Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
Preoperative Prognostic Nutritional Index as a Useful Tool for Predicting Postoperative Delirium in Elderly Patients with Degenerative Lumbar Diseases
Authors Zhou J, Tang J, Xie S, Shao H, Xia C , Huang Y, Zhao T
Received 5 February 2025
Accepted for publication 29 May 2025
Published 7 June 2025 Volume 2025:21 Pages 851—859
DOI https://doi.org/10.2147/TCRM.S520912
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor De Yun Wang
Jinlei Zhou,1,* Jing Tang,2,* Shanggao Xie,1,* Haiyu Shao,1 Chen Xia,1 Yazeng Huang,1 Tingxiao Zhao1
1Center for Plastic & Reconstructive Surgery, Department of Orthopedics, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital, Hangzhou Medical College), Hangzhou, Zhejiang, People’s Republic of China; 2Zhejiang Rehabilitation Medical Center, Department of Orthopedics, Hangzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Tingxiao Zhao; Yazeng Huang, Center for Plastic & Reconstructive Surgery, Department of Orthopedics, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital, Hangzhou Medical College), Shangtang Road 158#, Hangzhou, Zhejiang, People’s Republic of China, Email [email protected]; [email protected]
Purpose: The high incidence of postoperative delirium (POD) among patients undergoing lumbar spine surgery presents a significant barrier to achieving enhanced postoperative recovery. Accordingly, a thorough understanding and precise identification of common risk factors for POD in this surgical context are crucial to mitigating its occurrence and facilitating improved recovery outcomes. This study is the first to assess the predictive value of the Prognostic Nutritional Index (PNI) for POD in elderly patients undergoing transforaminal lumbar interbody fusion (TLIF) for degenerative lumbar spine disease.
Methods: We conducted a retrospective analysis of the outcomes of TLIF surgery in elderly patients with degenerative lumbar spine disease between 2020 and 2024. The diagnosis of POD was based on postoperative medical records during hospitalization, using the Confusion Assessment Method. The PNI was calculated based on preoperative serum albumin levels and total lymphocyte counts. Multivariate logistic regression analysis was performed to evaluate the relationship between preoperative PNI scores and the occurrence of POD. Finally, the optimal PNI cut-off point for predicting POD was determined using the receiver operating characteristic curve.
Results: POD was observed in 61 of 370 patients, with PNI being significantly lower in the delirium group. The mean PNI values were 43.02± 3.44 in the non-delirium group and 48.53± 3.72 in the delirium group. Multivariate logistic regression analysis revealed that low PNI (OR: 0.743; 95% CI: 0.597– 0.924; p = 0.008), low serum albumin levels (OR: 0.759; 95% CI: 0.584– 0.987; p = 0.040), and advanced age (OR: 1.096; 95% CI: 1.030– 1.166; p = 0.004) were independent predictors of POD following TLIF. The area under the curve (AUC) for PNI on the receiver operating characteristic curve was 0.864± 0.025. The cutoff value for PNI, determined using the Youden index, was 45.825, with a sensitivity of 82.0% and a specificity of 74.4%.
Conclusion: The preoperative use of PNI holds promise as a valuable tool for assessing the risk of POD in elderly patients undergoing TLIF.
Keywords: postoperative delirium, delirium, prognostic nutritional index, controlled nutritional status index, transforaminal lumbar interbody fusion, dystrophy, elderly population
Introduction
Postoperative delirium (POD), an acute-onset transient psychiatric syndrome, is characterized by global cognitive impairment, reduced levels of consciousness, attentional disturbances, fluctuations in psychomotor activity, and disruptions in the sleep-wake cycle.1,2 Simultaneously, the high incidence of POD among patients undergoing lumbar spine surgery has emerged as a significant barrier to achieving swift postoperative recovery. Numerous clinical studies have reported that the incidence of POD among patients undergoing lumbar spine surgery ranges from 11.8% to 14.5%.3–5 In a retrospective study, Fineberg observed that patients with POD incurred additional costs of $8,065 for lumbar decompression procedures and $10,530 for lumbar fusion surgeries.3 Therefore, a comprehensive understanding and precise identification of common risk factors for POD in lumbar spine surgery are crucial for lowering its incidence and improving postoperative safety in these procedures.
The pathophysiological mechanisms underlying POD remain incompletely understood, with two predominant hypotheses prevailing. The first centers on neuroinflammation, proposing that peripheral cytokines compromise the integrity of the blood-brain barrier, thereby precipitating central inflammatory cascades; chronic stress is thought to act synergistically, modulating cytokine release and elevating cortisol levels.6 The second hypothesis implicates dysregulation of neurotransmitter systems, involving perturbations in critical neuromodulators such as acetylcholine, dopamine, glutamate, γ-aminobutyric acid, and serotonin.7 Furthermore, advanced age, as an independent risk factor, often elevates the risk of POD due to factors such as frailty, diminished functional reserve and recovery capacity, and reduced cerebral blood flow.8,9 A meta-analysis revealed that up to 21.3% of spinal surgery patients experience POD, with prevalence rates reaching as high as 40% in patients over the age of 70.8 Additionally, Prof. Pan’s study reported a POD prevalence of 14.5% among elderly patients undergoing lumbar spine surgery.4
In recent years, a growing body of research has underscored the high prevalence of malnutrition among elderly patients with degenerative spinal diseases and its significant association with clinical outcomes, emphasizing the critical importance of assessing nutritional status prior to surgery.10–12 The Prognostic Nutritional Index (PNI), derived from serum albumin levels and total lymphocyte counts, is extensively employed as a reliable tool for nutritional assessment across diverse clinical domains.13 The distinctive advantage of the PNI lies in its incorporation of the lymphocyte count, which enhances predictive sensitivity by reflecting the inflammatory status. This dual “nutritional-inflammatory” assessment renders the PNI a valuable tool for perioperative risk stratification.14,15 Shin reported that patients with a preoperative PNI < 50 exhibited a significantly higher risk of postoperative complications during orthopedic scoliosis surgery.12 However, no studies to date have investigated the relationship between preoperative PNI scores and the incidence of POD in elderly patients undergoing transforaminal lumbar interbody fusion (TLIF).
Therefore, this study aims to evaluate whether preoperative PNI scores can serve as reliable predictors of POD in this patient population. We hypothesize that the preoperative PNI score may serve as a crucial tool in assessing the risk of POD in elderly patients undergoing TLIF. Furthermore, we posit that lower PNI scores and albumin levels correlate with an increased risk of POD in this patient population.
Methods
Patients
Between January 2020 and July 2024, a total of 2333 patients who underwent lumbar fusion surgery at our institution were enrolled in this retrospective study. This study was approved by the Medical Ethics Review Committee of Zhejiang Provincial People’s Hospital (No. QT2025041). Given the retrospective nature of the analysis, the requirement for informed consent was waived. The inclusion criteria were as follows: (1) patients aged ≥ 60 years; (2) patients who underwent single-segment TLIF for degenerative lumbar spine disease; (3) availability of complete records detailing the patients’ visits and relevant clinical data. The exclusion criteria were as follows: (1) patients with spinal infections, tumours, or traumatic injuries; (2) those diagnosed with Parkinson’s disease or any malignant condition; and (3) Patients with cognitive impairment including dementia.16 All cases adhered rigorously to the inclusion and exclusion criteria defined by the research center, with the diagnosis of POD established in strict accordance with the Confusion Assessment Method (CAM).17 Enrolled patients were subsequently stratified into POD and non-POD groups.
Measured Data
Data were collected on gender, age, BMI, type of lumbar spine disease, personal and medical history, operative segment, duration of surgery, intraoperative blood loss, and postoperative complications. Laboratory indices were collected, including preoperative serum albumin levels, total cholesterol levels, hemoglobin levels, white blood cell count, total lymphocyte count and PNI. The PNI was originally introduced as a tool to predict postoperative complications by evaluating the preoperative nutritional status of patients undergoing colorectal cancer surgery.13 In addition, the PNI demonstrates high predictive accuracy for treatment outcomes across a broad spectrum of malignancies.18,19 The PNI is calculated using the following formula: PNI = 10 × serum albumin concentration (g/dL) + 0.005 × total lymphocyte count (per µL).18 It is noteworthy that immune competence plays a vital role in facilitating prompt postoperative recovery, with serum albumin levels and lymphocyte counts serving as key surrogate markers of immune function.20,21 The PNI, which combines serum albumin concentration and lymphocyte count, functions as a composite marker of systemic immunological competence and nutritional-metabolic status.
TLIF Surgical Procedure
All procedures in this study involved standardized single-level TLIF, performed by a dedicated surgical team led by a chief physician with over 20 years of certified expertise in spine surgery. The patient was positioned prone, with soft pads placed beneath the anterior chest and pelvis to allow the abdomen to hang freely. After standard sterile preparation, a posterior midline incision was made over the affected segment, and the skin and subcutaneous tissue were incised sequentially. The bilateral erector spinae muscles were dissected, allowing for adequate exposure of the laminae and facet joints of the affected segments. Pedicle screws were inserted bilaterally at the pedicle roots of the diseased level. A total laminectomy was then performed to decompress the posterior spinal canal. After gentle retraction of the dural sac and nerve roots, a rectangular incision was made in the annulus fibrosus of the affected disc, and the nucleus pulposus was meticulously removed. The cartilaginous endplates were thoroughly curetted, and any osseous obstructions were excised. A combination of autologous and artificial bone graft was implanted into the anterior intervertebral space, followed by placement of an interbody fusion device packed with autogenous cancellous bone. After installation of the connecting rods and secure fixation of the locking nuts, the surgical site was copiously irrigated. Two drainage tubes were positioned, vancomycin powder was applied locally, and the incision was closed in anatomical layers and dressed appropriately.22
Statistical Analysis
The Kolmogorov–Smirnov test was employed to assess whether continuous variables followed a normal distribution. An independent t-test was used for comparisons of normally distributed variables, the Mann–Whitney U-test for non-normally distributed variables, and the chi-square test for categorical data. Multivariate logistic regression analysis with backward elimination was performed to evaluate the variables of interest and identify independent risk factors for POD. Receiver operating characteristic (ROC) curves were generated for the candidate parameters, and the area under the curve (AUC) was calculated to evaluate their accuracy and reliability in predicting the occurrence of POD. Statistical analyses were conducted using SPSS software (version 20.0; IBM Corp)., with all tests being two-sided. A p-value < 0.05 was considered indicative of statistical significance.
Results
Patients
The details of 2,333 patients were initially collected, and following a meticulous screening process, 370 patients meeting the study’s criteria were ultimately included, as illustrated in Figure 1. Among these, 61 patients (16.5%) were classified into the POD group, while the remaining 309 patients (83.5%) comprised the non-POD group. As presented in Table 1, the POD group was significantly older than the non-POD group (71.56±4.84 vs 68.96±5.81, p = 0.001), and a higher proportion of patients in the delirium group had a lower BMI (21.10±2.35 vs 21.86±2.36, p = 0.024). Furthermore, the PNI was significantly lower in the POD group compared to the non-POD group (43.02±3.44 vs 48.53±3.72, p < 0.001). Apart from these findings, no significant differences were observed in other demographic or clinical characteristics between the two groups. Table 2 illustrates that preoperative serum albumin levels were markedly lower in the POD group compared to the non-POD group (36.06±5.95 vs 40.50±3.01, p < 0.001). However, no significant differences were observed between the two groups regarding preoperative laboratory values or surgical outcomes, including total cholesterol and hemoglobin levels, operative duration, and intraoperative blood loss.
 |
Table 1 Demographics for Patients |
 |
Table 2 Preoperative Laboratory Data and Operative Outcomes |
 |
Figure 1 Patient Inclusion and Exclusion Flowchart. |
PNI and POD
As shown in Table 3, we included the factors from Tables 1 and 2 with p-values < 0.05 as potential influences on POD in a univariate logistic regression analysis. We identified age (OR: 1.087; 95% CI: 1.032–1.145; p = 0.002), BMI (OR: 0.873; 95% CI: 0.776–0.982; p = 0.024), serum albumin levels (OR: 0.577; 95% CI: 0.497–0.669; p < 0.001), and PNI scores (OR: 0.608; 95% CI: 0.534–0.693; p < 0.001) as significant risk factors for POD. Furthermore, Table 3 illustrates that age (OR: 1.096; 95% CI: 1.030–1.166; p = 0.004), serum albumin levels (OR: 0.759; 95% CI: 0.584–0.987; p = 0.040), and PNI scores (OR: 0.743; 95% CI: 0.597–0.924; p = 0.008) remained significant predictors in the multivariate logistic regression analysis model. As depicted in Figure 2, the predictive value of PNI for POD was evaluated using an ROC curve, revealing an AUC of 0.864 ± 0.025. The cutoff value of PNI, as determined by the Youden index, was 45.825, with a sensitivity of 82.0% and a specificity of 74.4%.
 |
Table 3 Univariate and Multivariate Logistic Regression Analysis |
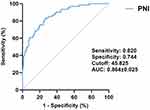 |
Figure 2 ROC curve for GNRI. |
Complications
As presented in Table 4, the complication rate was 14.8% in the delirium group compared to 8.7% in the non-delirium group (p = 0.07). In the delirium group, complications included surgical site skin infection 2 (3.3%), deep venous thrombosis 1 (1.6%), pneumonia 1 (1.6%), urinary tract infection 1 (1.6%), hypokalemia 1 (1.6%), hyponatremia 2 (3.3%), and depression 1 (1.6%). In the non-delirium group, complications included surgical site skin infection 4 (1.3%), deep infection 2 (0.6%), deep venous thrombosis 4 (1.3%), pulmonary embolism 1 (0.3%), pneumonia 4 (1.3%), urinary tract infection 3 (1%), hypokalemia 3 (1%), hyponatremia 4 (1.3%), and depression 2 (0.6%). None of the patients with surgical site infections required surgical intervention, and no cases of deep vein thrombosis progressed to pulmonary embolism.
 |
Table 4 Postoperative Complication Except for Delirium |
Discussion
To date, this is the first study to evaluate the validity of preoperative PNI scores in predicting the occurrence of POD in elderly patients undergoing TLIF. The findings revealed that PNI scores were independent risk factors for the development of POD following TLIF. Specifically, a lower PNI was associated with a higher likelihood of developing POD. Additionally, advanced age and reduced serum albumin levels were similarly identified as significant risk factors for postoperative delirium.
In recent years, the global annual volume of spinal surgeries has surpassed 4.83 million, with the incidence of POD reaching as high as 23–40.5% among elderly patients over 70 years old, particularly those undergoing lumbar fusion procedures.23–25 With healthcare costs related to the management of spinal POD reaching $150 billion annually, early identification of patients at risk is crucial.3 Numerous factors contribute to the development of POD in TLIF, including cerebral oxygen desaturation caused by prone positioning, postoperative glucocorticoid shock, and extensive surgical exposure, which elevates the risk of micro emboli formation and systemic inflammatory responses.3,26,27 In this study, Tables 1 and 2 reveal significant differences between the delirium and non-delirium groups in terms of age, BMI, PNI scores, and serum albumin levels. Logistic regression analyses further highlighted the most critical risk factors for TLIF-associated POD as low PNI, low serum albumin levels, and advanced age, as demonstrated in Table 3. Furthermore, Figure 2 illustrates that the AUC of PNI on the ROC curve is 0.864±0.025, thereby affirming the robustness of its predictive value.
In recent years, numerous studies have confirmed that preoperative malnutrition is a significant contributor to POD, a finding that is consistent with the results of the present study. Tei and Oe highlighted that low preoperative PNI is a significant factor contributing to the occurrence of POD in elderly patients with colorectal cancer and spinal deformities.12,28 In addition, Shin further observed that a preoperative PNI < 50 significantly elevates the risk of POD in patients undergoing orthopedic scoliosis surgery.12 Compared to orthopedic scoliosis surgery, single-segment TLIF surgery is less invasive, involves less blood loss, has a shorter operative duration, and demands lower postoperative nutritional consumption. Therefore, it requires less preoperative nutritional reserve, which further supports the conclusion that a PNI < 45.825 serves as an important risk factor for POD in patients undergoing TLIF. Serum albumin is widely recognized not only as a nutritional indicator but also as a crucial antioxidant in plasma, attributed to its free sulfhydryl groups. In the central nervous system, low serum albumin levels elevate the production of oxygen free radicals, which induces oxidative stress and results in the necrosis of nerve cells.29 Furthermore, Bin discovered that serum albumin promotes the development of POD through the mechanisms involving T-tau and P-tau.30 As a pivotal marker of immune function, lymphocyte count plays a vital role in facilitating postoperative recovery.21 Beyond its immunological significance, lymphocyte count also serves as an indirect indicator of systemic inflammation. The prevailing hypothesis regarding the pathophysiological mechanism of POD centers on neuroinflammation, wherein peripheral cytokines compromise the integrity of the blood-brain barrier, thereby initiating a central inflammatory cascade.6 In this context, the PNI not only reflects preoperative nutritional status via serum albumin levels but also captures inflammatory burden through lymphocyte counts. This dual “nutrition-inflammation” profiling substantially enhances the predictive sensitivity of the PNI in assessing POD risk.14,15 As an independent risk factor, advanced age frequently contributes to the development of POD due to factors such as frailty, a substantial decline in functional reserve and resilience, and reduced cerebral blood flow.8,9 A meta-analysis revealed that up to 21.3% of spinal surgery patients experience POD, with prevalence rates reaching as high as 40% in elderly patients over 70 years of age.8 Therefore, prior to planning the implementation of TLIF, it is essential to give greater attention to elderly patients with malnutrition, enhance preoperative nutritional support, and focus on health education, thereby facilitating more effective postoperative rehabilitation.
There are several shortcomings in this study. Firstly, this was a single-center retrospective study, which may have been influenced by various confounding factors. Therefore, a prospective multicenter study will be necessary in the future to fully validate these findings. Secondly, postoperative outcomes were not analyzed in this study, and further research is needed to explore whether postoperative blood markers contribute to the development of POD, as well as the impact of POD on surgical outcomes. Thirdly, ICD-10 diagnostic codes for POD were not incorporated in the present study. Future investigations should aim to include these diagnostic codes to enhance the methodological rigor and diagnostic precision of the research.
Conclusion
Risk factors for POD in elderly patients with degenerative lumbar spine disease undergoing TLIF include a PNI of less than 45.825, low serum albumin levels, and advanced age. The preoperative use of PNI holds promise as a valuable tool for assessing the risk of POD in elderly patients undergoing TLIF.
Ethical Approval
This study was approved by the Medical Ethics Review Committee of Zhejiang Provincial People’s Hospital (No. QT2025041). Informed consent was not required for this retrospective analysis, as all data were anonymized and devoid of patient identifiers. The institutional ethics committee waived the need for individual consent to access medical records. Throughout the study, patient confidentiality was rigorously maintained in accordance with the Personal Information Protection Act and the principles outlined in the Declaration of Helsinki. Access to raw data was restricted to authorized researchers via the hospital’s encrypted data system, and all analytical outcomes were reported in aggregated form to preclude the identification of individual participants. The study protocol adhered strictly to the ethical tenets of the Declaration of Helsinki governing medical research.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Oh ES, Fong TG, Hshieh TT, et al. Delirium in Older Persons: advances in Diagnosis and Treatment. JAMA. 2017;318(12):1161–1174. doi:10.1001/jama.2017.12067
2. Scholz AF, Oldroyd C, Mccarthy K, et al. Systematic review and meta-analysis of risk factors for postoperative delirium among older patients undergoing gastrointestinal surgery. Br J Surg. 2016;103(2):e21–8. doi:10.1002/bjs.10062
3. Fineberg SJ, Nandyala SV, Marquez-Lara A, et al. Incidence and risk factors for postoperative delirium after lumbar spine surgery. Spine. 2013;38(20):1790–1796. doi:10.1097/BRS.0b013e3182a0d507
4. Pan Z, Huang K, Huang W, et al. The risk factors associated with delirium after lumbar spine surgery in elderly patients. Quant Imag Med Surg. 2019;9(4):700–710. doi:10.21037/qims.2019.04.09
5. Lee JK, Park YS. Delirium after spinal surgery in Korean population. Spine. 2010;35(18):1729–1732. doi:10.1097/BRS.0b013e3181c423fc
6. Glumac S, Kardum G, Sodic L, et al. Effects of dexamethasone on early cognitive decline after cardiac surgery: a randomised controlled trial. Eur J Anaesthesiol. 2017;34(11):776–784. doi:10.1097/EJA.0000000000000647
7. Inouye SK, Westendorp RG, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–922.
8. Shi C, Yang C, Gao R, et al. Risk Factors for Delirium After Spinal Surgery: a Meta-Analysis. World Neurosurg. 2015;84(5):1466–1472. doi:10.1016/j.wneu.2015.05.057
9. Bajaj S, Alkozei A, Dailey NS, et al. Brain Aging: uncovering Cortical Characteristics of Healthy Aging in Young Adults. Front Aging Neurosci. 2017;9:412. doi:10.3389/fnagi.2017.00412
10. Gold C, Ray E, Christianson D, et al. Risk factors for delirium in elderly patients after lumbar spinal fusion. Clin Neurol Neurosurg. 2022;219:107318.
11. Oe S, Yamato Y, Hasegawa T, et al. Association between a prognostic nutritional index less than 50 and the risk of medical complications after adult spinal deformity surgery. J Neurosurg Spine. 2020;33(2):219–224. doi:10.3171/2020.1.SPINE191410
12. Oe S, Togawa D, Yamato Y, et al. Preoperative Age and Prognostic Nutritional Index Are Useful Factors for Evaluating Postoperative Delirium Among Patients With Adult Spinal Deformity. Spine. 2019;44(7):472–478. doi:10.1097/BRS.0000000000002872
13. Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai zasshi. 1984;85(9):1001–1005.
14. Mazzola P, Ward L, Zazzetta S, et al. Association Between Preoperative Malnutrition and Postoperative Delirium After Hip Fracture Surgery in Older Adults. J Am Geriatr Soc. 2017;65(6):1222–1228.
15. Zhang L, Ma W, Qiu Z, et al. Prognostic nutritional index as a prognostic biomarker for gastrointestinal cancer patients treated with immune checkpoint inhibitors. Front Immunol. 2023;14:1219929. doi:10.3389/fimmu.2023.1219929
16. Arevalo-Rodriguez I, Smailagic N, Roqué-Figuls M, et al. Mini-Mental State Examination (MMSE) for the early detection of dementia in people with mild cognitive impairment (MCI). Cochrane Database Syst Rev. 2021;7(7):Cd010783. doi:10.1002/14651858.CD010783.pub3
17. Inouye SK, Van Dyck CH, Alessi CA, et al. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Internal Med. 1990;113(12):941–948. doi:10.7326/0003-4819-113-12-941
18. Mohri Y, Inoue Y, Tanaka K, et al. Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World J Surg. 2013;37(11):2688–2692.
19. Liu JY, Dong HM, Wang WL, et al. The Effect of the Prognostic Nutritional Index on the Toxic Side Effects of Radiochemotherapy and Prognosis After Radical Surgery for Gastric Cancer. Cancer Manage Res. 2021;13:3385–3392. doi:10.2147/CMAR.S301140
20. DL Denny, T Trotter, G Lindseth. Preoperative Nutritional Status and Risk for Subsyndromal Delirium in Older Adults Following Joint Replacement Surgery. Orthopedic Nursing. 2020;39(6):393–394. doi:10.1097/NOR.0000000000000719
21. Hall BM, Geraci TC, Machan JT, et al. Lack of Lymphocyte Recovery After Esophagectomy Predicts Overall and Recurrence-Free Survival. J Surg Res. 2020;246:379–383. doi:10.1016/j.jss.2019.09.010
22. Faldini C, Borghi R, Chehrassan M, et al. Transforaminal lumbar interbody fusion. Eur Spine J. 2017;26(Suppl 3):429–430. doi:10.1007/s00586-017-5288-z
23. Ushida T, Yokoyama T, Kishida Y, et al. Incidence and risk factors of postoperative delirium in cervical spine surgery. Spine. 2009;34(23):2500–2504.
24. Brown CHT, Laflam A, Max L, et al. Delirium After Spine Surgery in Older Adults: incidence, Risk Factors, and Outcomes. J Am Geriatr Soc. 2016;64(10):2101–2108.
25. Kobayashi K, Imagama S, Ando K, et al. Risk Factors for Delirium After Spine Surgery in Extremely Elderly Patients Aged 80 Years or Older and Review of the Literature: japan Association of Spine Surgeons with Ambition Multicenter Study. Global Spine J. 2017;7(6):560–566. doi:10.1177/2192568217700115
26. Deiner S, Chu I, Mahanian M, et al. Prone position is associated with mild cerebral oxygen desaturation in elderly surgical patients. PLoS One. 2014;9(9):e106387. doi:10.1371/journal.pone.0106387
27. Mu DL, Wang DX, Li LH, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care. 2010;14(6):R238. doi:10.1186/cc9393
28. Tei M, Wakasugi M, Kishi K, et al. Incidence and risk factors of postoperative delirium in elderly patients who underwent laparoscopic surgery for colorectal cancer. Int J Colorectal Dis. 2016;31(1):67–73.
29. Allen SJ, Watson JJ, Shoemark DK, et al. GDNF, NGF and BDNF as therapeutic options for neurodegeneration. Pharmacol Ther. 2013;138(2):155–175.
30. Wang B, Xin Y, Tang X, et al. Potential value of serum prealbumin and serum albumin in the identification of postoperative delirium in patients undergoing knee/Hip replacement: an observational study and internal validation study. Front Neurol. 2024;15:1375383. doi:10.3389/fneur.2024.1375383
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

