Back to Journals » Neuropsychiatric Disease and Treatment » Volume 21
Prevalence and Associated Factors of Depression in Patients with Ischaemic Stroke: A Cross-Sectional Study
Authors Li Y, Qin W, Chen Y, Zhang D, Zhao Y
Received 24 December 2024
Accepted for publication 31 March 2025
Published 14 April 2025 Volume 2025:21 Pages 875—883
DOI https://doi.org/10.2147/NDT.S514184
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yu-Ping Ning
Yifan Li,1,* Wei Qin,1,* Yitong Chen,2 Dongli Zhang,1 Yongchen Zhao1
1Department of Integrative Traditional Chinese and Western Medicine, Affiliated Hospital of Hebei University, Baoding, Hebei, People’s Republic of China; 2Clinical Specialty of Integrated Chinese and Western Medicine, Hebei University, Baoding, Hebei, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Dongli Zhang; Yongchen Zhao, Department of Integrative Traditional Chinese and Western Medicine, Affiliated Hospital of Hebei University, No. 212 Yuhua East Road, Baoding City, Hebei Province, 071000, People’s Republic of China, Tel +86 0312 5981919, Email [email protected]; [email protected]
Objective: To investigate the prevalence and severity of depression in patients with ischaemic stroke and identify its associated factors using a cross-sectional design over a 6-month period.
Methods: This cross-sectional study included 499 patients with ischaemic stroke who met the diagnostic and inclusion criteria. Depression levels were assessed using the Hamilton Depression Rating Scale (HAMD). Data collection included demographic variables, clinical data and self-reported measures. Neurological deficits were assessed using the National Institutes of Health Stroke Scale (NIHSS), whereas activities of daily living (ADL) were evaluated using the ADL scale. Chi-squared tests and t-tests were used to compare the mild and moderate depression groups. Multiple logistic regression identified independent predictors of depression. The predictive effectiveness of risk factors was evaluated using receiver operating characteristic (ROC) curves.
Results: Of the 499 patients, 305 (61.1%) had mild depression and 194 (38.9%) had moderate depression, with a mean HAMD score of 15.27 ± 6.43. Significant differences were observed between groups in hypertension (p < 0.001), diabetes mellitus (p < 0.001), education level (p < 0.001), stroke location (p = 0.037), ADL score (p < 0.001) and NIHSS score (p < 0.001). Logistic regression identified hypertension (odds ratio [OR] = 1.963), diabetes mellitus (OR = 4.126), lower education level (OR = 1.460), left-sided stroke (OR = 1.690), lower ADL scores (OR = 0.718) and higher NIHSS scores (OR = 1.213) as independent predictors of depression. The ROC analysis showed that NIHSS (area under the curve [AUC] = 0.797) and ADL (AUC = 0.741) scores were the most effective predictors.
Conclusion: Depression is common among patients with ischaemic stroke and is substantially influenced by vascular risk factors, education level, stroke location, daily living abilities and neurological deficits. The NIHSS and ADL scores demonstrated strong predictive value in identifying patients at risk of depression.
Keywords: stroke, depression, multiple logistic regression
Introduction
Post-stroke depression (PSD) is a common complication of stroke. Patients with depression may present with low mood, retardation of thought, self-accusation and self-incrimination. Post-stroke depression may worsen patients’ mental distress, aggravate their physical symptoms, delay functional recovery and increase the risk of recurrent stroke and death, imposing a heavy burden on their families and society.1,2
It has been reported that the prevalence of PSD ranges from 20% to 79% (mostly 40%–50%) in global populations, with severe depression accounting for approximately 10%. This statistic reflects the proportion of existing PSD cases observed in diverse geographic regions and populations.3,4 In addition to affecting patients’ emotions, depression can impair cognitive function and reduce treatment compliance, all of which may have adverse effects on neurological recovery and prognosis.5–8 A prior meta-analysis also documented that PSD was associated with long-term functional impairment and increased mortality.9
Studies have shown that optimised strategies such as transcranial magnetic stimulation, ketamine and electroconvulsive therapy can help treat varying degrees of depression.10,11 Esketamine nasal spray and psilocybin have also shown potential for treating treatment-resistant depression.12 Early identification and the prevention of PSD are also required in clinical practice. At present, the lack of unified diagnostic criteria for PSD results in a high risk of misdiagnosis or missed diagnosis, which may adversely affect clinical treatment and prognosis. Further clarification of the degree of depression and its associated factors in patients with PSD, along with the identification of relevant correlations, may contribute to better management and the mitigation of PSD progression.13
Post-stroke depression is a multifactorial disease with a complex pathogenesis, involving neuroanatomy, neuroendocrinology and immunomodulation.14,15 According to a recent report, the occurrence of PSD may be attributed to inflammatory reactions, changes in neural plasticity and neurotransmitter imbalances.16 Previous studies have identified various factors associated with PSD, including vascular risk factors (eg hypertension, diabetes mellitus),17 demographic factors (eg age, gender, marital status),18 stroke characteristics (eg lesion location, stroke severity)19 and psychosocial factors (eg lack of social support).20 Chronic conditions, such as hypertension and diabetes mellitus, are believed to contribute to PSD by inducing cerebrovascular damage.
A notable association has been observed between right hemispheric stroke and the incidence of depression in the subacute phase following stroke. These findings highlight the multifactorial nature of PSD and the necessity of evaluating multiple variables when studying its occurrence and severity. Although considerable attention has been given to the incidence and influencing factors of PSD,21,22 few studies have examined factors affecting depression severity in patients with stroke.
This cross-sectional study assesses the prevalence of depression among patients with ischaemic stroke, compares clinical characteristics across different levels of depression and identifies independent factors associated with depression severity. It aims to serve as a reference for the early identification, comprehensive prevention and treatment and prognosis evaluation of PSD.
Although the literature extensively covers factors associated with the development of PSD, there is a relative scarcity of research that prospectively examines variables linked to depression severity in the acute and subacute phases after stroke. Furthermore, the interplay between specific clinical characteristics and their differential impact on varying degrees of depression remains largely under-investigated. This study addresses these gaps by prospectively evaluating the incidence of depression in patients with ischaemic stroke, comparing the clinical characteristics of patients with different degrees of depression and screening for independent influencing factors on the degree of depression in these patients. It aims to provide a reference for the early identification, comprehensive prevention and treatment, and prognosis evaluation of PSD.
Materials and Methods
Study Participants
This cross-sectional study determined the required sample size based on an estimated prevalence of PSD of 40%, as reported in previous studies, with a margin of error of 5% and a confidence level of 95%. Using these parameters, the minimum sample size was calculated to be 369 participants. To account for potential dropouts and ensure sufficient statistical power, 499 consecutive patients with ischaemic stroke were included. These patients were hospitalised in the Department of Integrated Traditional Chinese and Western Medicine at the Affiliated Hospital of Hebei University between October 2016 and December 2018. All the patients received standardised treatment, including antiplatelet therapy, lipid-lowering agents, neurotrophic support and interventions to improve blood circulation. Treatment protocols remained largely consistent across groups.
Inclusion Criteria
Patients were included in the study based on the following criteria: (1) patients aged ≥18 years; (2) patients diagnosed with acute ischaemic stroke through cranial computed tomography (CT) or magnetic resonance imaging (MRI);23 (3) patients with an onset time of ≤2 weeks and a stable condition; and (4) patients who provided written informed consent.
Exclusion Criteria
The following criteria were used to exclude patients from the study: (1) patients with malignant tumours in the intracranial or extracranial regions; (2) patients with severe infections or metabolic disorders; (3) patients with a history of mental illness (eg major depressive disorder, bipolar disorder, schizophrenia or anxiety disorders) or those taking antidepressants, as these conditions could confound the assessment of PSD; and (4) patients with aphasia or consciousness disorders that prevented meaningful participation in the assessment.
Ethical Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the Affiliated Hospital of Hebei University (No. HDFYLL-KY-2023-137). Written informed consent was obtained from all patients or their guardians before participation.
Methods of Study
Stroke-related assessments using the National Institutes of Health Stroke Scale (NIHSS) and the activities of daily living (ADL) scale were conducted upon admission to evaluate initial stroke severity and functional capacity. Depression assessments using the Hamilton Depression Rating Scale (HAMD) were completed within 2 weeks of stroke onset during hospitalisation, ensuring clinical stability.
Data collection: A customised questionnaire was developed to collect baseline data from all patients, including gender, age, marital status, level of education and vascular risk factors. The presence of hypertension, diabetes mellitus, coronary heart disease and dyslipidaemia was determined based on patients’ medical history or the clinical diagnoses made by their treating physicians.
Stroke-related assessment: Stroke type was identified based on cranial CT or MRI findings. Only patients with ischaemic stroke were included in this study. Stroke severity was assessed using the NIHSS,24 which has a total score range of 0–42 points, with higher scores indicating more severe neurological deficits. The level of functional independence was evaluated using the Barthel index,25 which has a total score range of 0–100 points. Higher ADL scores indicate greater functional independence, with scores ≥60 generally reflecting moderate to good functional ability, whereas scores <60 suggest substantial dependence in daily activities.26
Depression assessment: The degree of depression in the enrolled patients was assessed using the HAMD-17.21 The total score ranged from 0 to 54 points, with 7–17 points indicating mild depression, 18–24 points indicating moderate depression and >24 points indicating severe depression. Patients were divided into mild and moderate depression groups based on their HAMD-17 scores.
Statistical analysis: SPSS 22.0 software (IBM, Armonk, NY, USA) was used for statistical analysis. Measurement data were expressed as mean ± standard deviation, whereas categorical data were presented as counts (percentages). All continuous variables were tested for normality using the Shapiro–Wilk test before applying parametric statistical methods. The results indicated that the data followed a normal distribution. Inter-group comparisons were performed using the t-test for continuous variables and the χ²-test for categorical variables. Variables with statistically significant differences in univariate analysis were included in multiple logistic regression analysis to identify independent influencing factors of depression.
Additionally, receiver operating characteristic (ROC) curve analysis was used to assess the predictive effectiveness of the independent influencing factors identified through logistic regression. The area under the curve (AUC) and 95% confidence interval (CI) were calculated for each factor to determine its discriminatory ability, with higher AUC values indicating better predictive performance. A p-value of <0.05 was considered statistically significant.
Results
Sample Characteristics and Comparison of General and Clinical Data in Patients with Different Degrees of Depression
A total of 499 patients with ischaemic stroke were included in this study, comprising 203 men (40.68%) and 296 women (59.32%), with a mean age of 67.35 ± 11.42 years. The average HAMD score of the included patients was 15.27 ± 6.43 points. Among them, 305 patients (61.12%) had mild depression and 194 (38.88%) had moderate depression, as shown in Table 1.
 |
Table 1 Comparison of General Data and Clinical Characteristics of Patients with Different Degrees of Depression [n (%)] |
No statistically significant differences were observed between the two groups in terms of gender and stroke type (p > 0.05). However, significant differences were found in age, marital status, level of education, hypertension, diabetes mellitus, coronary heart disease, hyperlipidaemia and stroke location (p < 0.05 for all). By contrast, stroke onset time did not differ significantly between the groups (9.67 ± 2.34 vs 9.67 ± 2.26 days, p = 0.999). Patients in the moderate depression group had higher NIHSS scores and lower ADL scores than those in the mild depression group, with statistically significant differences (p < 0.05 for both).
Multiple Logistic Regression Analysis of Depression in Patients with Ischaemic Stroke
In this study, variables that reached statistical significance (p < 0.05) in the univariate analysis were included in the multivariable logistic regression model. This approach ensured that only the most relevant associated factors were retained. The results of the univariate analysis are provided in Table 1 to illustrate the relationships between variables before multivariable analysis.
Before conducting logistic regression, we confirmed that its assumptions were met, including the absence of significant multicollinearity, as indicated by the variance inflation factors below 5. The linearity of continuous independent variables with the logit of the outcome was assessed using the Box–Tidwell test, which showed no significant deviations. Additionally, Cook’s distance analysis revealed no influential outliers affecting the model. The logistic regression model was statistically significant, as indicated by the Omnibus test (χ²= 127.36, p < 0.001), and the Nagelkerke R²value was 0.328, suggesting that the model explained 32.8% of the variance in depression severity.
As shown in Table 2, hypertension (odds ratio [OR] = 1.963, 95% CI: 1.333–2.890, p = 0.001), diabetes mellitus (OR = 4.126, 95% CI: 2.774–6.136, p < 0.001), level of education (OR = 1.460, 95% CI: 1.267–1.683, p < 0.001), left hemispheric stroke (OR = 1.690, 95% CI: 1.126–2.539, p = 0.011), ADL score (OR = 0.718, 95% CI: 0.574–0.899, p = 0.004) and NIHSS score (OR = 1.213, 95% CI: 1.108–1.328, p < 0.001) were identified as independent influencing factors of PSD.
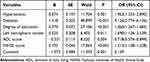 |
Table 2 Multivariate Logistic Regression Analysis of Influential Factors of Depression in Patients with Ischemic Stroke |
Receiver Operating Characteristic Curve Analysis
The ROC curve analysis was performed to assess the predictive effectiveness of the identified risk factors for depression in patients with ischaemic stroke. The results are summarised in Table 3 and illustrated in Figure 1.
 |
Table 3 Receiver-Operating Curve Analysis of Influential Factors for Predicting Moderate Depression in Patients with Ischemic Stroke |
 |
Figure 1 ROC Curve Analysis of Key Risk Factors for Depression in Ischaemic Stroke Patients. |
Among the variables analysed, the NIHSS score demonstrated the highest predictive value, with an AUC of 0.797 (95% CI: 0.759–0.832, p < 0.001), indicating excellent discrimination. The ADL score also demonstrated strong predictive ability, with an AUC of 0.741 (95% CI: 0.700–0.778, p < 0.001). Other factors, including diabetes mellitus (AUC = 0.668, 95% CI: 0.625–0.709, p < 0.001) and education level (primary school and below) (AUC = 0.638, 95% CI: 0.594–0.681, p < 0.001), demonstrated moderate predictive effectiveness. Hypertension (AUC = 0.584, 95% CI: 0.540–0.628, p < 0.001) and left hemispheric stroke (AUC = 0.557, 95% CI: 0.512–0.601, p = 0.032) demonstrated relatively weak predictive performance.
Discussion
In this study, patients with ischaemic stroke exhibited a high incidence of depression (HAMD score of 15.27 ± 6.43 points), with mild and moderate depression accounting for 61.12% and 38.88% of cases, respectively. This highlights the necessity of clinical screening and diagnosis of depression in patients with stroke.
Multiple logistic regression in this study indicated that vascular conditions such as hypertension and diabetes mellitus were significantly associated with PSD. More specifically, chronic diseases such as hypertension and diabetes mellitus can induce cerebrovascular lesions, damaging the white matter and cortex, thus affecting emotion-related brain regions and inducing depression.27 Several existing studies have confirmed the importance of managing these vascular risk factors in preventing stroke and improving prognosis.28–30 Moreover, depression may be induced by physical and mental stress as well as lifestyle changes in patients with long-term chronic diseases. This highlights the importance of aggressive management of hypertension and diabetes mellitus in patients with stroke, not only to prevent recurrent stroke but also to reduce the risk of developing PSD. The regular monitoring of blood pressure and glucose levels, coupled with lifestyle interventions and appropriate medication, should be a standard part of post-stroke care.
Furthermore, our study revealed a positive correlation between the level of education and PSD. Patients with a higher level of education had a greater risk of depression. This may be because highly educated patients have higher levels of disease awareness and greater concern about prognosis and recurrence risk, both of which may increase psychological pressure.31 In addition, because of high levels of work-related stress, highly educated patients may experience a reduced ability to work and disrupted social activities caused by stroke-induced functional impairment, which in turn increases the risk of depression. As a result, psychological counselling should be considered for patients with a higher level of education to help alleviate their psychological pressure.
Left hemispheric stroke was found to be significantly associated with depression. It is speculated that the left hemisphere is dominant in emotional processing, and its impairment may cause emotional dysregulation and, hence, increase the risk of depression.19,32–34 Damage to the left cerebral hemisphere is thought to be associated with depression, with a higher incidence observed in cases involving the left frontal cortex and the left basal ganglia. The underlying mechanism is that 5-HT and NE are more easily depleted in the left cerebral hemisphere than in the right, and damage to the NE and 5-HTergic neuronal pathways in these regions reduces NE and 5-HT levels, leading to PSD.35
Some promising intervention strategies, such as deep transcranial magnetic stimulation, continuous theta burst stimulation and Stanford neuromodulation therapy, have shown potential antidepressant effects in patients with depression.36–38 In addition, special attention should be given to screening patients with left hemispheric stroke, with early psychological intervention applied to mitigate the risk of depression. These findings underscore the need for routine depression screening in patients with left hemispheric strokes. Moreover, they support the exploration and implementation of neuromodulation therapies alongside traditional psychological interventions for this specific patient population.
Furthermore, the degree of PSD was positively correlated with the severity of neurological deficits and negatively correlated with ADL.35,39 Patients with more severe neurological damage may have a higher degree of dependence in daily life activities, leading to increased physical and mental strain and a higher risk of depression. Therefore, in post-stroke rehabilitation, personalised rehabilitation programmes should be adopted to encourage patient engagement, improve ADL and promote social participation, thereby reducing the occurrence of depression. This highlights the importance of comprehensive rehabilitation programmes that focus not only on physical recovery but also on improving ADL and fostering social engagement. Early and intensive rehabilitation efforts, tailored to individual patient needs, can help mitigate the risk of depression by fostering independence and improving quality of life.
However, this study has several limitations. First, it was a single-centre study with a relatively small sample size, which may limit the generalisability of the findings. The consecutive enrolment of participants could introduce selection bias, as it may not fully represent the broader population of patients with ischaemic stroke. Future multicentre studies with larger sample sizes are needed to validate these results and enhance generalisability. Second, the cross-sectional design of this study prevented the examination of changes in depression at different stages of stroke recovery. Third, the HAMD was used to assess depression. Although widely utilised, the HAMD is a clinician-administered scale that relies on subjective interpretation and may be influenced by observer bias. Additionally, it may not fully capture the nuances of depressive symptoms experienced by patients with stroke, potentially leading to an under- or overestimation of depression severity. Future studies should consider incorporating self-report measures and qualitative assessments to provide a more comprehensive understanding of PSD. Finally, this study did not investigate the impact of post-stroke cognitive impairment on depression, which warrants further exploration in future research.
Conclusion
This study reports a high incidence of PSD and identifies factors associated with vascular conditions, level of education, stroke location, neurological deficits and ADL. The findings suggest that personalised psychological interventions and rehabilitation tailored to patients with these factors may help support their physical and mental well-being and improve their quality of life. Additionally, a dynamic assessment of depression in patients with stroke is essential for the early identification and timely implementation of preventive and therapeutic strategies for PSD.
Funding
Effect of blood biochemical index monitoring on TCM syndrome distribution and prognosis in patients with mild cognitive impairment (Project number: 2024069).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Feng XY, Shen TT, Wu QC. et al. A novel approach to treating post-stroke depression: administration of Botulinum Toxin A via local facial injection. Front Neurol. 2024;15:1372547. doi:10.3389/fneur.2024.1372547
2. Das J, Rajanikant GK. Post stroke depression: the sequelae of cerebral stroke. Neurosci Biobehav Rev. 2018;90:104–114. doi:10.1016/j.neubiorev.2018.04.005
3. Wu Y, Deng J, Ma J, et al. Unraveling the pathogenesis of post-stroke depression in a hemorrhagic mouse model through frontal lobe circuitry and JAK-STAT Signaling. Adv Sci (Weinh). 2024;1:e2402152.
4. Suñer-Soler R, Maldonado E, Rodrigo-Gil J, et al. Sex-related differences in post-stroke anxiety, depression and quality of life in a cohort of smokers. Brain Sci. 2024;14(6):521. doi:10.3390/brainsci14060521
5. Ortiz GA, Sacco RL. National Institutes of Health Stroke Scale (NIHSS)[M]//Wiley StatsRef: statistics Reference Online. 2014.
6. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–709. doi:10.1016/0895-4356(89)90065-6
7. Hamilton M. Development of a rating scale for primary depressive illness. British J Soc Clin Psychol. 1967;6(4):278–296. doi:10.1111/j.2044-8260.1967.tb00530.x
8. Backhouse EV, Mchutchison CA, Cvoro V, et al. Cognitive ability, education and socioeconomic status in childhood and risk of post-stroke depression: a systematic review and meta-analysis. PLoS One. 2018;13(7):e0200525. doi:10.1371/journal.pone.0200525
9. Ayerbe L, Ayis S, Wolfe CD, et al. Natural history, predictors and outcomes of depression after stroke: systematic review and meta-analysis. Br J Psychiatry. 2013;202(1):14–21. doi:10.1192/bjp.bp.111.107664
10. Huang XB, Zheng W. Ketamine and electroconvulsive therapy for treatment-refractory depression. Alpha Psychiatry. 2023;24(6):244–246. doi:10.5152/alphapsychiatry.2023.231358
11. Wen KS, Zheng W. Optimization strategies of transcranial magnetic stimulation in major depressive disorder. Alpha Psychiatry. 2023;24(6):270–272. doi:10.5152/alphapsychiatry.2023.231401
12. Yuan S, Luo X, Zhang B. Individualized repetitive transcranial magnetic stimulation for depression based on magnetic resonance imaging. Alpha Psychiatry. 2023;24(6):273–275. doi:10.5152/alphapsychiatry.2023.231412
13. Richter D, Ebert A, Mazul L, et al. Brainstem raphe hypoechogenicity is an independent predictor of post-stroke depression. Ultraschall Med. 2024. doi:10.1055/a-2296-3484
14. Chang X, He Y, Liu Y, et al. Serum brain derived neurotrophic factor levels and post-stroke depression in ischemic stroke patients. J Affect Disord. 2024;17:
15. Fang C, Zhang Z, Xu H, et al. Natural products for the treatment of post-stroke depression. Front Pharmacol. 2022;13:918531. doi:10.3389/fphar.2022.918531
16. Wang Z, Y SHI, F LIU, et al. Diversiform etiologies for post-stroke depression. Frontiers in Psychiatry. 2019;9:761. doi:10.3389/fpsyt.2018.00761
17. Amytis T, Bruce O, Nada EH, et al. Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American stroke association. Stroke. 2016;48(1):2. doi:10.1161/STROKEAHA.116.015868
18. Shi Y, Yang D, Zeng Y, et al. Risk factors for post-stroke depression: a meta-analysis. Front Aging Neurosci. 2017;9:218. doi:10.3389/fnagi.2017.00218
19. Wei N, Yong W, Li X, et al. Post-stroke depression and lesion location: a systematic review. J Neurol. 2015;262(1):81–90. doi:10.1007/s00415-014-7534-1
20. Bi H, Wang M. Role of social support in poststroke depression: a meta-analysis. Frontiers in Psychiatry. 2022;13:924277. doi:10.3389/fpsyt.2022.924277
21. Zhang N, Song JG, J GUR, et al. Correlation study of event-related potentials and monoamine neurotransmitter levels in patients with post-stroke depression. Chin J Pract Diagnosis Ther. 2012;26(12):(in Chinese).1177–1179.
22. Towfighi A, Ovbiagele B, Husseini ELN, et al. Poststroke depression: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48(2):e30–e43. doi:10.1161/STR.0000000000000113
23. Chinese Society of Neurology, Chinese Stroke Society. Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2023. Chin J Neurol. 2024;57(06):523–559.
24. Bruno A, Saha C, Williams LS. Percent change on the National Institutes of Health Stroke Scale: a useful acute stroke outcome measure. J Stroke Cerebrovasc Dis. 2009;18(1):56–59. doi:10.1016/j.jstrokecerebrovasdis.2008.09.002
25. Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: a reliability study. Int Disabil Stud. 1988;10(2):61–63. doi:10.3109/09638288809164103
26. Nakao S, Takata S, Uemura H, et al. Relationship between Barthel Index scores during the acute phase of rehabilitation and subsequent ADL in stroke patients. J Med Invest. 2010;57(1–2):81–88. doi:10.2152/jmi.57.81
27. Medeiros GC, Roy D, Kontos N, et al. Post-stroke depression: a 2020 updated review. General Hospital Psychiatry. 2020;66:70–80. doi:10.1016/j.genhosppsych.2020.06.011
28. Guzik A, Bushnell C. Stroke epidemiology and risk factor management. Continuum. 2017;23(1):15–39.
29. Hu D, Sun Y. Epidemiology, risk factors for stroke, and management of atrial fibrillation in China. Journal of the American College of Cardiology. 2008;52(10):865–868. doi:10.1016/j.jacc.2008.05.042
30. Rundek T, Sacco RL. Risk factor management to prevent first stroke. Neurol Clinics. 2008;26(4):1007–1045. doi:10.1016/j.ncl.2008.09.001
31. DE RYCK A, Brouns R, Geurden M, et al. Risk factors for poststroke depression: identification of inconsistencies based on a systematic review. J Geriatric Psychiatry Neurol. 2014;27(3):147–158. doi:10.1177/0891988714527514
32. X LUO, Fang W, Ji J, et al. Association of lesion location with post-stroke depression in China: a systematic review and meta-analysis. EC Psychol Psychiatry. 2023;12(3):34–45.
33. Li J, Oakley LD, Li Y, et al. Development and initial validation of a clinical measure to assess early symptoms of post-stroke depression in the acute stroke patient. J Clin Nurs. 2018;27(3–4):784–794. doi:10.1111/jocn.14099
34. Chen J, Liu J, Zeng Y, et al. Development and initial validation of a clinical measure to assess symptoms of post-stroke depression in stroke patients at the rehabilitation stage. Frontiers in Psychology. 2022;13:928257. doi:10.3389/fpsyg.2022.928257
35. Zhan Q, Kong F. Mechanisms associated with post-stroke depression and pharmacologic therapy. Front Neurol. 2023;14:1274709. doi:10.3389/fneur.2023.1274709
36. Lan XJ, Yang XH, Mo Y, et al. Deep transcranial magnetic stimulation for treatment-resistant depression: a systematic review and meta-analysis of randomized controlled studies. Asian J Psychiatr. 2024;96:104032. doi:10.1016/j.ajp.2024.104032
37. Cai DB, Qin XD, Qin ZJ, et al. Adjunctive continuous theta burst stimulation for major depressive disorder or bipolar depression: a meta-analysis of randomized controlled studies. J Affect Disord. 2024;1(346):266–272. doi:10.1016/j.jad.2023.10.161
38. Lan XJ, Cai DB, Liu QM, et al. Stanford neuromodulation therapy for treatment-resistant depression: a systematic review. Front Psychiatry. 2023;14:1290364. doi:10.3389/fpsyt.2023.1290364
39. Butsing N, Zauszniewski JA, Ruksakulpiwat S, et al. Association between post-stroke depression and functional outcomes: a systematic review. PLoS One. 2024;19(8):e0309158. doi:10.1371/journal.pone.0309158
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
The Psychological Impact of Quarantine During the COVID-19 Pandemic on Quarantined Non-Healthcare Workers, Quarantined Healthcare Workers, and Medical Staff at the Quarantine Facility in Saudi Arabia
Alfaifi A, Darraj A, El-Setouhy M
Psychology Research and Behavior Management 2022, 15:1259-1270
Published Date: 17 May 2022
Depression and Associated Risk Factors Among Type 2 Diabetic Patients: A Cross Sectional Study on a Convenience Sample from the Diabetic Center, Khamis Mushait; Saudi Arabia
Abuhegazy H, Mujairi A, Banah F, Agdi Y, Elkeshishi H, Kamel A, Abdullah A, Elsheikh M
Neuropsychiatric Disease and Treatment 2022, 18:1975-1984
Published Date: 31 August 2022
Association Between Breakfast Consumption and Suicidal Attempts in Adolescents
Park H, Lee K
Psychology Research and Behavior Management 2022, 15:2529-2541
Published Date: 13 September 2022
Sex Differences in Stroke Risk Factors, Clinical Profiles, and In-Hospital Outcomes Among Stroke Patients Admitted to the Medical Ward of Dessie Comprehensive Specialized Hospital, Northeast Ethiopia
Abdu H, Seyoum G
Degenerative Neurological and Neuromuscular Disease 2022, 12:133-144
Published Date: 21 October 2022
Knowledge of Cardiovascular Disease Risk Factors and Its Primary Prevention Practices Among the Saudi Public – A Questionnaire-Based Cross-Sectional Study
Bashatah A, Syed W, Al-Rawi MBA
International Journal of General Medicine 2023, 16:4745-4756
Published Date: 20 October 2023

