Back to Journals » Risk Management and Healthcare Policy » Volume 18
Quality Assessment of Plain Chest X-Rays of the Expatriates in Jordan: Multi-Centres Study
Authors Ayasrah M , Al Hrout RA, Rawahneh K
Received 29 November 2024
Accepted for publication 12 March 2025
Published 20 March 2025 Volume 2025:18 Pages 933—945
DOI https://doi.org/10.2147/RMHP.S507002
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Mohammad Ayasrah,1 Rasha Aeadah Al Hrout,2,3 Khaleel Rawahneh4
1Department of Allied Medical Sciences, Faculty of Applied Medical Science, Jordan University of Science and Technology, Irbid, 22110, Jordan; 2Medical Radiologic Technologies, College of Allied Medical Sciences, Zarqa University, Zarqa, 13132, Jordan; 3MSc. School of Physics, Universiti Sains Malaysia, USM, Penang, 11800, Malaysia; 4Madaba Health Directorate, Ministry of Health, Madaba, 17110, Jordan
Mohammad Ayasrah
Department of Allied Medical Sciences, Faculty of Applied Medical Sciences, Jordan University of Science and Technology, P.O. Box 3030, Irbid, 22110, Jordan
, Tel +962 27201000-26939
, Fax +962 27201087
, Email [email protected]
Background: High-quality diagnostic imaging is critical to patient safety and effective healthcare. This study assesses the quality of plain chest X-rays (CXR) for expatriates in Jordan, with a focus on complying to American College of Radiology (ACR) and European Commission (EC) criteria at 12 healthcare facilities.
Methods: A retrospective cross-sectional evaluation of 1020 CXR radiographs from 2023 was performed. A quantitative classification approach was used to assess CXR for ACR and EC compliance, which included exposure, anatomical visibility, organ superimposition, and image annotation.
Results: Only 15% of CXRs passed all of the quality standards. While exposure and anatomical visualization demonstrated adequate compliance, organ superimposition and image annotation were much lower, at 23% and 29%, respectively, revealing gaps that may impact diagnostic accuracy and patient safety.
Conclusion: Significant discrepancies in CXR quality highlight the need for enhanced training, rigorous adherence to imaging protocols, and robust quality control to improve diagnosis accuracy and patient outcomes, especially in expatriate screening programs.
Keywords: patient safety, diagnostic imaging quality, radiographic standards compliance, digital radiography, healthcare quality
Introduction
Maintaining quality standards in healthcare imaging is essential for improving diagnostic services and ensuring patient safety.1 The Middle East attracts a significant expatriate workforce due to economic opportunities, which presents unique healthcare challenges, as these populations frequently have distinct health needs compared to local residents.2,3 Expatriates often navigate transitions between countries that possess varying healthcare infrastructures, which complicates the maintenance of consistent healthcare standards.4 The quality assessment (QA) of CXR is crucial for enhancing clinical outcomes and informing treatment strategies.5 Effective QA optimizes image quality, decreases patient radiation exposure, and reduces the need for repeat.6 Plain CXR are the most performed diagnostic x-ray examination.7 In 2016, approximately 691 million radiographic procedures were performed in the United States, including CT scans, dental imaging, and nuclear medicine testing.8 CXR constituted almost 44% of all radiographs. The majority of these radiographs (48%) were obtained in outpatient clinics.9 This distribution reflects the significant demand for and broad accessibility to x-ray services.
CXR are an essential diagnostic tool extensively used for the screening and diagnosis of numerous thoracic disorders, including tuberculosis (TB), pneumonia, lung cancer, and cardiovascular disorders. CXR is frequently mandated for expatriates as a screening tool during visa or work placement health assessments in countries such as the USA, Canada, Oman, and Jordan to identify infectious diseases like TB.10–13 In Jordan, expatriates seeking work permits must complete CXR screenings as a component of a national TB control initiative for optimal healthcare and patient safety.14–16
High-quality imaging is essential for accurate diagnoses across various conditions. Suboptimal image quality may result in misdiagnoses, postponed treatments, and jeopardized patient safety, affecting not only tuberculosis but also other significant health conditions identifiable through chest radiographs. Consistently achieving high-quality CXR interpretations is challenging due to various medical and technical factors that can introduce errors or artifacts, thereby impacting diagnostic accuracy.17 Misdiagnoses in infectious diseases such as tuberculosis can lead to swift disease transmission and increased pressure on healthcare systems, underscoring the need for optimized, quality-controlled CXR imaging.18
The transition from conventional film-based radiography to digital imaging, predominantly utilizing DICOM formats, has enhanced image storage, portability, and accessibility.19
Several regulatory entities, such as the ACR)20 and the European Commission’s Directorate-General for Research and Innovation (ECDGRI),21 have formulated guidelines to guarantee high-quality CXRs that facilitate precise pulmonary diagnostics. These guidelines emphasize essential imaging aspects including adequate inspiration, rotation, organ superimposition, exposure, anatomical coverage, and appropriate image annotation, which are vital for generating diagnostically valid images.20,22
However, previous studies have shown that adherence to these quality standards can vary considerably among regions. Research conducted by Okeji et al revealed that at a Nigerian teaching hospital, only 16%, 14%, and 32% of CXR assessed from 2014 to 2016 met all European diagnostic quality standards each year, with common deficiencies such as inadequate collimation, incorrect scapula positioning, and inferior darkroom processing.23
Chand et al found that merely 52.3% of the 1101 evaluated CXRs met European quality standards, whereas 47.7% were substandard due to insufficient inspiration, penetration, and rotation.24
Liaqat et al noted in their research at the Pakistan Institute of Medical Sciences that 61.8% of 1560 CXR had radiographic problems, with positioning errors accounting for 16.5% of the rejected images.25 A recent study by Suwal et al in Nepal revealed that only 22.2% of 450 CXR at Tribhuvan University Teaching Hospital met European standards, showing exceptional anatomical coverage compliance (97.56%) but significant deficiencies in rotation (55.56%) and scapula positioning (42.22%).26
The Ministry of Health (MoH) of Jordan administers a nationwide tuberculosis screening program for expats, having performed 90,176 CXR in 2023 alone.27 Notwithstanding the scale of this initiative, a thorough assessment of CXR quality across these facilities has yet to be conducted. This study seeks to evaluate the quality of CXR from 12 Centers for Chest Diseases and Health of Expatriates (CCDHE) in Jordan, adhering to the standards established by the ACR and the ECDGRI. This study underscores the critical necessity for standardized imaging protocols to rectify site-specific quality disparities, hence enhancing patient safety and improving diagnostic accuracy in expatriate healthcare.
Materials and Methods
This retrospective observational research evaluates the quality of CXRs of expatriates in Jordan, specifically examining conformity to the criteria set by the ACR and European guidelines. The study was carried out between April and December 2023 using a single-phase cluster sampling technique. Specifically, all the 12 CCDHE in Jordan were selected. This method is especially appropriate for observational studies, since it produces reliable estimates of the frequency of inadequate radiography techniques among expatriates.
Sample Size
The sample size was determined using a proportion-based methodology to guarantee accurate data representation. A conservative estimate of 30% was chosen since previous research indicated that adherence to X-ray quality criteria was on average thirty 30%.23 Utilizing a Z-score of 1.96 for a 95% confidence interval and a 5% margin of error, the minimum requisite sample size was 323 CXRs. To improve accuracy and deliver a thorough review, the study was broadened to encompass all CCDHEs, facilitating a more extensive assessment of X-ray quality across locations and assuring adequate statistical power to detect significant differences.
Sampling Method
For a broad sample, three CCDHEs from the northern, central, and southern regions of Jordan were chosen for a pilot study, while the other nine were systematically allocated to different areas. The study encompassed all CXR conducted throughout the study period, except those for pre-employment exams of Jordanian citizens. Ethical approval was obtained from the Institutional Review Board (IRB) at Jordan University of Science and Technology (Approval No. 4/2022, dated 2/6/2022). IRB determined that individual informed consent was not required for this study. This decision was based on the nature of the research, which involved anonymized radiographic data collected from healthcare centers without direct involvement of individual patients. The management of seven CCDHEs gave permission for anonymised chest radiographs to be viewed and analysed. There was no direct patient involvement in the study, and no personally identifiable patient information was utilized.
A total of 1020 CXR were acquired in DICOM format or conventional film, yielding a comprehensive dataset for analysis to evaluate regional discrepancies and quality standards across CCDHEs.
Analysis Parameters
Methods of Analysis
The initial analysis included using descriptive statistics to provide a summary of the data. Categorical variables, such as the quality categories of chest radiographs, were described using proportions according to recognized recommendations. The mean and standard deviation (SD) will be computed for continuous data to provide measures of central tendency and dispersion, respectively.
Evaluation of Radiographic Image Quality
The chest radiographs were evaluated according to the quality standards established by the ACR and the ECDGRI illustrated in Table 1. The assessment encompassed eight distinct categories, each essential for determining the overall quality of the CXR imaging.
Two radiographers participated in the evaluation process. These radiographers have 8–10 years of professional experience and varied in their level of expertise. Both were radiologic technology master’s degree holders who had undergone specialized training in the ACR and ECDGRI standards to guarantee uniform and consistent image evaluations. An Inter-Rater Reliability (IRR) analysis was performed to evaluate the reliability and consistency of the assessments. The radiographers conducted an independent review of all 1020 CXR images, and the agreement level between their assessments was quantified using Cohen’s Kappa statistic.
 |
Table 1 Criteria for Radiographic Image Evaluation |
Equipment
The majority of the participating CCDHEs had just completed renovations and acquired new digital radiography equipment via an international assistance grant. Five facilities utilized Carestream’s DRX-Compass X-ray Systems, and two locations employed analogue systems from Shimadzu with wet processing. All images obtained during the trial were examined on radiology workstations with dual 3-megapixel screens, facilitating high-resolution image evaluation and precise assessment. This updated configuration enabled accurate assessment and uniformity in the evaluation of radiographic quality.
Data Management
The radiographs were uploaded to the PACS (Picture Archiving and Communication System) account for safe and efficient administration. Radiographers, supervised by radiologists, assessed each image by using the criteria outlined in Table 1 to evaluate the quality of each radiograph.
Results
The study had 1020 participants, of which 65.2% were male, aged 21 to 48 years (mean: 29.6, SD: 6.2). A majority of participants (41.2%) originated from northern Jordan. Commonly utilized radiographic settings are 125/110 kVp and 3/5 mAs. Significantly, 88.2% of radiographs employed digital technology, underscoring a substantial transition to digital imaging in clinical practice.
In assessing the quality of chest radiographs, it is crucial to take into account both specific criteria and overall performance. Although certain components adhered to high standards, hardly 15% of radiographs concurrently fulfilled all quality criteria (Figure 1). This indicates a substantial disparity between fulfilling specific standards and attaining overall excellence in radiographic imaging.
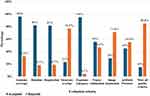 |
Figure 1 Acceptance and rejection rates for various CXR radiographic quality control metrics. |
An Inter-Rater Reliability (IRR) assessment was performed between two independent radiographers to ensure consistency and reliability in radiographic image evaluations. Nine criteria were evaluated, and binary decisions (Accepted/Rejected) were documented for each criterion by both readers. The radiographers’ agreement was measured using Cohen’s Kappa coefficient. The IRR analysis revealed complete concordance between the two readers, indicated by a Cohen’s Kappa value of 1.0. The result demonstrates consistent evaluation of CXR image quality across all criteria, highlighting the robustness and reliability of the assessment methodology used in this study.
The comprehensive evaluation of CXR quality subcategorization encompassed various parameters, including patient information, anatomical coverage, complete inspiration, artifacts, overlapping structures, radiography exposure, rotation, and collimation. Each criterion was carefully assessed to ascertain the overall quality of the CXR images.
The analysis of the “Image Annotation” subcategory indicated an acceptance rate of 29% and a rejection rate of 71%. Frequent mistakes comprised absent orientation indicators and annotations that obscured critical diagnostic areas, especially in analogue systems.
Notwithstanding discrepancies, certain criteria exhibited robust compliance. In terms of rotation, 82% of the radiographs were perfectly aligned, and 95% had sufficient exposure, which allowed anatomical details to be clearly seen. Nonetheless, a noteworthy issue was the occurrence of artifacts, affecting 55% of the radiographs and markedly diminishing diagnostic efficacy.
Anatomical overlap and collimation presented further difficulties. Merely 23% of images successfully avoided the overlap of closely neighbouring structures, which is essential for accurate sickness diagnosis. Collimation was correctly implemented in 55% of cases, suggesting a common occurrence of x-ray beam extension beyond the area of interest, which may result in excessive radiation exposure and diminished image quality. Notably, 81% of cases exhibited sufficient respiration during the imaging procedure.
The evaluation of rotation and symmetry, measured by the equidistant distance between the Sternoclavicular Joint (SCJ) and the adjacent spinous process of the thoracic vertebrae, indicated that deviations over 10 mm, classified as “Inadequate”, represented 18.1% of all cases, as illustrated in Table 2. Only 4.4% attained a ‘Perfect’ rating with no tangible variation (0 mm), whilst the rest, 77.5%, were classified into ‘Good’ and ‘Moderate’ categories, exhibiting variances between 1 and 9.99 mm. These findings indicate improved compliance with tolerance ranges that conform to globally recognized standards. “Of those rejected cases classified as Inadequate”, 185 cases were found to be 18.1% of the dataset (N=1020). The analysis of rotation direction indicated a marginal predominance of rightward rotation, observed in 51.4% of cases (95 cases), relative to leftward rotation at 48.6% (90 instances), as illustrated in Figure 2.
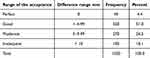 |
Table 2 Distribution of Radiographic Acceptance Levels by Deviation in Rotation and Symmetry Measurements |
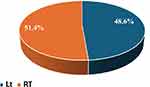 |
Figure 2 Distribution of Left and Right Rotation in Rejected Cases Classified as ‘Inadequate. |
The analysis of artifact acceptance rates, presented in Table 3, indicates notable gender disparities. The acceptance rate for males was 57.7%, whereas for females it was 21.1%. Chi-square tests demonstrated the statistical significance of these differences, with all results yielding a p-value of <0.001.
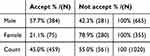 |
Table 3 Artifact Acceptance Rates by Gender |
The study analyzed radiographic collimation by categorizing it into four classifications as shown in Table 4: “Perfect”, “Good”, “Moderate”, and “Inadequate”, according to compliance with OEA criteria. Merely 7.6% of the sample attained “Perfect” adherence. In contrast, a majority (52.5%) were classified as “Inadequate”, with exposures surpassing 60% of the OEA. Only 25.6% of instances achieved “Perfect” or “Good” standards, underscoring considerable problems with excessive exposure in radiography treatments.
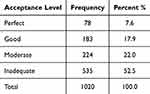 |
Table 4 Distribution of Collimation Acceptance Levels |
Discussion
Introduction
In this study, 1020 cases were evaluated, with a majority being male (65.2%). Participants, primarily undergoing chest radiographs for work permit purposes, had an average age of 29.6 years (SD=6.2; range: 21–48), aligning with the working age range of 20–80 years.31 The primary objective was to assess chest radiograph quality using criteria such as patient information, anatomical coverage, full inspiration, artifacts, overlapping structures, radiographic exposure, rotation, and collimation, essential for diagnostic excellence. Notably, 88.2% of radiographs utilized digital imaging, reflecting a shift toward advanced technology. However, only 15% met all quality requirements, highlighting discrepancies between individual criterion compliance and overall quality achievement.
Novel Features of the Study
The present study introduces an important improvement in the evaluation of CXR quality through a comprehensive and quantitative classification system termed Perfect, Good, Moderate, and Inadequate (PGMI). This distinctive approach to CXR assessment is influenced by the high standards employed in mammography quality assurance.32 It seeks to enhance the precision of evaluations by a methodical and comprehensive analysis. Historically, CXR evaluations have been subjective; however, our application of this methodology offers a level of precision that facilitates the correct identification of deviations in the quality requirements of CXR imaging.
The PGMI categorization system for rotation and symmetry was meticulously developed with specific measurement criteria for each category: ‘Perfect’ required no apparent deviation from ideal norms, while “Good’ permitted modest variations of up to 5 mm; (Figure 3A).”Moderate’ included errors between 5 mm and 9 mm, while ‘Inadequate’ included deviations beyond 10 mm (Figure 3B). The implementation of these quantifiable criteria signifies a transition from less precise methodologies, providing a framework that highlights minor fluctuations that could influence diagnostic outcomes. This stringent methodology not only improves the understanding of each CXR but also fosters a culture of precision in radiographic evaluation techniques.
The PGMI framework is can also be used to assess collimation quality to minimize radiation exposure to ensure safety and enhance image clarity. Optimal collimation necessitates a span of 5 cm above the shoulders and below the 12th rib, encompassing both acromioclavicular joints. This standard delineates compliance with clinically pertinent domains.
We computed the OEA, AEA, and EEA. The OEA is the multiplication of the chest width (biacromial distance) and trunk width (Figure 4A). The AEA is defined by the horizontal and vertical film dimensions (Figure 4B). The EEA, indicative of unnecessary exposure, is the difference between AEA and OEA. Overexposure ratio was defined as follows: Overexposure = (Exposed Area - Optimum Area)/Optimal Area. To classify the degree of overexposure, specific ranges were established to evaluate quality. A score ranging from 0 to 0.2 is classified as “Perfect”, representing optimal exposure with minimal overexposure. Scores between 0.201 and 0.4 are categorized as “Good”, indicating acceptable levels of exposure. Scores within 0.401 to 0.6 are labelled as “Moderate”, highlighting suboptimal exposure that may affect diagnostic quality. Finally, any score exceeding 0.601 is classified as “Inadequate”, reflecting excessive exposure that compromises both image quality and patient safety. This structured approach ensures consistent assessment of exposure levels across radiographic evaluations.
We aim to improve radiography quality, patient safety, and diagnostic accuracy by incorporating these novel approaches into standard practice. This work is distinguished by the application of PGMI technology, emphasizing critical aspects for enhancing CXR quality. PGMI serves as a comprehensive instrument that evaluates both rotation and collimation, hence greatly influencing diagnostic image quality and patient safety.
Overall Results
The compliance rate observed in the study was 15%, which is consistent with previously reported low rates, including 14% in Okeji et al23 and 22% in Suwal et al26 as displayed in Table 5. Chand R B’s study24 demonstrated an adherence rate of 52%, suggesting improved compliance. Low compliance is frequently attributed to multiple errors within a single image, particularly in regions such as organ superimposition (23%) and image annotations (29%). The frequent inconsistencies notably impact overall acceptance rates, indicating difficulties in upholding diagnostic imaging standards.
 |
Table 5 Comparative Analysis of Compliance with Diagnostic Imaging Quality Standards Across Multiple Studies |
Rotation and Symmetry
Our results indicate an 82% rotation and symmetry compliance rate, which is higher than the average of previous studies (53%), and comparable to Chand R B’s 78.2%.24 This exceeds the rates reported by Abubakar et al (32.3%)33 and Okeji et al (28%).23 Rotation and symmetry are essential for assessing heart size, tracheal deviation, and costophrenic angles. Right-sided rotation leads to an underestimation of heart size, whereas left-sided rotation results in an overestimation.34 Lung soft tissue thickness, influenced by rotation, may distort the representation of lung disease, while chest asymmetry complicates assessments of tracheal deviation.35 The detailed categorization in our study enhanced the understanding of alignment challenges.
Appropriate Collimation
The collimation adherence rate in our study was 55%, which is lower than the 58.8% reported by Abubakar et al33 and significantly below the rates observed by Okeji et al.23 This disparity highlights the necessity for enhancements that ensure that radiation is restricted to the relevant clinical area. The quantitative evaluation of the PGMI system underscores the necessity of thorough training and strict compliance with collimation standards, which are critical for reducing radiation exposure and enhancing diagnostic image quality.
Adequate Inspiration
CXRs are routinely conducted at end-deep inspiration to optimize lung volume visualization and reduce blurring of lung bases.36 Insufficient inspiration may resemble erroneous pathologies, including mediastinal or cardiac enlargement.37 Proper inspiration is evidenced by the visibility of at least 9 posterior or 7 anterior ribs on a PA CXR. Figure 5 indicates that the majority of patients in the study exhibited 9 or 10 visible ribs, representing 39% and 38% of the cases, respectively.
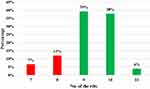 |
Figure 5 Distribution of Respiration Levels by Visible Rib Count. |
This study attained an inspiration compliance rate of 81%, which is lower than the rate reported by Okeji et al (97%)23 but higher than that of Chand R B (65.2%).24 Suwal et al documented a compliance rate of 92.9%, whereas Abubakar et al33 reported a slightly lower rate of 83.8% in their study. The observed variations indicate discrepancies in protocol adherence, methodologies, or the quality of equipment utilized across studies.
Artifacts Management
The management of artifacts plays a crucial role in determining the diagnostic value of radiographs. Artifacts were present in 55% of the images, potentially obscuring essential diagnostic details. Earlier research indicated reduced rates, with Okeji et al23 reporting 31% and Abubakar et al reporting 17%.33 Significant gender disparities in artifact acceptance were observed, with males demonstrating a higher acceptance rate of 57.7% in contrast to females at 21.1%.
The prevalence of artifacts varied, with most cases (96.4%) exhibiting 1 to 4 artifacts, while only 3.6% displayed as many as 14 artifacts (Figure 6). The average number of artifacts per image was 1.9 (SD = 2.8), indicating significant variability.
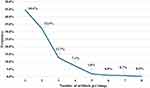 |
Figure 6 Frequency Distribution of Artifacts in Chest Radiographs. |
The most common artifact identified was related to brassieres (Figure 7). Requiring patients to remove objects from the waist up during routine CXR reduces artifacts, particularly with digital receptors, which are more capable of detecting subtle details, such as t-shirt stencils, compared to traditional films.38
Appropriate Exposure and Penetration
Digital and analogue CXR devices vary in exposure efficacy, which is essential for precise diagnosis. Digital radiography attained optimal exposure in all 900 cases owing to sophisticated processing capabilities. Conversely, Table 6 indicates that analogue systems achieved accurate exposure in 56.7% of cases, with 30% underexposed and 13.3% overexposed, potentially obscuring essential diagnostic information.
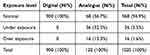 |
Table 6 Comparison of Exposure Levels in Digital and Analogue CXR Systems |
The results indicate that digital systems exhibit superior performance, achieving “Appropriate Exposure and Penetration” rates of 95%, which exceed the findings of previous studies by Suwal et al (82%), Chand R B (76%),24 and Abubakar et al (65.4%).33 The enhancement is linked to the extensive implementation of digital technology, currently utilized in 88.2% of radiographs. The findings underscore the significance of adopting digital systems in clinical environments to improve diagnostic precision and minimize errors associated with exposure concerns.
Organ Superimposition and Coverage
The research indicated a low efficacy in minimizing scapula superimposition over the lung field, achieving a success rate of merely 23%. The observed rate is considerably lower than those documented in previous studies: Suwal et al (57.8%), Chand R B (85.3%),24 Okeji et al (61%), and Abubakar et al (65.4%).33 The low success rate suggests problems with the implementation or adherence to appropriate CXR techniques, especially the failure to advance the shoulders forward to avoid scapula overlap. This step is essential for improving the visibility of lung abnormalities and the accuracy of diagnoses. Enhanced training and stricter compliance with protocols are crucial for optimizing the quality of PA CXR in clinical practice.
Limitations of the Study
This research possesses multiple limitations. The cross-sectional, retrospective approach restricts the capacity to determine causality or evaluate alterations in radiography quality over time. While 1020 CXR radiographs from 12 CCDHEs were examined, the emphasis on centers designated for expatriate screenings may restrict the generality of the findings to other locations or healthcare environments. Furthermore, the study focused on quantitative evaluations rather than examining qualitative elements that can provide more profound understanding of the reasons behind quality disparities, such as radiographer training or protocol adherence.
Conclusions
This study assessed the adequacy of factor of CXR for expatriates in Jordan in accordance with ACR and EC guidelines. Despite advancements in digital radiography, only 15% of CXRs adhered to all quality standards, exhibiting particularly low compliance in organ superimposition at 23% and image annotation at 29%. A novel quantitative classification method, derived from mammography, has been introduced to enhance assessment. The results highlight the necessity for improved training and rigorous compliance with protocols. Future research should investigate qualitative factors influencing image quality and evaluate the long-term effects of targeted interventions on diagnostic accuracy and patient safety.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical Approval
The IRB at Jordan University of Sciences and Technology granted ethical approval for this study (Approval No. 4/2022, dated 2/6/2022), confirming adherence to ethical standards. The research focused on assessing the quality of chest radiography in healthcare facilities, without direct involvement of individual patients. Consequently, The IRB determined that individual consent was not required as the study exclusively involved anonymized data from healthcare centers, with no direct involvement of identifiable human participants. This approach aligns with institutional research guidelines for studies utilizing non-identifiable data. Data were managed with strict confidentiality, ensuring that no identifiable patient information was utilized in the study.
Acknowledgments
The authors express their sincere gratitude to the Ministry of Higher Education and Scientific Research for its financial support of this study. We express deep appreciation to the Deanship of Research at Jordan University of Science and Technology for their indispensable contribution in overseeing and handling the financial parts of the financing. Their meticulous supervision and operational assistance were essential to the successful implementation of our study endeavour.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by the Ministry of Higher Education and Scientific Research of Jordan through the Scientific/Research and Innovation Support Fund, grant number MPH/1/55/2022, dated 3/7/2023. The Deanship of Research at Jordan University of Science and Technology (JUST) expertly managed the administration and oversight of the funding.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Mosadeghrad AM. Factors influencing healthcare service quality. Int J Health Policy Manag. 2014;3(2):77–89. doi:10.15171/ijhpm.2014.65
2. Mansfeld Y, Winckler O. The role of the tourism industry in transforming a rentier to a long-term viable economy: the case of Bahrain. Curr Issues Tour. 2008;11(3):237–267. doi:10.1080/13683500802140307
3. Mello SF, Tomei PA. The impact of the COVID‐19 pandemic on expatriates: a pathway to work‐life harmony? Glob Bus Organ Excell. 2021;40(5):6–22. doi:10.1002/joe.22088
4. Biswas T, Mäkelä L, Andresen M. Work and non-work-related antecedents of expatriates’ well-being: a meta-analysis. Hum Resour Manag Rev. 2022;32(3):100889. doi:10.1016/j.hrmr.2021.100889
5. Andronikou S, Lambert E, Halton J, et al. Guidelines for the use of chest radiographs in community-acquired pneumonia in children and adolescents. Pediatr Radiol. 2017;47(11):1405–1411. doi:10.1007/s00247-017-3944-4
6. Tompe A, Sargar K. X-ray image quality assurance. StatPearls. StatPearls Publishing; 2024. Available from. http://www.ncbi.nlm.nih.gov/books/NBK564362/.
7. Guo R, Passi K, Jain CK. Tuberculosis diagnostics and localization in chest X-Rays via deep learning models. Front Artif Intell. 2020;3:583427. doi:10.3389/frai.2020.583427
8. Mahesh M, Ansari AJ, Mettler FA. Patient exposure from radiologic and nuclear medicine procedures in the United States and worldwide: 2009–2018. Radiology. 2023;307(1):e221263. doi:10.1148/radiol.221263
9. Singh R, Kalra MK, Nitiwarangkul C, et al. Deep learning in chest radiography: detection of findings and presence of change. PLoS One. 2018;13(10):e0204155. doi:10.1371/journal.pone.0204155
10. Singh J, Al-Abri S, Petersen E, et al. Importance of tuberculosis screening of resident visa applicants in low TB incidence settings: experience from Oman. J Epidemiol Glob Health. 2022;12(3):281–291. doi:10.1007/s44197-022-00040-w
11. Lim J. Analysis of five years of US immigration medical exams. Korean J Aerosp Environ Med. 2021;31(3):77–81. doi:10.46246/KJAsEM.210018
12. Ubaidi BAA. Tuberculosis screening among expatriate in Bahrain. 4(3): 282–288.
13. International Organization for Migration. Enhancing Access to Prevention and Health Care for Syrian Refugees in Jordan. Published online 2014. Available from: https://www.iom.int/sites/g/files/tmzbdl486/files/2018-07/IOM%20Jordan%20Emergency%20Health%20Response%20%26%20Syria%20Crisis%20info%20sheet%20August%2020.pdf.
14. Hassan FMA, Al-Saci D. Jordan: Supporting Stable Development in a Challenging Region: A Joint World Bank-Islamic Development Bank Evaluation. World Bank; Islamic Development Bank; 2004.
15. United Nations High Commissioner for Refugees U. Work Permits for Syrian Refugees in Jordan. UNHCR Jordan. 2024. Available from: https://help.unhcr.org/jordan/en/frequently-asked-questions-unhcr/work-permit-syrian-faqs/https%3A%2F%2Fhelp.unhcr.org%2Fjordan%2Fen%2Ffrequently-asked-questions-unhcr%2Fwork-permit-syrian-faqs%2F.
16. Herrera Diaz M, Haworth-Brockman M, Keynan Y. Review of evidence for using chest x-rays for active tuberculosis screening in long-term care in Canada. Front Public Health. 2020;8:16. doi:10.3389/fpubh.2020.00016
17. Jones CM, Buchlak QD, Oakden‐Rayner L, et al. Chest radiographs and machine learning – past, present and future. J Med Imaging Radiat Oncol. 2021;65(5):538–544. doi:10.1111/1754-9485.13274
18. Koppaka R, Bock N. Chest radiography in tuberculosis detection. In: Toman’s tuberculosis: case detection, treatment, and monitoring. questions and answers. 2nd ed. World Health Organization; 2004. Availale from: https://iris.who.int/bitstream/handle/10665/252424/?sequence=1.
19. INTERNATIONAL ORGANIZATION FOR MIGRATION I. Screening Chest X-Ray Interpretations and Radiographic Techniques.
20. Donnelly EF, Kazerooni EA, Lee E, et al.; Expert Panel on Thoracic Imaging. ACR appropriateness criteria® lung cancer screening. J Am Coll Radiol JACR. 2018;15(11S):S341–S346. doi:10.1016/j.jacr.2018.09.025.
21. Carmichael J, Maccia C, Moores B. European guidelines on quality criteria for diagnostic radiographic images. Published online 1996. Available from: https://www.sprmn.pt/pdf/EuropeanGuidelineseur16260.pdf.
22. Teoh EJ, Nazir S, Benamore R. Adapted anatomical image criteria for PA chest radiography | the royal college of radiologists. adapted anatomical image criteria for PA chest radiography. 2022. Avalable from: https://www.rcr.ac.uk/career-development/audit-quality-improvement/auditlive-radiology/adapted-anatomical-image-criteria-for-pa-chest-radiography/.
23. Okeji M, Agwuna K, Abubakar U, Izge I, Aninworie A, Arogundade I. Evaluation of diagnostic quality of chest radiographs seen in a Nigerian teaching hospital. J Adv Med Res. 2017;23(3):1–635114. doi:10.9734/JAMMR/2017/35114
24. Chand RB, Thapa N, Paudel S, Pokharel GB, Joshi BR, Pant DK. Evaluation of image quality in chest radiographs. J Inst Med Nepal. 2013;35(1):50–52. doi:10.59779/jiomnepal.590
25. Liaqat R, Majeed AI, Malik MN, Shafi A, Shah SZ, Liaqat B. Confronting our mistakes: a comprehensive evaluation of radiographic errors in digital chest radiography among adult population in a public sector hospital. Ann PIMS-Shaheed Zulfiqar Ali Bhutto Med Univ. 2021;17(2):129–133. doi:10.48036/apims.v17i2.440
26. Suwal S, Koirala S, Chataut D. Evaluation of the Diagnostic Quality of Chest Radiographs. Nepal J Radiol. 2022;12(1):13–17. doi:10.3126/njr.v12i1.42266
27. MINISTRY OF HEALTH M. MoH Yearly statistical Report 2022. Jordan. 2022. Available from: https://www.moh.gov.jo/ebv4.0/root_storage/ar/eb_list_page/%D8%AA%D9%82%D8%B1%D9%8A%D8%B1_2022-0.pdf.
28. Torres FS, Eifer DA, Tijmes FS, Nguyen ET, Hanneman K. Diagnostic performance of chest radiography measurements for the assessment of cardiac chamber enlargement. CMAJ. 2021;193(44):E1683–E1692. doi:10.1503/cmaj.210083
29. North Z. How to interpret chest radiographs (X-rays): a systematic approach. Nursing Times.
30. Lloyd-Jones G. Chest X-ray Anatomy. 2024. Available from: https://www.radiologymasterclass.co.uk/tutorials/chest/chest_home_anatomy/chest_anatomy_page6.
31. Emerson E, Fortune N, Llewellyn G, Stancliffe R. Loneliness, social support, social isolation and wellbeing among working age adults with and without disability: cross-sectional study. Disabil Health J. 2021;14(1):100965. doi:10.1016/j.dhjo.2020.100965
32. Alukić E, Homar K, Pavić M, Žibert J, Mekiš N. The impact of subjective image quality evaluation in mammography. Radiography. 2023;29(3):526–532. doi:10.1016/j.radi.2023.02.025
33. Abubakar U, Ibrahim A, Nwodo VK, et al. Assessment of the quality of postero-anterior chest radiographs seen in a north-west Nigerian tertiary hospital. J Adv Med Pharm Sci. 2019; 1–7. doi:10.9734/jamps/2019/v21i130120
34. Klein JS, Rosado-de-Christenson ML. A Systematic Approach to Chest Radiographic Analysis. In: Hodler J, Kubik-Huch RA, von Schulthess GK, editors. Diseases of the Chest, Breast, Heart and Vessels 2019-2022: Diagnostic and Interventional Imaging. IDKD Springer Series. Springer; 2019. Available from: http://www.ncbi.nlm.nih.gov/books/NBK553874/.
35. Desai S, Padley S. Respiratory Tract. In: Aids to Radiological Differential Diagnosis.In: Davies SG, BChir. Saunders; 2009.
36. Cain N. Chest X-Ray and Chest CT. In: Amalou H, Suh RD, Wood BJ editors. The Radiology Survival Kit: What You Need to Know for USMLE and the Clinics. Springer International Publishing; 2021:35–93. doi:10.1007/978-3-030-84365-6_4.
37. Corne J, Au-Yong I. Chest X-ray made easy E-book: chest X-ray made easy E-book. Elsevier Health Sci. 2022.
38. Bell DJ. Clothing artifact. Radiopaedia. doi:10.53347/rID-69009
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




