovar schwarzengrund inoculated in vegetables from organic farming. J Food Safe. 2016;36(4):489–496. doi:10.1111/jfs.12266
28. Koffi-Nevry R, Kouassi KC, Nanga ZY, Koussémon M, Loukou GY. Antibacterial activity of two bell pepper extracts: capsicum annuum L. and Capsicum frutescens. Inter J Food Proper. 2012;15(5):961–971. doi:10.1080/10942912.2010.509896
29. Clinical, Institute LS. Performance Standards for Antimicrobial Susceptibility Testing. Wayne, PA: Clinical and Laboratory Standards Institute; 2020.
30. Rodriguez-Tudela J, Barchiesi F, Bille J, et al. Method for the determination of minimum inhibitory concentration (MIC) by broth dilution of fermentative yeasts. Clin Microbiol Infect. 2003;9(8):i–viii. doi:10.1046/j.1469-0691.2003.00789.x
31. Farouk SM, Abu-Hussien SH, Abd-Elhalim BT, et al. Biosynthesis and characterization of silver nanoparticles from Punica granatum (pomegranate) peel waste and its application to inhibit foodborne pathogens. Sci Rep. 2023;13(1):19469. doi:10.1038/s41598-023-46355-x
32. Yimgang LV, Kouipou Toghueo RM, Mbekou IMK, Dize D, Boyom FF, Nevárez-Moorillón GV. Crude metabolites from endophytic fungi inhabiting Cameroonian Annona muricata inhibit the causative agents of urinary tract infections. PLoS One. 2022;17(5):e0267246. doi:10.1371/journal.pone.0267246
33. Abu-Hussien SH, Hemdan B, Abd-Elhalim BT, et al. Larvicidal potential, antimicrobial properties and molecular docking analysis of Egyptian mint (Mentha rotundifolia) against Culex pipiens L. (Diptera: Culicidae) and midgut-borne Staphylococcus aureus. Sci Rep. 2024;14(1):1697. doi:10.1038/s41598-024-51634-2
34. Al-Mudallal NH, Al-Jumaily EF, Muhimen NA, Al-Shaibany AA-W. Isolation and identification of mutan’s streptococci bacteria from human dental plaque samples. Al-Nahrain J Sci. 2008;11(3):98–105.
35. Gomaa HH, Amin DY, Ahmed AR, Ismail NA, El Dougdoug KA, Abd-Elhalim BT. Antimicrobial, antibiofilm, and antiviral investigations using Egyptian Phoenix dactylifera L. pits extract. AMB Express. 2024;14(1):44. doi:10.1186/s13568-024-01695-3
36. Abdellatif AAH, Mohammed HA, Abdulla MH, et al. Green synthesized silver nanoparticles using the plant-based reducing agent Matricaria chamomilla induce cell death in colorectal cancer cells. Eur Rev Med Pharmacol Sci. 2023;27(20):10112–10125. doi:10.26355/eurrev_202310_34191
37. Sadan M, Naem M, Tawfeek HM, et al. Can silver nanoparticles stabilized by Fenugreek (Trigonella foenm-graecum) improve tibial bone defects repair in rabbits? A preliminary study. Open Vet J. 2024;14(5):1281–1293. doi:10.5455/OVJ.2024.v14.i5.23
38. Abdellatif AA, Zayed G, El-Bakry A, Zaky A, Saleem IY, Tawfeek HM. Novel gold nanoparticles coated with somatostatin as a potential delivery system for targeting somatostatin receptors. Drug Dev Ind Pharm. 2016;42(11):1782–1791. doi:10.3109/03639045.2016.1173052
39. Abdellatif AAH, Abou-Taleb HA, Abd El Ghany AA, Lutz I, Bouazzaoui A. Targeting of somatostatin receptors expressed in blood cells using quantum dots coated with vapreotide. Saudi Pharm J. 2018;26(8):1162–1169. doi:10.1016/j.jsps.2018.07.004
40. Abdellatif AAH, Alsharidah M, Al Rugaie O, Tawfeek HM, Tolba NS. Silver nanoparticle-coated ethyl cellulose inhibits tumor necrosis factor-alpha of breast cancer cells. Drug Des Devel Ther. 2021;15:2035–2046. doi:10.2147/DDDT.S310760
41. Lellouche J, Friedman A, Lellouche JP, Gedanken A, Banin E. Improved antibacterial and antibiofilm activity of magnesium fluoride nanoparticles obtained by water-based ultrasound chemistry. Nanomedicine. 2012;8(5):702–711. doi:10.1016/j.nano.2011.09.002
42. Gurib-Fakim A. Medicinal plants: traditions of yesterday and drugs of tomorrow. Mol Aspects Med. 2006;27(1):1–93. doi:10.1016/j.mam.2005.07.008
43. Hwang HJ, Li DD, Lee J, Kang MK, Moon HR, Lee JH. Compounds that have an anti-biofilm effect against common bacteria at very low concentrations and their antibiotic combination effect. Antibiotics. 2023;12(5). doi:10.3390/antibiotics12050853
44. Manso T, Lores M, de Miguel T. Antimicrobial activity of polyphenols and natural polyphenolic extracts on clinical isolates. Antibiotics. 2021;11(1). doi:10.3390/antibiotics11010046
45. Ramos GE, Lopez MH, Flores AM, Figueroa GT, De Leon FG. Effect of lixiviated sediments affected with treated water on Selenastrum capricornutum, Printz and Origanum vulgare L. J Environ Sci Health a Tox Hazard Subst Environ Eng. 2010;45(1):23–31. doi:10.1080/10934520903388616
46. Valdivieso-Ugarte M, Gomez-Llorente C, Plaza-Diaz J, Gil A. Antimicrobial, antioxidant, and immunomodulatory properties of essential oils: a systematic review. Nutrients. 2019;11(11):2786. doi:10.3390/nu11112786
47. Onder A, Izgi MN, Cinar AS, Zengin G, Yilmaz MA. The characterization of phenolic compounds via LC-ESI-MS/MS, antioxidant, enzyme inhibitory activities of Salvia absconditiflora, salvia sclarea, and salvia palaestina: a comparative analysis. S Afr J Bot. 2022;150:313–322. doi:10.1016/j.sajb.2022.07.030
48. Elshibani FA, Mohammed HA, Abouzied AS, et al. Phytochemical and biological activity profiles of Thymbra linearifolia: an exclusively native species of Libyan green mountains. Arab J Chem. 2023;16(6):104775.
49. Zengin G, Uysal A, Diuzheva A, et al. Characterization of phytochemical components of Ferula halophila extracts using HPLC-MS/MS and their pharmacological potentials: a multi-functional insight. J Pharma Biomed Anal. 2018;160:374–382.
50. Fang N, Yu S, Prior RL. LC/MS/MS characterization of phenolic constituents in dried plums. J Agric Food Chem. 2002;50(12):3579–3585. doi:10.1021/jf0201327
51. Martins J, Batista T, Pinto G, Canhoto J. Seasonal variation of phenolic compounds in strawberry tree (Arbutus unedo L.) leaves and inhibitory potential on phytophthora cinnamomi. Trees. 2021;35(5):1571–1586.
52. Salerno R, Casale F, Calandruccio C, Procopio A. Characterization of flavonoids in citrus bergamia (Bergamot) polyphenolic fraction by liquid chromatography–high resolution mass spectrometry (LC/HRMS). Pharma Nutri. 2016;4:S1–S7.
53. Carazzone C, Mascherpa D, Gazzani G, Papetti A. Identification of phenolic constituents in red chicory salads (Cichorium intybus) by high-performance liquid chromatography with diode array detection and electrospray ionisation tandem mass spectrometry. Food Chem. 2013;138(2–3):1062–1071. doi:10.1016/j.foodchem.2012.11.060
54. Mohammed HA, Abdulkarim AK, Alamami AD, Elshibani FA. Phytochemical constituents and biological activities of Jasonia glutinosa L.: the first report for the plant growing in North Africa. J Chem. 2022;2022(1):4510176. doi:10.1155/2022/4510176
55. Taamalli A, Arraez-Roman D, Abaza L, et al. LC-MS-based metabolite profiling of methanolic extracts from the medicinal and aromatic species Mentha pulegium and Origanum majorana. Phytochem Anal. 2015;26(5):320–330. doi:10.1002/pca.2566
56. Liu G, Ma J, Chen Y, et al. Investigation of flavonoid profile of Scutellaria bacalensis Georgi by high performance liquid chromatography with diode array detection and electrospray ion trap mass spectrometry. J Chromatogr A. 2009;1216(23):4809–4814. doi:10.1016/j.chroma.2009.04.021
57. Elshibani FA, Alamami AD, Mohammed HA, et al. A multidisciplinary approach to the antioxidant and hepatoprotective activities of arbutus pavarii pampan fruit; in vitro and in vivo biological evaluations, and in silico investigations. J Enzyme Inhib Med Chem. 2024;39(1):2293639. doi:10.1080/14756366.2023.2293639
58. Sun Y, Li H, Hu J, et al. Qualitative and quantitative analysis of phenolics in tetrastigma hemsleyanum and their antioxidant and antiproliferative activities. J Agricul Food Chem. 2013;61(44):10507–10515. doi:10.1021/jf4037547
59. Ibrahim RM, El-Halawany AM, Saleh DO, Embe N, El-Shabrawy AE-RO, El-Hawary SS. HPLC-DAD-MS/MS profiling of phenolics from securigera securidaca flowers and its anti-hyperglycemic and anti-hyperlipidemic activities. Revista Brasileira de Farmacognosia. 2015;25(2):134–141. doi:10.1016/j.bjp.2015.02.008
60. Tambun R, Alexander V, Ginting Y. Performance comparison of maceration method, soxhletation method, and microwave-assisted extraction in extracting active compounds from soursop leaves (Annona muricata): a review. IOP Conf Series: Mater Scie Engine. 2021;1122(1). doi:10.1088/1757-899x/1122/1/012095
61. Bhardwaj K, Dubey W. Exploring potential of hydro-alcoholic extract of stem of marjoram as natural preservative against food spoilage bacteria Bacillus cereus and Bacillus megaterium in homemade Mango jam. Vegetos. 2021;34(4):898–908. doi:10.1007/s42535-021-00243-9
62. Bouaouina S, Aouf A, Touati A, et al. Effect of nanoencapsulation on the antimicrobial and antibiofilm activities of Algerian Origanum glandulosum desf. against multidrug-resistant clinical isolates. Nanomaterials. 2022;12(15):2630. doi:10.3390/nano12152630
63. Wijesundara NM, Rupasinghe HPV. Essential oils from Origanum vulgare and salvia officinalis exhibit antibacterial and anti-biofilm activities against streptococcus pyogenes. Microb Pathog. 2018;117:118–127. doi:10.1016/j.micpath.2018.02.026
64. Mokhtari H, Eskandarinezhad M, Barhaghi MS, et al. Comparative antibacterial effects of ginger and marjoram extract versus conventional irrigants on mature Enterococcus faecalis biofilms: an in vitro study. J Clin Exp Dent. 2023;15(4):e304–e310. doi:10.4317/jced.60081
65. Mohammed HA, Sulaiman GM, Albukhaty S, Al‐Saffar AZ, Elshibani FA, Chrysin REA. The Flavonoid Molecule of Antioxidant Interest. ChemistrySelect. 2023;8(48):e202303306.
66. Havsteen BH. The biochemistry and medical significance of the flavonoids. Pharmacol Ther. 2002;96(2–3):67–202. doi:10.1016/s0163-7258(02)00298-x
67. Zhang L, Kong Y, Wu D, et al. Three flavonoids targeting the beta-hydroxyacyl-acyl carrier protein dehydratase from Helicobacter pylori: crystal structure characterization with enzymatic inhibition assay. Protein Sci. 2008;17(11):1971–1978. doi:10.1110/ps.036186.108
68. Lu L, Zhao Y, Yi G, et al. Quinic acid: a potential antibiofilm agent against clinical resistant pseudomonas aeruginosa. Chin Med. 2021;16(1):72. doi:10.1186/s13020-021-00481-8
69. Benali T, Bakrim S, Ghchime R, et al. Pharmacological insights into the multifaceted biological properties of quinic acid. Biotechnol Genet Eng Rev. 2022:1–30. doi:10.1080/02648725.2022.2122303.
70. Kot B, Wicha J, Piechota M, Wolska K, Gruzewska A. Antibiofilm activity of trans-cinnamaldehyde, p-coumaric, and ferulic acids on uropathogenic Escherichia coli. Turk J Med Sci. 2015;45(4):919–924. doi:10.3906/sag-1406-112
71. Pei ZJ, Li C, Dai W, et al. The anti-biofilm activity and mechanism of apigenin-7-o-glucoside against Staphylococcus aureus and Escherichia coli. Infect Drug Resist. 2023;16:2129–2140. doi:10.2147/IDR.S387157
72. Liu Y, Han L, Yang H, Liu S, Huang C. Effect of apigenin on surface-associated characteristics and adherence of Streptococcus mutans. Dent Mater J. 2020;39(6):933–940. doi:10.4012/dmj.2019-255
73. Mohammed HA, Khan RA, Abdel-Hafez AA, et al. Phytochemical profiling, in vitro and in silico anti-microbial and anti-cancer activity evaluations and staph gyraseB and h-TOP-IIbeta receptor-docking studies of major constituents of zygophyllum coccineum L. Aqueous-ethanolic extract and its subsequent fractions: an approach to validate traditional phytomedicinal knowledge. Molecules. 2021;26(3). doi:10.3390/molecules26030577
74. Rugaie OA, Mohammed HA, Alsamani S, et al. Antimicrobial, antibiofilm, and antioxidant potentials of four halophytic plants, euphorbia chamaesyce, bassia arabica, fagonia mollis, and haloxylon salicornicum growing in Qassim Region of Saudi Arabia: phytochemical profile and in vitro and in silico bioactivity investigations. Antibiotics. 2023;12(3). doi:10.3390/antibiotics12030501
75. Mohammed HA, Aspatwar A, Aljarbooa AF, Qureshi KA. Comparative study of volatile oil constituents, anti-microbial properties, and antibiofilm activities in eucalyptus camaldulensis and eucalyptus globulus : insights from central Saudi Arabia. J Essent Oil Bear Plants. 2024;27(2):341–355. doi:10.1080/0972060x.2024.2324343
76. Ma R, Levard C, Marinakos SM, et al. Size-controlled dissolution of organic-coated silver nanoparticles. Environ Sci Technol. 2012;46(2):752–759. doi:10.1021/es201686j
77. Govindan Nadar R, Chackaravarthy G, Ramachandran G, et al. Isolation and molecular identification of biofilm producing P. aeruginosa and K. pneumoniae from urinary tract infections patient urine sample. J Infect Public Health. 2021;14(12):1875–1880. doi:10.1016/j.jiph.2021.11.004
78. Almalki MA, Varghese R. Prevalence of catheter associated biofilm producing bacteria and their antibiotic sensitivity pattern. J King Saud Univ Sci. 2020;32(2):1427–1433. doi:10.1016/j.jksus.2019.11.037
79. Chant C, Smith OM, Marshall JC, Friedrich JO. Relationship of catheter-associated urinary tract infection to mortality and length of stay in critically ill patients: a systematic review and meta-analysis of observational studies. Crit Care Med. 2011;39(5):1167–1173. doi:10.1097/CCM.0b013e31820a8581
80. Hooton TM, Bradley SF, Cardenas DD, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 international clinical practice guidelines from the infectious diseases society of America. Clin Infect Dis. 2010;50(5):625–663. doi:10.1086/650482
81. Saleem M, Syed Khaja AS, Hossain A, et al. Catheter-associated urinary tract infection in intensive care unit patients at a tertiary care hospital, Hail, Kingdom of Saudi Arabia. Diagnostics. 2022;12(7). doi:10.3390/diagnostics12071695
82. Kader AA, Angamuthu K. Extended-spectrum beta-lactamases in urinary isolates of Escherichia coli, Klebsiella pneumoniae and other gram-negative bacteria in a hospital in Eastern Province, Saudi Arabia. Saudi Med J. 2005;26(6):956–959.
83. Albu S, Voidazan S, Bilca D, et al. Bacteriuria and asymptomatic infection in chronic patients with indwelling urinary catheter: the incidence of ESBL bacteria. Medicine. 2018;97(33):e11796. doi:10.1097/MD.0000000000011796
84. Mazzariol A, Bazaj A, Cornaglia G. Multi-drug-resistant Gram-negative bacteria causing urinary tract infections: a review. J Chemother. 2017;29(sup1):2–9. doi:10.1080/1120009X.2017.1380395
85. Mohanta YK, Biswas K, Jena SK, Hashem A, Abd Allah EF, Mohanta TK. Anti-biofilm and antibacterial activities of silver nanoparticles synthesized by the reducing activity of phytoconstituents present in the Indian medicinal plants. Front Microbiol. 2020;11:1143. doi:10.3389/fmicb.2020.01143
86. Goda RM, El-Baz AM, Khalaf EM, Alharbi NK, Elkhooly TA, Shohayeb MM. Combating bacterial biofilm formation in urinary catheter by green silver nanoparticle. Antibiotics. 2022;11(4). doi:10.3390/antibiotics11040495
87. Lethongkam S, Paosen S, Bilhman S, et al. Eucalyptus-mediated synthesized silver nanoparticles-coated urinary catheter inhibits microbial migration and biofilm formation. Nanomaterials. 2022;12(22):
88. Divya M, Kiran GS, Hassan S, Selvin J. Biogenic synthesis and effect of silver nanoparticles (AgNPs) to combat catheter-related urinary tract infections. Biocataly Agricul Biotechnol. 2019;18:101037. doi:10.1016/j.bcab.2019.101037
89. Morones JR, Elechiguerra JL, Camacho A, et al. The bactericidal effect of silver nanoparticles. Nanotechnology. 2005;16(10):2346–2353. doi:10.1088/0957-4484/16/10/059
90. Verma SK, Jha E, Sahoo B, et al. Mechanistic insight into the rapid one-step facile biofabrication of antibacterial silver nanoparticles from bacterial release and their biogenicity and concentration-dependent in vitro cytotoxicity to colon cells. RSC Advances. 2017;7(64):40034–40045. doi:10.1039/c7ra05943d
91. Yuan Z, Li J, Cui L, Xu B, Zhang H, Yu C-P. Interaction of silver nanoparticles with pure nitrifying bacteria. Chemosphere. 2013;90(4):1404–1411. doi:10.1016/j.chemosphere.2012.08.032
92. Li WR, Xie XB, Shi QS, Zeng HY, Ou-Yang YS, Chen YB. Antibacterial activity and mechanism of silver nanoparticles on Escherichia coli. Appl Microbiol Biotechnol. 2010;85(4):1115–1122. doi:10.1007/s00253-009-2159-5
93. Zhang T, Wang L, Chen Q, Chen C. Cytotoxic potential of silver nanoparticles. Yonsei Med J. 2014;55(2):283–291. doi:10.3349/ymj.2014.55.2.283
94. Kalishwaralal K, BarathManiKanth S, Pandian SRK, Deepak V, Gurunathan S. Silver nanoparticles impede the biofilm formation by pseudomonas aeruginosa and staphylococcus epidermidis. Colloids and Surfaces B: Biointerfaces. 2010;79(2):340–344. doi:10.1016/j.colsurfb.2010.04.014
95. Park E-J, Yi J, Kim Y, Choi K, Park K. Silver nanoparticles induce cytotoxicity by a Trojan-horse type mechanism. Toxicology in Vitro. 2010;24(3):872–878. doi:10.1016/j.tiv.2009.12.001
96. Mohanta YK, Biswas K, Jena SK, Hashem A, EF A, Mohanta TK. Anti-biofilm and antibacterial activities of silver nanoparticles synthesized by the reducing activity of phytoconstituents present in the Indian medicinal plants. Front Microbiol. 2020;11. doi:10.3389/fmicb.2020.01143.
97. Deans SG, Svoboda KP. The antimicrobial properties of marjoram (Origanum majorana L.) volatile oil. Flav Fragran J. 2006;5(3):187–190. doi:10.1002/ffj.2730050311
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




