Back to Journals » Journal of Inflammation Research » Volume 18
Prognostic Value of Inflammatory and Nutritional Indicators in Non-Metastatic Soft Tissue Sarcomas
Authors Yan Y, Zhang Y, Chen Y , Zhong G, Huang W, Zhang Y
Received 28 October 2024
Accepted for publication 20 January 2025
Published 10 February 2025 Volume 2025:18 Pages 1941—1950
DOI https://doi.org/10.2147/JIR.S501079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Yuan Yan,1– 3,* Yunhui Zhang,1– 3,* Yonghan Chen,1– 3,* Guoqing Zhong,2,3 Wenhan Huang,2,3 Yu Zhang1– 3
1School of Medicine, South China University of Technology, Guangzhou, Guangdong, People’s Republic of China; 2Department of Orthopaedics Oncology, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 3School of Materials Science and Engineering (National Engineering Research Center for Tissue Restoration and Reconstruction), South China University of Technology, Guangzhou, Guangdong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yu Zhang; Wenhan Huang, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Zhongshan 2nd Road, Guangzhou, Guangdong, People’s Republic of China, Email [email protected]; [email protected]
Background: Soft tissue sarcoma (STS) has lacked reliable prognostic indicators. This study evaluates blood-based inflammatory and nutritional indexes to identify good predictors for STS outcomes. These indicators included neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), lymphocyte-to-monocyte ratio (LMR), systemic inflammation response index (SIRI), lymphocyte-to-monocyte ratio (PNI), albumin-to-globulin ratio (AGR), and platelet-to-albumin ratio (PAR).
Methods: A total of 93 were included, and blood indexes were measured preoperatively. Univariate and multivariate regression analyses identified significant predictors, and model performance was assessed using the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), Concordance Index (C-index), and Likelihood Ratio Chi-Square (LR_χ 2).
Results: Univariate analysis indicated that NLR, PLR, LMR, SIRI, AGR, and PAR show potentially significant differences (P< 0.01), except for PNI. Further analysis showed that SIRI and AGR have a high C-index, LR_χ 2, and − 2 log-likelihood, lower AIC and BIC, indicating a better model fit for overall survival (OS) and disease-free survival (DFS). The combination index of the SIRI+AGR+Enneking stage achieved the best accuracy (C-index: 0.751 for DFS; C-index: 0.755 for OS). Multivariate regression showed higher Enneking staging (HR=2.720, P=0.038), lower AGR (HR=2.091, P=0.014), and higher SIRI (HR=2.078, P=0.034) as independent prognostic factors for DFS. Meanwhile, low AGR (HR=3.729, P=0.034), and high SIRI (HR=3.729, P=0.016) remained independent prognostic factors for OS.
Conclusion: Preoperative SIRI is a better predictive index compared to NLR, PLR, and LMR. Preoperative SIRI and AGR are independent risk factors for both DFS and OS. The combination index of the SIRI+AGR+Enneking stage provides a more robust prediction of clinical prognosis in STS patients.
Keywords: soft tissue sarcoma, prognostic index, inflammatory, survival analysis
Introduction
Soft tissue sarcoma (STS) is a rare and heterogeneous group of malignant tumors, characterized by over 50 subtypes, comprising only 1% of all cancers.1,2 Despite advances in multimodal treatment, the prognosis for STS, particularly high-grade tumors, remains poor. Studies indicate a recurrence rate as high as 35%,2,3 with a five-year survival rate ranging between 50% and 70%.4,5 Previous large-scale cohort studies have identified several prognostic factors related to STS, including age, tumor size, depth of invasion, sites, pathological grading, and surgical margins.2,3
Inflammation-related closely to the regulation of the tumor microenvironment and can influence various life processes of tumor cells. Reportedly, inflammation is implicated in regulating the tumor microenvironment, influencing cell proliferation, migration, invasion, and immune suppression, thereby driving tumor progression.6 Several inflammation-related markers, such as the neutrophil–lymphocyte ratio (NLR), platelet–lymphocyte ratio (PLR), and lymphocyte–monocyte ratio (LMR), the systemic inflammation response index (SIRI), have been shown to correlate with the prognosis of various cancer patients, such as gastrointestinal tumors, lymphoma, lung cancer, breast cancer, pancreatic cancer or sarcoma.7–14
In addition, some markers related to inflammation, which are also considered related to nutrition or coagulation, have been used for prognosis prediction, such as the Prognostic Nutritional Index (PNI), Platelet/Albumin Ratio (PAR), and Albumin-to-Globulin Ratio (AGR). PNI was considered a superior nutritional and immune prognostic index.15 PAR is an index involving the counts of albumin and platelets. Platelets can influence tumor occurrence and progression through their involvement in coagulation, promotion of inflammatory responses, and angiogenesis.16,17 For example, a study indicates platelets can regulate tumor angiogenesis through the VGFR-integrin pathway.18 The AGR, involving the counts of albumin and globulin, can comprehensively evaluate the nutritional and inflammatory status of the patient,19,20 and has been used to predict mortality or survival in prostate cancer and colon cancer.21,22
Interestingly, the majority of these indicators claim to have good predictive value; however, there are clear similarities or significant correlations among them. It remains unclear which ones are more suitable or superior for predicting the prognosis of soft tissue sarcoma. The study aims to explore the prognostic values of NLR, PLR, LMR, SIRI, PNI, AGR, and PAR in STS patients, and to further compare these markers to provide a more accurate prognostic assessment.
Materials and Methods
Study Design and Subjects
The flowchart of inclusion and exclusion is presented in Figure 1. The study included pathologically confirmed soft tissue sarcomas, excluding cases with distant metastasis. The study initially included 118 patients, of whom 93 were ultimately enrolled between January 1, 2016, and December 30, 2022. Exclusions were due to 4 patients having metastases at diagnosis, 18 being diagnosed with chondrosarcoma, and 2 being lost to follow-up.
 |
Figure 1 Inclusion and exclusion criteria flowchart. |
Data Collection
Demographics and clinical characteristics include gender, age, maximum tumor diameter, primary tumor site, histological type, pathological grade, stage, sites and times of metastasis, Musculoskeletal Tumor Society (AJCC) stage,23 American Joint Committee on Cancer staging (MSTS)/Enneking stage,24 etc. Laboratory blood indicators were collected based on preoperative test results, including electrolytes, total protein, albumin, globulin, C-reactive protein, white blood cell count, red blood cell count, hemoglobin, platelet count, neutrophil count, lymphocyte count, and monocyte count. Overall survival (OS) was defined from the time of pathological diagnosis to the event of tumor-specific death or last follow-up. Disease-free survival (DFS) was defined from the time of surgery to the event of tumor recurrence or metastasis.
Calculation Methods of Blood Indicators
1) NLR=Neutrophil Count/Lymphocyte count (×109/L) and lymphocytes (×109/L) from the complete blood count);
2) PLR=Platelet Count/Lymphocyte Count;
3) LMR=Monocyte Count/Lymphocyte Count (LMR is calculated using the absolute values of lymphocytes and monocytes (×109/L));
4) SIRI=Neutrophil Count × Monocyte Count/Lymphocyte Count;
5) PNI=10×Serum Albumin (g/dL)+0.005×Lymphocyte Count (/mm3);
6) AGR=Serum Albumin/Globulin (globulin is calculated as total protein minus serum albumin);
7) PAR=Platelet Count/Serum Albumin.
Statistical Analysis
Continuous variables were presented as mean ± standard deviation, and categorical variables were presented as frequencies and percentages. The primary and secondary outcomes were OS and DFS, respectively. Kaplan–Meier curves were used to visualize survival outcomes, and differences between variable groups were compared using the Log Rank test. A Receiver Operating Characteristic (ROC) curve and Youden Index (Sensitivity + Specificity – 1) were calculated to determine the optimal cutoff values. Univariate Cox regression analysis was performed to identify potential prognostic factors. The Chi-Square (χ2) test was used to analyze the relationships between inflammatory and other related indexes and clinicopathological parameters. Likelihood ratio tests were used to compare univariate models. Nested models were compared using the likelihood ratio χ2 test. Model prediction capability, complexity, and goodness-of-fit were assessed using the Akaike Information Criterion (AIC), Bayesian Information Criterion (BIC), Concordance Index (C-index), LR_χ2 (Likelihood Ratio Chi-Square), and −2 Log-Likelihood. Higher LR_χ2 and C-index values, as well as lower AIC, BIC, and −2 Log-Likelihood values, are associated with more accurate prognostic prediction. Hazard Ratios (HR) estimated from Cox analysis will be reported as relative risks with corresponding 95% Confidence Intervals (CI). Variables with a P value <0.1 in the univariate Cox regression analysis will be analyzed comprehensively using AIC, BIC, C-index, LR_χ2, and −2 Log-Likelihood before they are included in the multivariate survival analysis. The stepwise forward selection method will be used to determine independent prognostic variables related to OS and DFS. SPSS v22.0 (IBM Corp, Armonk, NY, USA) and R software (Version 3.6.1, Institute for Statistics and Mathematics, Vienna, Austria) were used to perform statistical calculations. P value <0.05 will be considered statistically significant.
The optimal cutoff values were calculated as follows. According to the OS outcomes, the ROC analysis method was used to calculate the area under the curve (AUC) and the maximum Youden index. Among them, the cutoff value of NLR was 1.9, PLR was 143.4, SIRI was 0.9680, AGR was 1.34, PAR was 8.79, and PNI was 43.1. Patients were then divided into high and low groups based on these cutoff values. More details are as follows: High NLR vs Low NLR (>3.1 vs ≤3.1), High PLR vs Low PLR (>143.4 vs ≤143.4), High SIRI vs Low SIRI (>0.968 vs ≤0.968), High AGR vs Low AGR (>1.34 vs ≤1.34), High PAR vs Low PAR (>8.79 vs ≤8.79), High PNI vs Low PNI (>43.1 vs ≤43.1)
Result
Characteristics of the patients are presented in Table 1. A total of 93 patients were included in the study, comprising 57 males and 36 females, with an average age of 44.5 ± 20.4 years. The most common primary tumor site was the limbs (70.9%), followed by the trunk (18.2%), pelvis (9.6%), and other locations (1.0%). According to the MSTS/Enneking staging system, patients were staged as follows: 8 in stage IA (8.6%), 11 in stage IB (11.8%), 25 in stage IIA (26.8%), and 49 in stage IIB (52.6%). Based on the AJCC staging system, the distribution was: 8 in stage IA (8.6%), 10 in stage IB (10.7%), 23 in stage IIA (24.7%), 5 in stage IIB (5.3%), and 47 in stage III (50.5%). Thirty-four patients (63.4%) received combined radiotherapy, 62 patients (66.6%) received combined chemotherapy, 16 patients (19.4%) received targeted therapy, and 7 patients (7.5%) underwent immunotherapy. By the last follow-up, 48 patients experienced disease progression (recurrence or metastasis), with 32 patients (34.4%) showing tumor recurrence. Additionally, 38 patients (39.7%) developed distant metastasis. The sites of distant metastasis included the lungs (31 cases, 83.7%), bones (9 cases, 16.2%), and brain (4 cases, 10.8%). A total of 28 patients died, and 65 patients survived. The mean overall survival (Mean-OS) for STS patients was 60.1 ± 4.2 months, while the median disease-free survival (Median-DFS) was 25.0 ± 9.6 months. The pathological subtypes included in the study are shown in Table 2.
 |
Table 1 Demographic and Clinical-Pathological Characteristics |
 |
Table 2 The Classification of Subtypes of Soft Tissue Sarcoma |
The results of the univariate analysis are shown in Table 3. The Enneking stage (stage I vs stage II, HR = 2.950, 95% CI [1.167, 7.458], P = 0.022), NLR (HR = 2.348, 95% CI [1.204, 4.579], P = 0.012), SIRI (HR = 2.089, 95% CI [1.122, 3.886], P = 0.013), PAR (HR = 2.399, 95% CI [1.174, 4.901], P = 0.016), AGR (HR = 2.181, 95% CI [1.221, 3.897], P = 0.008) were significantly associated with DFS. The tumor site (P = 0.065) and PLR (P = 0.089) both showed a trend towards significance (0.05 < P < 0.1). Similarly, the univariate analysis revealed significant associations with OS for the following factors: Enneking stage (Stage I vs Stage II, HR=4.331, 95% CI [1.022, 18.358], P=0.047), NLR (HR=2.643, 95% CI [1.067, 6.548], P=0.036), SIRI (HR=4.185, 95% CI [1.446, 12.113], P=0.008), PAR (HR=3.433, 95% CI [1.426, 8.265], P=0.006), AGR (HR=2.261, 95% CI [1.043, 4.901], P=0.039) and LMR (HR=3.110, 95% CI [1.260, 7.677], P=0.014). The tumor site and LMR showed a trend toward significance (0.05 < P < 0.1).
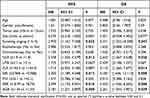 |
Table 3 Univariate Cox Proportional Analysis Regarding as Disease-Free Survival and Overall Survival |
A further evaluation is presented in Table 4, using C-index, LR_χ2, −2 log-likelihood, AIC, and BIC for comparing the predictive performance of the prognostic indexes. They are categorized into inflammation-related (NLR, PLR, LMR, and SIRI) and nutrition-related indexes (PAR, AGR, and PNI). All seven indexes are relatively effective predictors for DFS. Further analysis showed that SIRI and AGR have a high C-index, LR_χ2, and −2 log-likelihood, lower AIC and BIC, indicating better model fit and predictive accuracy for DFS and OS.
 |
Table 4 Comparison of the Prognostic Efficacy of the Indexes Regarding as Disease-Free Survival or Overall Survival |
As shown in Table 4, SIRI has a high C-index (0.610), LR_χ2 (6.466), and −2 log-likelihood (388.825), as well as lower AIC (389.527) and BIC (391.398) indices. These results indicate that SIRI has superior predictive accuracy and goodness-of-fit, and the model is simpler. Among the other prognostic indexes, AGR showed higher LR_χ2 and lower AIC and BIC compared to PAR and PNI, suggesting that AGR has better predictive accuracy and goodness-of-fit with lower model complexity. In contrast, PNI performed poorly, with no statistically significant difference in survival analysis. Furthermore, through stepwise matching, we compared the performance of the combined indexes (Figure 2 and Table 4). The results showed that the combination index of the SIRI+AGR+Enneking stage achieved the best accuracy (C-index = 0.751) and better model fit (AIC = 375.209; BIC = 380.823; −2 Log-Likelihood = 385.586; LR_χ2=10.360).
In the multivariate Cox proportional hazards model (Figure 3 and Table 5), we identified higher Enneking stage (HR=2.720, 95% CI [1.058, 6.991], P=0.038), lower AGR (HR=2.091, 95% CI [1.163, 3.759], P=0.014), and higher SIRI (HR=2.078, 95% CI [1.056, 4.087], P=0.034) as independent prognostic factors for DFS. Upon testing, the results of SIRI and AGR showed that there was no interaction between them (P=0.868).
 |
Table 5 Multivariate Cox Proportional Analysis Regarding as Disease-Free Survival or Overall Survival |
 |
Figure 3 Kaplan–Meier curves for OS in STS patients according to (A) SIRI, (B) AGR and DFS in STS patients according to (C) SIRI, (D) AGR. |
A similar method was used to further compare the predictive efficacy of these indexes for predicting OS (Table 4). SIRI has a higher C-index (0.659), LR_χ2 (8.206), −2 log-likelihood (215.019), and has lower AIC (219.167) and BIC (220.499) indices. The results show that SIRI has the best prediction accuracy and goodness-of-fit, and the model complexity is lower. Among other prognostic indicators, AGR, compared with PAR and PNI, has better prediction accuracy, goodness-of-fit, and lower-complex model (AIC=219.381; BIC=220.713; −2 log-likelihood=219.940; LR_χ2=4.516). Furthermore, we progressively compared the results of the combined indicators (Figure 2 and Table 4). The results showed that the combination index of the SIRI+AGR+Enneking stage has the best accuracy (C-index=0.755) and better model fit (AIC=211.612; BIC=215.609; −2 log-likelihood=205.082; LR_χ2 =16.270).
In the multivariate Cox proportional hazards model (Figure 3 and Table 5), we identified lower AGR (HR=2.321, 95% CI [1.064, 5.062], P=0.034), and higher SIRI (HR=3.729, 95% CI [1.278, 10.884], P=0.016) as independent prognostic factors for DFS. The results of SIRI and AGR showed that there was no interaction between them (P=0.490).
A correlation analysis of clinical features with SIRI and AGR is provided in Table S1.
Discussion
This study is the first to report the prognostic role of SIRI and AGR in STS patients. Our results showed that SIRI, AGR, and Enneking stage are independent prognostic risk factors for OS and DFS in STS patients. SIRI demonstrated superior predictive performance compared to other inflammation-related prognostic indicators such as NLR, PLR, and LMR. Furthermore, the combined index of the SIRI+AGR+ Enneking stage showed the best performance in all predictive models, while other indicators, including PNI and PAR, were not independent prognostic factors for STS.
Previous studies have preliminarily explored the prognostic value of inflammatory markers STS, including NLR, PLR, LMR, etc.10–12,25–30 However, the reported results vary slightly, likely due to differences in cohort composition and subtype distribution. For example, in 2014 Szkandera et al developed a nomogram incorporating LMR, rather than NLR or PLR, based on a cohort of 340 cases.28 In 2018, Hiromi Sasaki et al26 reported that the Glasgow Prognostic Score, NLR, and PLR are simple predictors of outcomes in STS patients. In 2020, D. Viñal et al27 reported that NLR was significantly associated with longer PFS and OS, while PLR and LMR showed no correlation. In 2022, Hashimoto K et al25 studied 22 elderly STS patients and identified C-reactive protein, albumin levels, neutrophil counts, and NLR as poor prognostic factors. In 2023, Fausti et al30 demonstrated that LMR specifically predicts the efficacy of Trabectedin as a second-line treatment in STS. Most recently, in 2016, Qi et al13 first established a new immune-inflammatory marker called SIRI based on patients with advanced pancreatic cancer undergoing chemotherapy to predict their prognosis. Subsequently, SIRI has also been confirmed to be associated with the prognosis of advanced tumors such as gastric cancer,31 colorectal cancer,32 advanced pancreatic cancer,13 and renal cancer.33
However, their calculation formulas indicate a clear correlation between these indices. Moreover, few have explored their prognostic value in STS. Therefore, we utilized this cohort to compare the strengths and weaknesses of these markers. First, our study indeed confirmed the predictive value of these markers. To further compare the reliability of these inflammatory indexes, this study used AIC, BIC, C-index, and LR_χ2 to further evaluate the accuracy and predictive ability of the model established by these indices. We observed that the predictive ability of SIRI was greater than that of other predictors such as NLR, LMR, and PLR, and it had lower model complexity and better goodness of fit. Elevated SIRI values were more likely to indicate a poor prognosis, consistent with previous studies on other solid tumors.33 Interestingly, there was a correlation between SIRI, AJCC stage, tumor size, and distant metastasis, reflecting that inflammatory status may reflect the overall disease burden and aggressiveness of sarcomas (Table S1). Therefore, our results may indicate that among STS patients before radical resection, those with a SIRI score <0.986 have worse prognostic outcomes than those with a SIRI score >0.986. Besides, the optimal cutoff value of this study was 0.968, which was similar to that of Li et al31 (cutoff value = 0.82, gastric adenocarcinoma) and Chen et al34 (cutoff value = 1.21, gastric cancer), but different from the results of Qi et al13 (cutoff value = 1.8, pancreatic cancer), which may be due to the heterogeneity of the tumor itself, state and population. Besides, this study including multiple subtypes such as fibrosarcoma, undifferentiated sarcoma, and liposarcoma may further lead to the difference in results. In the future, monitoring the SIRI, or incorporating it into machine learning models or nomograms, could assist in predicting survival outcomes for these rare types of tumors.
Hypoalbuminemia and hyperglobulinemia are considered to be associated with systemic inflammation in cancer patients.19,35,36 Many studies have shown that PNI as a nutritional index has a good ability to predict the prognosis of solid tumors. At present, only one study in 2021 supports that low PNI is an independent survival risk factor for STS,37 but our study suggests that PNI is not the independent prognostic risk factor for STS, which may be due to differences in population, tumor subtype, tumor stage, etc.38 Our study indicates that AGR and PAR are associated with prognosis. AGR is an independent prognostic risk factor in both DFS and OS and shows better predictive ability than PAR. Albumin is typically used to reflect the nutritional status and systemic inflammatory response in cancer patients, and globulin plays an important role in immunity and inflammation.39 In 2015, Shibutani et al40 analyzed 66 patients with metastatic colorectal cancer receiving palliative chemotherapy and found that high AGR before treatment was a marker of good prognosis. Subsequently, in 2019, Bozkaya et al41 explored a cohort of 251 patients, indicating that high AGR was an independent prognostic factor for OS and PFS in patients with metastatic gastric cancer. A meta-analysis summarized42 four clinical trials (sample sizes ranging from 214 to 6041) on metastatic prostate cancer cases, revealing that AGR showed significant independent predictive value for progression-free survival (OR=0.6420) and cancer-specific survival (OR=0.412) (P<0.01). Guo-Yue Lv,19 through a meta-analysis, investigated the role of AGR in multiple cancer types (15,356 cases), finding that preoperative low AGR was associated with an increased five-year mortality rate (relative risk RR=2.12, 95% CI: 1.48–3.03) and poorer progression-free survival (HR=1.64, 95% CI: 1.26–2.14). These studies demonstrate that preoperative low AGR is associated with poor prognosis across various types of tumors. This study is the first to investigate the prognostic role of AGR in non-metastatic soft-tissue sarcoma and indicates that AGR can also serve as a prognostic indicator in STS.
In conclusion, we found that the combined use of AGR and SIRI provides better predictive performance with high accuracy and consistency, effectively improving the accuracy of prognosis prediction. The findings of this study may help establish an individualized treatment framework for STS, identifying patients with increased risk and poor prognosis.
This study has several limitations. Firstly, being a single-center, retrospective study, there is an inherent bias in data collection methods. Second, certain important variables that were not considered in the risk factor analysis may potentially impact the interpretation and inference of the results. Third, the rarity of the disease limits the expansion of the sample size. Finally, the complex subtypes classification of STS might limit the generalizability and representativeness of the study findings.
Conclusion
Preoperative SIRI is a better predictive indicator compared to NLR, PLR, and LMR. Preoperative SIRI and AGR are independent risk factors for PFS and OS in non-metastatic STS patients. The combination index of the SIRI+AGR+Enneking stage provides a more robust prediction of clinical prognosis in STS patients. The findings may help establish an individualized treatment framework for STS, identifying patients with increased risk and poor prognosis.
Acknowledgments
This study was supported by grants from the National Key R&D Program of China (Grant No.2021YFC2400700); Key Research and Development Program of Guangzhou (No.2023B01J0022); National Natural Science Foundation of China (U21A2084); Natural Science Foundation of Guangdong Province (2022A1515011323).
Funding
This study was supported by grants from the National Key R&D Program of China (Grant No.2021YFC2400700); Key Research and Development Program of Guangzhou (No.2023B01J0022); National Natural Science Foundation of China (U21A2084); Natural Science Foundation of Guangdong Province (2022A1515011323).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29. doi:10.3322/caac.20138
2. Stojadinovic A, Leung DH, Hoos A, Jaques DP, Lewis JJ, Brennan MF. Ana lysis of the prognostic significance of microscopic margins in 2084 localized primary adult soft tissue sarcomas. Ann Surg. 2002;235(3):424–434. doi:10.1097/00000658-200203000-00015
3. Kattan MW, Leung DHY, Brennan MF. Postoperative nomogr am for 12-year sarcoma-specific death. J Clin Oncol. 2002;20(3):791–796. doi:10.1200/JCO.2002.20.3.791
4. Kraybill WG, Harris J, Spiro IJ, et al. Long-term results of a Phase 2 study of neoadjuvant chemotherapy and radiotherapy in the management of high-risk, high-grade, soft tissue sarcomas of the extremities and body wall: radiation therapy oncology group trial 9514. Cancer. 2010;116(19):4613–4621. doi:10.1002/cncr.25350
5. Chowdhary M, Chowdhary A, Sen N, Zaorsky NG, Patel KR, Wang D. Does the addition of chemotherapy to neoadjuvant radiotherapy impact survival in high-risk extremity/trunk soft-tissue sarcoma? Cancer. 2019;125(21):3801–3809. doi:10.1002/cncr.32386
6. Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi:10.1038/nature01322
7. Templeton AJ, McNamara MG, Šeruga B, et al. Prognostic ro le of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. doi:10.1093/jnci/dju124
8. Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y. Prognostic value of lymphoc yte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev. 2015;41(10):971–978. doi:10.1016/j.ctrv.2015.10.003
9. Lee SF, Ng TY, Spika D. Prognostic value of lymphocyte-monocyte ratio at diagnosis in Hodgkin lymphoma: a meta-analysis. BMC Cancer. 2019;19(1):338. doi:10.1186/s12885-019-5552-1
10. Nakamura T, Matsumine A, Matsubara T, Asanuma K, Uchida A, Sudo A. The c ombined use of the neutrophil-lymphocyte ratio and C-reactive protein level as prognostic predictors in adult patients with soft tissue sarcoma. J Surg Oncol. 2013;108(7):481–485. doi:10.1002/jso.23424
11. Que Y, Qiu H, Li Y, et al. Preoperative platelet-lymphocyte ratio is superior to neutrophil-lymphocyte ratio as a prognostic factor for soft-tissue sarcoma. BMC Cancer. 2015;15(1):648. doi:10.1186/s12885-015-1654-6
12. Watanabe S, Shimoi T, Nishikawa T, et al. Lymphocyte-to-m onocyte ratio as a prognostic and potential tumor microenvironment indicator in advanced soft tissue sarcoma treated with first-line doxorubicin therapy. Sci Rep. 2023;13(1):10734. doi:10.1038/s41598-023-37616-w
13. Qi Q, Zhuang L, Shen Y, et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer. 2016;122(14):2158–2167. doi:10.1002/cncr.30057
14. Wang X, Ni X, Tang G. Prognostic role of platelet-to-lymphocyte ratio in patients with bladder cancer: a meta-analysis. Front Oncol. 2019;9:757. doi:10.3389/fonc.2019.00757
15. Shi J, Liu T, Ge Y, et al. Cholesterol-modified prognostic nutritional index (CPNI) as an effective tool for assessing the nutrition status and predicting survival in patients with breast cancer. BMC Med. 2023;21(1):512. doi:10.1186/s12916-023-03225-7
16. Yang WJ, Zhang GL, Cao KX, et al. Heparanase from triple‑negative breast cancer and platelets acts as an enhancer of metastasis. Int J Oncol. 2020;57(4):890–904. doi:10.3892/ijo.2020.5115
17. Li S, Lu Z, Wu S, et al. The dynamic role of platelets in cancer progression and their therapeutic implications. Nat Rev Cancer. 2024;24(1):72–87. doi:10.1038/s41568-023-00639-6
18. Jiang L, Luan Y, Miao X, et al. Platelet releasate promotes breast cancer growth and angiogenesis via VEGF-integrin cooperative signalling. Br J Cancer. 2017;117(5):695–703. doi:10.1038/bjc.2017.214
19. Lv GY, An L, Sun XD, Hu YL, Sun DW. Pretreatment albumin to globulin ratio can serve as a prognostic marker in human cancers: a meta-analysis. Clin Chim Acta. 2018;476:81–91. doi:10.1016/j.cca.2017.11.019
20. Soeters PB, Wolfe RR, Shenkin A. Hypoalbuminemia: pathogenesis and clinical significance. JPEN J Parenter Enteral Nutr. 2019;43(2):181–193. doi:10.1002/jpen.1451
21. Fujikawa H, Toiyama Y, Inoue Y, et al. Prognostic impact of preoperative albumin-to-globulin ratio in patients with colon cancer undergoing surgery with curative intent. Anticancer Res. 2017;37(3):1335–1342.
22. Salciccia S, Frisenda M, Bevilacqua G, et al. Prognostic value of albumin to globulin ratio in non-metastatic and metastatic prostate cancer patients: a meta-analysis and systematic review. Int J mol Sci. 2022;23(19):11501. doi:10.3390/ijms231911501
23. Tanaka K, Tsumura H. Eighth edition of the American Joint Committee on Cancer staging system for soft tissue sarcoma of the trunk and extremity: in search of a better staging system. Ann Transl Med. 2019;7(Suppl 1):S11. doi:10.21037/atm.2019.01.31
24. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;(153):106–120.
25. Hashimoto K, Nishimura S, Shinyashiki Y, Ito T, Akagi M. Characterizing inflammatory markers in highly aggressive soft tissue sarcomas. Medicine (Baltimore). 2022;101(39):e30688. doi:10.1097/MD.0000000000030688
26. Sasaki H, Nagano S, Komiya S, Taniguchi N, Setoguchi T. Validation of different nutritional assessment tools in predicting prognosis of patients with soft tissue spindle-cell sarcomas. Nutrients. 2018;10(6):765. doi:10.3390/nu10060765
27. Viñal D, Martinez D, Garcia-Cuesta JA, et al. Prognostic value of neutrophil-to-lymphocyte ratio and other inflammatory markers in patients with high-risk soft tissue sarcomas. Clin Transl Oncol. 2020;22(10):1849–1856. doi:10.1007/s12094-020-02324-8
28. Szkandera J, Gerger A, Liegl-Atzwanger B, et al. The lymphocyte/monocyte ratio predicts poor clinical outcome and improves the predictive accuracy in patients with soft tissue sarcomas. Int, J, Cancer. 2014;135(2):362–370. doi:10.1002/ijc.28677
29. Rosner M, Dolznig H, Schipany K, Mikula M, Brandau O, Hengstschläger M. Human amniotic fluid stem cells as a model for functional studies of genes involved in human genetic diseases or oncogenesis. Oncotarget. 2011;2(9):705–712. doi:10.18632/oncotarget.328
30. Fausti V, De Vita A, Vanni S, et al. Systemic inflammatory indices in second-line soft tissue sarcoma patients: focus on lymphocyte/monocyte ratio and trabectedin. Cancers (Basel). 2023;15(4):1080. doi:10.3390/cancers15041080
31. Li S, Lan X, Gao H, et al. Systemic Inflammation Response Index (SIRI), cancer stem cells and survival of localised gastric adenocarcinoma after curative resection. J Cancer Res Clin Oncol. 2017;143(12):2455–2468. doi:10.1007/s00432-017-2506-3
32. Cai H, Li J, Chen Y, Zhang Q, Liu Y, Jia H. Preoperative inflammation and nutrition-based comprehensive biomarker for predicting prognosis in resectable colorectal cancer. Front Oncol. 2023;13:1279487. doi:10.3389/fonc.2023.1279487
33. Arı E, Köseoğlu H, Eroğlu T. Predictive value of SIRI and SII for metastases in RCC: a prospective clinical study. BMC Urol. 2024;24(1):14. doi:10.1186/s12894-024-01401-2
34. Chen L, Chen Y, Zhang L, et al. In gastric cancer patients receiving neoadjuvant chemotherapy systemic inflammation response index is a useful prognostic indicator. Pathol Oncol Res. 2021;27:1609811. doi:10.3389/pore.2021.1609811
35. Meyer EJ, Nenke MA, Rankin W, Lewis JG, Torpy DJ. Corticosteroid-binding globulin: a review of basic and clinical advances. Horm Metab Res. 2016;48(6):359–371. doi:10.1055/s-0042-108071
36. Panotopoulos J, Posch F, Alici B, et al. Hemoglobin, alkalic phosphatase, and C-reactive protein predict the outcome in patients with liposarcoma. J Orthop Res. 2015;33(5):765–770. doi:10.1002/jor.22827
37. Matsuyama Y, Nakamura T, Yoshida K, et al. Role of the prognostic nutritional index in patients with soft-tissue sarcoma. Vivo Athens Greece. 2021;35(4):2349–2355.
38. McMillan DC, Watson WS, O’Gorman P, Preston T, Scott HR, McArdle CS. Albumin concentrations are primarily determined by the body cell mass and the systemic inflammatory response in cancer patients with weight loss. Nutr Cancer. 2001;39(2):210–213. doi:10.1207/S15327914nc392_8
39. Hill LA, Bodnar TS, Weinberg J, Hammond GL. Corticosteroid-binding globulin is a biomarker of inflammation onset and severity in female rats. J Endocrinol. 2016;230(2):215–225. doi:10.1530/JOE-16-0047
40. Shibutani M, Maeda K, Nagahara H, et al. The pretreatment albumin to globulin ratio predicts chemotherapeutic outcomes in patients with unresectable metastatic colorectal cancer. BMC Cancer. 2015;15(1):347. doi:10.1186/s12885-015-1375-x
41. Bozkaya Y, Erdem GU, Demirci NS, et al. Prognostic importance of the albumin to globulin ratio in metastatic gastric cancer patients. Curr Med Res Opin. 2019;35(2):275–282. doi:10.1080/03007995.2018.1479683
42. Le Cesne A, Judson I, Crowther D, et al. Randomized Phase III study comparing conventional-dose doxorubicin plus ifosfamide versus high-dose doxorubicin plus ifosfamide plus recombinant human granulocyte-macrophage colony-stimulating factor in advanced soft tissue sarcomas: a trial of the European organization for research and treatment of cancer/soft tissue and bone sarcoma group. J Clin Oncol. 2000;18(14):2676–2684. doi:10.1200/JCO.2000.18.14.2676
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


