Back to Journals » Infection and Drug Resistance » Volume 17
Prevalence and Genotype Distribution of Human Papillomavirus Infection Among Women in Wuhan, China: A Retrospective Study
Authors Wang D , Yan X, Yang L, Zhang L
Received 27 May 2024
Accepted for publication 19 August 2024
Published 24 August 2024 Volume 2024:17 Pages 3677—3688
DOI https://doi.org/10.2147/IDR.S471176
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Dong Wang,* Xinsheng Yan,* Luo Yang, Litao Zhang
Department of Clinical Laboratory, Wuhan Asia General Hospital, Wuhan Asia General Hospital Affiliated to Wuhan University of Science and Technology, Wuhan, 430056, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Dong Wang; Litao Zhang, Email [email protected]; [email protected]
Purpose: Human papillomavirus (HPV) infection is a prevalent sexually transmitted infection worldwide, with its persistence being a significant factor in the development of cervical cancer and precancerous lesions. Understanding the prevalence and genotypes distribution of HPV can aid in the implementation of more focused strategies for cervical cancer prevention and treatment. This study aimed to investigate the prevalence and genotype distribution of HPV infection among outpatient-based populations in Wuhan, China.
Methods: Our study retrospectively analyzed the results of cervical HPV screening in 14,492 outpatient women. The cervicovaginal infection of 18 high-risk genotypes and 10 low-risk genotypes were analyzed by PCR and reverse dot hybridization techniques.
Results: The overall prevalence of HPV infection in the outpatient female population was 15.33%, with a predominance of single infection and a predominance of dual infection among multiple infections. The top five genotypes in terms of prevalence of HR-HPV and LR-HPV were HPV-52 (3.77%), 53 (1.46%), 16 (1.31%), 58 (1.19%), 39 (1.18%) for HR-HPV, and HPV-54 (1.23%), 61 (1.08%), 81 (1.04%), 42 (0.87%), 44 (0.70%) for LR-HPV. Two peaks of HPV infection prevalence were observed among women under 25 years (22.88%) and over 56 years (24.26%). The prevalence and genotype distribution of HPV infection varied among different outpatient populations, with higher rates of HPV single infection, multiple infections, and infection across all ages observed in the gynecology outpatient population compared to the health check-up population.
Conclusion: This study revealed the HPV prevalence and genotype distribution among different outpatient populations in Wuhan city, which may provide guidance for HPV vaccination and cervical cancer prevention strategies in the region.
Keywords: human papillomavirus, prevalence, genotype, high-risk HPV, low-risk HPV, cervical cancer
Introduction
Cervical cancer is a prevalent malignant tumor that significantly impacts women’s health worldwide, ranking fourth among cancer-related causes of mortality in women.1,2 The primary cause of cervical cancer and its precancerous lesions is persistent infection with human papillomavirus (HPV),3 which can also lead to high-grade lesions and invasive carcinomas in various areas such as the vagina, vulva, and perianal region.3,4 In 2020, there were around 604,000 new cases and 342,000 deaths attributed to cervical cancer worldwide, with a substantial majority occurring in low- and middle-income countries.1 Notably, China, bearing a heavy burden of cervical cancer cases, was projected to experience 109,000 new cases and 59,000 deaths in 2020, with incidence rates continuing to rise.5 Despite significant attention from the Chinese government towards prevention and control efforts, there remains a considerable gap in achieving the goal of eradicating cervical cancer, particularly due to limited HPV vaccine coverage.6 Presently, cervical cancer prevention and control in China primarily rely on screening, with HPV testing/cytology, colposcopy, and histological biopsy being the common “three-step” screening methods.7,8 Cervical exfoliative cytology and human papillomavirus (HPV) nucleic acid testing are currently available in most regions of China, and these screening methods are widely practiced in local medical institutions. The “Guidelines for Cervical Cancer Screening in China” recommend that women begin screening at age 25. Women aged 25 to 64 years should undergo HPV nucleic acid testing alone or HPV testing in combination with cytology every five years, or cytology alone every three years.9 Additionally, women aged 65 years or older may discontinue screening if there is a sufficient record of previous negative screening results. HPV genotyping, offering enhanced sensitivity, reproducibility, and cost-effectiveness compared to cytology, plays a crucial role in reducing the burden of cervical cancer and other HPV-related diseases.7
Most HPV infections are transient and typically cleared or suppressed by the body’s immune mechanisms within 1–2 years. However, a small number of persistent infections can progress to pre-cancerous lesions and eventually lead to cancer development.10,11 There are over 200 identified HPV genotypes, categorized as high-risk (HR) or low-risk (LR) based on their association with malignant lesions.12,13 Invasive cervical carcinogenesis is largely attributed to persistent infection with HR-HPV, with HPV-16 and HPV-18 accounting for approximately 70% of cervical cancer cases.14,15 Globally, the prevalence of HPV in women with normal cervical cytology is around 10.5%, with a slightly lower rate of 8% in Asia.11 A study conducted in mainland China revealed an overall HR-HPV prevalence of 19.0% among women, with the most common subtypes being 16, 52, 58, 53, and 18.16 However, the prevalence and genotype distribution of HPV are region-specific and age-specific. In addition, the prevalence and genotype distribution of HPV infection vary among different populations. Consequently, our study investigates the epidemiological characteristics of HPV infection in outpatient populations, including those attending gynecological outpatient clinics and medical examination centers. A significant portion of the gynecological outpatient population suffers from conditions such as vaginitis and cervicitis, rendering them more susceptible to HPV infection due to compromised local resistance in the genital tract. Therefore, it is crucial to examine the prevalence and genotype distribution of HPV infection in the outpatient population of the region before the implementation of mass HPV vaccination. This investigation will aid in establishing the genotype profile of HPV infection and in developing an optimal vaccine protection strategy tailored to specific target populations. Additionally, it will contribute to a more comprehensive assessment of the epidemiological characteristics of HPV infection. With a population of more than 14 million in Wuhan, China, there are few studies in the region on 28 HPV genotyping tests and their infection profiling based on cervical cells from outpatient female populations, including gynecology clinics and physical examination centers.
Our study retrospectively analyzed the screening results of 28 HPV genotypes in cervical cells of 14,492 outpatient women from gynecological outpatient clinics and medical examination centers. By analyzing the infection characteristics of various outpatient populations, we aimed to understand the distribution of HPV genotypes and the current infection status among specific female populations in the region, and to provide a more scientific basis for cervical cancer screening, early prevention and treatment strategies and vaccination in the region.
Materials and Methods
Study Participants
A total of 14,492 women from Wuhan, ranging in age from 15 to 81 years, were included in this study. These women visited the outpatient clinic of Wuhan Asia General Hospital between September 2020 and December 2023. Cervical exfoliated cell samples were collected from all participants to detect 28 different types of HPV genotypes. The women were categorized into two groups based on their reason for consultation: 7070 cases in the gynecology clinic group and 7422 cases in the physical examination center group. Furthermore, the participants were divided into eight age groups: ≤ 25 years old, 26–30 years old, 31–35 years old, 36–40 years old, 41–45 years old, 46–50 years old, 51–55 years old, and ≥ 56 years old. The inclusion criteria included: (1) was living in Wuhan city; (2) no intravaginal medication or vaginal douching within 72 hours; (3) abstaining from sexual intercourse within 24 hours; (4) was willing to undergo cervical HPV screening. The exclusion criteria were as follows: (1) during menstrual period; (2) pregnant women; (3) history of hysterectomy; (4) suffering from cancer and having undergone radiation therapy and chemotherapy.
Instruments and Reagents
The PCR amplifier model SLAN 96S (Shanghai Hongshi Medical Technology Co., Ltd)., the automatic nucleic acid extractor model ANDiS350 (Shanghai Sidi Biomedical Technology Co., Ltd)., the nucleic acid hybridiser model HS2400 and the ACME2400 Integrated Nucleic Acid Workstation (Guangzhou Heshi Biotechnology Co., Ltd)., the Thermo Cell thermostatic metal bath (Hangzhou BORI Science and Technology Co., Ltd)., and the electronic thermostat Sampling station (Mona Biotechnology Co., Ltd). The Viral Nucleic Acid Extraction Reagent (Magnetic Bead Method) and Human Papilloma Virus Nucleic Acid Detection and Genotyping Kit (PCR-Reverse Dot Hybridisation Method) are products of Guangzhou Heshi Biotechnology Co., Ltd.
Specimen Collection and Preservation
Cervical exfoliated cell samples were collected from each participant by professional gynecologists using a cervical brush to obtain an adequate quantity of epithelial cells. Subsequently, the cervical brushes were removed and placed into sterile tubes containing 2 mL of cell preservation solution, which were then stored at a temperature of 2–8°C. The samples were sent to our clinical laboratory in time for HPV DNA genotype testing. If the samples cannot be tested in a timely manner, they may be stored at 2–8°C for no more than two weeks or at −20±5°C for no longer than one year.
DNA Extraction and HPV Genotyping
HPV-DNA was extracted using the Viral Nucleic Acid Extraction Kit (Magnetic Bead Method) and subjected to PCR amplification and reverse dot hybridisation following the instructions of the Guangzhou Heshi HPV Nucleic Acid Detection and Genotyping Kit. Each number on the hybridisation strip corresponds to a specific HPV genotype. The HPV genotype is determined based on the presence or absence of blue dots in the corresponding number area. The kit can simultaneously detect 28 HPV genotypes in human cervical exfoliated cell samples, including: 18 HR-HPV genotypes (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 82, 26, 53, 73), and 10 LR-HPV genotypes (6, 11, 40, 42, 43, 44, 54, 61, 81, 83).
Statistical Analysis
This descriptive study utilized SPSS software (version 24.0) for statistical analysis. Descriptive analyses were conducted on the infection rates and composition ratios of various HPV genotypes. The comparison of infection rates among groups was performed using the χ²-test, with a significance level of P < 0.05 indicating statistical significance.
Results
Analysis of Overall HPV Infection
Among 14,492 cases of female subjects, 2221 cases of HPV positivity were detected, resulting in an overall infection rate of 15.33%. Specifically, 1290 cases of HPV positivity were found among 7070 cases in the gynecology clinic (GC for short) group, with an infection rate of 18.25%. On the other hand, 931 cases of HPV positivity were detected among 7422 cases in the physical examination center (PEC for short) group, resulting in an infection rate of 12.54%. The variance in HPV infection rates between the GC group and the PEC group was statistically significant (18.25% > 12.54%, P < 0.001, Table 1 and Figure 1).
 |
Table 1 Overall Status of HPV Infection |
 |
Figure 1 Proportion of HPV positivity in gynecology clinic group and physical examination center group. |
Prevalence of Type-Specific HR-HPV and LR-HPV Infections
The distribution of HPV genotypes among HPV-positive cases was illustrated in Table 2 and Figure 2. A total of 2221 HPV-positive cases were detected in all tested populations, of which a total of 3100 case-times HPV-positive subtypes were detected in the 2221 HPV-positive cases, and all 28 HPV genotypes were detected. The top five prevalent HR-HPV genotypes were HPV-52 (3.77%), 53 (1.46%), 16 (1.31%), 58 (1.19%), and 39 (1.18%); while the top five LR-HPV genotypes were HPV-54 (1.23%), 61 (1.08%), 81 (1.04%), 42 (0.87%), and 44 (0.70%). In the gynecology clinic group, there were 1866 HPV-positive infections, with the top five prevalence rates of HR-HPV being 52 (4.63%), 53 (1.81%), 16 (1.80%), 51 (1.54%), and 39 (1.51%), and for LR-HPV being 54 (1.32%), 61 (1.27%), 81 (1.07%), 42 (0.99%), and 44 (0.69%). In the physical examination center group, there were 1234 HPV-positive infections, with the top five prevalence rates of HR-HPV being 52 (2.95%), 53 (1.12%), 58 (1.00%), 39 (0.86%), and 16 (0.85%), and for LR-HPV being 54 (1.15%), 81 (1.00%), 61 (0.89%), 42 (0.75%), and 44 (0.70%).
 |
Table 2 Prevalence of Various HPV Genotypes in HPV-Positive Cases |
 |
Figure 2 (A–C) Distribution of HPV genotypes among total HPV-positive cases (A), gynecological outpatients (B), health examination population (C). |
The distribution of the top five genotypes of HR-HPV and LR-HPV prevalence by age group is illustrated in Figure 3. The number of HPV-positive cases in the age groups ≤25, 26–30, 31–35, 36–40, 41–45, 46–50, 51–55, and ≥56 were 378, 581, 665, 418, 273, 270, 227, and 288, respectively. In the ≤25 years age group, the top five genotypes of HR-HPV and LR-HPV prevalence were HR-HPV 52 (5.51%), 16 (2.97%), 53 (2.86%), 58 (2.44%), 51 (1.91%), and LR-HPV 54 (2.22%), 6 (1.48%), 40 (1.48%), 42 (1.48%), 11 (1.27%). In the 26–30 age group, the prevalence rates of HR-HPV were 52 (3.82%), 16 (1.44%), 58 (1.27%), 53 (1.24%), and 51 (1.17%), while LR-HPV rates were 54 (0.87%), 81 (0.84%), 42 (0.74%), 61 (0.70%), and 40 (0.47%). For individuals aged 31–35, the rates of HR-HPV were 52 (3.25%), 39 (1.30%), 53 (1.14%), 51 (1.06%), and 58 (1.03%), with LR-HPV rates of 54 (1.06%), 61 (1.00%), 81 (0.84%), 40 (0.65%), and 42 (0.62%). HR-HPV 52 (3.05%), 39 (1.19%), 51 (1.11%), 53 (1.07%), 58 (0.99%) and LR-HPV 61 (1.07%), 54 (0.91%), 81 (0.91%), 42 (0.82%), 44 (0.66%) in the group of 36–40 years. HR-HPV 52 (3.33%), 53 (1.41%), 58 (1.09%), 68 (1.02%), 16 (0.90%) and LR-HPV 54 (1.35%), 42 (0.96%), 44 (0.83%), 81 (0.83%), 61 (0.70%) in the group of 41–45 years. HR-HPV 52 (4.14%), 53 (1.10%), 16 (1.01%), 39 (0.93%), 56 (0.93%) and LR-HPV 81 (1.86%), 54 (1.61%), 42 (1.35%), 44 (1.35%), 61 (1.35%) in the group of 46–50 years. HR-HPV 52 (4.49%), 53 (1.94%), 16 (1.63%), 68 (1.33%), 51 (0.92%) and LR-HPV 61 (1.94%), 54 (1.63%), 81 (1.22%), 44 (1.02%), 42 (0.82%) in the group of 51–55 years. HR-HPV 52 (5.75%), 53 (3.51%), 16 (2.81%), 58 (2.38%), 68 (2.38%) and LR-HPV 81 (2.10%), 54 (1.96%), 61 (1.96%), 44 (1.54%), 42 (1.12%) in the ≥56 years group.
Prevalence Analysis of Single and Multiple HPV Infections
A total of 2,221 cases of HPV positivity were detected in the female population examined. The highest prevalence was found in single infections at 11.29%, followed by dual infections at 2.72%. Additionally, 191 cases of triple infections and above were identified, with a prevalence rate of 1.32%. Moreover, 7 cases of hexa-infection and above were detected, with a prevalence rate of 0.05% (Table 3). In the gynecology clinic (GC for short) group, single infections were predominant at a prevalence of 13.03%, followed by dual infections at 3.39% (Table 3). In addition, in the physical examination center (PEC for short) group, the prevalence of single infections was highest at 9.63%, followed by dual infections at 2.07% (Table 3). The difference in the composition ratios of different prevalence rates of HPV between the GC group and the PEC group was statistically significant (χ2=103.34, P<0.001). Furthermore, the prevalence of HPV single, dual, triple, quadruple, and quintuple infections in the GC group was higher than that in the PEC group (Table 3). Among the HPV-positive cases in the outpatient female population, HPV single infection accounted for the highest percentage (73.66%), followed by dually infected (17.74%), and multiple infections (≥3) accounted for the lowest percentage (8.60%). The percentages of HPV single infection, dual infection, and multiple infection (≥3) among HPV-positive cases in the GC group and the PEC group were 71.40%, 18.60%, 10.00%; and 76.80%, 16.54%, 6.66%, respectively (Figure 4).
 |
Table 3 Distribution of HPV Infection Feature Among HPV-Positive Cases |
 |
Figure 4 Distribution of HPV single and multiple infections in HPV-positive cases among different groups. |
Prevalence Distribution of HPV Infection in Different Age Groups
Among the 14,492 cases analyzed, the prevalence of HPV infection in the ≤ 25 years old group, 26–30 years old group, 31–35 years old group, 36–40 years old group, 41–45 years old group, 46–50 years old group, 51–55 years old group, and ≥ 56 years old group were 22.88%, 13.76%, 13.12%, 13.88%, 14.35%, 17.16%, 17.53%, and 24.26%, respectively. Notably, the two peaks of the prevalence of HVP infection were in the ≤ 25-year-old group and the ≥ 56-year-old group (Table 4 and Figure 5A). The prevalence of HVP single infection was 13.56%, 9.85%, 9.60%, 11.45%, 11.85%, 13.10%, 13.46%, and 15.29%, and the prevalence of multiple infection was 9.32%, 3.91%, 3.52%, 2.43%, 2.50%, 4.06%, 4.07%, and 8.97%, respectively, for each of the above age groups. Similarly, its two peaks of HVP infection prevalence were in the ≤ 25 years and ≥ 56 years groups. In addition, the HPV infection prevalence of all ages in the gynecology clinic (GC for short) group and the physical examination center (PEC for short) group showed an approximate U-shaped trend, and the HPV infection prevalence of all ages in the GC group was higher than that in the PEC group (Table 5 and Figure 5B).
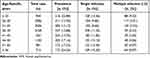 |
Table 4 Prevalence of HPV Infection in Different Age Groups |
 |
Table 5 Prevalence of HPV Infection at All Ages in GC and PEC Groups |
 |
Figure 5 Trends in the prevalence of HPV infection among various age groups. (A) total HPV-positive cases. (B). Abbreviations: GC, gynecology clinic; PEC, physical examination center. |
Discussion
In the absence of the preventive HPV vaccine being included in the national immunisation programme, cervical cancer screening remains the primary method of prevention and control in China.17,18 Currently, cervical cytology and HPV DNA testing are the two most crucial screening methods. Research has shown that the prevalence and genotypes distribution of HPV vary among different ethnic groups, countries, age groups, and female patients with distinct Pap smear results.19,20 HPV genotyping and trend analysis can help identify high-risk groups for cervical cancer, guide the development of cervical cancer vaccines based on infection types, predict lesion progression, and assess prognosis. This is immensely important for the prevention, early diagnosis, and vaccine development related to cervical intraepithelial neoplasia and cervical cancer.
Among the 14,492 female subjects in this study, HPV genotyping identified 2221 HPV-positive cases, resulting in an overall HPV infection rate of 15.33%. This rate was similar to that of Huzhou City, China (15.50%), but lower than rates observed in Kunming (22.03%),21 Chongqing (26.15%),22 Jilin (34.40%),23 and Fujian (38.3%),24 indicating geographical variations in HPV infection rates across China. Our study also found a higher HPV infection rate in the gynecology clinic group (18.25%) compared to the physical examination center group (12.54%), suggesting differences in HPV prevalence among female populations seeking care from different sources. The gynecology clinic group, mostly consisting of individuals with various gynecological conditions like vaginitis, cervicitis, and pelvic inflammatory disease, may exhibit increased susceptibility to HPV infection due to compromised local resistance in the genital tract.
HPV vaccination prior to sexual activity has been shown to effectively prevent HPV infection, serving as a crucial method in the prevention of cervical cancer.25,26 In China, bivalent (HPV16/18), quadrivalent (HPV6/11/16/18), and nine-valent (HPV6/11/16/18/31/33/45/52/58) HPV vaccines were introduced between July 2017 and the end of 2018.27 Currently, the HPV vaccine in China is not part of an immunization program; it is administered voluntarily and at the individual’s own expense.28 From 2018 to 2020, a total of 21.6 million doses of HPV vaccines were administered to women aged 9 to 45, resulting in an estimated full-series cumulative coverage of only 2.24%.29 Among the regions, Beijing, Shanghai, and Zhejiang exhibited the highest estimated coverage levels at 8.28%, 7.37%, and 4.68%, respectively, while Tibet, Qinghai, and Xinjiang reported the lowest coverage levels at 0.06%, 0.39%, and 0.46%.29 Overall, China’s HPV vaccination rate remains relatively low, primarily due to an insufficient supply of vaccines, their relatively high cost, and a general lack of public awareness regarding the necessity of vaccination.30 Understanding the local distribution of HPV genotypes is essential before implementing widespread HPV vaccination, as it can aid in vaccine development and the establishment of optimal vaccine protection strategies. Our study revealed that the top five genotypes of high-risk HPV prevalence among female subjects were HPV52/53/16/58/39, while the top five genotypes of low-risk HPV prevalence were HPV54/61/81/42/44. Interestingly, the top five genotypes of high-risk HPV prevalence in Wuhan differed only in specific genotypes when compared to Kunming (HPV52/16/58/53/51), but were in line with the high-risk HPV infection types observed in Shanghai (HPV52/16/58/53/39). Different subtypes of HPV infection are associated with varying risks of cervical carcinogenesis, with multiple and persistent infections linked to the recurrence of cervical intraepithelial neoplasia and cervical cancer. Low-risk HPV types, such as HPV6, 11, 30, 39, 40, 42, 43, and 44, typically cause benign growths like condyloma acuminatum, but can also result in mild cervical intraepithelial neoplasia.31,32 On the other hand, high-risk HPV types, including HPV 16, 18, 31, 33, 35, 45, and 52, among others, are known oncogenic types, particularly HPV 16 and 18, which are closely associated with the development of severe cervical intraepithelial neoplasia and cervical cancer.33,34 Our study revealed consistent rankings of LR-HPV types in both the gynecology clinic and physical examination center groups, while prevalent genotypes of HR-HPV predominantly included HPV types 52, 53, 16, 51, 39, 58, and 68, with minor variations in rankings. Notably, HPV52 was the most prevalent HR-HPV type across different age groups in our region, while the ranking of LR-HPV types varied significantly by age. Furthermore, a clinical study demonstrated that the nine-valent HPV vaccine was more effective in reducing the incidence of high-grade cervical, vulvar, and vaginal lesions associated with HPV types 31, 33, 45, 52, and 58 compared to the quadrivalent vaccine, with sustained efficacy for up to six years and a 90% prevention rate for cervical cancer development.35 Based on our findings on HPV prevalence in Wuhan, the development of a new multivalent cervical cancer vaccine containing HR-HPV types 52, 53, 16, 51, 39, 58, and 68 may offer enhanced protection against cervical cancer in the region.
HPV infections in this study were mainly single infections, followed by dual infections, with multiple infections (n≥3) being less frequent. The role of multiple HPV infections as a predictor of disease severity remains unclear, although some studies suggest they may contribute to the development of cervical lesions and increase the risk of cervical cancer.36,37 Moreover, our study found a higher prevalence of multiple HPV infections among gynecology outpatients compared to the general physical examination population, highlighting the need for further research to elucidate the association between multiple HPV infections and cervical lesions.
In this study, it was observed in terms of age subgroups that the two peaks of overall HVP prevalence in the female population were ≤ 25 and ≥ 56 years, then HPV prevalence declined with age, then remained stable for a period of time, and then began to rise in the age range of 46–50 years, with the highest rate of infection in the age range of ≥ 56 years. The rates of HPV mono-infection and multi-infection followed a similar trend to overall HPV prevalence. The high prevalence of HPV infection in young women may be attributed to factors such as limited sexual knowledge, inadequate protection during sexual activity, cervical underdevelopment, and immature immune defenses against HPV.38 As women develop adaptive immune responses, there is a decreasing trend in HPV infections. However, menopausal women may find it more challenging to recover from HPV infection due to hormonal imbalances disrupting the physiological immune mechanisms, potentially leading to reactivation of uncleared HPV infections.39,40 Furthermore, there was no bimodal pattern of HPV infection observed in the gynecology outpatient and physical examination population. In the gynecology outpatient clinic, women over 56 years of age had a peak rate of HPV infection, while in the physical examination population, women under 25 years of age showed a peak rate of HPV infection. Therefore, strengthening health education for young women (≤ 25 years old) who have a history of sexual intercourse, increasing the HPV vaccination rate, and enhancing the HPV screening rate in both young and older female populations are crucial for effectively preventing cervical cancer.
The results of this study showed the prevalence and genotype distribution of HPV infection among the outpatient population in Wuhan, China, which is helpful in providing a more scientific basis for the development of cervical cancer prevention and control strategies and the design of novel HPV vaccines. However, there are some limitations in this study. First, all 14,492 women included in the study were from the outpatient population, which means that our results may only represent the hospital population. Second, our investigation lacked cervical exfoliative cytology and histopathology results, which prevented us from analyzing the association between the prevalence and genotype distribution of HPV infection and cervical examination abnormalities. Thirdly, detailed information on HPV vaccination, sexual behaviors, education level and occupation of the study population was lacking, and therefore we were unable to assess the impact of these factors on the prevalence and genotype distribution of HPV infection.
Conclusions
Our data indicate a high overall prevalence of HPV infection in the outpatient female population, with a predominance of mono-infections and a dominance of binary infections in cases of multiple infections. The top five genotypes in terms of prevalence of HR-HPV and LR-HPV were HPV52/53/16/58/39 and HPV54/61/81/42/44, respectively. The prevalence and genotype distribution of HPV infection varied among different outpatient populations. Rates of HPV single-infection, multi-infection, and infection across all ages were higher in the gynecology outpatient population compared to the health check-up population. HPV infection peaks were observed in women aged ≤ 25 and ≥ 56 years, highlighting the importance of HPV screening in these age groups. Furthermore, enhancing HPV vaccination rates and health education for Chinese women, particularly young women, is crucial. Developing a multivalent HPV vaccine that includes HR-HPV types 52, 53, 16, 51, 39, 58, and 68, prevalent in the region, and increasing vaccination coverage could offer targeted protection against cervical cancer in the female population of Wuhan.
Data Sharing Statement
All the data in this study are included in the published articles.
Ethical Approval and Consent to Participate
This study was approved by the Ethics Committee of Wuhan Asia General Hospital and conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from the patients/participants. For participants under 18 years old, consent for their participation was obtained from their parents or legal guardian as well as their own consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by research and innovation fund of Wuhan Asia General Hospital (No. 2022KYCX1-B09).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention. WHO Guidelines Approved by the Guidelines Review Committee; 2021.
3. McBride AA. Oncogenic human papillomaviruses. Philos Trans R Soc Lond B Biol Sci. 2017;372:1732. doi:10.1098/rstb.2016.0273
4. Giuliano AR, Nyitray AG, Kreimer AR, et al. EUROGIN 2014 roadmap: differences in human papillomavirus infection natural history, transmission and human papillomavirus-related cancer incidence by gender and anatomic site of infection. Int J Cancer. 2015;136(12):2752–2760. doi:10.1002/ijc.29082
5. Arbyn M, Weiderpass E, Bruni L, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. doi:10.1016/S2214-109X(19)30482-6
6. Xia CF, Qiao YL, Zhang Y, Zhao FH. WHO’s global strategy of cervical cancer elimination and the challenges and initiatives in China. Zhonghua Yi Xue Za Zhi. 2020;100(44):3484–3488. doi:10.3760/cma.j.cn112137-20200909-02606
7. of Cancer P B, CPMA C, Chinese O, et al. Chinese expert consensus on the use of human papillomavirus nucleic acid testing for cervical cancer screening (2022). Zhonghua Yi Xue Za Zhi. 2023;103:1184–1195. doi:10.3760/cma.j.cn112137-20230117-00096
8. Ren WH, Zhao XL, Zhao FH. Global guidelines for cervical cancer screening: a systematic review. Zhonghua Yi Xue Za Zhi. 2021;101:1882–1889. doi:10.3760/cma.j.cn112137-20210115-00134
9. Li MZ, Wei LH, Sui L, et al. Guidelines for cervical cancer screening in China. Chin J Clini Obst Gynecol. 2023;24(04):437–442. doi:10.13390/j.issn.1672-1861.2023.04.029
10. Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet. 2007;370:890–907. doi:10.1016/S0140-6736(07)61416-0
11. Bruni L, Diaz M, Castellsague X, Ferrer E, Bosch FX, de Sanjose S. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202(12):1789–1799. doi:10.1086/657321
12. de Villiers EM, Fauquet C, Broker TR, Bernard HU, Zur Hausen H. Classification of papillomaviruses. Virology. 2004;324(1):17–27. doi:10.1016/j.virol.2004.03.033
13. Seyoum A, Assefa N, Gure T, Seyoum B, Mulu A, Mihret A. Prevalence and Genotype Distribution of High-Risk Human Papillomavirus Infection Among Sub-Saharan African Women: a Systematic Review and Meta-Analysis. Front Public Health. 2022;10:890880. doi:10.3389/fpubh.2022.890880
14. de Sanjose S, Quint WG, Alemany L, et al. Human papillomavirus genotype attribution in invasive cervical cancer: a retrospective cross-sectional worldwide study. Lancet Oncol. 2010;11(11):1048–1056. doi:10.1016/S1470-2045(10)70230-8
15. Humans IWGotEoCRt. Biological agents. IARC Monogr Eval Carcinog Risks Hum. 2012;100(Pt B):1–441.
16. Li K, Li Q, Song L, Wang D, Yin R. The distribution and prevalence of human papillomavirus in women in mainland China. Cancer. 2019;125(7):1030–1037. doi:10.1002/cncr.32003
17. Xu X, Wang Y, Liu Y, et al. A nationwide post-marketing survey of knowledge, attitudes and recommendations towards human papillomavirus vaccines among healthcare providers in China. Prev Med. 2021;146:106484. doi:10.1016/j.ypmed.2021.106484
18. Zhang J, Zhao Y, Dai Y, et al. Effectiveness of High-risk Human Papillomavirus Testing for Cervical Cancer Screening in China: a Multicenter, Open-label, Randomized Clinical Trial. JAMA Oncol. 2021;7(2):263–270. doi:10.1001/jamaoncol.2020.6575
19. de Sanjose S, Diaz M, Castellsague X, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis. 2007;7(7):453–459. doi:10.1016/S1473-3099(07)70158-5
20. Galati L, Peronace C, Fiorillo MT, et al. Six years genotype distribution of Human Papillomavirus in Calabria Region, Southern Italy: a retrospective study. Infect Agent Cancer. 2017;12:43. doi:10.1186/s13027-017-0154-5
21. Zhang Y, Xu Y, Dian Z, et al. Prevalence and Genotype Distribution of Human Papillomavirus Infection Among 40,613 Women: an Outpatient-Based Population Study in Kunming, Yunnan. Front Public Health. 2022;10:922587. doi:10.3389/fpubh.2022.922587
22. Tang Y, Zheng L, Yang S, Li B, Su H, Zhang LP. Epidemiology and genotype distribution of human papillomavirus (HPV) in Southwest China: a cross-sectional five years study in non-vaccinated women. Virol J. 2017;14(1):84. doi:10.1186/s12985-017-0751-3
23. Hao S, Wang C, Liu S, He J, Jiang Y. HPV genotypic spectrum in Jilin province, China, where non-vaccine-covered HPV53 and 51 are prevalent, exhibits a bimodal age-specific pattern. PLoS One. 2020;15(3):e0230640. doi:10.1371/journal.pone.0230640
24. Wu C, Zhu X, Kang Y, et al. Epidemiology of Humanpapilloma virus infection among women in Fujian, China. BMC Public Health. 2017;18(1):95. doi:10.1186/s12889-017-4651-7
25. Markowitz LE, Liu G, Hariri S, Steinau M, Dunne EF, Unger ER. Prevalence of HPV After Introduction of the Vaccination Program in the United States. Pediatrics. 2016;137(3):e20151968. doi:10.1542/peds.2015-1968
26. Garland SM, Kjaer SK, Munoz N, et al. Impact and Effectiveness of the Quadrivalent Human Papillomavirus Vaccine: a Systematic Review of 10 Years of Real-world Experience. Clin Infect Dis. 2016;63(4):519–527. doi:10.1093/cid/ciw354
27. Lin Y, Lin Z, He F, et al. HPV vaccination intent and willingness to pay for 2-,4-, and 9-valent HPV vaccines: a study of adult women aged 27-45 years in China. Vaccine. 2020;38(14):3021–3030. doi:10.1016/j.vaccine.2020.02.042
28. Affiliated Association for Standardized Management and Practice of Immunization Program, China Association for Vaccines, Expert consensus on the immunization strategy and practice of human papillomavirus vaccine for female adolescents in the Yangtze River Delta region. Chin J Prevent Med. 2023;(02):135–153. doi:10.3760/cma.j.cn112150-20221110-01093
29. Song YF, Liu XX, Yin ZD. Human papillomavirus vaccine coverage among the 9-45-year-old female population of China in 2018-2020. Chin J Vacci Immuni. 2021;27(05):570–575. doi:10.19914/j.CJVI.2021101
30. Lingnan Cervical Cancer Prevention and Treatment Union of the Third Affiliated Hospital of Sun Yat-sen University; Cervical Cancer Prevention and Treatment Committee of Guangdong Preventive Medicine Association Less, Chinese expert consensus on the safety of human papillomavirus vaccination. J Chin Phys. 2023;(11):1644–1660. doi:10.3760/cma.j.cn431274-20231007-00343
31. Viens LJ, Henley SJ, Watson M, et al. Human Papillomavirus-Associated Cancers - United States, 2008-2012. MMWR Morb Mortal Wkly Rep. 2016;65(26):661–666. doi:10.15585/mmwr.mm6526a1
32. Shoja Z, Farahmand M, Hosseini N, Jalilvand S. A Meta-Analysis on Human Papillomavirus Type Distribution among Women with Cervical Neoplasia in the WHO Eastern Mediterranean Region. Intervirology. 2019;62(3–4):101–111. doi:10.1159/000502824
33. Thomas TL. Cancer Prevention: HPV Vaccination. Semin Oncol Nurs. 2016;32(3):273–280. doi:10.1016/j.soncn.2016.05.007
34. Lowy DR, Schiller JT. Reducing HPV-associated cancer globally. Cancer Prev Res. 2012;5(1):18–23. doi:10.1158/1940-6207.CAPR-11-0542
35. Huh WK, Joura EA, Giuliano AR, et al. Final efficacy, immunogenicity, and safety analyses of a nine-valent human papillomavirus vaccine in women aged 16-26 years: a randomised, double-blind trial. Lancet. 2017;390(10108):2143–2159. doi:10.1016/S0140-6736(17)31821-4
36. Na J, Li Y, Wang J, Wang X, Lu J, Han S. The correlation between multiple HPV infections and the occurrence, development, and prognosis of cervical cancer. Front Microbiol. 2023;14:1220522. doi:10.3389/fmicb.2023.1220522
37. Fantin C, Freitas JB, Teles HFM, Oliveira BAS, Brito DV. High prevalence of HPV 18 and multiple infections with oncogenic HPV genotypes in women at risk of cervical cancer examined in Manaus, Brazil. Braz J Med Biol Res. 2023;56:e12720. doi:10.1590/1414-431X2023e12720
38. Liu Z, Nyitray AG, Hwang LY, et al. Acquisition, Persistence, and Clearance of Human Papillomavirus Infection Among Male Virgins Residing in Brazil, Mexico, and the United States. J Infect Dis. 2018;217(5):767–776. doi:10.1093/infdis/jix588
39. Trottier H, Ferreira S, Thomann P, et al. Human papillomavirus infection and reinfection in adult women: the role of sexual activity and natural immunity. Cancer Res. 2010;70(21):8569–8577. doi:10.1158/0008-5472.CAN-10-0621
40. Li Z, Liu F, Cheng S, et al. Prevalence of HPV infection among 28,457 Chinese women in Yunnan Province, southwest China. Sci Rep. 2016;6:21039. doi:10.1038/srep21039
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


