Back to Journals » Neuropsychiatric Disease and Treatment » Volume 21
Prevalence, Diagnosis, and Treatment of Generalized Anxiety Disorder in Working Individuals: A Cross-Sectional Study Using Health Claims and Survey Data in Japan
Authors Matsuyama S , Otsubo T, Nomoto K , Misago R, Higa S
Received 25 December 2024
Accepted for publication 24 June 2025
Published 9 July 2025 Volume 2025:21 Pages 1371—1385
DOI https://doi.org/10.2147/NDT.S513964
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Taro Kishi
Satoshi Matsuyama,1,* Tempei Otsubo,2,* Keisuke Nomoto,1,* Rikiya Misago,1 Shingo Higa1,*
1Medical Affairs, Viatris Pharmaceuticals Japan G.K., Tokyo, Japan; 2Department of Psychosomatic and Psychiatric Medicine, Tokyo Women’s Medical University Adachi Medical Center, Tokyo, Japan
*These authors contributed equally to this work
Correspondence: Satoshi Matsuyama, Medical affairs, Viatris Pharmaceuticals Japan G.K, Azabudai Hills Mori JP Tower, 1-3-1 Azabudai, Minato-ku, Tokyo, 106-0041, Japan, Tel +81-3-5656-0400, Fax +81-3-5656-0603, Email [email protected]
Purpose: Generalized anxiety disorder (GAD) is a common anxiety disorder, and in Japan is poorly understood to be a serious condition among medical practitioners and the general public. This study was, therefore, conducted targeting individuals with probable GAD, to estimate the prevalence of probable GAD as the primary outcome, and to assess medical consultation behavior, diagnosis, treatment, quality of life (QOL), severity of depression symptoms, and work productivity as secondary outcomes.
Patients and Methods: This was conducted as a cross-sectional study focusing on individuals with probable GAD, using a database comprising medical claims data from May 2022 to November 2022, and linked survey data collected in November 2022, provided by DeSC Healthcare, Inc. (DeSC). Probable GAD was defined as a score of ≥ 10 in the Generalized Anxiety Disorder 7-item questionnaire (GAD-7). Secondary endpoints were assessed from claims data and online survey data.
Results: In the study population (n = 18,995), the overall prevalence of probable GAD was 6.4%. Among the probable GAD group, a total of 89.7% individuals received medical consultation; and among this population, 15.8% of individuals consulted with a psychiatric specialist. In the probable GAD group, the most common psychiatric disorder diagnoses were sleep disorders, mood disorders other than bipolar disorder, and somatoform disorders. The most commonly prescribed drugs were antianxiety drugs, followed by hypnotics, and antidepressants. QOL and work productivity were lower in the probable GAD group than the non-probable GAD group; whereas, severity of depression was higher in the probable GAD group.
Conclusion: The study findings showed a high prevalence of probable GAD, low consultation behavior, and clarified the diagnosis and treatment status for GAD. These findings highlight the need to raise awareness of GAD among both physicians and patients, leading to appropriate consultation behavior, diagnosis, and treatment.
Keywords: GAD-7, generalized anxiety disorder, Japan, prevalence, survey, claims data
Introduction
Generalized anxiety disorder (GAD) is defined as a psychiatric condition characterized by excessive uncontrollable anxiety and worry, occurring more days than not for at least 6 months, about a number of events or activities such as work or school performance. Key symptoms of GAD include restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbances.1 These symptoms may lead to serious impairment of social and occupational functioning and exert a negative impact on the quality of life (QOL) and work productivity.2,3
It is believed that GAD is one of the most common anxiety disorders and there has been a global trend to conduct research worldwide to gain a better understanding of this condition. The World Mental Health (WMH) Survey Initiative includes 29 surveys carried out in 26 countries from 2001 to 2012.4 The results indicate the combined lifetime prevalence of GAD was 3.7%, and 12-month prevalence was 1.8%. Additionally, efforts to understand the treatment landscape and recommend therapeutic agents have led to the publication of several clinical GAD guidelines. These include the “S3 guideline on anxiety disorders”,5 “Canadian clinical practice guidelines”,6 “World Federation of Societies of Biological Psychiatry (WFSBP) guidelines”.7 Systematic reviews and network meta-analyses have also been conducted to clarify optimal treatment approaches.8
In Japan, generally GAD is not widely recognized, and the number of studies on this condition remains limited. Even so, there have been several reports on prevalence rates, and one study using the GAD screening questionnaire based on the Diagnostic and statistical manual of mental disorders, Fourth Edition (DSM-IV)9 showed that the prevalence of anxiety disorders likely to be diagnosed as GAD was 3.2%, in 2003.10 Regarding other surveys based on DSM-IV, in the World Mental Health Japan Survey 1st (WMHJ1, 2002–2006) it was estimated that lifetime and 12-month prevalences of GAD were 2.6% and 1.2%, respectively.11 WMHJ 2nd (2013–2015) showed a lifetime prevalence of 1.6% and a 12-month prevalence of 0.6%.12
In one web-based, cross-sectional online survey related to GAD among the general population in Japan conducted in 2022, the prevalence of probable GAD (GAD-7 score equal to or greater than 10) was 7.6%.13 This survey also showed that individuals with probable GAD had a greater diagnostic history of depression, panic disorder and social anxiety disorder than GAD. Another survey among 509 physicians conducted in 2022 reported that depression, panic disorder and social anxiety disorder were the most frequently reported comorbidities in GAD patients.14 These surveys suggest the possibility that many GAD patients are diagnosed and treated as having different disorders.
Although these studies have provided preliminary estimates of the prevalence and characteristics of GAD, a research gap remains, as they have relied solely on self-reports from patients or doctors and have not integrated clinical and patient-reported data. Consequently, comprehensive information on the prevalence, diagnosis, medical consultation, and treatment of GAD in Japan is still limited. The lack of standardized care, such as the absence of psychotropic drugs indicated for GAD and the lack of treatment guidelines has caused low awareness of GAD as a serious condition among both healthcare providers and the public, potentially contributing to underdiagnosis and suboptimal treatment. Of great importance may be the fact that outcomes are poorer when GAD treatment is initiated at a later stage, and it is especially important to start treatment within one year of onset.15 Reporting the actual status of GAD in Japan, from an integrated perspective, using claims and survey data, will be relevant to clinical practitioners in the field.
Therefore, to provide a comprehensive description of GAD in a real-world setting, in Japan, we conducted this study using a database combining claims and survey data. Specifically, the aim of this study was to estimate the prevalence of probable GAD and to assess medical consultation behavior, diagnosis, treatment, severity of depression symptoms, QOL and work productivity, among individuals with probable GAD. More specifically, in this context, diagnosis and treatment refer to the diagnostic names based on the ICD-10 codes, and prescribed medications listed in the claims data.
Materials and Methods
Study Design and Data Source
This was conducted as a cross-sectional study focusing on GAD patients using a database comprising medical claims data and survey data provided by DeSC Healthcare, Inc., (DeSC) Tokyo, Japan.
Data for this study included the data from employment-based insurance subscribers of multiple health insurance associations contracted by DeSC, who responded to an online survey on mental disorders for working individuals conducted by DeSC in November 2022, among registrants with an online health application, “kencom®” (limited to those 19 years of age or older), which is a health promotion support application provided to subscribers registered with DeSC. In the online survey conducted in November 2022, participants replied to several self-administered questionnaires. The Japanese version of the GAD-7 questionnaire was used to measure anxiety levels. The GAD-7 is an easy-to-use, 7-item, 4-point (0 to 3) scale that was developed as a self-administered questionnaire for the assessment of GAD. Both original and Japanese versions of GAD-716,17 demonstrated high sensitivity and specificity in the diagnosis of GAD, when using a cutoff value of 10. Patient Health Questionnaire-9 (PHQ-9), which consists of 9 questions, was used to assess the severity of depression symptoms.18 EuroQol 5 dimensions 5-level (EQ-5D-5L), which assesses 5 dimensions: “mobility”, “self-care”, “usual activities”, “pain/discomfort” and “anxiety/depression”, and the EuroQol Visual Analog Scale (EQ-VAS) were used to measure QOL.19 The Work Productivity and Activity Impairment Questionnaire Global Health (WPAI-GH) was used to measure the degree of effect of health problems on work and daily activities, where a high WPAI-GH score indicates a greater effect on work and daily activities.20 By using the integrated anonymously processed medical claims receipt data and online survey response data provided by DeSC, it was possible to evaluate the prevalence of probable GAD, including individuals that did not visit medical institutions, and to conduct an assessment of actual clinical factors among individuals with probable GAD; and individuals with probable non-GAD from a broader perspective.
Subject Population
Individuals who met the following inclusion criteria and analysis of probable GAD prevalence were eligible for inclusion in the study: individuals who had response data from the online survey conducted by DeSC in November 2022; individuals who were self-reported workers; and individuals who had a total score in the GAD-7 questionnaire.
Individuals who met any of the following criteria, in the past 3 years (Figure 1), including the month the online survey was conducted were not included in the study: substance use disorder (ICD10 Code: F10-F19); schizophrenia (ICD10 Code: F20-F29); and dementia (ICD10 Code: F00-F09). Individuals with substance use disorders, or schizophrenia, were excluded as they are listed in the differential diagnosis of the DSM-5 diagnostic criteria of GAD. Individuals with dementia were excluded because the accuracy of responses cannot be guaranteed using self-report tools.
 |
Figure 1 Subject disposition. Abbreviations: DeSC, DeSC Healthcare, Inc., Japan; GAD, generalized anxiety disorder; GAD-7, Generalized Anxiety Disorder 7-item. |
In addition, the following exclusion criterion was set for the analysis of clinical factors (Figure 1): individuals who were not enrolled in the database for 7 consecutive months, including the month the online survey was conducted and the preceding 6 months.
Subject Flowchart
After the analysis population was identified according to the inclusion and exclusion criteria, individuals included in the analysis of clinical factors were divided into the probable GAD group and the probable non-GAD group, based on GAD-7 scores, not based on physician’s diagnosis, and further subdivided as shown below (Figure 1).
Probable GAD group
Individuals who had a GAD-7 score of ≥10. This group was subdivided into two groups as follows.
- Medical consultation group: Individuals who received at least one medical consultation within 7 months of the study data collection period. The medical consultation group was further subdivided as follows: specialist consultation group, which was defined as individuals who consulted with a psychiatric specialist (department code of psychiatry [department code: 02] or psychosomatic medicine [33], or one or more medical practice codes corresponding to specified medical practices, refer to Supplementary Table 1); and non-specialist consultation group, which was defined as individuals who consulted with a non-specialist (and who had never received consultation with a psychiatric specialist).
- No medical consultation group: Individuals who did not receive medical consultation within 7 months of the study data collection period.
Probable non-GAD group
Individuals who had a GAD-7 score of <10. This group was subdivided into two groups.
- Medical consultation group: Individuals with at least one medical consultation within 7 months of the study data collection period.
- No medical consultation group: Individuals without medical consultation within 7 months of the study data collection period.
Study Endpoints
The primary endpoint was the prevalence of probable GAD and was defined by a GAD-7 score of ≥10, in working individuals. The secondary endpoints included the following:
- Percentages of individuals who received medical consultation, and the percentages of individuals who consulted with psychiatric specialists in individuals with probable GAD who received medical consultation.
- Percentage of prescription drugs, focusing on psychotropic drugs (refer to Supplementary Table 2) in individuals with probable GAD who consulted with a psychiatric specialist, in individuals with probable GAD who consulted with a non-specialist; and in individuals with probable GAD who received medical consultation.
- Percentages of diagnosis (mental disorder and physical disease, refer to Supplementary Tables 3 and 4) in individuals with probable GAD who consulted with a psychiatric specialist, in individuals with probable GAD who consulted with a non-specialist, in individuals with probable GAD who received medical consultation, in individuals with probable GAD.
- Depression assessment, QOL and work productivity in individuals who consulted with psychiatric specialist and individuals who consulted with non-specialist among individuals with probable GAD; and in individuals with probable GAD, and individuals with probable non-GAD.
Additionally, exploratory endpoints were incorporated, namely the prevalence, when probable GAD was defined as a GAD-7 score ≥10 and the response to the question about the degree of impact on daily life was “very difficult” or “extremely difficult”.
Statistical Analysis
As summary statistics, frequency and percentage were calculated for categorical variables and mean, standard deviation, median were calculated for continuous variables.
To estimate the prevalence of probable GAD, the number, proportion and 95% confidence intervals (95% CI, using the Clopper–Pearson method) of individuals with probable GAD were calculated using the number of individuals included in the analysis of GAD prevalence (individuals who met all inclusion criteria) and did not meet any of exclusion criteria, as the denominator. In addition, stratification was conducted by age categories and sex.
To assess the distribution of subgroups, the numbers and percentages of individuals who received medical consultation in probable GAD and probable non-GAD, and the percentages of individuals who consulted with psychiatric specialists in individuals with probable GAD who received medical consultation were calculated.
To assess diagnosis and prescription drugs in each subgroup, the numbers and percentages of each diagnosis and prescription drug were calculated for each of the following three groups: 1. individuals with probable GAD who consulted with a psychiatric specialist and a non-specialist; 2. individuals with probable GAD who received medical consultation; and 3. individuals with probable GAD.
To assess the EQ-5D-5L index score, EQ-VAS score, PHQ-9 score, depression severity based on PHQ-9 score, and WPAI-GH scores for 4 domains in each subgroup, summary statistics for the scores were calculated and compared for each of the following two groups using Wilcoxon rank sum test for PHQ-9 depression severity and t-test for continuous variables: 1. individuals with probable GAD who consulted with a psychiatric specialist and a non-specialist; and 2. individuals with probable GAD and probable non-GAD.
To assess the correlation between GAD-7 and PHQ-9 scores, Pearson’s correlation coefficient was calculated.
Multivariate logistic regression analysis was conducted to examine the association between independent variables and the condition of probable GAD. No imputation for missing data was conducted.
Data analysis was performed using Statistical Analysis Software (SAS Institute, Cary, NC, USA, version 9.4).
Results
Among the individuals included in the DeSC database (n = 917,147), on the basis of the inclusion and exclusion criteria, 18,995 individuals (Analysis set 1) were identified as eligible for analysis of GAD prevalence (Figure 1). Among the analysis set, 18,742 individuals (Analysis set 2) were included in the analysis of clinical factors.
Prevalence
In the study population for the analysis of GAD prevalence (n = 18,995), the overall prevalence of probable GAD, defined by a GAD-7 score ≥10, was 6.4% (95% CI: 6.0–6.7%) (Table 1).
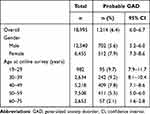 |
Table 1 Prevalence of Probable GAD by Gender and Age Category |
The prevalence of probable GAD in the population where the exploratory endpoints were used (in addition to GAD-7 score ≥10, the degree of impact on daily life was also “very difficult” or “extremely difficult”) was 1.2% (224/18,995).
By sex, the estimated prevalence of probable GAD was higher in females 7.9% (95% CI: 7.3–8.6%) than in males 5.6% (95% CI: 5.2–6.0%). By age category, the estimated prevalence of probable GAD was higher in the younger age groups, and decreased values were observed in older age groups.
Demographics
A total of 1,188 individuals were included in the probable GAD group. By sex, the probable GAD group comprised 58.6% males and 41.4% females (Table 2). In this group, the mean age was 45.5 years. A total of 17,554 individuals were included in the probable non-GAD group. By sex, the probable non-GAD group comprised 66.8% males and 33.2% females. In this group, the mean age was 49.2 years.
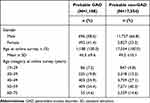 |
Table 2 Demographics |
Medical Consultation
Among the probable GAD group, a total of 89.7% (1,066/1,188) individuals received medical consultation for any reason; and among this population 15.8% (168/1,066) of individuals consulted with a psychiatric specialist. Therefore, a total of 14.1% (168/1,188) individuals in the probable GAD group were found to have consulted with a psychiatric specialist. A total of 122 individuals did not have claims data for medical consultation and were classified as receiving “No medical consultation”.
Among the exploratory analysis group, a total of 89.0% (194/218) of individuals received medical consultation for any reason; and among this population 25.8% (50/194) of individuals consulted with a psychiatric specialist. A total of 22.9% (50/218) individuals in the exploratory analysis group were, therefore, found to have consulted with a psychiatric specialist.
In assessing visits to medical institutions by severity on the basis of GAD-7 scores, 12.8% (107/837) of individuals with moderate anxiety (10–14) visited a psychiatric specialist, compared to 17.4% (61/351) of individuals with severe anxiety (15–21), indicating that the proportion of visits to a psychiatric specialist was higher in the group with a higher GAD-7 score. Additionally, among individuals who received medical consultation, the GAD-7 scores of the specialist consultation group were higher compared to those in the non-specialist consultation group (mean: 14.0 vs 13.3).
Depression Assessment (PHQ-9)
In the comparison between the probable GAD group and the probable non-GAD group (Table 3), the PHQ-9 score was significantly higher in the probable GAD group (mean: 13.9 vs 3.3).
 |
Table 3 Comparison of PHQ-9, QOL and Work Productivity Between the Probable GAD Group and Probable Non-GAD Group |
In the comparison between the specialist consultation group and the non-specialist consultation group among the probable GAD group (Table 4), the PHQ-9 score was significantly higher in the specialist consultation group (mean: 15.5 vs 13.6).
 |
Table 4 Comparison of PHQ-9, QOL, and Work Productivity Between Specialist Consultation Group and Non-Specialist Consultation Group Among the Probable GAD Group |
In the correlation analysis, a strong correlation was shown between GAD-7 and PHQ-9 scores (r = 0.811).
Additionally, associations were found between probable GAD and PHQ-9 values with statistical significance (p < 0.001) in the results of the multivariate logistic regression analysis conducted to examine the association between independent variables and the condition of probable GAD (n = 18,742) (Supplementary Table 5).
Quality of Life Assessment (EQ-5D-5L, EQ-VAS)
In the comparison between the probable GAD group and the probable non-GAD group (Table 3), both the EQ-5D-5L index score (0.767 vs 0.916) and EQ-VAS score (58.8 vs 80.4) were significantly lower in the probable GAD group. These differences were larger in the anxiety/depression and pain/discomfort (median 2.0 vs 1.0; and 2.0 vs 1.0 respectively) dimensions.
In the comparison between the specialist consultation group and the non-specialist consultation group (Table 4), both the EQ-5D-5L index score (0.712 vs 0.774) and EQ-VAS score (53.9 vs 59.2) were significantly lower in the specialist consultation group. This difference was notably larger in the anxiety/depression dimension (median 3.0 vs 2.0). Individuals with a lower QOL score were more likely to consult with a psychiatric specialist.
Work Productivity (WPAI)
In the comparison between the probable GAD group and the probable non-GAD group (Table 3), the WPAI score was higher in the probable GAD group for the following items: absenteeism, presenteeism, overall work impairment, and activity impairment. In the comparison between the specialist consultation group and non-specialist consultation group among the probable GAD group (Table 4), the WPAI score was higher in the specialist consultation group in all the following items: absenteeism, presenteeism, overall work impairment, and activity impairment.
Diagnosis
In the analysis of diagnoses made at medical consultations, in this study we focused on mental disorders and physical diseases (Supplementary Tables 3, 4) which are considered to be comorbidities of GAD at high frequencies.
Among the diagnoses made of the 1,066 individuals that comprised the probable GAD group (Table 5), the most common mental disorders were sleep disorders, mood disorders other than bipolar disorder (BP), somatoform disorders, and GAD. In the probable GAD group, the most common physical diseases were asthma, constipation, dizziness, pain, headache, and nausea and vomiting.
 |
Table 5 Diagnoses of Specialist Consultation Group and Non-Specialist Consultation Group in the Probable GAD Group |
Among the diagnoses of the 168 individuals who consulted with a psychiatric specialist in the probable GAD group, the most common mental disorders were mood disorders other than BP, sleep disorders, and GAD. In this group, the most common physical diseases were constipation, headache, dizziness, asthma, pain, and irritable bowel syndrome.
Treatment (Prescription Drugs)
Among the prescription drugs of 1,066 individuals who comprised the probable GAD group (Table 6), the most commonly prescribed drugs were antianxiety drugs, followed by hypnotics, and antidepressants. The majority of antianxiety drugs were benzodiazepine anxiolytics. The most prescribed hypnotics were benzodiazepine hypnotics, followed by non-benzodiazepine hypnotics (Z-drugs), and orexin receptor antagonists. The most prescribed antidepressants were selective serotonin reuptake inhibitors (SSRIs), followed by serotonin and norepinephrine reuptake inhibitors (SNRIs); and tricyclics or tetracyclics/serotonin2-antagonist/reuptake inhibitor (SARI).
 |
Table 6 Prescription Drugs of Specialist Consultation Group and Non-Specialist Consultation Group in the Probable GAD Group |
Regarding prescribed drugs among the 168 individuals who consulted with a psychiatric specialist in the probable GAD group (Table 6) the most common drugs were antianxiety drugs, followed by antidepressants and hypnotics. The most prescribed antianxiety drugs were benzodiazepine anxiolytics. The most prescribed antidepressants were SSRIs, followed by SNRIs and tricyclics or tetracyclics/SARI. The most prescribed hypnotic drugs were benzodiazepine hypnotics, followed by Z-drugs and orexin receptor antagonists.
In 898 individuals who consulted with a non-specialist, the number of antidepressant drugs prescribed (n = 14) was smaller compared to hypnotics (n = 41) and antianxiety drugs (n = 39) (Table 6).
Discussion
This study investigated the prevalence of GAD in Japan in a large sample size, using health insurance database combined claims data with survey result data. This unique methodology enabled us to clarify the actual status associated with GAD, including the consultation situation, diagnosis, and prescription drugs under the current situation that GAD is not frequently diagnosed in Japan.
The prevalence of probable GAD as defined by a GAD-7 score ≥10 was 6.4%, which is a higher value than observed in previously reported studies. Tajima et al reported a GAD prevalence value of 3.2% in 2003.10 Whereas Ishikawa et al reported a GAD prevalence value of 2.6% over the period 2002–2006;11 and a value of 1.6% in the period 2013–2015.12 The relatively high prevalence of probable GAD found in our study may be due to the fact that probable GAD was identified using a self-reporting screening tool. Additionally, as our study was conducted during the COVID-19 pandemic, it is possible that COVID-19 may have exerted an influence on GAD prevalence. This is consistent with a general population survey conducted in 2022,13 in which the prevalence of probable GAD was reported to be 7.6%. Our results show a higher prevalence of probable GAD in females and younger aged individuals, which is consistent with the results of previous reports.11,13
The EQ-5D-5L, EQ-VAS and WPAI scores were significantly worse in the probable GAD group than in the probable non-GAD group, suggesting that probable GAD has negative effects on both QOL and work productivity. To improve this situation, it is suggested that affected individuals should receive medical consultation, to obtain appropriate diagnosis and treatment.
Regarding medical consultation, although not all individuals in the probable GAD group required medical treatment, 89.7% of individuals received medical consultation for any reason; and 14.1% of individuals received medical consultation with a psychiatric specialist. It was shown that individuals with high GAD-7 scores and individuals with symptoms of high severity were more likely to visit a psychiatric specialist than individuals with lower GAD-7 scores and symptoms of mild severity. Additionally, depression assessment PHQ-9 scores and QOL values (EQ-5D-5L, EQ-VAS) were higher; whereas work productivity scores (WPAI) were lower in the specialist consultation group compared to those in the non-specialist consultation group, which may suggest that individuals with greater disruption to daily activities were more likely to consult with psychiatric specialists. However, as complications and cultural backgrounds were not considered, it is necessary to interpret the findings cautiously. In cases where physical symptoms caused by comorbidities are severe, patients may visit a physician other than a psychiatrist; and cultural factors include, consultation barriers and stigma attached to psychiatric illness in Japan, which may lead to people refraining from visiting psychiatrist medical facilities.21 As a previous survey showed, in Japan the awareness of GAD is low, and many people think that the symptoms are caused by personality traits.13 By raising awareness and correctly understanding the disease, in the general population, more people will be able to seek medical consultation that is best suited for them.
Among the 1,066 individuals in the probable GAD group that sought medical consultation, the main diagnoses (mental disorders) were sleep disorders (18.4%) and mood disorders other than BP (14.4%). The diagnosis of GAD was comparatively low and only 3.8% of individuals were diagnosed with this condition. Even in the specialist consultation group, the proportion of individuals diagnosed with GAD was only 10.7%, which was low compared with 75.6% for the diagnosis of mood disorders other than BP, and 65.5% for sleep disorders. It is known that GAD is often comorbid10 with other psychiatric disorders,22 and it is, therefore noteworthy that in our study that sleep disorders and mood disorders other than BP were the most common diagnoses made in 40 individuals diagnosed with GAD in the probable GAD group. While a GAD-7 score ≥10 is not a definitive diagnosis of GAD, our results show that proactive diagnosis of GAD is low as evidenced by the fact that a small number of individuals were diagnosed with GAD, compared to other psychiatric disorders, even by psychiatric specialists. In a previous survey of Japanese specialists, more than one-half of participants responded that disease awareness of GAD even among psychiatric specialists was insufficient, and it is considered important to make them aware of GAD.14 The low rate of GAD diagnosis may provide proof of low disease awareness.
Regarding the diagnosis of physical diseases, among 40 individuals diagnosed with GAD in the probable GAD group, the most frequent physical diagnoses were headache, constipation, dizziness, asthma, and pain. These conditions and symptoms are commonly thought to be associated with excessive anxiety.23–29 When treating these physical symptoms, consideration should be made regarding the possibility of underlying concomitant GAD in the afflicted individuals. In addition, it is generally known that GAD is commonly comorbid with depression.30 In our study, a strong positive correlation was confirmed between GAD-7 and PHQ-9 scores (r = 0.811). In consideration of this finding, it is recommended that at the time of depression diagnosis an assessment should simultaneously be made to confirm GAD comorbidity and excessive anxiety.
Regarding the status of treatment in the probable GAD group, antidepressants were prescribed to fewer individuals than antianxiety drugs and hypnotics. In the specialist consultation group, however, it was shown that antidepressants were prescribed to approximately the same number of individuals as antianxiety drugs and hypnotics. Conversely, non-specialists prescribed antidepressants to fewer individuals compared to hypnotics and antianxiety drugs. Among the 40 individuals that were diagnosed with GAD in the probable GAD group, the prescription rate of antidepressants in the non-specialist consultation group (4.5%, 1/22) was much lower than in the specialist consultation group (44.4%, 8/18). From these findings, it is, however, not possible to assess whether antidepressants were used appropriately or whether the prescription pattern was affected by the severity of symptoms. Regarding hypnotic drugs, the use of benzodiazepine hypnotics accounts for approximately half of all prescribed hypnotic drugs, followed by Z-drugs. Regarding antianxiety drugs, the most commonly prescribed class was benzodiazepine anxiolytics. Excessive prescription of benzodiazepine anxiolytics is considered to be one of the major problems in appropriately using psychotropic drugs, and in Japan warnings are provided regarding the dose and administration period of benzodiazepine anxiolytics.31,32 In our study, information was not collected on dose information and administration periods. The results of this study indicate that benzodiazepine anxiolytics are prescribed at slightly higher rates by non-specialists, but it is not possible to conclude whether or not this prescription rate is excessive. Indeed, it was reported that the prescription of antianxiety drugs has been decreasing year by year.33 The prescription situation for psychotropic drugs may be starting to become more appropriate, largely due to the efforts of medical professionals, including psychiatric specialists.
Limitations
The health survey was distributed to users of a computer-based health application. It is to be noted that there is selection bias inherent to the usage of the DeSC database. DeSC distributes health surveys to users of a computer-based health application. There is a possibility that users of such an application may take a greater interest in their health status, than non-users, which may influence the survey results, especially with regard to GAD-7, QOL and WPAI scores. Additionally, as the survey data were collected online, individuals without technical access were unable to participate and provide survey data. Essentially, the data derived from the individuals covered by employment-based health insurance, thereby comprised of employees of large businesses and their dependents. As such, there may be limited external generalizability in the results of this study to people outside the workforce, and to individuals that are self-employed, civil servants and individuals employed by small companies. Reflecting the characteristics of data source population, the age range of subjects included in the study results are predominantly in the range 20–60 years, and there may be limited generalizability to people that are outside this age range.
The GAD prevalence data were self-reported in the survey data and was not objectively obtained from doctors’ diagnoses which means that recall bias and/or reporting bias may have resulted in either an over-reporting or under-reporting of the true population prevalence. The GAD-7 scores of individuals who received treatments and experienced controlled symptoms was low, and they may be included in the probable non-GAD group. As stated previously, this may have resulted in over-reporting or under-reporting the true population prevalence of probable non-GAD. Finally, as the dosage, duration, and combination of prescribed drugs were not collected, it was not possible to evaluate the true appropriateness in the use of drugs.
Conclusion
The prevalence of probable GAD in our study is estimated as 6.4% in working individuals. Individuals with probable GAD showed lower QOL and work productivity, and higher depressive tendencies. Additionally, it was shown that the proportion of individuals who consulted with psychiatric specialists was low.
Few individuals were diagnosed with GAD even in the probable GAD group. The most common physical diagnoses among individuals that were diagnosed with GAD in the probable GAD group were headache, constipation, dizziness, asthma, and pain. This finding suggests that it is necessary to determine whether anxiety is involved when treating patients with such physical diseases.
The study results indicate a requirement for raising awareness of GAD among both physicians and the general population, including patients, leading to appropriate consultation behavior, diagnosis, and treatment. The development of a Japanese clinical guideline on GAD is a potential solution.
It is recommended that future research initiatives will be of paramount importance to raise awareness of GAD and develop clinical guidelines in Japan.
Abbreviations
BP, bipolar disorder; CI, confidence interval; COVID-19, Corona Virus Disease 2019; DSM, CSS: Clinical Study Support, Inc., Diagnostic and statistical manual of mental disorders; EQ-5D-5L, EuroQol 5 dimensions 5-level; EQ-VAS, EuroQol Visual Analog Scale; GAD, generalized anxiety disorder; GAD-7, Generalized Anxiety Disorder 7-item; ICD, International Classification of Diseases; IEC, Independent ethics committee; IRB, institutional review board; PHQ-9, Patient Health Questionnaire-9; QOL, quality of life; DeSC, DeSC Healthcare, Inc.; SARI, serotonin2-antagonist / reuptake inhibitor; SAS, Statistical Analysis Software; SNRI, serotonin and norepinephrine reuptake inhibitor; SSRI: selective serotonin reuptake inhibitor; WMH: World Mental Health; WFSBP, World Federation of Societies of Biological Psychiatry; WMHJ, World Mental Health Japan Survey; WPAI-GH, Work Productivity and Activity Impairment Questionnaire Global Health.
Data Sharing Statement
The data that support the findings of this study are available from DeSC., but restrictions apply to the availability of these data, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with the permission of DeSC.
Ethics Approval and Informed Consent
As this survey used only anonymized data, and because Viatris Pharmaceuticals Japan G.K., Clinical Study Support, Inc. (CSS), and the medical experts did not possess or receive data correspondence sheets, it was impossible to identify any individual. In addition, DeSC does not have a correspondence table for the data provided to Viatris Pharmaceuticals Japan G.K., and it is, therefore, impossible to identify individuals from this data. Therefore, no new individual level consent was obtained for the use of the data in this study. However, IRB/IEC approval was obtained from the Kitamachi Clinic Ethical Committee (Tokyo, Japan) on May 15, 2024 (approval No.: LUU10154). Additionally, this survey was conducted in consideration of the Declaration of Helsinki (revised October 2013) by the World Medical Association and the Ethical Guidelines for Medical Research Involving Human Subjects.
Acknowledgments
This work was sponsored and funded by Viatris Pharmaceuticals Japan G.K., Tokyo, Japan. Statistical analysis and medical writing were supported by CSS, Nagoya, Japan, and funded by Viatris Pharmaceuticals Japan G.K.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Viatris Pharmaceuticals Japan G.K.
Disclosure
Satoshi Matsuyama, Keisuke Nomoto, Rikiya Misago, and Shingo Higa are full-time employees of Viatris Pharmaceuticals Japan G.K. Tempei Otsubo has received lecture fees from Viatris Pharmaceuticals Japan G.K.; Takeda Pharmaceutical Co., Ltd.; Otsuka Pharmaceutical; Sumitomo Pharma Co., Ltd.; YoshitomiYakuhin; Mochida; Meiji Seika Pharma Co., Ltd.; Kyowa Pharmaceutical; Lundbeck Japan; and IQVIA. The authors report no other conflicts of interest in this work.
References
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition, text revision (DSM-5-TR®). 2022.
2. Wittchen HU, Carter RM, Pfister H, Montgomery SA, Kessler RC. Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey. Int Clin Psychopharmacol. 2000;15(6):319–328. doi:10.1097/00004850-200015060-00002
3. Allgulander C, Baldwin DS. Pharmacotherapy of generalized anxiety disorder. Mod Trends Pharmacopsych. 2013;29:119–127.
4. Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiatry. 2017;74(5):465–475. doi:10.1001/jamapsychiatry.2017.0056
5. Bandelow B, Lichte T, Rudolf S, Wiltink J, Beutel ME. The diagnosis of and treatment recommendations for anxiety disorders. Dtsch Arztebl Int. 2014;111(27–28):473–480. doi:10.3238/arztebl.2014.0473
6. Katzman MA, Bleau P, Blier P, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry. 2014;14(Suppl 1):S1. doi:10.1186/1471-244X-14-S1-S1
7. Bandelow B, Allgulander C, Baldwin DS, et al. World federation of societies of biological psychiatry (WFSBP) guidelines for treatment of anxiety, obsessive-compulsive and posttraumatic stress disorders - version 3. Part I: anxiety disorders. World J Biol Psych. 2023;24(2):79–117. doi:10.1080/15622975.2022.2086295
8. Slee A, Nazareth I, Bondaronek P, Liu Y, Cheng Z, Freemantle N. Pharmacological treatments for generalised anxiety disorder: a systematic review and network meta-analysis. Lancet. 2019;393(10173):768–777. doi:10.1016/S0140-6736(18)31793-8
9. American Psychiatric Association W, DC. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV.
10. Tajima O. Current status of generalized anxiety disorder (GAD) in Japan—based on a questionnaire with 20,000 respondents in the general public. Jpn J Clin Psychopharmacol. 2004;7:1795–1798.
11. Ishikawa H, Kawakami N, Kessler RC. Lifetime and 12-month prevalence, severity and unmet need for treatment of common mental disorders in Japan: results from the final dataset of world mental health Japan survey. Epidemiol Psychiatr Sci. 2016;25(3):217–229. doi:10.1017/S2045796015000566
12. Ishikawa H, Tachimori H, Takeshima T, et al. Prevalence, treatment, and the correlates of common mental disorders in the mid 2010’s in Japan: the results of the world mental health Japan 2nd survey. J Affect Disord. 2018;241:554–562.
13. Matsuyama S, Otsubo T, Nomoto K, Higa S, Takashio O. Prevalence of generalized anxiety disorder in japan: a general population survey. Neuropsychiatr Dis Treat. 2024;20:1355–1366. doi:10.2147/NDT.S456272
14. Nomoto K, Takashio O, Matsuyama S, Higa S, Otsubo T. Diagnosis and treatment of generalized anxiety disorder in Japan: psychiatric specialist survey. Neuropsychiatr Dis Treat. 2024;20:1001–1010. doi:10.2147/NDT.S456276
15. Altamura AC, Dell’osso B, D’Urso N, Russo M, Fumagalli S, Mundo E. Duration of untreated illness as a predictor of treatment response and clinical course in generalized anxiety disorder. CNS Spectr. 2008;13(5):415–422. doi:10.1017/S1092852900016588
16. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
17. Muramatsu K. An up-to-date letter in the Japanese version of PHQ, PHQ-9, PHQ-15. Graduate School Clin Psychol Niigata Seiryo Univ. 2014;7:35–39.
18. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
19. Herdman M, Gudex C, Lloyd A, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–1736. doi:10.1007/s11136-011-9903-x
20. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–365. doi:10.2165/00019053-199304050-00006
21. Kato S.Psychiatrists’ stigma towards individuals with mental illness: a better understanding of mental illness is needed. Psychiatria et Neurologia Japonica. 2017;119(9):672–685.
22. Otsubo T. Current status and issues of generalized anxiety disorder in Japan. Anxiety Disord Res. 2022;14(1):2–11. doi:10.14389/jsad.14.1_2
23. Victor T, Hu X, Campbell J, White R, Buse D, Lipton R. Association between migraine, anxiety and depression. Cephalalgia. 2010;30(5):567–575. doi:10.1111/j.1468-2982.2009.01944.x
24. Lampl C, Thomas H, Tassorelli C, et al. Headache, depression and anxiety: associations in the Eurolight project. J Headache Pain. 2016;17(1):59. doi:10.1186/s10194-016-0649-2
25. Cheng C, Chan AO, Hui WM, Lam SK. Coping strategies, illness perception, anxiety and depression of patients with idiopathic constipation: a population-based study. Aliment Pharmacol Ther. 2003;18(3):319–326. doi:10.1046/j.1365-2036.2003.01663.x
26. Staab JP, Ruckenstein MJ. Expanding the differential diagnosis of chronic dizziness. Arch Otolaryngol Head Neck Surg. 2007;133(2):170–176. doi:10.1001/archotol.133.2.170
27. ten Thoren C, Petermann F. Reviewing asthma and anxiety. Respir Med. 2000;94(5):409–415. doi:10.1053/rmed.1999.0757
28. Deshmukh VM, Toelle BG, Usherwood T, O’Grady B, Jenkins CR. Anxiety, panic and adult asthma: a cognitive-behavioral perspective. Respir Med. 2007;101(2):194–202. doi:10.1016/j.rmed.2006.05.005
29. de Heer EW, Gerrits MM, Beekman AT, et al. The association of depression and anxiety with pain: a study from NESDA. PLoS One. 2014;9(10):e106907. doi:10.1371/journal.pone.0106907
30. Simon NM. Generalized anxiety disorder and psychiatric comorbidities such as depression, bipolar disorder, and substance abuse. J Clin Psychiatry. 2009;70(Suppl 2):10–14. doi:10.4088/JCP.s.7002.02
31. Ministry of Health LaWoJ. Request for proper use of benzodiazepine receptor agonists. Available from: https://www.mhlw.go.jp/file/05-Shingikai-11121000-Iyakushokuhinkyoku-Soumuka/0000156315.pdf.
32. Pharmaceuticals and Medical Devices Agency. Dependence on benzodiazepine receptor agonists. Available from: https://www.pmda.go.jp/files/000268322.pdf.
33. Mishima K, Takeshima M, Enomoto M. Research on the actual prescription status of psychotropic drugs using large-scale medical fee data. Ministry of health, labour and welfare science research grant, disease and disability countermeasures research field, comprehensive research on disability policy. FY2020 comprehensive research report. Ministry of Health, Labor and Welfare Science Research Results Database. Available from: https://mhlw-grants.niph.go.jp/project/147990.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

