Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 18
Prevalence of Hypertension and Its Associated Factors Among Patients with Type 2 Diabetes in Southern Afghanistan: A Multi-Center Cross-Sectional Study
Authors Stanikzai MH , Amirzada ME, Ishaq N, Kamil KA , Anwary Z, Farzad A , Baray AH, Sayam H
Received 30 October 2024
Accepted for publication 25 February 2025
Published 5 March 2025 Volume 2025:18 Pages 715—725
DOI https://doi.org/10.2147/DMSO.S503725
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rebecca Conway
Muhammad Haroon Stanikzai,1 Mohammad Essa Amirzada,2 Niamatullah Ishaq,3 Kamil Ahmad Kamil,4 Zabihullah Anwary,5 Asadullah Farzad,6 Ahmad Haroon Baray,1 Hadia Sayam1
1Department of Public Health, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan; 2Department of Surgery, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan; 3Department of Radiology, Faculty of Medicine, Kandahar University, Kandahar, Afghanistan; 4Internal Medicine Department, Mirwais Regional Hospital, Kandahar, Afghanistan; 5Clinic Department, Faculty of Medicine, Bost University, Lashkar Gah, Helmand, Afghanistan; 6Para-clinic Department, Faculty of Medicine, Bost University, Lashkar Gah, Helmand, Afghanistan
Correspondence: Muhammad Haroon Stanikzai, Department of Public Health, Faculty of Medicine, Kandahar University, District # 10, Kandahar, 3801, Afghanistan, Tel +93704775578, Email [email protected]
Background: Hypertension among patients with type 2 diabetes results in higher rates of cardiovascular complications and deaths. However, there is limited data on the prevalence of hypertension and its associated factors among patients with type 2 diabetes in Afghanistan.
Objective: Our study aims to determine the prevalence of hypertension and its associated factors among patients with type 2 diabetes in southern Afghanistan.
Methods: This was a multi-center hospital-based cross-sectional study employed from January to June 2024 in southern Afghanistan. A total of 609 randomly selected patients with type 2 diabetes were included in the analysis. Diabetes patients were examined for the presence/absence of hypertension diagnosis using a criterion set by the American Heart Association. The binary logistic regression analysis was performed to test for risk factors associated with hypertension among patients with type 2 diabetes.
Results: Among the 609 patients with diabetes included in the study, 55.3% (95% CI: 51.2%– 59.3%) had hypertension. According to the results of binary logistic regression, female gender [AOR, adjusted odds ratio =1.73, 95% CI (1.09– 2.74)], age of ≥ 50 years [4.35 (2.78– 2.6.81)], having diabetes for five or more years [2.13 (1.37– 3.31)], poor glycemic control [1.80 (1.18– 2.75)], and the presence of depressive symptoms [3.25 (2.59– 4.80)] were associated with hypertension among patients with diabetes.
Conclusion: Due to the high prevalence (55.3%) of hypertension among patients with type 2 diabetes in Afghanistan, it is imperative to develop targeted interventions aimed at early detection and ensuring adequate care, especially for those most at risk for hypertension.
Keywords: Afghanistan, diabetes patients, hypertension, risk factors, type 2 diabetes
Introduction
Hypertension among patients with diabetes is a major public health concern in most developing countries, impacting health outcomes, quality of life, and increasing healthcare costs.1–3 For instance, hypertension in patients with diabetes leads to higher rates of cardiovascular complications and deaths.4,5 Additionally, the overlap between hypertension and diabetes is associated with a reduced quality of life,6,7 and higher healthcare costs.8,9 Given these negative outcomes, research into this issue is warranted.
Previous studies from low and middle-income countries (LMICs) have shown that hypertension is prevalent among patients with type 2 diabetes. For instance, a recent systematic review in Ethiopia found the prevalence of hypertension among patients with diabetes was 55%.10 Hinneh et al reported a higher prevalence (58.1%) of hypertension among diabetes patients in Africa.3 Other studies have indicated hypertension prevalence in the range of 37% to 86% among patients with type 2 diabetes.11–15 In 2022, a single-center study with 321 patients with diabetes in Kabul (Central Afghanistan) found a 70% prevalence of hypertension.16
Many factors affect the prevalence of hypertension among patients with type 2 diabetes. A meta-analysis assessing the risk factors for hypertension among patients with diabetes showed that urban residency increased the likelihood of hypertension.10 Another meta-analysis reported that female gender, increasing age, urban residence, longer duration of illness, and higher Body Mass Index (BMI) influence the prevalence of hypertension in patients with diabetes.3 Other important risk factors include low wealth status, insufficient physical activity, smoking, alcohol consumption, limited knowledge about diabetes, onset of renal disease, non-adherence to medications, and poor glycemic control.11,13,14,17–19 Moreover, mental health conditions predispose diabetes patients to diabetes-related complications, including hypertension.20–22 In Afghanistan, old age and female gender were found to have a significant effect on hypertension prevalence in patients with diabetes.16
However, research regarding the prevalence and correlates of hypertension among patients with diabetes is still at its earliest stages in Afghanistan.16,23 A study that includes data from multiple centers and examines a wide range of factors is a crucial first step to fully comprehend the hypertension phenomena among diabetes patients in Afghanistan. Therefore, this multi-center cross-sectional study aimed to determine the prevalence and associated factors of hypertension among patients with type 2 diabetes in southern Afghanistan.
Methods
Study Settings and Design
This cross-sectional study was conducted between January and June 2024 and carried out in three public hospitals in southern Afghanistan. Patients were selected from three hospitals: Mirwais Regional Hospital (Kandahar province), Kandahar Teaching Hospital (Kandahar province), and Bost Teaching Hospital (Helmand province). All study sites provided diabetes care for the public sector and were selected for convenience. These three hospitals are public healthcare facilities with the capacity to offer specialized diabetes care in southern Afghanistan.
Study Population
The diagnosis of diabetes was based on the guidelines of the American Diabetes Association.24 Patients who were at least 18 years of age and had been diagnosed with type 2 diabetes for at least a year were considered to meet the inclusion criteria. The study excluded pregnant women and patients with a critical condition.
Sample Size and Sampling
The sample size for this study was calculated using the formula (N = Z2 x (P) x (1-P)/ d2), taking the following parameters into consideration: prevalence of hypertension among patients with diabetes in Afghanistan (p=0.05, maximum estimates), a 95% confidence interval (CI), 5% margin of error, and a 10% non-response rate. It was multiplied by 1.5 (design effect), resulting in a final estimated sample size of 630. We used and analyzed data with complete information, which means a list-wise deletion approach was used and data with missing values were excluded from analysis (4 patients were excluded).
The patients were selected using the random sampling technique. Initially, the total sample size was proportionally allocated to the three study sites based on the number of diabetes patients served at medical Outpatient Departments (OPDs) during the month before the start of the data collection. This resulted in 350 patients allocated to MRH, 175 to Bost Teaching Hospital, and 105 to Kandahar Teaching Hospital. Subsequently, at the three hospitals, the clinical staff provided the lists of patients who were receiving treatment for diabetes in the outpatient departments of the study sites. Patients who met the inclusion criteria were randomly selected using Microsoft Excel software.
Study Variables
Dependent Variable
The dependent variable was the presence (1) or absence (0) of hypertension diagnosis among patients with type 2 diabetes. Hypertension was defined as a systolic blood pressure (SBP) of ≥ 140 mm Hg and/or diastolic blood pressure (DBP) of ≥ 90 mm Hg, and/or taking medicines for hypertension treatment.25 We followed the guidelines set by the American Heart Association for blood pressure measurement.25 Blood pressure recordings were obtained in a sitting position after 10 minutes of rest. We used a manual sphygmomanometer, and the average of three intermittent (5-minute intervals) readings was recorded.
Independent Variables
To examine the factors determining hypertension presence among patients with diabetes, we designed the study questionnaire comprising questions on sociodemographic characteristics, clinical, and other related information that may influence blood pressure. The sociodemographic characteristics we examined included age (< 40 years, 40–49 years, ≥ 50 years), sex (female, male), residence (urban, rural), education level (no formal education, religious studies, primary, secondary/higher), marital status (single, married, divorced, widowed), employment (formally employed, privately employed, self-employed, housewife, unemployed), household members (2–5, > 5), monthly household income in Afghanis (< 10,000, ≥ 10,000), and BMI. Body weight was assessed using BMI classification (normal, underweight, overweight, obese) based on the WHO criteria for Asians.26
The clinical and other related information gathered included disease duration (< 5 years, ≥ 5 years), family history of hypertension (yes, no), exposure to diabetes health education (yes, no), adherence to diet (yes, no), engagement in regular physical activity (yes, no), number of anti-diabetic medications (one, more than one), currently smoking (yes, no), and glycemic control status (good, poor). Glycemic control status was defined as “poor” for patients with HbA1C ≥ 7 and “good” for those with HbA1C < 7.27
Depression in patients with diabetes was assessed using the PHQ-9 scale, which included the frequency that patients were bothered by nine depressive symptoms within the last two weeks.28 Each depressive symptom had 0 to 3 points, yielding a total score of 27. The total score of 0–4 were considered no/minimal depression, 5–9 as mild depression, 10–14 moderate depression, 15–19 severe depression, and ≥ 20 extremely severe depression. A score of ≥ 5 indicated “with depressive symptoms” in our study. Previous studies have shown that the Pashtu version of PHQ-9 has acceptable reliability among patients with chronic conditions.29,30 In the present study, we found very good internal consistency, with an alpha coefficient of 0.88.
Data Collection
We used a structured questionnaire, which included close-ended questions on sociodemographics, clinical, and other related information. Drafted initially in English, the questionnaire was translated into Pashtu, Afghanistan’s national language. Additionally, the questionnaire was pre-tested among 30 patients with diabetes in a non-participating health center (Fazli Curative Center) to ascertain its reliability.
To avoid coercion of patients, a team of six medical doctors (three males and three females), with a research background and who were not health workers, conducted the interviews. Interviewers received a one-day training specific to this study. Training included sessions on sampling procedures, interviewing techniques, blood pressure and weight measurement, and filling out questionnaires. Additionally, patients underwent laboratory tests for blood glucose and HbA1C. On a regular basis, the principal investigators monitored the data collection procedures at the study sites.
Statistical Analysis
All analyses were performed using the SPSS version 27 statistical software. Descriptive statistics were employed to explain the sociodemographic, clinical, and other related characteristics of the study participants. We have also provided the prevalence of hypertension (Figure 1). After a comprehensive literature review,10,11,19,31–36 we included relevant independent variables in the bivariate analysis. For the multivariable analysis, we retained the variables that had a p-value of less than 0.25 in the bivariate analysis.37,38 We obtained odds ratio and 95% CI [OR (95% CI)] from the bivariate and multivariable logistic regression analyses. A p-value of <0.05 was considered significant.
 |
Figure 1 Prevalence of hypertension among patients with type 2 diabetes (n=609). |
Results
A total of 609 patients with diabetes were included in the analysis (response rate 96.2%), and the majority of patients were male (71.8%). Most participants were aged ≥ 50 years (66.2%), married (71.4%), lived in urban areas (63.4%), and had no formal education (79.1%). About half of the participants were unemployed (51.6%), 95.2% (580) lived in households with more than five members, and 54% (329) had a monthly household income of less than 10000 (150 USD) per month. In terms of BMI, nearly two-thirds were overweight (37.2%; 226) or obese (23.9%; 146). Further details are presented in Table 1.
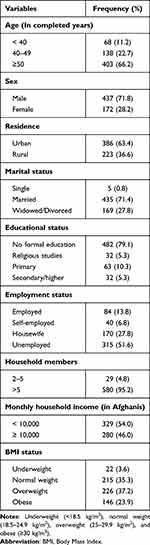 |
Table 1 Sociodemographic Characteristics of the Study Participants (n=609) |
As shown in Table 2, 58% (353) of participants had diabetes for five or more years, 55.8% (340) had a positive family history of hypertension, and the vast majority of the participants (81.3%) were on multiple anti-diabetic medications. Moreover, one in four patients (24.1%) received health education on diabetes, 325 (53.4%) adhered to dieting, and 226 (37.1%) engaged in regular physical activity. Further, 96 (15.8%) were currently smoking and 352 (57.8%) had poor glycemic control. Based on the PHQ-9 score, the vast majority of the participants had depressive symptoms (69.3%). The percentage of patients with mild, moderate, severe, and extremely severe depression symptoms is presented in Table 2.
 |
Table 2 Clinical and Other Related Characteristics of the Study Participants (n=609) |
Out of the 609 patients with diabetes included in the study, 55.3% (95% CI: 51.2%–59.3%) were found to have hypertension (Figure 1).
According to the results of binary logistic regression analysis, female gender [AOR=1.73, 95% CI (1.09–2.74)], age of ≥ 50 years [4.35 (2.78–2.6.81)], having diabetes for five or more years [2.13 (1.37–3.31)], poor glycemic control [1.80 (1.18–2.75)], and the presence of depressive symptoms [3.25 (2.59–4.80)] were associated with hypertension among patients with diabetes (Table 3).
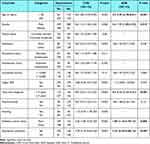 |
Table 3 Logistic Regression Analysis Results on Factors Associated with Hypertension Among Type 2 Diabetes Patients: Crude and Adjusted Odds Ratios with 95% CIs |
Discussion
This study investigated the prevalence and correlates of hypertension among patients with type 2 diabetes in southern Afghanistan. The findings revealed that 55.3% of participants had hypertension. Several factors were significantly associated with hypertension, including female gender, increasing age, longer duration of illness, poor glycemic control, and the presence of depressive symptoms.
In this study, we found that 55.3% of patients had hypertension. This finding was consistent with studies assessing the prevalence of hypertension among diabetes patients in many LMICs.3,10,11,18,39 However, some studies have reported a high prevalence of hypertension, ranging from 65% to 80%.14,40,41 The only available evidence in Afghanistan is from a study that was conducted in Kabul (urban population), where a higher prevalence (75%) of hypertension was found. This divergence could be due to the fact that urban diabetes patients have a higher risk of hypertension.3,10,42 Nonetheless, the prevalence of hypertension is higher than in the general population (55.4% vs 25%).43 Given the high prevalence reported in this study, it is imperative to integrate hypertension screening into diabetes management programs. Additionally, it is important to note that the data in the current study is mainly collected from public healthcare facilities in southern Afghanistan, and did not include private healthcare facilities that also offer diabetes care to a wider population in the study area. Studies in Afghanistan have shown that the quality of care for non-communicable diseases in often suboptimal in the public sector.44,45 Therefore, future studies with a larger sample, including private healthcare facilities and community settings, would provide a better understanding.
The age differences we found in our study are similar to those of other studies performed in LMICs, which found that the prevalence of hypertension was higher in older patients with diabetes.3,18 A systematic review encompassing 41 studies across Africa concluded that old age (≥50 years) is a major contributor to the high prevalence of hypertension among patients with diabetes.3 The high risk of hypertension in this age group may be due to age-related changes in blood vessels, decreased elasticity, and cumulative effects of metabolic disturbances associated with diabetes.2,32,46 This finding emphasizes the importance of prioritizing targeted hypertension prevention and management strategies for older patients.
The current findings observed that female patients with diabetes were more likely to have hypertension. This result is similar to previous studies conducted in Afghanistan,16 and Iran.47 However, other studies have reported that hypertension is more prevalent among male patients with diabetes.3,14 In Afghanistan, cultural barriers, women’s decision-making autonomy, wealth, and education have consistently affected the access and utilization of healthcare services by Afghan women, which may be contributing factors.48–50 The recent sociopolitical challenges could further compound these vulnerabilities.51 Therefore, addressing the underlying determinants influencing women’s choices regarding access and utilization of healthcare services is paramount, especially in regions like Afghanistan.
This study found that the likelihood of hypertension increased with the longer duration of illness. Patients who had diabetes for five or more years were 2.1 times more likely to have hypertension compared to patients who had diabetes for a shorter duration. This finding is in agreement with previous studies done in Ethiopia,31 Cameron,14 Iraq,15 and Africa.3,52 In patients with diabetes, prolonged exposure to elevated blood sugar levels results in vascular damage, thereby leading to high blood pressure.33 Additionally, a longer duration of diabetes is associated with several other complications, especially in patients with uncontrolled diabetes.33,53 Therefore, clinicians should be aware of the greater risk of hypertension and other complications in diabetes patients with a longer duration of illness.
The odds of hypertension were greater in patients with poor glycemic control than in those with good control. The association between poor glycemic control and hypertension is previously reported in studies from LMICs.3,31,32,35 Poor glycemic control remains a common problem that contributes significantly to diabetes-related complications and deaths, particularly in LMICs.1,54 In this study, a staggering proportion (57.8%) of patients had uncontrolled diabetes. To our knowledge, no previous study has reported on glycemic control status and its contributing factors among Afghan patients with diabetes. Hence, further research is needed to reveal the burden of uncontrolled diabetes in Afghanistan.
The final important variable which identified a significant association with hypertension was depression symptoms. The findings revealed that diabetes patients with depressive symptoms are more likely to have hypertension than those who had no/minimal depression symptoms. Depression is a common mental health condition in patients with chronic diseases.30,36,55 Moreover, depression symptoms are also associated with poorer outcomes in patients with hypertension and diabetes.34,56,57 Considering the high prevalence of depression symptoms in this study, it is imperative to screen diabetes patients for depression symptoms, and those at risk should be given bio-psycho-social support.
Limitations
This study has some limitations. First, most data in this multi-center study were self-reported, which could affect the validity of the results. Second, due to resource constraints, we were not able to assess dyslipidemia in our sample, which is a potential risk factor for hypertension among patients with diabetes. Therefore, future studies should investigate including this and other relevant variables (ie, medication adherence, dietary patterns, concomitant medical conditions, and corticosteroid use) in their analysis. Third, the sample was drawn from three public hospitals in southern Afghanistan. Hence, the findings may not be generalizable to the entire country. Therefore, future studies should consider a larger sample size and diabetes patients from different settings across Afghanistan. Finally, the cross-sectional nature of the data did not allow for causal inferences regarding factors that may affect hypertension prevalence among diabetic patients.
Conclusion
Our study revealed that hypertension is highly prevalent (55.3%) among patients with type 2 diabetes in southern Afghanistan. Older age, female gender, longer duration of diabetes, poor glycemic control, and the presence of depressive symptoms were determining factors for the presence of hypertension among patients with diabetes. Given the high prevalence of hypertension among patients with type 2 diabetes in Afghanistan, it is imperative to integrate hypertension screening into diabetes management programs.
Data Sharing Statement
The primary data used to support the findings of this study are available from the corresponding author upon request.
Ethical Approval
The study was approved by the Ethics Committee of the Faculty of Medicine at Kandahar University. The ethics committee also approved the use of either written or verbal consent in the study since many of the patients could neither read nor write. Informed consent, either written or oral, was obtained from all participants prior to their inclusion in the study. Moreover, the study was conducted according to the ethical principles outlined in the Declaration of Helsinki and the Good Clinical Practice (GCP) guidelines.
Funding
The authors received no specific funding for this work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Naghavi M, Ong KL, Aali A, et al. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet. 2024;403(10440):2100–2132. doi:10.1016/s0140-6736(24)00367-2
2. Brauer M, Roth GA, Aravkin AY, et al. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet. 2024;403(10440):2162–2203. doi:10.1016/s0140-6736(24)00933-4
3. Hinneh T, Akyirem S, Bossman IF, et al. Regional prevalence of hypertension among people diagnosed with diabetes in Africa, a systematic review and meta-analysis. PLOS Global Public Health. 2023;3(12):e0001931. doi:10.1371/journal.pgph.0001931
4. Sunkara N, Ha C. Hypertension in diabetes and the risk of cardiovascular disease. Cardiovasc Endocrinol. 2017;6(1):33–38. doi:10.1097/xce.0000000000000114
5. Tashko G, Gabbay RA. Evidence-based approach for managing hypertension in type 2 diabetes. Integr Blood Press Control. 2010;3:31–43. doi:10.2147/ibpc.s6984
6. Esubalew H, Belachew A, Seid Y, Wondmagegn H, Temesgen K, Ayele T. Health-related quality of life among type 2 diabetes mellitus patients using the 36-item short form health survey (SF-36) in central Ethiopia: a multicenter study. Diabetes Metab Syndr Obes. 2024;17:1039–1049. doi:10.2147/dmso.S448950
7. Adriaanse MC, Drewes HW, van der Heide I, Struijs JN, Baan CA. The impact of comorbid chronic conditions on quality of life in type 2 diabetes patients. Qual Life Res. 2016;25(1):175–182. doi:10.1007/s11136-015-1061-0
8. Tharkar S, Satyavani K, Viswanathan V. Cost of medical care among type 2 diabetic patients with a co-morbid condition—Hypertension in India. Diabetes Res Clin Pract. 2009;83(2):263–267. doi:10.1016/j.diabres.2008.11.027
9. Amon S, Aikins M, Haghparast-Bidgoli H, et al. Household economic burden of type-2 diabetes and hypertension comorbidity care in urban-poor Ghana: a mixed methods study. BMC Health Serv Res. 2024;24(1):1028. doi:10.1186/s12913-024-11516-9
10. Haile TG, Mariye T, Tadesse DB, Gebremeskel GG, Asefa GG, Getachew T. Prevalence of hypertension among type 2 diabetes mellitus patients in Ethiopia: a systematic review and meta-analysis. Int Health. 2023;15(3):235–241. doi:10.1093/inthealth/ihac060
11. Alsaadon H, Afroz A, Karim A, et al. Hypertension and its related factors among patients with type 2 diabetes mellitus – a multi-hospital study in Bangladesh. BMC Public Health. 2022;22(1):198. doi:10.1186/s12889-022-12509-1
12. Motedayen M, Sarokhani D, Meysami A, Jouybari L, Sanagoo A, Hasanpour Dehkordi A. The prevalence of hypertension in diabetic patients in Iran; a systematic review and meta-analysis. J Nephropathol. 2018;7(3):137–144. doi:10.15171/jnp.2018.32
13. Santra A, Mallick A. Prevalence of hypertension among individuals with diabetes and its determinants: evidences from the national family health survey 2015-16, India. Ann Hum Biol. 2022;49(2):133–144. doi:10.1080/03014460.2022.2072525
14. Kemche B, Saha Foudjo BU, Fokou E. Risk factors of hypertension among diabetic patients from Yaoundé Central Hospital and Etoug-Ebe Baptist Health Centre, Cameroon. J Diabetes Res. 2020;2020(1):1853516. doi:10.1155/2020/1853516
15. Mansour AA. Prevalence and control of hypertension in Iraqi diabetic patients: a prospective cohort study. Open Cardiovasc Med J. 2012;6(1):68–71. doi:10.2174/1874192401206010068
16. Naseri MW, Esmat HA, Bahee MD. Prevalence of hypertension in Type-2 diabetes mellitus. Ann Med Surg. 2022;78:103758. doi:10.1016/j.amsu.2022.103758
17. Muleta S, Melaku T, Chelkeba L, Assefa D. Blood pressure control and its determinants among diabetes mellitus co-morbid hypertensive patients at Jimma University Medical Center, South West Ethiopia. Clinical Hypertension. 2017;23(1):29. doi:10.1186/s40885-017-0085-x
18. Abdissa D, Kene K. Prevalence and determinants of hypertension among diabetic patients in Jimma University Medical Center, Southwest Ethiopia, 2019. Diabetes Metab Syndr Obes. 2020;13:2317–2325. doi:10.2147/dmso.S255695
19. Kenore Y, Abrha S, Yosef A, Gelgelu TB. Determinants of hypertension among patients with diabetes mellitus in public hospitals of Kembata Tambaro Zone, South nations nationalities and peoples region, Ethiopia, 2021; A case control study. J Multidiscip Healthc. 2022;15:2141–2152. doi:10.2147/jmdh.S379293
20. AlKhathami AD, Alamin MA, Alqahtani AM, Alsaeed WY, AlKhathami MA, Al-Dhafeeri AH. Depression and anxiety among hypertensive and diabetic primary health care patients. Could patients’ perception of their diseases control be used as a screening tool? Saudi Med J. 2017;38(6):621–628. doi:10.15537/smj.2017.6.17941
21. Udedi M, Pence B, Kauye F, Muula AS. The effect of depression management on diabetes and hypertension outcomes in low- and middle-income countries: a systematic review protocol. Syst Rev. 2018;7(1):223. doi:10.1186/s13643-018-0896-1
22. Egede LE. Effect of depression on self-management behaviors and health outcomes in adults with type 2 diabetes. Curr Diabetes Rev. 2005;1(3):235–243. doi:10.2174/157339905774574356
23. Stanikzai MH, Wafa MH, Rahimi BA, Sayam H. Conducting health research in the current afghan society: challenges, opportunities, and recommendations. Risk Manag Healthc Policy. 2023;16:2479–2483. doi:10.2147/rmhp.S441105
24. The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–20. doi:10.2337/diacare.26.2007.s5
25. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Hypertension. 2018;71(6):e13–e115. doi:10.1161/hyp.0000000000000065
26. WHO. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi:10.1016/s0140-6736(03)15268-3.
27. Qaseem A, Vijan S, Snow V, Cross JT, Weiss KB, Owens DK. Glycemic control and type 2 diabetes mellitus: the optimal hemoglobin A1c targets. A guidance statement from the American college of physicians. Ann Intern Med. 2007;147(6):417–422. doi:10.7326/0003-4819-147-6-200709180-00012
28. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi:10.1046/j.1525-1497.2001.016009606.x
29. Stanikzai MH, Ishaq N, Zafar MN, et al. Depression symptoms among Afghan TB patients: a multi-center study. Indian J Tuberc. 2024;71:S264–S268. doi:10.1016/j.ijtb.2024.08.016
30. Stanikzai MH, Zafar MN, Akbari K, Baray AH, Sayam H. Prevalence and predictors of depression symptoms among afghan hypertensive patients: secondary analysis of a multi-center cross-sectional study. Integr Blood Press Control. 2024;17:41–50. doi:10.2147/ibpc.S488064
31. Akalu Y, Belsti Y. Hypertension and its associated factors among type 2 diabetes mellitus patients at Debre Tabor general hospital, Northwest Ethiopia. Diabetes Metab Syndr Obes. 2020;13:1621–1631. doi:10.2147/dmso.S254537
32. Chew BH, Shariff Ghazali S, Ismail M, Haniff J, Bujang MA. Age ≥60years was an independent risk factor for diabetes-related complications despite good control of cardiovascular risk factors in patients with type 2 diabetes mellitus. Exp Gerontology. 2013;48(5):485–491. doi:10.1016/j.exger.2013.02.017
33. Iradukunda A, Kembabazi S, Ssewante N, Kazibwe A, Kabakambira JD. Diabetic complications and associated factors: a 5-year facility-based retrospective study at a tertiary hospital in Rwanda. Diabetes Metab Syndr Obes. 2021;14:4801–4810. doi:10.2147/dmso.S343974
34. Lin EH, Rutter CM, Katon W, et al. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33(2):264–269. doi:10.2337/dc09-1068
35. Sheleme T, Mamo G, Melaku T, Prevalence ST. Patterns and predictors of chronic complications of diabetes mellitus at a large referral hospital in Ethiopia: a prospective observational study. Diabetes Metab Syndr Obes. 2020;13:4909–4918. doi:10.2147/dmso.S281992
36. Tran NMH, Nguyen QNL, Vo TH, Le TTA, Ngo NH. Depression among patients with type 2 diabetes mellitus: prevalence and associated factors in Hue City. Vietnam Diabetes Metab Syndr Obes. 2021;14:505–513. doi:10.2147/dmso.S289988
37. Chowdhury MZI, Turin TC. Variable selection strategies and its importance in clinical prediction modelling. Fam Med Comm Health. 2020;8(1):e000262. doi:10.1136/fmch-2019-000262
38. Grant SW, Hickey GL, Head SJ. Statistical primer: multivariable regression considerations and pitfalls†. Eur J Cardiothorac Surg. 2018;55(2):179–185. doi:10.1093/ejcts/ezy403
39. Mwimo J, Kimondo FC, Mboya IB. Prevalence of hypertension and associated factors among diabetic patients in Kilimanjaro region, northern Tanzania: a hospital-based cross-sectional study. Clin Epidemiol Global Health. 2023;23:101387. doi:10.1016/j.cegh.2023.101387
40. Muddu M, Mutebi E, Ssinabulya I, Kizito S, Mondo CK. Hypertension among newly diagnosed diabetic patients at Mulago national referral hospital in Uganda: a cross sectional study. Cardiovasc J Afr. 2018;29(4):218–224. doi:10.5830/cvja-2018-015
41. Nouh F, Omar M, Younis M. Prevalence of hypertension among diabetic patients in Benghazi: a study of associated factors. Asian J Med Health. 2017;6(4):1–11. doi:10.9734/AJMAH/2017/35830
42. Akhtar S, Nasir JA, Javed A, et al. The prevalence of diabetes in Afghanistan: a systematic review and meta-analysis. BMC Public Health. 2021;21(1):941. doi:10.1186/s12889-021-10993-5
43. Dadras O, Stanikzai MH, Jafari M, Tawfiq E. Risk factors for non-communicable diseases in Afghanistan: insights of the nationwide population-based survey in 2018. J Health Popul Nutr. 2024;43(1):129. doi:10.1186/s41043-024-00625-0
44. Neyazi N, Mosadeghrad AM, AbouZeid A. Non-communicable diseases in Afghanistan: a silent tsunami. Lancet. 2023;401(10393):2035–2036. doi:10.1016/S0140-6736(23)01071-1
45. Neyazi N, Mosadeghrad AM, Afshari M, Isfahani P, Safi N. Strategies to tackle non-communicable diseases in Afghanistan: a scoping review. Front Public Health. 2023;11:982416. doi:10.3389/fpubh.2023.982416
46. Acelajado MC. Optimal management of hypertension in elderly patients. Integr Blood Press Control. 2010;3:145–153. doi:10.2147/ibpc.S6778
47. Taheri A, Khezri R, Dehghan A, Rezaeian M, Aune D, Rezaei F. Hypertension among persons with type 2 diabetes and its related demographic, socioeconomic and lifestyle factors in the Fasa cohort study. Sci Rep. 2024;14(1):18892. doi:10.1038/s41598-024-69062-7
48. Ezadi Z, Mohammadi N, Sarwari R, Jafari SM. Afghan women and access to health care in the past 25 years. eClinicalMedicine. 2022;43:101235. doi:10.1016/j.eclinm.2021.101235
49. Harsch S, Jawid A, Jawid ME, Saboga Nunes L, Sahrai D, Bittlingmayer UH. The relationship of health literacy, wellbeing and religious beliefs in neglected and unequal contexts—Results of a survey study in central Afghanistan. Health Promot J Austr. 2021;32(S1):80–87. doi:10.1002/hpja.419
50. Stanikzai MH, Wafa MH, Akbari K, et al. Afghan medical students’ perceptions, and experiences of their medical education and their professional intentions: a cross-sectional study. BMC Medl Educ. 2023;23(1):569. doi:10.1186/s12909-023-04577-7
51. Saboor L, Ahmad L, Ahmad A. The bleak future of Afghan women’s health under the Taliban. Lancet. 2022;399(10328):893–894. doi:10.1016/S0140-6736(22)00283-5
52. Ageru TA, Le CN, Wattanapisit A, et al. Diabetes self-care intervention strategies and their effectiveness in Sub-Saharan Africa: a systematic review. PLoS One. 2024;19(10):e0305860. doi:10.1371/journal.pone.0305860
53. Zoungas S, Woodward M, Li Q, et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. 2014;57(12):2465–2474. doi:10.1007/s00125-014-3369-7
54. Bitew ZW, Alemu A, Jember DA, et al. Prevalence of glycemic control and factors associated with poor glycemic control: a systematic review and meta-analysis. Inquiry. 2023;60:00469580231155716. doi:10.1177/00469580231155716
55. Gebre BB, Deribe B, Abeto M. Magnitude and associated factors of depression among hypertensive patients attending treatment follow up in chronic OPD at Hawassa University Comprehensive Specialized Hospital, Hawassa, Southern Ethiopia. Integr Blood Press Control. 2020;13:31–39. doi:10.2147/ibpc.S240015
56. Baray AH, Stanikzai MH, Wafa MH, Akbari K. High prevalence of uncontrolled hypertension among Afghan hypertensive patients: a multicenter cross-sectional study. Integr Blood Press Control. 2023;16:23–35. doi:10.2147/ibpc.S417205
57. Stanikzai MH, Wafa MH, Tawfiq E, et al. Predictors of non-adherence to antihypertensive medications: a cross-sectional study from a regional hospital in Afghanistan. PLoS One. 2023;18(12):e0295246. doi:10.1371/journal.pone.0295246
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Prevalence of Hypertension and Its Associated Risk Factors Among Patients with Rheumatoid Arthritis in the Kingdom of Saudi Arabia
Al-Ahmari AK
International Journal of General Medicine 2022, 15:6507-6517
Published Date: 8 August 2022
Prevalence of Hypertension and Its Association with Cardiovascular Risk Factors in College Students in Hunan, China
Li M, Cui X, Meng Y, Cheng M, He J, Yuan W, Ni J, Liu J
International Journal of General Medicine 2023, 16:411-423
Published Date: 3 February 2023
A Multifactorial Risk Score System for the Prediction of Diabetic Kidney Disease in Patients with Type 2 Diabetes Mellitus
Hui D, Zhang F, Lu Y, Hao H, Tian S, Fan X, Liu Y, Zhou X, Li R
Diabetes, Metabolic Syndrome and Obesity 2023, 16:385-395
Published Date: 10 February 2023
Leu72Met Polymorphism in Ghrelin Gene: A Potential Risk Factor for Hypertension in Type 2 Diabetes Patients
Buraczynska M, Golacki J, Zaluska W
Diabetes, Metabolic Syndrome and Obesity 2023, 16:557-564
Published Date: 1 March 2023
Knowledge of Cardiovascular Disease Risk Factors and Its Primary Prevention Practices Among the Saudi Public – A Questionnaire-Based Cross-Sectional Study
Bashatah A, Syed W, Al-Rawi MBA
International Journal of General Medicine 2023, 16:4745-4756
Published Date: 20 October 2023

