Back to Journals » Journal of Inflammation Research » Volume 17
Prognostic Value of Systemic Inflammation Response Index and N-Terminal Pro-B-Type Natriuretic Peptide in Patients with Myocardial Infarction with Nonobstructive Coronary Arteries- A Retrospective Study
Authors Hou H, Xu Y, Chen G, Yao H, Bi F
Received 6 August 2024
Accepted for publication 15 October 2024
Published 6 November 2024 Volume 2024:17 Pages 8281—8298
DOI https://doi.org/10.2147/JIR.S482596
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Ning Quan
Hua Hou,1 Yujia Xu,2 Guangxin Chen,3 Haifeng Yao,4 Fangjie Bi5
1School of Clinical Medicine, Binzhou Medical University, Binzhou, Shandong, People’s Republic of China; 2Department of Echocardiography, Zibo Central Hospital, Zibo, Shandong, People’s Republic of China; 3Department of Emergency, Zibo Central Hospital, Zibo, Shandong, People’s Republic of China; 4School of Clinical Medicine, Shandong Second Medical University, Weifang, Shandong, People’s Republic of China; 5Department of Cardiology, Zibo Central Hospital, Zibo, Shandong, People’s Republic of China
Correspondence: Fangjie Bi, Department of Cardiology, Zibo Central Hospital, Zhangdian District - Communist Youth, League West Road No. 54, Zibo, Shandong, 255000, People’s Republic of China, Tel +86- 185 6029 3603, Email [email protected]
Background: The Systemic Inflammation Response Index (SIRI) and N-terminal Pro–B-type natriuretic peptide (NT-proBNP) have been proposed as reliable predictors of poor prognosis in cardiovascular disease and all-cause mortality, However, their validity has not been extensively evaluated in patients with myocardial infarction with nonobstructive coronary arteries (MINOCA).
Patients and Methods: 259 patients diagnosed with MINOCA were enrolled in this study from January 2015 to December 2022, and serum levels of SIRI and NT-proBNP were detected. The primary endpoints were major adverse cardiovascular events (MACE). According to the occurrence of MACE during the follow-up period, patients were grouped into MACE and Non-MACE groups, and divided by the median values for SIRI and NT-proBNP into groups: low SIRI, high SIRI, low NT-proBNP, and high NT-proBNP.
Results: A statistically significant difference in the levels of SIRI and NT-proBNP was observed between the MACE group and the non-MACE group. Kaplan-Meier survival curve analysis revealed that patients with high SIRI and high NT-proBNP had a significantly higher risk of MACE (log-rank P < 0.001). Furthermore, even after adjusting for covariates, the high SIRI and high NT-proBNP were associated with an increased risk of MACE (P< 0.001, HR: 3.188, 95% CI 1.940– 5.241; P< 0.001, HR: 2.245, 95% CI 1.432– 3.519). Additionally, the combined prognosis prediction of SIRI and NT-proBNP was superior to a single prediction, and adding SIRI and NT-proBNP to the traditional risk factor model improved the model’s predictive value.
Conclusion: High levels of SIRI and NT-proBNP exhibit a significant correlation with an increased risk of MACE, thereby suggesting that SIRI can be used as a reliable inflammatory indicator for predicting the risk in MINOCA patients, with significantly improved prognostic value when combined with NT-proBNP.
Keywords: systemic inflammation response index, N-terminal pro–B-type natriuretic peptide, myocardial infarction with coronary nonobstructive, major adverse cardiac events, prognosis, risk assessment
Introduction
Myocardial infarction with nonobstructive coronary arteries (MINOCA) represents a special subtype of myocardial infarction (MI), distinguished by coronary angiography revealing an absence of significant obstruction in the coronary arteries (defined as major epicardial vessel diameter stenosis less than 50%), despite clinical presentations typical of acute myocardial infarction. Approximately 2.8% to 15% of acute myocardial infarction (AMI) patients are diagnosed with MINOCA.1,2 The pathophysiological mechanisms of MINOCA are diverse, encompassing both atherosclerotic (such as plaque rupture, erosion, and bleeding) and non-atherosclerotic factors (such as coronary artery spasm, microvascular dysfunction, embolism/thrombosis, spontaneous coronary dissection, and supply-demand mismatch). These mechanisms can precipitate myocardial ischemia, leading to myocardial infarction, even in the absence of overt coronary artery obstruction. Owing to the scarcity of evidence-based guidelines and prospective randomized controlled studies, treatment strategies for MINOCA are often individualized and rely on a comprehensive assessment of a patient’s specific circumstances.3
In the past, MINOCA was perceived as a benign condition with a low risk of adverse outcomes. However, recent research reveals that MINOCA patients are at a significantly elevated risk of adverse outcomes compared to age- and sex-matched controls without coronary heart disease, exhibiting higher short- and long-term mortality rates.4 The incidence of reinfarction and mortality at a median follow-up of 38 months is similar to that seen in myocardial infarction with coronary artery disease(MI-CAD) patients. The etiology of MINOCA is intricate and its treatment and prognosis are closely related to its pathogenesis. Evidence suggests that inflammation serves as the cornerstone of both atherosclerotic and non-atherosclerotic pathological mechanisms in MINOCA.5 Recently, the application of inflammatory indicators or biomarkers as predictors of cardiovascular disease severity and prognosis has garnered significant attention within the cardiovascular research landscape. Amid systemic inflammation, injury, and stress, key immune system components like neutrophils, lymphocytes, and monocytes undergo dynamic changes. Specifically, an increase in neutrophils and a concomitant decrease in lymphocytes are characteristic responses. Neutrophils play a pivotal role in early infection and immune regulation, and their increase can be influenced by multiple factors, such as neutrophil extrusion, inhibition of apoptosis, and growth factor stimulation. Conversely, the decline in lymphocytes may signify compromised immune function, stemming from neuroendocrine stress, tissue damage, and cytokine-mediated mechanisms. The contrasting shifts in these two cell populations reflect intricate immune and physiological responses that manifest early in response to acute stress, thus positioning them as early sensitivity markers (<6h).
Indices derived from complete blood count (CBC) have been proposed as reliable inflammatory biomarkers for predicting adverse outcomes in coronary artery disease, such as neutrophil-to-lymphocyte ratio (NLR),platelet-to-lymphocyte ratio (PLR), white blood cell count to mean platelet volume ratio (WMR), and neutrophil-to-platelet ratio (NPR), have shown association with long-term adverse cardiovascular events in patients with acute coronary syndrome or non-ST-elevation myocardial infarction(NSTEMI) patients after percutaneous coronary intervention (PCI).6–8 NLR, WMR, and NPR have also been confirmed to have good predictive value for long-term adverse cardiovascular events in MINOCA.8,9 A novel derived indicator of complete blood count involving neutrophil, monocyte, and lymphocyte counts-SIRI, has recently been proposed in the literature to assess the risk of neoplasia, stroke, and cardiovascular disease.10–13 It has demonstrated superior predictive capability compared to other inflammatory indicators or markers and potential utility in predicting the prognosis of MINOCA patients.14
Natriuretic peptides (NPs) are well-established markers for diagnosing and assessing prognosis in patients with heart failure (HF) and left ventricular insufficiency. Elevated NT-proBNP levels serve as a response to cardiac stress, such as myocardial ischemia or injury. In MINOCA, where the myocardium may be affected by a variety of causes including microvascular disease, and coronary artery spasm, increased NT-proBNP serves as a sensitive marker for assessing myocardial damage extent. High NT-proBNP levels are associated with an increased risk of heart failure. In MINOCA patients, elevated NT-proBNP may indicate a higher risk of heart failure, which is a key determinant of prognosis. Moreover, NT-proBNP dynamics provide valuable insights into post-infarction recovery and cardiac remodeling. A sustained elevation or inadequate decline in NT-proBNP levels over time portends a suboptimal prognosis. Although NT-proBNP has been identified to be associated with adverse prognostic events in MI,15–17 and is an independent indicator of clinical prognosis in acute STEMI patients,18 there is limited research on its use as a prognostic biomarker specifically in MINOCA patients.
To gain a better understanding of the clinical predictors for the progression and exacerbation of cardiovascular disease, and to offer new insights into early prevention and innovative management, it is essential to further investigate the potential utility of SIRI and NT-proBNP as prognostic biomarkers for this population.
Materials and Methods
Study Population
This is a single-center, observational, and retrospective cohort study, which was conducted on patients with MINOCA diagnosed at Zibo Central Hospital from January 2015 to December 2022.
The diagnosis of MINOCA was established based on the recognized criteria published by the American Heart Association in 2019 (see Supplementary Materials S1).
Criteria for excluding patients: (1) Patients with a history of previous MI, coronary artery revascularization (PCI or CABG), severe valvular disease, and congenital heart disease; (2) Death, cardiogenic shock, and mechanical complications of acute myocardial infarction during hospitalization; (3) Patients with acute/chronic infection, systemic inflammation, active autoimmune rheumatic disease, hematologic disease, malignant tumors, severe hepatic or renal insufficiency, severe anemia, or fever (>38 °C); (4) history of steroid or immunosuppressant medication use during hospitalization. Patients were considered ineligible for this study if the blood collection time window exceeded 24 hours, if they failed to follow up or provide adequate clinical information, or if their elevated troponin levels were attributed to other etiologies.
A total of 357 patients were diagnosed with MINOCA at Zibo Central Hospital between January 2015 and December 2022. Out of these, 98 patients were excluded from the study due to ineligibility (n=21) and meeting the exclusion criteria (n=77). Ultimately, a cohort of 259 minOCA patients was included in the final analysis of this study (Power 1-β:0.96). The study protocol complied with the Declaration of Helsinki and was approved by the Hospital Ethics Review Committee (Zibo Central Hospital). Since this was a retrospective study, the Ethics Committee approved exemptions from signing the informed consent form in accordance with national legal and institutional requirements. A combination of medical records and telephone interviews were used to collect data in the study. A flow chart of the study is shown in Figure 1.
Data Collection
General information of patients (including age, gender, height, weight, systolic blood pressure, and diastolic blood pressure at the moment of admission, heart rate, Killip classification), as well as risk factors (such as hypertension, diabetes mellitus, dyslipidemia, current or former smoking, and stay up late, etc) were extracted from the electronic medical information record system of the Zibo Central Hospital. Additionally, pre-onset emotional agitation history and results of echocardiography and laboratory indicators were collected. The following blood test indicators were collected: WBC, neutrophils, monocytes, lymphocytes, platelets, mean platelet volume (MPV), red cell distribution width (RDW), D-dimer, Hemoglobin A1C(HbA1C), lipid profile (including total cholesterol [TC], triglycerides [TG], low-density lipoprotein cholesterol [LDL-C], high-density lipoprotein cholesterol [HDL-C], Lp(a)), cystatin c, fasting plasma glucose (FPG), uric acid, creatinine, troponin I (TnI) and amino-terminal pro-brain natriuretic peptide (NT-proBNP).
In this study, the definitions and diagnostic criteria for hypertension, dyslipidemia, and other clinical diagnoses were based on the current domestic and international guidelines (see Supplementary Materials S2).
Biomarker Measurement
All laboratory indicators were measured using standard methods in the Department of Laboratory Medicine at Zibo Central Hospital. Patients typically had venous blood samples collected in the fasting state early in the morning following admission, ensuring the sampling occurred within 24 hours of symptom onset. The collected samples were uniformly processed by our laboratory center for centrifugation and standardized analysis. Details of the calibration and quality control procedures are provided in Supplementary Materials 3 and 4. Upon admission, patients received a standard echocardiographic examination, with the left ventricular ejection fraction (LVEF) determined using the dual-plane Simpson’s technique.
The corresponding indexes were calculated from the same blood sample test report, SIRI was calculated as Absolute Neutrophil Count [ANC] *Absolute Monocyte Count [AMC]/Absolute Lymphocyte Count [ALC], NLR was calculated as ANC/ ALC, WMR was calculated as White Blood Cell Count /Mean Platelet Volume Ratio [MPV], NPR calculated as ANC/Absolute Platelet Count [APC].
Clinical Endpoint and Follow-Up
Considering the persistent myocardial injury in patients with MINOCA, which stems from their complex pathophysiological processes, this can progress to chronic myocardial damage, ventricular remodeling, and impaired cardiac function. Consequently, MINOCA patients are likely to face an increased long-term cardiovascular risk.
The study was conducted until December 2023, with a mean follow-up duration of 48.4 (44.8–52.1) months (median follow-up duration of 47.0 (40.4–53.6) months). Each patient or their relatives were individually contacted via telephone, and computerized medical records were reviewed to obtain follow-up information. The first MACE observed during the follow-up period was used as the follow-up cut-off time. The primary endpoint of this study was the composite endpoint of major adverse cardiovascular events (MACE), including (1) all-cause death; (2) nonfatal MI; (3) stroke; (4) HF; (5) Re-hospitalization of angina pectoris; (6) revascularization; (7) cardiac death. The diagnosis of recurrent infarction refers to the fourth general definition of MI,19 and stroke is defined as the typical symptoms and imaging manifestations of neurological dysfunction and vascular brain injury caused by cerebral ischemia or hemorrhage.20 HF is defined as typical symptoms and evidence of structural or functional abnormalities of the heart.21 Angina rehospitalization refers to readmission to the hospital or emergency department due to angina chest discomfort (with evidence documented by the healthcare system). Cardiac death is defined as death from cardiac causes, ie, ACS, fatal arrhythmia, refractory heart failure, or sudden death without apparent cause.
Division of Patient Groups
The patients enrolled in the study were divided into two groups based on their occurrence of MACE during the follow-up period, with 89 patients experiencing MACE(MACE group) and 170 patients remaining event-free(Non-MACE group). The median values for SIRI and NT-proBNP were 1.743 and 358.00, respectively. Subsequently, the patients were divided into four groups based on these median values: those with low SIRI (SIRI≤1.743,n=130), high SIRI (SIRI>1.743,n=129), low NT-proBNP (NT-proBNP≤358.00,n=130) and high NT-proBNP (NT-proBNP>358.00,n=129).
Statistical Analysis
The continuous variables were reported as mean ± standard deviation (SD) or median (25th to 75th percentiles), while categorical variables were presented as counts and percentages (%). To assess data normality, either the Kolmogorov–Smirnov test or the Shapiro–Wilk test be used. Group differences were compared using the independent sample t-test or Mann–Whitney U-test. Categorical variables were analyzed using the chi-square (χ2) or Fisher exact test. The Kaplan-Meier survival analysis was employed to compute the cumulative incidence of long-term outcomes, and subsequently, a comparison was made between the high and low-indicator groups regarding the incidence of MACE. The Log rank test was used for comparison between groups. To determine the predictive indicators of MACE in patients with MINOCA, we performed a univariate Cox proportional risk analysis to assess the relationship between baseline variables and MACE. If the baseline variable showed p<0.05 in the univariate analysis or was clinically associated with MACE, the baseline variable was included in the multivariable Cox proportional risk analysis model. Examine the risk ratio hypothesis. Finally, utilizing the Akaike Information Criterion (AIC) for automated model selection, we have developed four models designed to account for confounding variables and refine the analysis by adjusting for key factors, including model fit and complexity. These factors encompass HBA1c, BMI, Killipclass, Creatinine, and CRP levels. The resulting models yield hazard ratios (HR) that reflect the adjusted associations. Evaluated the correlation between SIRI and NT-proBNP (as continuous or categorical variables) and MACE. Perform subgroup analysis, to study SIRI and NT-proBNP in age (<65 years or ≥65 years), gender (female or male), BMI (<25 or ≥25kg/m2), Killip classification (<2 or ≥2), hypertension (yes or no), dyslipidemia (yes or no), diabetes (yes or no), and current or former smoking (yes or no) were evaluated for consistency in predicting poor outcomes. The C-index, net reclassification improvement (NRI), and integrated discrimination improvement (IDI) statistical analyses were performed to evaluate the ability of SIRI and NT-proBNP to improve the predictive value of the traditional cardiovascular risk model.
The statistical analyses were performed using SPSS (version 27.0), R language (version 4.3.3), and GraphPad software (version 8.0). The results were considered statistically significant at a significance level of P<0.05.
Results
Study Population and Clinical Baseline Characteristics
Figure 1 shows the process of this study. The study comprised of the continuous enrollment of 10,744 AMI patients, among whom 357 (3.3%) met the diagnostic criteria of MINOCA. After application of the exclusion criteria, a total of 259 minOCA patients who fulfilled the inclusion criteria were enrolled and followed up until December 2022 (mean age 58.41±12.69 years, 63.3% of them were male). Table 1 presents the clinical, laboratory, and echocardiographic results of the study participants. During a median follow-up of 47.0 (40.4–53.6) months, a total of 89 cases (34.3%) of MACE were observed, including 5 cases (5.6%) of all-cause death (including 1 sudden cardiac death), 30 cases (33.7%) of non-fatal MI, 30 cases (33.7%) requiring re-hospitalizations due to angina pectoris, 9 cases (10.1%) of HF, and 7 cases (7.9%) of stroke occurrence. Among the patients who experienced MACE, a total of 19 individuals exhibited progression of coronary stenosis, with 8 necessitating revascularization. The MACE group exhibited higher BMI and Killip classification compared to the non-MACE group. Additionally, the MACE group demonstrated elevated levels of WBC count, neutrophil count, monocyte count, platelet count, red blood cell distribution width, HbA1c, TnI, CRP, NT-proBNP, SIRI, WMR, NPR and NLR in comparison to the non-MACE group. However, the lymphocyte count was higher in the non-MACE group. Statistically, there were no significant differences observed between the two groups in terms of age, hypertension, diabetes, dyslipidemia, current or former smoking, stay up late, pre-onset emotional excitement, TC, TG, TB, HDL-C, LDL-C, Lp (a), creatinine, uric acid, D-dimer, FPG, serum cystatin C, and WMR (Since there was no statistical difference in diabetes within this study and HbA1c exhibited significant statistical significance,HbA1c≥6.5% was subsequently used to replace diabetes for further statistical analysis).
 |
Table 1 Clinical and Laboratory Characteristics of Patients Grouped According to Whether MACE Occurred or Not |
Risk Factor Analysis for MACE Development
The study utilized Kaplan-Meier survival analysis to evaluate long-term survival. The results depicted in Figure 2 demonstrate that patients with high SIRI and NT-proBNP levels experienced a poorer outcome, exhibiting a significantly higher incidence of MACE (Log-rank P<0.001,HR:3.581, 95% CI 2.349 −5.458; Log-rank P<0.001,HR=2.289, 95CI% 1.503 −3.486). Furthermore, the investigation explored the impact of SIRI and NT-proBNP levels on MACE occurrence within different subgroups. As illustrated in Figure 3, each subgroup exhibited an increasing trend in MACE incidence for both high SIRI group compared to low SIRI group and high NT-proBNP group compared to low NT-proBNP group). Additionally, it is noteworthy that the SIRI and NT-proBNP levels were significantly higher in the MACE group than those observed in the Non-MACE group (P <0.05, Figure 4).
The independent indicators associated with MACE in each variable were identified through univariate and multivariable COX survival analyses, with MACE serving as the primary endpoint. The results were presented using hazard ratios (HR) and 95% confidence intervals (CI). Univariate Cox survival analyses demonstrated that BMI, Killip classification, Cys-C, HbA1c, Ln (NT-proBNP), Ln (SIRI), Ln(WMR), Ln (NLR), and Ln (NPR)were univariate predictors of MACE (Table 2). Multivariable analysis revealed that BMI (P=0.004, HR=1.119, 95% CI 1.036–1.209), HbA1c (P<0.001, HR=3.609, 95% CI 2.248–5.795), Ln (SIRI) (P=0.001, HR=2.190 95% CI 1.383–3.468), Ln(NT-proBNP) (P=0.004, HR=1.258, 95% CI 1.077–1.470), Ln (WMR) (P=0.025, HR=1.577 95% CI 1.060–0.348), Ln (NPR) (P=0.013, HR=1.884 95% CI 1.145–3.102) and Ln (NLR) (P=0.002, HR=1.611 95% CI 1.184–2.193) were able to independently predict the occurrence of MACE in MINOCA patients (Table 2). Due to WMR, NLR, NPR, and SIRI were all derived from blood cell measurements and were collinearity, each parameter was included separately in multivariable Cox proportional hazard regression analysis.
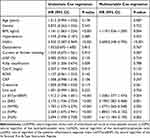 |
Table 2 Results of Univariate and Multivariable Cox Regression Analysis of MACE |
The correlation between SIRI, NT-proBNP, and MACE was investigated to assess their independent predictive value for clinical prognosis. After checking the proportional hazards assumption (P > 0.05), four separate Cox risk models were constructed and analyzed (Table 3). The models were adjusted for HBA1c, BMI, Killipclass, Creatinine, and CRP. The findings revealed that a high SIRI value (SIRI>1.743) was significantly associated with an increased risk of MACE and exhibited the highest hazard ratio (P<0.001, adjusted HR=2.904 95% CI 1.759–4.794). Similarly, high NT-proBNP (NT-proBNP >358.00) was also linked with an increased risk of MACE (P <0.001, adjusted HR=2.039 95% CI 1.289–3.225). Furthermore, the combined effect of high SIRI and high NT-proBNP was found to increase the risk of MACE (P<0.001, adjusted HR, 2.618 95% CI 1.676–4.087).
 |
Table 3 Results of Cox Proportional Risk Regression Analysis for Each Model |
To further investigate the association between high SIRI, NT-proBNP, and the risk of MACE, as well as to determine whether the incidence of MACE in different subgroups is influenced by other covariates, we conducted subgroup analyses based on age (<65 years or ≥65 years), gender (female or male), BMI (<25/<18.5 or ≥25 kg/m2), Killip classification (<2 or ≥2), hypertension (yes or no), HbA1c (<6.5%or≥6.5%), dyslipidemia(yes or no) and current or former smoking (yes or no).To evaluate the consistency of the effects of each indicator on MACE prognosis (Figure 5, Figure 6) we found no significant interaction between SIRI, NT-proBNP and age, gender, BMI, Killip classification, hypertension, HbA1c, dyslipidemia, and current or former smoking (yes or no). Notably, high SIRI and high NT-proBNP levels were consistently associated with an increased risk of MACE across all subgroups examined in this study. These findings further reinforce the robustness of the association between high SIRI and NT-proBNP levels with MACE.
Incremental Effects of SIRI and NT-proBNP on the Predictive Value of Mace
As presented in Table 4, the risk factor model, including age, gender, BMI, hypertension, HbA1c, dyslipidemia, and current or former smoking, yielded a c statistic of 0.650(95% CI:0.589,0.711). Upon incorporating SIRI and NT-proBNP into the established traditional risk model, the c statistic improved to 0.731 (95% CI: 0.679–0.782). In comparison to the baseline model incorporating conventional risk factors, the inclusion of SIRI and NT-proBNP exhibited a significant incremental effect. Notably, the addition of both SIRI and NT-proBNP demonstrated the most substantial enhancement compared to their individual incorporation. The c statistic was 0.731 (95% CI: 0.679–0.782), NRI was 0.413(95% CI: 0.261–1.003), and IDI was 0.239 (95% CI: 0.028–0.549). These findings underscored that supplementing the baseline model with SIRI and NT-proBNP yielded additional predictive value for adverse cardiovascular events, with superior prognostic capability observed when combining SIRI and NT-proBNP over traditional risk factors in MINOCA patients.
 |
Table 4 Evaluation of Predictive Models |
Discussion
The present study is the first to demonstrate the utility of the SIRI and NT-proBNP in predicting long-term outcomes among patients with MINOCA. The main findings of the study include:(1) high SIRI and high NT-proBNP levels were significantly associated with an increased risk of MACE in MINOCA patients; (2) both SIRI and NT-proBNP, either individually or in combination, were independent prognostic indicators for long-term outcomes within the MINOCA population; (3) the combined utilization of SIRI and NT-proBNP exhibited superior predictive capability for MACE compared to their individual use; (4) incorporation of SIRI and NT-proBNP into traditional risk models demonstrated a significant incremental effect.
MINOCA is a unique type of myocardial infarction. Its exact etiology has not been fully elucidated, which leads to the lack of sufficient evidence support in evidence-based treatment and prognosis evaluation. Therefore, the clinical management strategy of MINOCA is controversial. As a heterogeneous disease, the underlying pathophysiological mechanism of MINOCA is intricate and variable.22,23 Although the specific mechanism has not been fully revealed, existing studies have pointed out that inflammatory response plays a crucial role in the pathogenesis of MINOCA. Compared with myocardial infarction caused by coronary artery disease (MI-CAD), MINOCA showed more significant initial inflammatory activity in the acute phase, and its chronic inflammatory state was more persistent.24,25
A variety of inflammatory markers were elevated in patients with coronary artery spasm, such as soluble P-selectin, intercellular adhesion molecule-1, A2 phospholipase, and T-cell activation. Histological examination also showed neointimal hyperplasia with inflammatory cell infiltration, suggesting the importance of inflammation around the coronary artery in the mechanism of spasm.26–31 Inflammation and endothelial dysfunction are important pathophysiological mechanisms of coronary microvascular dysfunction(CMD) in MINOCA patients.32 Elevated CRP and hs-CRP are associated with impaired coronary flow reserve in CMD,33 which can directly inhibit the differentiation, survival, and regeneration of endothelial progenitor cells, affect the integrity of microvascular endothelium, promote the progression of atherosclerosis, and lead to adverse outcomes.34 It can also promote plaque progression, rupture, and the formation of embolic particles, leading to microcirculation embolism.35,36 In patients with spontaneous coronary artery dissection (SCAD), infiltrating neutrophils can be seen in the media of the diseased coronary artery and diffuse inflammatory reactions composed of eosinophils around the adventitia.37 Eosinophils release cytotoxic and collagen-dissolving substances, which have also been shown to cause smooth muscle degeneration and inner layer destruction.38 The importance of inflammation in the development of atherosclerosis and the instability of atherosclerotic plaques has also been fully demonstrated.39 Previous clinical studies have shown that MINOCA individuals may also have pro-inflammatory tendencies.40
Conventional indicators that can reflect the state of inflammation include whole blood cell count in the circulatory system and acute phase proteins (such as C-reactive protein and procalcitonin). As a readily available and cost-effective indicator, complete blood cell count has been shown to be closely related to the pathophysiological processes of endothelial dysfunction, plaque instability, immune imbalance, oxidative stress, and inflammatory response.2,41 Among these cellular components, neutrophils have been reported as a mediator of the acute inflammatory response, not only involved in microvascular injury and the non-reflux state of AMI,42 but also activated and induced inflammatory response in vivo, promoted coronary plaque abnormalities, induced atherosclerotic plaque rupture and thrombosis, and increased the risk of cardiovascular complications.43,44 On the other hand, circulating monocytes can infiltrate solid tissue into macrophages and participate in immune defense and injury repair processes. It can also activate and produce inflammatory reactions,45 promote abnormal coronary plaque status, induce atherosclerotic plaque rupture and thrombosis, and increase the risk of cardiovascular adverse events. Notably, abnormal reductions in lymphocyte counts indicate excessive apoptosis of lymphocytes, which not only weakens the function of the immune system but also promotes endothelial dysfunction, leading to abnormal aggregation and thrombosis after platelet activation.46 Complete blood cell count and CRP have been shown to have risk-predictive value in MINOCA.47,48 Unlike a single blood cell count, the composite index was less affected by factors such as body fluid changes. Recent studies have shown that some ratio-complete blood cell count derived indexes based on whole blood cell calculation can better reflect the inflammatory state of MINOCA and predict adverse cardiac outcomes than traditional inflammatory biomarkers. In a study including 72 patients with MINOCA, it was confirmed that NLR was a predictor of mortality within a median follow-up of 21 months.9 Mohammed et al also confirmed that WMR and NPR alone or in combination are independent predictors of long-term outcomes in the MINOCA population.8 Patients with high SIRI usually show increased neutrophils, increased monocytes, and decreased lymphocytes. This reveals the coexistence of nonspecific inflammation and adaptive immune response injury. Therefore, SIRI calculated by peripheral neutrophil, monocyte, and lymphocyte counts may be a powerful and reliable indicator of inflammation, which can better reflect the state of local immune response and systemic inflammation. SIRI was first used to predict the survival rate of pancreatic cancer patients receiving gemcitabine chemotherapy. Subsequently, it was found to have great potential in the prognosis of breast cancer, glioma, and nasopharyngeal carcinoma.49–51 Previous studies have shown that elevated SIRI increases the risk of stroke (ischemic and hemorrhagic stroke) and all-cause death.52 SIRI is positively correlated with the degree of coronary artery stenosis in elderly patients with ACS [75].SIRI 12 hours after PCI may be a more accurate and economical index to evaluate the long-term prognosis of STEMI patients.53 In this study, we found that SIRI levels were significantly associated with the risk of MACE in MINOCA patients. The clinical outcome of patients with high SIRI was worse than that of patients with low SIRI. The results of univariate and multivariable COX survival analysis showed that SIRI was an independent predictor of MACE in MINOCA patients. Even after adjusting for multiple clinical risk factors, SIRI is still associated with MACE risk. In addition, SIRI was added to the traditional cardiovascular risk model, and the results showed a significant incremental effect on the prediction of MACE.
The B-type natriuretic peptide (BNP) is a neurohormone primarily synthesized by ventricular myocytes and exists in the form of pro-BNP in cardiomyocytes. It is a member of the natriuretic peptide system and possesses vasodilatory, urine sodium excretion, sympathetic nervous system inhibition, and renin-angiotensin-aldosterone system inhibitory functions. The primary regulatory mechanism governing synthesis and secretion is myocardial wall stress. When cardiac volume expands and pressure load increases, pro-BNP is undergoes decomposition into active BNP and inactive NT-proBNP through the catalytic action of Corin and Furin proteolytic enzymes, resulting in a substantial release of these into the bloodstream, which can be quantified via immunoassay. In quantitative analysis, the measured value of NT-proBNP is more than 10 times higher than that of BNP, and it exhibits a relatively longer half-life. The blood concentration shows a positive correlation with the degree of cardiac dysfunction and is less susceptible to external factors (such as posture, activity, some therapies etc).54,55 Moreover, the plasma concentrations of NT-proBNP and BNP are approximately equal in healthy individuals. However, in cases of impaired cardiac function like heart failure and myocardial infarction, both markers are released at an increased rate, notably, the local NT-proBNP in the surrounding area is significantly up-regulated, with a more pronounced increase observed.54,56 The NT-proBNP exhibits characteristics such as an extended half-life, elevated blood concentration, robust stability, and resistance to interference when compared to BNP. NT-proBNP, a recognized biomarker in HF, plays an important role in myocardial dysfunction and the prognosis across various types of HF,57–59 extending its significance beyond HF alone. Previous studies have demonstrated the high sensitivity and specificity of NT-proBNP as an indicator for evaluating MI area size and left ventricular function in MI patients,60,61 Additionally, it serves as an early warning and diagnostic indicator for ST-segment elevation myocardial infarction (STEMI).62 There is increasing evidence suggests that NT-proBNP can also provide prognostic information for ACS patients. In the PRISM trial, sustained or new elevation of NT-proBNP levels within 72 hours after symptom onset was associated with an increased risk of cardiovascular events during the 30-day follow-up period.63 Elevated BNP values in patients with ACS are strongly independently associated with short - and long-term survival outcomes,64,65 leading to approval of NTproBNP levels for risk stratification in ACS.66 However, limited research has been conducted on MINOCA thus far, and the existing studies mainly focus on comparing clinical baseline levels.1,67 Our research expands on previous studies by exploring the prognostic importance of NT-proBNP in MINOCA patients, aim to elucidate whether it can provide any potential clinical prognostic value in this population. The results confirm that NT-proBNP levels are associated with increased risk of adverse cardiovascular events in MINOCA patients and can serve as an important indicator for risk stratification and prognosis assessment, either alone or in combination with other cardiac biomarkers and clinical indicators for more accurate patient evaluation. When used in conjunction with SIRI, predictive accuracy is further improved, providing more reliable evidence for clinical decision-making. In summary, NT-proBNP serves as a crucial cardiac biomarker offering valuable reference value for treatment and prognosis assessment of MINOCA patients, helping physicians identify high-risk individuals and take appropriate intervention measures.
Most importantly, when exploring the relationship between the combination of SIRI and NT-proBNP, we observed that the combined application of the two was significantly better than a single indicator in predicting clinical outcomes. Specifically, after fully adjusting the relevant covariates, the risk of adverse clinical outcomes faced by patients with high SIRI combined with high NT-proBNP was 2.618 times that of patients with low SIRI / low NT-proBNP. In addition, compared with the model that only included a single indicator, the model that introduced both SIRI and NT-proBNP showed a significant improvement in predictive ability. Interestingly, when performing multivariable COX proportional hazard regression analysis, the results of WMR, NLR, and NPR were consistent with previous studies and maintained consistency. However, in the analysis of CRP, we observed that the CRP level of patients in the MACE group was significantly higher than that in the non-MACE group, and this difference did not reach statistical significance after adjusting for confounding factors, which was contrary to some existing research conclusions. It should be emphasized that this is only a preliminary conclusion. Since this is a small-scale study, the results may be subject to bias. Our findings need further investigation to confirm. SIRI and NT-proBNP are limited as biomarkers, with SIRI reflecting systemic inflammation but with insufficient specificity and easily influenced by multiple factors, and NT-proBNP level affected by various non-cardiac factors. Both require standardization, and the results may vary due to treatment, age, gender, weight, and medication. Future studies need to expand the scope to explore their suitability in different patient populations and clinical settings.
In summary, the results of this study have important clinical significance. Both SIRI and NT-proBNP can independently predict adverse events in the prognosis of MINOCA patients, and the combined predictive value is better than the individual predictive value. SIRI can be calculated from complete blood cell count, and NT-proBNP is routinely tested on admission in patients with myocardial infarction. Both are cheap and easily available indicators. Given the high risk of severe cardiovascular events in MINOCA patients, early accurate diagnosis and effective treatment are essential. Evaluating SIRI and NT-proBNP not only helps to identify high-risk patients but also guides personalized intervention and reduces subsequent cardiovascular adverse events. This is essential to reduce the economic burden of MINOCA patients and improve their quality of life and prognosis. Based on the observational and retrospective nature of the trial, we can only conclude that no causal relationship can be established. The results still need to be further verified in multi-center prospective studies.
Limitations
This study has several limitations. Firstly, it is a single-center, observational, retrospective study with a relatively small sample size. This inherent limitation may result in data bias, an inability to fully adjust for potential confounding factors, and may restrict the statistical power to detect smaller yet clinically significant differences. Additionally, there may be subjective biases from patients and interpretive biases from the follow-up personnel during telephone follow-ups. Secondly, all patients were recruited from a single center, and our study population may not fully represent the broader population of MINOCA patients. Future research should aim to conduct a prospective, large-scale, multi-center clinical trial. It would also be beneficial to include more frequent blood count assessments, evaluation of plaque load, and other inflammatory biomarkers to validate our findings.
Conclusions
This study demonstrates that SIRI and NT-proBNP in MINOCA patients can be used to predict the occurrence of MACE and that SIRI and NT-proBNP, individually or in combination, may serve as reliable indicators for risk prediction, improving prediction for clinical outcomes in these patients. This can assist clinicians in determining management strategies, thus improving clinical prognosis for patients with MINOCA.
Data Sharing Statement
The data that support the findings of this study are not publicly available due to privacy and ethical restrictions. To obtain data from this study for academic research purposes, please make a formal request to the corresponding author. Requesters are required to provide specific research objectives, data usage plans, and measures to ensure data security and confidentiality. After necessary approval procedures, the corresponding author will consider providing the de-identified data.
Ethics Approval and Informed Consent
The study process was in accordance with the Declaration of Helsinki and was approved by the Ethics Review Committee of Zibo Central Hospital. The Ethics Review Committee approved exemptions from signing the informed consent form in accordance with national legal and institutional requirements.
Consent for Publication
The manuscript was approved by all authors for publication.
Acknowledgments
We sincerely thank the authors, reviewers, and editors for their invaluable contributions and efforts that have greatly enriched this.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Xu B, Abdu FA, Liu L. et al. Clinical outcomes and predictors of ST-elevation versus non-ST-elevation myocardial infarction with non-obstructive coronary arteries. Am J Med Sci. 2020;360(6):686–692. doi:10.1016/j.amjms.2020.07.016
2. Silvestre-Roig C, Braster Q, Ortega-Gomez A, Soehnlein O. Neutrophils as regulators of cardiovascular inflammation. Nat Rev Cardiol. 2020;17(6):327–340. doi:10.1038/s41569-019-0326-7
3. Khan A, Lahmar A, Riasat M, et al. Myocardial infarction with non-obstructive coronary arteries: an updated overview of pathophysiology, diagnosis, and management. Cureus. 2022;14(3):e23602. doi:10.7759/cureus.23602
4. Barr PR, Harrison W, Smyth D, Flynn C, Lee M, Kerr AJ. Myocardial infarction without obstructive coronary artery disease is not a benign condition (ANZACS-QI 10). Heart Lung & Circulation. 2018;27(2):165–174. doi:10.1016/j.hlc.2017.02.023
5. Stangret A, Dykacz W, Jabłoński K, et al. The cytokine trio - visfatin, placental growth factor and fractalkine - and their role in myocardial infarction with non-obstructive coronary arteries (MINOCA). Cytokine Growth Factor Rev. 2023;74:76–85. doi:10.1016/j.cytogfr.2023.08.009
6. Fan Z, Li Y, Ji H, Jian X. Prognostic utility of the combination of monocyte-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in patients with NSTEMI after primary percutaneous coronary intervention: a retrospective cohort study. BMJ Open. 2018;8(10):e023459. doi:10.1136/bmjopen-2018-023459
7. Azab B, Shah N, Akerman M, McGinn JT Jr. Value of platelet/lymphocyte ratio as a predictor of all-cause mortality after non-ST-elevation myocardial infarction. J Thromb Thrombolysis. 2012;34(3):326–334. doi:10.1007/s11239-012-0718-6
8. Mohammed AA, Liu L, Mareai RM, et al. Combination of white blood cell count to mean platelet volume ratio and neutrophil-to-platelet ratio predicts long-term adverse events in patients with MINOCA. Mediators Inflamm. 2022;2022:5642406. doi:10.1155/2022/5642406
9. Gürdal A, Keskin K, Siğirci S, Yildiz SS, Kiliçkesmez KO. Prognostic value of the neutrophil-to-lymphocyte ratio in patients with myocardial infarction with non-obstructive coronary arteries. Angiology. 2020;71(9):812–816. doi:10.1177/0003319720938621
10. Cao Y, Zheng X, Hu Y, et al. Levels of systemic inflammation response index are correlated with tumor-associated bacteria in colorectal cancer. Cell Death Dis. 2023;14(1):69. doi:10.1038/s41419-023-05602-9
11. Xia Y, Xia C, Wu L, Li Z, Li H, Zhang J. Systemic immune inflammation index (SII), system inflammation response index (SIRI) and risk of all-cause mortality and cardiovascular mortality: a 20-year follow-up cohort study of 42,875 US adults. J Clin Med. 2023;12(3):1128. doi:10.3390/jcm12031128
12. Li J, He D, Yu J, et al. Dynamic status of SII and SIRI alters the risk of cardiovascular diseases: evidence from Kailuan cohort study. J Inflamm Res. 2022;15:5945–5957. doi:10.2147/JIR.S378309
13. Zhang Y, Xing Z, Zhou K, Jiang S. The predictive role of systemic inflammation response index (SIRI) in the prognosis of stroke patients. Clin Interv Aging. 2021;16:1997–2007. doi:10.2147/CIA.S339221
14. Li Q, Ma X, Shao Q, et al. Prognostic impact of multiple lymphocyte-based inflammatory indices in acute coronary syndrome patients. Front Cardiovasc Med. 2022;9:811790. doi:10.3389/fcvm.2022.811790
15. Jering KS, Claggett BL, Pfeffer MA, et al. Prognostic importance of NT-proBNP (N-terminal pro-B-type natriuretic peptide) following high-risk myocardial infarction in the PARADISE-MI trial. Circulation. 2023;16(5):e010259. doi:10.1161/CIRCHEARTFAILURE.122.010259
16. Scirica BM, Kadakia MB, de Lemos JA, et al. Association between natriuretic peptides and mortality among patients admitted with myocardial infarction: a report from the ACTION registry(R)-GWTG™. Clin Chem. 2013;59(8):1205–1214. doi:10.1373/clinchem.2012.198556
17. Schellings DA, Adiyaman A, Dambrink JE, et al. Predictive value of NT-proBNP for 30-day mortality in patients with non-ST-elevation acute coronary syndromes: a comparison with the GRACE and TIMI risk scores. Vasc Health Risk Manag. 2016;12:471–476. doi:10.2147/VHRM.S117204
18. Zhu Y, He H, Qiu H, Shen G, Wang Z, Li W. Prognostic value of systemic immune-inflammation index and NT-proBNP in patients with acute ST-elevation myocardial infarction. Clin Interv Aging. 2023;18:397–407. doi:10.2147/CIA.S397614
19. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J. 2019;40(3):237–269. doi:10.1093/eurheartj/ehy462
20. Hicks KA, Mahaffey KW, Mehran R, et al. 2017 cardiovascular and stroke endpoint definitions for clinical trials. J Am Coll Cardiol. 2018;71(9):1021–1034. doi:10.1016/j.jacc.2017.12.048
21. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726. doi:10.1093/eurheartj/ehab368
22. Agewall S, Beltrame JF, Reynolds HR, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary arteries. Eur Heart J. 2017;38(3):143–153. doi:10.1093/eurheartj/ehw149
23. Niccoli G, Scalone G, Crea F. Acute myocardial infarction with no obstructive coronary atherosclerosis: mechanisms and management. Eur Heart J. 2015;36(8):475–481. doi:10.1093/eurheartj/ehu469
24. Hjort M, Eggers KM, Lakic TG, et al. Biomarker concentrations and their temporal changes in patients with myocardial infarction and nonobstructive compared with obstructive coronary arteries: results from the PLATO trial. J Am Heart Assoc. 2023;12(1):e027466. doi:10.1161/JAHA.122.027466
25. Hjort M, Eggers KM, Lindhagen L, et al. Increased inflammatory activity in patients 3 months after myocardial infarction with nonobstructive coronary arteries. Clin Chem. 2019;65(8):1023–1030. doi:10.1373/clinchem.2018.301085
26. Hung MY, Wu YH, Bamodu OA, et al. Activation of the monocytic α7 nicotinic acetylcholine receptor modulates oxidative stress and inflammation-associated development of coronary artery spasm via a p38 MAP-kinase signaling-dependent pathway. Free Radic Biol Med. 2018;120:266–276. doi:10.1016/j.freeradbiomed.2018.03.050
27. Kugiyama K, Ota Y, Kawano H, et al. Increase in plasma levels of secretory type II phospholipase A(2) in patients with coronary spastic angina. Cardiovasc Res. 2000;47(1):159–165. doi:10.1016/S0008-6363(00)00060-2
28. Kaikita K, Ogawa H, Yasue H, et al. Soluble P-selectin is released into the coronary circulation after coronary spasm. Circulation. 1995;92(7):1726–1730. doi:10.1161/01.CIR.92.7.1726
29. Soejima H, Irie A, Miyamoto S, et al. Preference toward a T-helper type 1 response in patients with coronary spastic angina. Circulation. 2003;107(17):2196–2200. doi:10.1161/01.CIR.0000066317.23972.CE
30. Suzuki H, Kawai S, Aizawa T, et al. Histological evaluation of coronary plaque in patients with variant angina: relationship between vasospasm and neointimal hyperplasia in primary coronary lesions. J Am Coll Cardiol. 1999;33(1):198–205. doi:10.1016/S0735-1097(98)00520-8
31. Ogawa H, Sakamoto T, Nishiyama K, et al. Elevated levels of soluble intercellular adhesion molecule-1 in the coronary circulation of patients with coronary organic stenosis and spasm. Jpn Circ J. 2000;64(3):170–176. doi:10.1253/jcj.64.170
32. Recio-Mayoral A, Rimoldi OE, Camici PG, Kaski JC. Inflammation and microvascular dysfunction in cardiac syndrome X patients without conventional risk factors for coronary artery disease. JACC Cardiovasc Imaging. 2013;6(6):660–667. doi:10.1016/j.jcmg.2012.12.011
33. Sinha A, Ma Y, Scherzer R, et al. Role of T-cell dysfunction, inflammation, and coagulation in microvascular disease in HIV. J Am Heart Assoc. 2016;5(12). doi:10.1161/JAHA.116.004243
34. Verma S, Kuliszewski MA, Li SH, et al. C-reactive protein attenuates endothelial progenitor cell survival, differentiation, and function: further evidence of a mechanistic link between C-reactive protein and cardiovascular disease. Circulation. 2004;109(17):2058–2067. doi:10.1161/01.CIR.0000127577.63323.24
35. Oikonomou E, Leopoulou M, Theofilis P, et al. A link between inflammation and thrombosis in atherosclerotic cardiovascular diseases: clinical and therapeutic implications. Atherosclerosis. 2020;309:16–26. doi:10.1016/j.atherosclerosis.2020.07.027
36. Kleinbongard P, Heusch G. A fresh look at coronary microembolization. Nat Rev Cardiol. 2022;19(4):265–280. doi:10.1038/s41569-021-00632-2
37. Hayes SN, Kim ESH, Saw J, et al. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American Heart Association. Circulation. 2018;137(19):e523–e557. doi:10.1161/CIR.0000000000000564
38. Pitliya A, Datta S, Kalayci A, et al. Eosinophilic inflammation in spontaneous coronary artery dissection: a potential therapeutic target? Med Hypotheses. 2018;121:91–94. doi:10.1016/j.mehy.2018.09.039
39. Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999;340(2):115–126. doi:10.1056/NEJM199901143400207
40. Daniel M, Ekenbäck C, Agewall S, et al. Risk factors and markers for acute myocardial infarction with angiographically normal coronary arteries. Am J Cardiol. 2015;116(6):838–844. doi:10.1016/j.amjcard.2015.06.011
41. Yang Y, Song C, Jia L, et al. Prognostic value of multiple complete blood count-derived indices in intermediate coronary lesions. Angiology;2023:33197231198678. doi:10.1177/00033197231198678
42. Vrints CJ. Pathophysiology of the no-reflow phenomenon. Acute Cardiac Care. 2009;11(2):69–76. doi:10.1080/17482940902978061
43. Petzold T, Zhang Z, Ballesteros I, et al. Neutrophil ”plucking” on megakaryocytes drives platelet production and boosts cardiovascular disease. Immunity. 2022;55(12):2285–2299.e2287. doi:10.1016/j.immuni.2022.10.001
44. Klopf J, Brostjan C, Eilenberg W, Neumayer C. Neutrophil extracellular traps and their implications in cardiovascular and inflammatory disease. Int J Mol Sci. 2021;22(2):559. doi:10.3390/ijms22020559
45. Ankeny RF, Hinds MT, Nerem RM. Dynamic shear stress regulation of inflammatory and thrombotic pathways in baboon endothelial outgrowth cells. Tissue Eng Part A. 2013;19(13–14):1573–1582. doi:10.1089/ten.tea.2012.0300
46. Harm T, Bild A, Dittrich K, et al. Acute coronary syndrome is associated with a substantial change in the platelet lipidome. Cardiovasc Res. 2022;118(8):1904–1916. doi:10.1093/cvr/cvab238
47. Eggers KM, Baron T, Hjort M, Nordenskjöld AM, Tornvall P, Lindahl B. Clinical and prognostic implications of C-reactive protein levels in myocardial infarction with nonobstructive coronary arteries. Clin Cardiol. 2021;44(7):1019–1027. doi:10.1002/clc.23651
48. Ciliberti G, Coiro S, Tritto I, et al. Predictors of poor clinical outcomes in patients with acute myocardial infarction and non-obstructed coronary arteries (MINOCA). Int J Cardiol. 2018;267:41–45. doi:10.1016/j.ijcard.2018.03.092
49. Qi Q, Zhuang L, Shen Y, et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer. 2016;122(14):2158–2167. doi:10.1002/cncr.30057
50. He Q, Li L, Ren Q. The prognostic value of preoperative systemic inflammatory response index (SIRI) in patients with high-grade glioma and the establishment of a nomogram. Front Oncol. 2021;11:671811. doi:10.3389/fonc.2021.671811
51. He WZ, Jiang C, Liu LL, et al. Association of body composition with survival and inflammatory responses in patients with non-metastatic nasopharyngeal cancer. Oral Oncol. 2020;108:104771. doi:10.1016/j.oraloncology.2020.104771
52. Jin Z, Wu Q, Chen S, et al. The associations of two novel inflammation indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res. 2021;14:131–140. doi:10.2147/JIR.S283835
53. Liu Y, Liu J, Liu L, et al. Association of systemic inflammatory response index and pan-immune-inflammation-value with long-term adverse cardiovascular events in ST-segment elevation myocardial infarction patients after primary percutaneous coronary intervention. J Inflamm Res. 2023;16:3437–3454. doi:10.2147/JIR.S421491
54. Hall C. Essential biochemistry and physiology of (NT-pro)BNP. Eur J Heart Fail. 2004;6(3):257–260. doi:10.1016/j.ejheart.2003.12.015
55. Hellenkamp K, von Haehling S. The relevance of biomarkers in acute heart failure. Der Internist. 2019;60(6):587–596. doi:10.1007/s00108-019-0606-7
56. Hall C. NT-ProBNP: the mechanism behind the marker. J Card Fail. 2005;11(5):S81–83. doi:10.1016/j.cardfail.2005.04.019
57. Schmitt W, Rühs H, Burghaus R, et al. NT-proBNP qualifies as a surrogate for clinical end points in heart failure. Clin Pharmacol Ther. 2021;110(2):498–507. doi:10.1002/cpt.2222
58. Salah K, Stienen S, Pinto YM, et al. Prognosis and NT-proBNP in heart failure patients with preserved versus reduced ejection fraction. Heart. 2019;105(15):1182–1189. doi:10.1136/heartjnl-2018-314173
59. Oremus M, Don-Wauchope A, McKelvie R, et al. BNP and NT-proBNP as prognostic markers in persons with chronic stable heart failure. Heart Fail Rev. 2014;19(4):471–505. doi:10.1007/s10741-014-9439-6
60. Steen H, Futterer S, Merten C, Jünger C, Katus HA, Giannitsis E. Relative role of NT-pro BNP and cardiac troponin T at 96 hours for estimation of infarct size and left ventricular function after acute myocardial infarction. J Cardiovasc Magn Reson. 2007;9(5):749–758. doi:10.1080/10976640701544589
61. Talwar S, Squire IB, Downie PF, et al. Profile of plasma N-terminal proBNP following acute myocardial infarction; correlation with left ventricular systolic dysfunction. Eur Heart J. 2000;21(18):1514–1521. doi:10.1053/euhj.1999.2045
62. Shanmuganathan M, Masi A, Burrage MK, et al. Acute response in the noninfarcted myocardium predicts long-term major adverse cardiac events after STEMI. JACC Cardiovasc Imaging. 2023;16(1):46–59. doi:10.1016/j.jcmg.2022.09.015
63. Heeschen C, Hamm CW, Mitrovic V, Lantelme NH, White HD. N-terminal pro-B-type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation. 2004;110(20):3206–3212. doi:10.1161/01.CIR.0000147611.92021.2B
64. Omland T, Aakvaag A, Bonarjee VV, et al. Plasma brain natriuretic peptide as an indicator of left ventricular systolic function and long-term survival after acute myocardial infarction. Comparison with plasma atrial natriuretic peptide and N-terminal proatrial natriuretic peptide. Circulation. 1996;93(11):1963–1969. doi:10.1161/01.CIR.93.11.1963
65. Jernberg T, Stridsberg M, Venge P, Lindahl B. N-terminal pro brain natriuretic peptide on admission for early risk stratification of patients with chest pain and no ST-segment elevation. J Am Coll Cardiol. 2002;40(3):437–445. doi:10.1016/S0735-1097(02)01986-1
66. Morrow DA, Braunwald E. Future of biomarkers in acute coronary syndromes: moving toward a multimarker strategy. Circulation. 2003;108(3):250–252. doi:10.1161/01.CIR.0000078080.37974.D2
67. Zhang S, Zhang X, Wu S, et al. Analysis of clinical features and the outcome of in-hospital mortality of myocardial infarction with non-obstructive coronary arteries. Zhonghua xin xue guan bing za zhi. 2022;50(9):873–880. doi:10.3760/cma.j.cn112148-20220531-00429
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Metabolic Score for Insulin Resistance (METS-IR) Predicts Adverse Cardiovascular Events in Patients with Type 2 Diabetes and Ischemic Cardiomyopathy
Zhang X, Liu F, Li W, Zhang J, Zhang T, Yu X, Luo J, Zhao Q, Zhang J, Fang B, Yang Y, Li X
Diabetes, Metabolic Syndrome and Obesity 2023, 16:1283-1295
Published Date: 5 May 2023
Association of Systemic Inflammation Response Index with Short-Term All-Cause Mortality in Decompensated Liver Cirrhosis Patients
Cheng J, Ju H, Wang G, He C, Wang W
Journal of Inflammation Research 2024, 17:8985-8995
Published Date: 18 November 2024







