Back to Journals » Infection and Drug Resistance » Volume 18
Predictors for Invasive Pulmonary Aspergillosis in Acute-on-Chronic Liver Failure Patients: A Retrospective Study
Authors Yuan C, Zhu R , Hu L, Li J
Received 25 September 2024
Accepted for publication 8 February 2025
Published 17 February 2025 Volume 2025:18 Pages 909—918
DOI https://doi.org/10.2147/IDR.S497840
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandip Patil
Chenxi Yuan,1,2,* Rongqing Zhu,1,2,* Lifen Hu,1,2 Jiabin Li1,2
1Department of Infectious Diseases & Anhui Center for Surveillance of Bacterial Resistance, The First Affiliated Hospital of Anhui Medical University, Hefei, 230022, People’s Republic of China; 2Anhui Province Key Laboratory of Infectious Diseases & Institute of Bacterial Resistance, Anhui Medical University, Hefei, 230022, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jiabin Li; Lifen Hu, Email [email protected]; [email protected]
Introduction: Acute-on-chronic liver failure (ACLF) is a severe syndrome that manifests as acute liver function deterioration and organ failure. Coinfection with invasive pulmonary aspergillosis (IPA) in ACLF patients is characterized by high mortality and increasing morbidity. The aim of this study was to explore the early warning factors and prognosis of ACLF patients with IPA coinfection.
Methods: In this retrospective study, we collected clinical, biochemical, and microbiological data from patients with ACLF and IPA from May 2019 to May 2023. Univariable and multivariate analyses were used to identify independent risk factors for IPA in ACLF patients. Moreover, the area under the curve (AUC) and decision curve analysis (DCA) were used to evaluate the model performance.
Results: A total of 438 patients with ACLF were enrolled, 408 (93.2%) non-IPA patients and 30 IPA (6.8%) including 29 probable cases and one proven case. The 28-day case fatality rate (56.7% vs 29.4%) was higher in ACLF patients with IPA than in ACLF patients without IPA, but without statistical difference. Multivariate analysis revealed that early warning factors for IPA coinfection in ACLF patients included nausea (p = 0.010), expectoration (p < 0.001), bacterial and fungal infections (p < 0.001), corticosteroid use (p = 0.037), surgery (p = 0.081), haemoptysis (p = 0.015) and increased leukocyte counts (p = 0.010). The AUC was 0.934 (p < 0.001), and DCA verified the validity and clinical effectiveness of our model.
Conclusion: These findings provide valuable insights for clinicians in the early diagnosis of IPA in ACLF patients and may facilitate timely intervention and treatment.
Keywords: acute-on-chronic liver failure, invasive pulmonary aspergillosis, decision curve analysis
Introduction
Acute-on-chronic liver failure (ACLF), a severe clinical syndrome caused by various factors, including severe disruption of synthesis, detoxification, immune metabolism, and biological transformation, is characterized by acute decompensation, organ failure and high 28-day mortality (32%).1–3 It presents as a group of clinical symptoms mainly characterized by hepatic insult, jaundice and coagulopathy, with decreased liver function, severe disruption of the cellular immune system, and increased risk of infection and death.1,4–10 A variety of bacterial, parasitic, and fungal infections may affect the liver. The prevalence of fungal coinfection ranges between 2% and 15%, and fungal coinfection has been associated with worsening liver function and increasing mortality.11–13
Aspergillus fumigatus was listed as the critical priority group in the first fungal priority pathogen list issued by the World Health Organization (WHO) in 2022, and relevant research and public health action need to be expanded.14 Invasive pulmonary aspergillosis (IPA) is a severe opportunistic infection that mainly affects immunocompromised patients, leading to prolonged neutropenia and cancer.13 It is difficult to obtain pathologic samples from patients at high risk of IPA, so it is important to identify early diagnostic warning signs. The 6-week mortality of IPA is 20–30%, especially in critical patients.15–18
IPA seriously affects the prognosis of patients with ACLF and leads to deterioration of their condition. The prevalence of IPA in hepatitis B virus (HBV)-related ACLF patients has been reported to be 5.0–8.3%, with the mortality rate increasing to 80% in patients with IPA.2,19 In terms of liver failure with IPA coinfection, patients with hepatic failure without a definite type or mainly individual cases have been studied.12,16,17,20,21 So far, there are few studies on the ACLF patients with IPA, and some scholars have analyzed its prognosis model and treatment, but its early warning risk factors are still unknown.22–24
The onset of IPA in the context of liver failure is occult, and early symptoms and imaging features are not typical, making it difficult to diagnose. Few studies have focused on Aspergillus infection in ACLF patients, and early warning signs for developing IPA in ACLF patients have not been characterized.
The primary aim of this study was to compare the clinical phenotypes of ACLF patients with IPA and non-IPA patients to identify early warning risk factors. This study developed a model for the early diagnosis of IPA in ACLF patients to facilitate timely intervention and treatment and improve patient survival.
Materials and Methods
Study Design and Participants
A retrospective study was conducted among 438 ACLF patients from May 2019 to May 2023 at the First Affiliated Hospital of Anhui Medical University. The exclusion criteria were as follows: (1) younger than 18 years, (2) immunocompromised due to human immunodeficiency virus infection, and (3) prior to organ transplantation or pregnancy before or during hospitalization. The study protocol adhered to the principles outlined in the Declaration of Helsinki and complied with relevant national laws and policies. Approval for this study was obtained from the Human Ethics Committee of Anhui Medical University (approval no. TJ20240556). Given the retrospective nature of the study, the ethics committee waived the requirement for informed consent. Verbal informed consent was obtained and the ethics committee approved this consent process. We ensure that the data was anonymized or maintained with confidentiality.
Diagnosis
Patients who were diagnosed with ACLF during hospitalization were screened. ACLF diagnosis was defined according to the Asian Pacific Association for the Study of the Liver (APASL) consensus recommendations for ACLF:25 (1) jaundice (serum bilirubin ≥5 mg/dL (85 mmol/L)); (2) coagulopathy (international normalized ratio (INR) ≥1.5); and (3) complications within 4 weeks due to clinical ascites and/or encephalopathy. Failure to meet one of the above three criteria excluded the diagnosis of ACLF. We classified the ACLF patients with IPA into proven, probable and possible groups based on the European Organization for Research and Treatment of Cancer and Mycoses Study Group Education and Research Consortium (EORTC/MSGERC) consensus definitions of invasive fungal disease.26,27 In this study, patients were defined as having probable IPA if they had at least 1 clinical feature and had available mycologic evidence. Clinical features included the presence of 1 of the following patterns on computed tomography (CT): dense, well-circumscribed lesions with or without a halo sign, an air crescent sign, a cavity, or wedge-shaped and segmental or lobar consolidation. Mycological evidence included (1) galactomannan antigen detection in plasma with a cut-off point of 0.5 and (2) microscopic detection of fungal elements in bronchial brushing, bronchoalveolar lavage (BAL) or sputum, indicating the presence of a mould. The proven group was defined as patients who met the criteria for probable IPA and whose blood culture yielded Aspergillus. The flow chart for selecting ACLF patients with IPA is shown in Figure 1.
 |
Figure 1 Flow diagram of patient selection. |
Data Retrieval
We extracted the patients’ clinical information from the hospital’s electronic medical records database. The following data were collected: demographic data (sex and age), patient clinical characteristics (fever, nausea, expectoration, altered consciousness, acute variceal bleeding, and haemoptysis), diabetes status, presence of comorbidities (hepatorenal syndrome, hepatic encephalopathy, septicaemia, spontaneous peritonitis, hyponatremia, hypoproteinaemia, and gastrointestinal bleeding), liver aetiology (hepatitis B virus, drug use, alcohol use, autoimmune disease, and hepatolenticular degeneration), invasive operation including puncture and intubation, surgery, mechanical ventilation, transjugular intrahepatic portosystemic shunt (TIPS) placement, albumin infusion, artificial liver support system use, baseline full blood count, biochemistry results, liver and renal function, corticosteroid use, antimicrobial exposure (carbapenems and cephalosporins), length of hospital stay, ICU admission, 28-day fatality rate and documentation of bacterial and fungal infections. In our study, bacterial and fungal infections specifically referred to bacterial and fungal infections in addition to IPA coinfection in ACLF patients.
Statistical Analysis
IBM SPSS 24.0 and R software (version 4.3.2) were used for analysis. Normally distributed data are presented as the mean± standard deviation (SD). The independent sample t test was used for comparisons between two groups. Nonnormally distributed data are expressed as medians (Q1‒Q3), and the Mann‒Whitney U-test was used for comparisons between two groups. Categorical variables are expressed as the sample size (n) and percentage (%). The chi-squared test or Fisher’s exact test was used for categorical variables. We considered a P value <0.05 to indicate statistical significance. Variables found to be significantly different (P < 0.05) in group comparisons were included in binary logistic regression (LR) to identify risk factors for ACLF in patients with IPA. Binary logistic regression (LR) can apply the minimum number of factors to construct the model, not all of which are statistically significant factors. Therefore, “surgery” is included in the model construction. The results are reported as β, standard error, odds ratio (OR), and P values. To make the results of the predictive model more obvious, factors included in the model were considered to indicate statistical significance, were used as visual indicators on a graph. In addition, the corresponding area under the curve (AUC) was calculated to assess the discrimination ability. Moreover, decision curve analysis (DCA) was used to evaluate the model performance.
Results
Clinical Phenotype of ACLF Patients With IPA
The hospital records of 571 patients with liver failure who were hospitalized between May 2019 and May 2023 were screened; 133 individuals were excluded, 438 patients with ACLF were ultimately enrolled in the study, and 30 patients were diagnosed with IPA - 29 probable cases and one proven case (Figure 1). As shown in Table 1, the median age was 53 years (Q1-Q3: 46–61 years), and 335 (76%) of the 438 patients were male. The main aetiologies of ACLF among patients with known causes were HBV and alcohol use. The most frequent symptoms were expectoration (66.7% vs 11.0%), nausea (16.7% vs 4.2%) and acute variceal bleeding (13.3% vs 10.5%) in the IPA group and non-IPA group. The occurrence rates of other symptoms, such as haemoptysis, altered consciousness, and fever, were greater in the ACLF with IPA group.
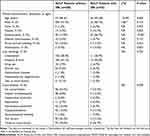 |
Table 1 | Baseline Characteristics of the Study Participants (n=438) |
Compared with the non-IPA group, the IPA group had more leukocytes [6.2 (4.4–8.9) *109/L vs 9.0 (6.2–13.0) *109/L], a lower lymphocyte percentage [17.5 (10.6–23.4) vs 14.0 (7.5–25.2)] and a lower monocyte percentage [8.7 (6.7–11.0) vs 7.4 (5.7–9.3)]. The total protein, globulin, total bilirubin, platelet, prothrombin time, INR, and thrombin time were greater in the non-IPA group, while the serum urea and haemoglobin levels were lower than those in the IPA group, as shown in Table 2.
 |
Table 2 Laboratory Parameters and Clinical Outcomes of the Study Participants (n=438) |
Hepatic encephalopathy and gastrointestinal bleeding occurred more frequently in patients with ACLF and IPA, while hepatorenal syndrome, septicaemia, spontaneous peritonitis, hypoproteinaemia and multiple comorbidities were less frequent in patients with ACLF and IPA.
The mean model for end-stage liver disease score (25.0 vs 23.1, p = 0.211) was greater in the ACLF patients than in the ACLF patients with IPA. Nevertheless, the ICU admission rate (23.3% vs 2.7%, p < 0.001) and bacterial and fungal infection rate (63.3% vs 15.0%, p < 0.001) were greater in ACLF patients with IPA. Patients with IPA coinfection received more clinical interventions than patients without IPA coinfection, including surgery (13.3% vs 2.0%, p < 0.001), mechanical ventilation (16.7% vs 2.0%, p < 0.001), invasive operations (83.3% vs 68.9%), albumin infusion (86.7% vs 85.5%), artificial liver support system use (70.0% vs 44.9%, p = 0.008), carbapenem application (66.7% vs 43.6%, p = 0.014), and corticosteroid use (43.3% vs 11.3%, p < 0.001).
Risk Factors for IPA in ACLF Patients
In this study, univariable analysis revealed statistically significant differences in 17 factors, including total protein, globulin, serum urea, leukocyte count, neutrophil count, monocyte percentage, thrombin time, surgery, mechanical ventilation, corticosteroid use, artificial liver support system use, nausea, expectoration, haemoptysis, ICU admission, carbapenem use, and bacterial and fungal infections, between the IPA group and the non-IPA group. As shown in Table 3, 7 variables, including leukocyte count, corticosteroid use, nausea, expectoration, haemoptysis, surgery and bacterial and fungal infections, were identified as early warning signs for IPA occurrence in ACLF patients. Based on independent predictors identified through binary logistic regression, we developed a risk prediction model for the early detection of IPA in ACLF patients, aiming to guide clinical interventions (Figure 1). To make the results of the predictive model more obvious, we converted the indicators into a nomogram. The validity of our model was determined using multiple indicators, including the AUC (0.934, p < 0.001), Youden’s index (0.758), sensitivity (0.900), specificity (0.858), cut-off value (0.064), Hosmer–Lemeshow test (chi2 = 6.974, p = 0.539) and DCA (Figure 2). The DCA revealed that using this model provides additional benefits for the entire cohort, as shown in Figure 3.
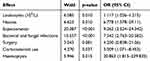 |
Table 3 | Multivariable Logistic Regression for Exploring Risk Factor of ACLF With IPA Patients |
 |
Figure 2 ROC curves of the model for the risk of ACLF with IPA. |
 |
Figure 3 Nomogram and DCA curves of the model for the risk of ACLF with IPA. (A) Nomogram and (B) decision curve analysis of the model for the risk of ACLF with IPA. |
Clinical Outcomes
We found that the 28-day case fatality rate did not significantly differ between the groups; however, there was a clear trend towards a higher 28-day case fatality rate in the IPA group, as shown in Figure 3. The 28-day case fatality rate (56.7% vs 29.4%) was greater in ACLF patients with IPA, and the length of hospital stay was longer (24 days [Q1-Q3: 15–47 days] vs 22 days [Q1-Q3: 9–39 days], p = 0.1), as shown in Table 2. The 28-day mortality rate among patients was 31.3% (137 of 438 patients). No significant difference in the 28-day case fatality rate was observed between female and male patients. Infections were considered a significant contributing factor to death for ACLF patients. As shown in sTable 1, there was a significant difference between the incidence of bacterial and fungal infections and the 28-day case fatality rate of IPA among the ACLF patients (26.3% vs 14.6%, p = 0.003). The sTable 2 shown the infection sites and cases for “Bacterial and fungal infections” in ACLF patients.
Discussion
Identifying the early warning risk factors for IPA in ACLF patients is critical for administering early antifungal prophylaxis and empiric treatment. This study is the first to describe the early warning signs of ACLF patients with IPA. The incidence of IPA coinfection in ACLF patients was 6.8% in this study. Leukocyte count, corticosteroid use, nausea, expectoration, haemoptysis, surgery, and bacterial and fungal infections were identified as early warning signs for IPA occurrence in ACLF patients. This retrospective study established an early prediction model for ACLF patients with IPA to guide clinicians in achieving an early IPA diagnosis in these patients.
ACLF patients with IPA group had an increased leukocytes count, especially neutrophil count, while had a decreased lymphocyte percentage as compared to the ACLF patients without IPA group. These findings suggest that the innate immune system plays an important role in the development of ACLF, which is consistent with previous findings.3 Our findings first indicated that nausea was significantly associated with early warning risk factors of IPA, possibly because inflammation, septicaemia and Invasive Aspergillosis can also affect the gastrointestinal tract in patients with cirrhosis and portal hypertension.
Underlying pulmonary disease is more likely to occur in the upper airway, bronchi, lung parenchyma, and contiguous structures.28,29 It has the potential to cause extensive and diffuse damage to the respiratory mucosa, disrupting normal ciliary clearance. Moreover, underlying pulmonary disease can create conditions conducive to fungal invasion by impairing alveolar macrophages, hindering local phagocytic activity, delaying immune response initiation, and suppressing anti-inflammatory mechanisms.30 Thus, these phenomena explain why expectoration and haemoptysis were identified as independent factors influencing IPA development.31 When encountering patients with these symptoms clinically, clinicians need to be aware that they may be at high risk of IPA and initiate targeted early prevention and treatment.
This study also indicated that bacterial and fungal infections were independent risk factors for IPA in ACLF patients, consistent with previous results.28,32 Infection promotes a highly inflammatory state in ACLF patients.33,34 Recently, it has been shown that the immune response to sepsis is biphasic, ie, the initial hyperinflammatory phase may be followed by an anti-inflammatory response, leading to a hyperinflammatory condition.33,35,36 This process is known as compensatory anti-inflammatory response syndrome or immune paralysis and can be viewed as a form of acquired immunodeficiency.4,34 The existence of a constant and persistent hyperinflammatory milieu contributes to immunosuppression by inhibiting innate immune defensive responses and regulating immune cell expansion.37,38 The clinical consequence of this inhibition is increased susceptibility to IPA infection, a serious opportunistic infection that mainly affects immunocompromised patients.39 Steroid exposure is a well-known risk factor for IPA coinfection. Several studies have demonstrated that corticosteroids have immunosuppressive effects and impair phagocytosis, oxidative bursts, cytokine and chemokine production, and the antifungal activity of monocytes/macrophages, which may increase the risk of IPA coinfection.
Our study had several limitations. First, due to the low incidence of fungal coinfection in ACLF patients and the retrospective nature of this study, the sample sizes of the two groups were unbalanced. Second, due to the retrospective nature of the study, some data, such as the dosage, specific timing, and duration of antibiotic and glucocorticoid treatment before admission, were missing. As our analysis revealed inconsistent predictive effects of different antibiotics and hormones on patient outcomes, further prospective studies are needed to confirm the effect of antibiotic and glucocorticoid use on IPA.
Conclusions
Compared with ACLF patients without IPA, ACLF patients with IPA had a higher 28-day case fatality rate, but without statistical difference. Leukocyte count, corticosteroid use, nausea, expectoration, haemoptysis, bacterial and fungal infections, and surgery were significantly more common in ACLF patients with IPA. This study can help clinicians effectively identify high-risk patients and initiate targeted early prevention and treatment.
Data Sharing Statement
The data that support the findings of this study are included and will be available from the corresponding author(s) upon reasonable request.
Ethics/Ethical Approval
The study protocol adhered to the principles outlined in the Declaration of Helsinki and complied with relevant national laws and policies. Approval for this study was obtained from the Human Ethics Committee of Anhui Medical University (approval no. TJ20240556). Given the retrospective nature of the study, the ethics committee waived the requirement for informed consent.
Acknowledgments
The authors would like to thank all study participants for their involvement in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81973983, 82270015, 82302577, 82304209, 82370016), Project funded by China Postdoctoral Science Foundation (No. 2023M730018, 2022M720196), Anhui Province Scientific Research Planning Project (2023AH010083, 2023AH053282, AHWJ2022a018).
Disclosure
All authors participated in the development, review and approval of the manuscript. All authors have read and approved the final manuscript. We confirm that the manuscript has not been submitted (or simultaneously) elsewhere, is not under consideration by another journal at the time of submission and that no portion of the data has been or will be published elsewhere. The authors declare that they have no conflicts of interest to disclose and have approved the manuscript. Chenxi Yuan, Rongqing Zhu, Jiabin Li and Lifen Hu declare that they have no competing interests.
References
1. Arroyo V, Moreau R, Jalan R. Acute-on-chronic liver failure. New Engl J Med. 2020;382(22):2137–2145.
2. Arroyo V, Moreau R, Kamath PS, et al. Acute-on-chronic liver failure in cirrhosis. Nature Reviews Disease Primers. 2016;2:16041. doi:10.1038/nrdp.2016.41
3. Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144(7):
4. Wasmuth HE, Kunz D, Yagmur E, et al. Patients with acute on chronic liver failure display ”sepsis-like” immune paralysis. J Hepatol. 2005;42(2):195–201. doi:10.1016/j.jhep.2004.10.019
5. Hernaez R, Solà E, Moreau R, Ginès P. Acute-on-chronic liver failure: an update. Gut. 2017;66(3):541–553. doi:10.1136/gutjnl-2016-312670
6. Malik R, Mookerjee RP, Jalan R. Infection and inflammation in liver failure: two sides of the same coin. J Hepatol. 2009;51(3):426–429. doi:10.1016/j.jhep.2009.06.013
7. Delano MJ, Ward PA. The immune system’s role in sepsis progression, resolution, and long-term outcome. Immunol Rev. 2016;274(1):330–353. doi:10.1111/imr.12499
8. Bajaj JS, O’Leary JG, Reddy KR, et al. Survival in infection-related acute-on-chronic liver failure is defined by extrahepatic organ failures. Hepatology. 2014;60(1):250–256. doi:10.1002/hep.27077
9. Jalan R, Yurdaydin C, Bajaj JS, et al. Toward an improved definition of acute-on-chronic liver failure. Gastroenterology. 2014;147(1):4–10. doi:10.1053/j.gastro.2014.05.005
10. Li H, Chen LY, Zhang NN, et al. Characteristics, diagnosis and prognosis of acute-on-chronic liver failure in cirrhosis associated to hepatitis B. Sci Rep. 2016;6(1):25487. doi:10.1038/srep25487
11. Schmiedel Y, Zimmerli S. Common invasive fungal diseases: an overview of invasive candidiasis, aspergillosis, cryptococcosis, and Pneumocystis pneumonia. Swiss Med Weekly. 2016;146:w14281.
12. Prodanovic H, Cracco C, Massard J, et al. Invasive pulmonary aspergillosis in patients with decompensated cirrhosis: case series. BMC Gastroenterol. 2007;7(1):2. doi:10.1186/1471-230X-7-2
13. Ma R, Chen Q, Huang Y, et al. The Prognosis of Patients Tested Positive for Stenotrophomonas maltophilia from Different Sources. Infect Drug Resist. 2023;16:4779–4787. doi:10.2147/IDR.S417151
14. Parums DV. Editorial: the world health organization (WHO) fungal priority pathogens list in response to emerging fungal pathogens during the COVID-19 pandemic. Med Sci Monit: Inter Med J Exp Clin Res. 2022;28:e939088.
15. Herbrecht R, Denning DW, Patterson TF, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. New Engl J Med. 2002;347(6):408–415.
16. Tavazzi G, Via G, Marzani FC, Mojoli F. Invasive pulmonary aspergillosis after near-drowning. Lancet Infect Dis. 2016;16(12):1430. doi:10.1016/S1473-3099(16)30202-X
17. Moreno-González G, Ricart de Mesones A, Tazi-Mezalek R, Marron-Moya MT, Rosell A, Mañez R. Invasive pulmonary aspergillosis with disseminated infection in immunocompetent patient. Canadian Resp J. 2016;2016:7984032. doi:10.1155/2016/7984032
18. Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van Wijngaerden E. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med. 2004;170(6):621–625. doi:10.1164/rccm.200401-093OC
19. Zhang X, Shen S, Dai X, et al. Clinical risk score for invasive pulmonary aspergillosis in patients with liver failure: a retrospective study in Zhejiang. Front Med. 2021;8:762504. doi:10.3389/fmed.2021.762504
20. Gustot T, Maillart E, Bocci M, et al. Invasive aspergillosis in patients with severe alcoholic hepatitis. J Hepatol. 2014;60(2):267–274. doi:10.1016/j.jhep.2013.09.011
21. Zhang X, Yang M, Hu J, Zhao H, Li L. Epidemiology of invasive pulmonary aspergillosis in patients with liver failure: clinical presentation, risk factors, and outcomes. J Inter Med Res. 2018;46(2):819–827. doi:10.1177/0300060517729907
22. Chen D, Qian Z, Su H, et al. Invasive pulmonary aspergillosis in acute-on-chronic liver failure patients: short-term outcomes and antifungal options. Infect Dis Ther. 2021;10(4):2525–2538. doi:10.1007/s40121-021-00524-5
23. Gao J, Zhang Q, Wu Y, et al. Improving survival of acute-on-chronic liver failure patients complicated with invasive pulmonary aspergillosis. Sci Rep. 2018;8(1):876. doi:10.1038/s41598-018-19320-2
24. Yu X, Xu L, Zheng J, et al. Efficacy and safety of voriconazole in the treatment of invasive pulmonary aspergillosis in patients with liver failure: study protocol for a randomized controlled clinical trial. Trials. 2023;24(1):811. doi:10.1186/s13063-023-07755-6
25. Sarin SK, Choudhury A, Sharma MK, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Internat. 2019;13(4):353–390. doi:10.1007/s12072-019-09946-3
26. Alexander BD, Lamoth F, Heussel CP, et al. Guidance on imaging for invasive pulmonary aspergillosis and mucormycosis: from the imaging working group for the revision and update of the consensus definitions of fungal disease from the EORTC/MSGERC. Clin Infec Dis: Off Publ Infec Dis Soc Ame. 2021;72(Suppl 2):S79–s88. doi:10.1093/cid/ciaa1855
27. Donnelly JP, Chen SC, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer and the Mycoses Study Group Education and Research Consortium. Clin Infec Dis: Off Publ Infec Dis Soc Ame. 2020;71(6):1367–1376. doi:10.1093/cid/ciz1008
28. Tudesq JJ, Peyrony O, Lemiale V, Azoulay E. Invasive pulmonary aspergillosis in nonimmunocompromised hosts. Semin Resp Crit Care Med. 2019;40(4):540–547. doi:10.1055/s-0039-1696968
29. Perfect JR, Cox GM, Lee JY, et al. The impact of culture isolation of Aspergillus species: a hospital-based survey of aspergillosis. Clin Infec Dis: Off Publ Infec Dis Soc Ame. 2001;33(11):1824–1833. doi:10.1086/323900
30. Woo YD, Jeong D, Chung DH. Development and functions of alveolar macrophages. Mol Cells. 2021;44(5):292–300. doi:10.14348/molcells.2021.0058
31. Cornillet A, Camus C, Nimubona S, et al. Comparison of epidemiological, clinical, and biological features of invasive aspergillosis in neutropenic and nonneutropenic patients: a 6-year survey. Clin Infec Dis: Off Publ Infec Dis Soc Ame. 2006;43(5):577–584. doi:10.1086/505870
32. Garnacho-Montero J, Amaya-Villar R, Ortiz-Leyba C, et al. Isolation of Aspergillus spp. from the respiratory tract in critically ill patients: risk factors, clinical presentation and outcome. Critical Care. 2005;9(3):R191–9. doi:10.1186/cc3488
33. Clària J, Stauber RE, Coenraad MJ, et al. Systemic inflammation in decompensated cirrhosis: characterization and role in acute-on-chronic liver failure. Hepatology. 2016;64(4):1249–1264. doi:10.1002/hep.28740
34. Bernsmeier C, Pop OT, Singanayagam A, et al. Patients with acute-on-chronic liver failure have increased numbers of regulatory immune cells expressing the receptor tyrosine kinase MERTK. Gastroenterology. 2015;148(3):603–15.e14. doi:10.1053/j.gastro.2014.11.045
35. Casulleras M, Zhang IW, López-Vicario C, Leukocytes CJ. Systemic inflammation and immunopathology in acute-on-chronic liver failure. Cells. 2020;9(12):2632. doi:10.3390/cells9122632
36. Li J, Liang X, Jiang J, et al. PBMC transcriptomics identifies immune-metabolism disorder during the development of HBV-ACLF. Gut. 2022;71(1):163–175. doi:10.1136/gutjnl-2020-323395
37. O’Brien AJ, Fullerton JN, Massey KA, et al. Immunosuppression in acutely decompensated cirrhosis is mediated by prostaglandin E2. Nat Med. 2014;20(5):518–523. doi:10.1038/nm.3516
38. Bernsmeier C, Triantafyllou E, Brenig R, et al. CD14(+) CD15(-) HLA-DR(-) myeloid-derived suppressor cells impair antimicrobial responses in patients with acute-on-chronic liver failure. Gut. 2018;67(6):1155–1167. doi:10.1136/gutjnl-2017-314184
39. Jenks JD, Nam HH, Hoenigl M. Invasive aspergillosis in critically ill patients: review of definitions and diagnostic approaches. Mycoses. 2021;64(9):1002–1014. doi:10.1111/myc.13274
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

