Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 20
Relationship Between COPD Progression and Frailty Progression: A Five-year Observation in Real Clinical Practice
Authors Nishimura K , Kusunose M , Shibayama A, Nakayasu K
Received 15 December 2024
Accepted for publication 5 June 2025
Published 14 June 2025 Volume 2025:20 Pages 1955—1964
DOI https://doi.org/10.2147/COPD.S512326
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Koichi Nishimura,1,2 Masaaki Kusunose,3 Ayumi Shibayama,4 Kazuhito Nakayasu5
1National Center for Geriatrics and Gerontology, Obu, Aichi, Japan; 2Clinic Nishimura, Ayabe, Kyoto, Japan; 3Department of Respiratory Medicine, National Center for Geriatrics and Gerontology, Obu, Aichi, Japan; 4Department of Nursing, National Center for Geriatrics and Gerontology, Obu, Aichi, Japan; 5Data Research Section, Kondo Inc., Osaka, Japan
Correspondence: Koichi Nishimura, Clinic Nishimura, 4-3. Kohigashi, Kuri-cho, Ayabe, 623-0222, Japan, Tel +81-773-47-0321, Fax +81-773-47-0201, Email [email protected]
Purpose: Although a cross-sectional association between frailty and chronic obstructive pulmonary disease (COPD) has been established, the longitudinal relationship between the progression of both frailty and COPD remains unclear.
Materials and Methods: This longitudinal study followed 87 COPD patients over five years, with evaluations conducted every six months. Participants underwent pulmonary function tests and completed the Kihon Checklist, a tool widely used in Japan to assess frailty. Kihon Checklist scores range from 0 (no frailty) to 25 (severe frailty), categorizing participants as robust (0– 3), pre-frail (4– 7), or frail (8– 25). Annual changes were analyzed using linear mixed models.
Results: A significant association was observed between time and worsening frailty classification, with patients transitioning from robust to pre-frail or from pre-frail to frail (odds ratio: 1.224, p = 0.004). However, the GOLD stages (GOLD 1 to GOLD 4) did not exhibit significant progression over five years. The cohort demonstrated significant declines in forced expiratory volume in one second (FEV1) and increases in Kihon Checklist total scores. FEV1 decreased by an estimated mean of 28.6 mL per year (95% CI: 18.9– 38.4, p < 0.001), while the Kihon Checklist total score increased by 0.30 annually (95% CI: 0.09– 0.51, p = 0.006). Estimated FEV1 declined significantly from baseline after two years in the baseline frail group (p < 0.01), after 3.5 years in the pre-frail group (p < 0.01), and after four years in the robust group (p < 0.05). Although the GOLD 3+4 group showed a significant increase in Kihon Checklist total scores after 3.5 years (p < 0.05), no significant change was observed in the GOLD 1 and GOLD 2 groups.
Conclusion: COPD patients with frailty show a more rapid decline in FEV1, indicating accelerated COPD progression. These findings suggest frailty is static and only COPD is progressing.
Keywords: disease progression, Kihon Checklist, linear mixed models
Introduction
Lung function progressively declines with age, leading to a gradual reduction in forced expiratory volume in one second (FEV1) and the FEV1/forced vital capacity (FVC) ratio.1,2 The changes observed in the lungs of aging individuals mirror those seen in patients with chronic obstructive pulmonary disease (COPD), as many mechanisms associated with aging are also present in COPD. COPD is recognized as a model disease of aging, with some researchers supporting the hypothesis that it represents a state of accelerated aging.3,4
Frailty, characterized by age-related declines in physical and psychological function, cognitive ability, and social interaction, increases vulnerability in both the body and mind. It is closely associated with the concept of aging and may even be considered synonymous with the aging process itself. Studies have reported a high prevalence of frailty among patients with COPD.5–9 Comparisons between COPD patients with and without frailty have demonstrated that those with frailty experience more severe dyspnea, suffer greater symptom burden, have poorer quality of life, face a higher risk of acute exacerbations,10–14 and exhibit increased mortality rates.10–13,15–18
There have also been several longitudinal studies published on the progression of frailty and the progression of low lung function and chronic respiratory disorders.19–24 However, most studies have analyzed general population samples or epidemiological research data similar to this, and it must be said that the results of studies analyzing the relationship between the progression of disease and the progression of frailty in subjects with a diagnosis of COPD are extremely limited. Lee et al reported that COPD was associated with a faster transition from robust to pre-frail or frail status in initially robust women.21 He et al found that, when compared with subjects with normal spirometry findings, patients with COPD and preserved ratio impaired spirometry (PRISm) findings showed accelerated progression of the frailty index (FI), which is a widely used multidimensional assessment of frailty that incorporates health deficits from multiple organs and systems.20 Cheng et al showed that frailty was associated with increased risk of COPD and that COPD was identified as a susceptibility factor for frailty, affirming a reciprocal causal relationship between frailty and COPD, using bidirectional two-sample Mendelian randomization analysis.19
COPD, characterized by airflow limitation, is widely recognized for its progressive nature, with FEV1 declining annually as the disease advances.25 Similarly, the total score on the Kihon Checklist, a tool widely used in Japan to assess frailty,7,17,26–29 is expected to increase with age. However, how frailty and the Kihon Checklist total score progress in individual cases remains largely unknown. Just as the annual decrease in FEV1 is utilized to assess COPD progression, an increase in the Kihon Checklist total score over time may lead to the development of frailty. The Kihon Checklist has been used in a cohort study of COPD patients conducted at our facility since 2015, with responses collected from patients every six months. We reanalyzed the data from this cohort study to compare the progression of frailty and COPD. The aim of this study is to describe the longitudinal changes in lung function and frailty in patients with COPD, and to investigate the possible association between baseline frailty and lung function decline.
Materials and Methods
Study Design and Patient Enrollment
Since 2013, the Outpatient Respiratory Medicine Clinic at the National Center for Geriatrics and Gerontology (NCGG) has conducted a cohort study on subjects with COPD.7,14,17 Participants meeting the inclusion criteria and providing consent were evaluated every six months, which included pulmonary function tests. In 2015, the Kihon Checklist was added to assess frailty. For this analysis, the baseline was defined as the first administration of the Kihon Checklist, with changes in the total score tracked over five years.
Eligible participants were clinically stable COPD patients aged 50 years or older, with a smoking history of more than 10 pack-years and a post-bronchodilator FEV1/FVC ratio below 0.7. Patients were excluded if they had a self-reported history of asthma, abnormal chest radiographs, or active lung disease. Additional exclusion criteria included unresolved comorbidities or an acute exacerbation of COPD within three months prior to study enrollment. All patients had been receiving regular treatment at the clinic for at least six months prior to inclusion, ensuring that any observed changes could not be attributed to new medical interventions. The study adhered to the ethical standards of the Declaration of Helsinki and was approved by the NCGG Ethics Committee (No. 1138–3; updated July 2020). Written informed consent was obtained from all participants before inclusion.
Patient recruitment occurred between February 2015 and March 2018, with participants encouraged to complete 11 evaluations over five years. To ensure robust data analysis, only participants who completed at least three evaluations during the five-year period were included. The final assessment was completed in March 2023. When participants experienced an acute exacerbation within three months prior to a scheduled evaluation, assessments were delayed ensuring compliance with the exclusion criteria.
Study Assessment
During each visit, participants were instructed to refrain from using bronchodilators for at least 12 hours prior to testing. Spirometry was performed using a CHESTAC-8800 spirometer (Chest, Tokyo, Japan) following inhalation of a long-acting bronchodilator in dry powder form under physician supervision. Residual volume (RV) was measured using the closed-circuit helium dilution method, and diffusing capacity for carbon monoxide (DLCO) was assessed using the single-breath technique. All tests were conducted in accordance with the protocols of the American Thoracic Society and the European Respiratory Society.30 Predicted values for lung function parameters were calculated based on the guidelines of the Japanese Respiratory Society.31
The Kihon Checklist consists of 25 questions assessing daily living activities, physical abilities, nutritional status, oral health, cognitive function, and risk of depression.26,32,33 The total score ranges from 0 (no frailty) to 25 (severe frailty), with participants classified as robust (0–3), pre-frail (4–7), or frail (8–25) based on their score.27 Body mass index (BMI) was calculated using measurements obtained at the same time as the pulmonary function test, rather than self-reported data.
Statistical Analysis
Patient backgrounds were compared using the Kruskal–Wallis test or Fisher’s exact test. The relationship between time and changes in GOLD and frailty classifications was analyzed using a generalized linear mixed model (GLMM) with a cumulative logit link function for the ordinal response variable. Random effects accounted for subject-specific variability, while fixed effects included time (years). Annual changes in FEV1 and Kihon Checklist total scores for the entire cohort were estimated using a linear mixed model, with each metric as the dependent variable, time as a fixed effect, and subjects as a random effect. Covariate adjustments were not applied. Means and 95% confidence intervals (CIs) at each measurement point were estimated using a linear mixed model, with timepoint as a fixed effect and subjects as a random effect. The Type III test of fixed effects assessed whether the values of each metric remained constant over time. Pairwise comparisons were performed to identify differences from baseline values, applying the Bonferroni method to adjust for multiple comparisons. Summary statistics are presented as mean ± standard deviation or estimated mean with 95% CIs. All analyses were performed using SPSS Statistics, version 28.0 (IBM Corp)., with p-values below 0.05 considered statistically significant.
Results
Subject Characteristics
There were 87 participants, 80 of whom were male, with varying degrees of airflow limitation ranging from mild to very severe. The mean age of the participants was 75.3 years, and the average FEV1 was 1.79 L (71.7% predicted) at baseline (Table 1). Based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification, 29 patients (33.3%) were categorized as GOLD 1 (FEV1 ≥ 80% predicted), 44 (50.6%) as GOLD 2 (50% ≤ FEV1 < 80% predicted), 11 (12.6%) as GOLD 3 (30% ≤ FEV1 < 50% predicted), and 3 (3.4%) as GOLD 4 (FEV1 < 30% predicted). Due to the small number of patients in the GOLD 3 and 4 categories, these were combined into a single group of 14 patients for subsequent analyses.
 |
Table 1 Comparison of Patient Characteristics at Baseline Between Robust, Pre-Frail and Frail Groups Classified by the Kihon Checklist Total Score in 87 Subjects with COPD |
At baseline, frailty status was assessed using the Kihon Checklist total score, with 44 patients (50.6%) classified as robust, 25 (28.7%) as pre-frail, and 18 (20.7%) as frail (Table 1). A comparison of physiological measures among the robust, pre-frail, and frail groups revealed significant differences in FEV1 and DLco (p = 0.014 and p < 0.001, respectively; by Kruskal–Wallis test). Advanced frailty was associated with greater airflow limitation and reduced pulmonary diffusion capacity.
At the end of the five-year follow-up, 63 participants were still alive, 12 had died, and information was unavailable for 12 participants. Among the 87 participants, 12 completed all 11 biannual assessments over the study period, 23 completed 10 assessments (the most common number), and 10 completed 9 assessments. Conversely, 8 participants completed only 3 assessments, 4 completed 4 assessments, and 6 completed 5 assessments; all were included in the analysis.
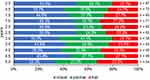
Five-year Progress of GOLD Stage and Frailty Status
The severity of GOLD airflow limitation, classified by FEV1, and frailty status, classified by the Kihon Checklist total score, were assessed at six-monthly intervals over a five-year period, as shown in Figures 1 and 2. However, variability in the number of cases analyzed at each visit limited the ability to draw definitive conclusions from the raw data alone.
An analysis was conducted to evaluate whether GOLD classification changed over time, using a generalized linear mixed model (GLMM) with GOLD 1, GOLD 2, and GOLD 3+4 as the outcome variables. The results revealed that neither the fixed effect nor the fixed coefficient was statistically significant. The odds ratio was estimated to be 1.013, indicating a minimal increase in the probability of advancing to a higher GOLD category with each passing year. However, this finding was not statistically significant (p = 0.900). Therefore, it cannot be concluded that GOLD classification progresses over time.
In contrast, analysis focusing on frailty categorization (robust, pre-frail, frail) showed a different trend. The odds ratio was estimated at 1.224, suggesting that the likelihood of transitioning to a higher frailty category increased by 1.224 times per year. A significant relationship was identified between the passage of time and a deterioration in frailty classification.
Five-year Progress of FEV1 and Kihon Checklist Total Score
The group as a whole exhibited a mean annual decline in FEV1 of 28.6 mL per year (95% CI: 18.9–38.4, p < 0.001) and a mean change in the Kihon Checklist total score of 0.30 per year (95% CI: 0.09–0.51, p = 0.006), as estimated by the linear mixed model. The fixed-effect Type III test yielded statistically significant results for both measures. The linear mixed model provided estimated means and 95% CIs for each measurement point at six-monthly intervals over a five-year period, revealing a progressive decline in FEV1 over time. Significant differences were identified at the two-year mark and subsequently, when compared with baseline values (Figure 3; see Table S1 in the electronic supplementary material for details). The Kihon Checklist total score remained relatively stable, plateauing over an extended period, with a significant increase observed only at the five-year mark (Figure 4; see Table S1 in the electronic supplementary material for details).
Comparisons of Five-year Progress Between Baseline Classifications
The differences in FEV1 between baseline and estimates derived from a linear mixed model at six-monthly intervals are shown for the robust, pre-frail, and frail groups (Figure 5; absolute FEV1 values are provided in Table S2 of the electronic supplementary material). When the interaction was assessed using a fixed-effect Type III test, a statistically significant difference was identified in the pattern of change among the three groups (p = 0.003). Estimated FEV1 values were significantly lower than baseline after two years in the frail group (p < 0.01), after 3.5 years in the pre-frail group (p < 0.01), and after four years in the robust group (p<0.05).
Figure 6 illustrates the differences in the Kihon Checklist total score between baseline and estimates calculated by a linear mixed model at six-monthly intervals for the GOLD 1, GOLD 2, and GOLD 3+4 groups (absolute Kihon Checklist total scores are provided in Table S3 of the electronic supplementary material). The Type III test for fixed effects was not significant (p = 0.293), indicating no significant differences in the pattern of change among the three groups. After 3.5 years, the GOLD 3+4 group demonstrated a significant increase in Kihon Checklist total scores compared to baseline, whereas the GOLD 1 and GOLD 2 groups showed no significant changes in scores over the five-year study period.
Discussion
While there have been reports on the cross-sectional association between COPD and frailty, this study represents, to the best of our knowledge, the first attempt to take a step further in understanding their relationship by comparing the progression of both COPD and frailty over time. Throughout the five-year study period, significant deterioration was observed in both FEV1, a determinant of GOLD severity, and the Kihon Checklist total score, a measure used to define frailty. Specifically, FEV1 declined by 28.6 mL per year, while the Kihon Checklist total score increased by 0.30 points annually across the entire cohort. Conversely, the three frailty categories, as defined by the Kihon Checklist total score—robust, pre-frail, and frail—exhibited progression over the five-year period. This indicates an annual probability of 1.224 for transitioning to a higher frailty category, such as from robust to pre-frail or from pre-frail to frail. However, the GOLD categories (GOLD 1, GOLD 2, and GOLD 3+4), defined by FEV1, did not exhibit similar progression during the same period. The lack of apparent migration between GOLD categories over five years suggests that this timeframe may be insufficient to observe changes within these groupings. As such, FEV1 and the Kihon Checklist total score were used as continuous measures to further explore the relationship between COPD progression and frailty.
The most significant finding from this study is that, in comparison with robust COPD patients, frail COPD patients experienced a more rapid decline in FEV1, indicating faster COPD progression. Conversely, for individuals who had already developed COPD, the progression of the Kihon Checklist total score did not appear to be so influenced by the stage of COPD. The cross-sectional association between frailty and COPD, as demonstrated in numerous previous studies, suggests that frailty may be one of the possible contributors to COPD progression.
In this study, the authors assessed frailty by evaluating the Kihon Checklist total score, a method currently employed only in Japan. In a longitudinal study focusing on community-dwelling older adults, Ohashi et al reported that the median Kihon Checklist total score increased from 2 in 2011 to 3 in 2016.28 Moreover, Imai et al observed a significant increase in the Kihon Checklist total score, rising from 2 in 2016 to 3 in 2022.29 They also reported increases of 1 point in the Kihon Checklist total score over five years and six years, respectively.28,29 Our research on COPD patients revealed that the mean Kihon Checklist total score rose from 4.9 to 6.7 over five years, and estimated an average annual increase of 0.30 points, suggesting a slightly faster pace of deterioration. Given that the participants were COPD patients, it is not surprising that their scores were comparatively higher. This discrepancy of the deterioration speed may be attributed to the higher baseline scores in our cohort.
One study on COPD patients, which monitored 119 individuals over two years, found that 17.6% showed an improvement in frailty status, 11.7% experienced a decline, and 70.5% remained stable.34 Two studies conducted in Japanese community-dwelling older adults that examined changes in the Kihon Checklist total score also reported transitions between frailty states, suggesting that the rate of change is generally similar.28,29 In the present study, the estimated probability of transitioning to a higher frailty category increasing by 1.224 times annually aligns closely with existing findings in the literature. Furthermore, when comparing studies of community-dwelling older adults and COPD patients, it is unlikely that any disparities were found in the rate of frailty progression. These facts may be findings consistent with the results observed in this study, which showed no differences in the rate of deterioration of Kihon Checklist total score by GOLD stage.
Historically, a decline in FEV1 has been regarded as a hallmark of COPD progression, and COPD has been considered a progressive disease.25,35 Smoking cessation has been demonstrated to lessen FEV1 decline and slow the progression of COPD,36–38 even though numerous clinical trials have used the rate of FEV1 decline as a primary or secondary endpoint.37,39,40 However, research involving large patient cohorts has shown significant variability in the annual rate of FEV1 decline among individuals.41 In this study, the frequency distribution of cases with respect to the annual rate of FEV1 decline also exhibited wide variability, consistent with findings from previous reports. Conversely, minimal attention has been given to transitions between severity classification groups, such as GOLD 1 to GOLD 4, which are based on FEV1.
All clinical indicators should fulfil three essential roles: the ability to distinguish subjects (discriminative property), the ability to detect changes (evaluative property), and the ability to predict future outcomes (predictive property). In terms of evaluative property, it is crucial to gather insights from two perspectives: evaluating improvements through medical interventions and assessing the progression of deterioration over time in progressive diseases. The discriminative and predictive properties of frailty have been widely investigated,5–18 alongside potential improvements achieved through rehabilitation.34,42–45 Furthermore, substantial evidence has been accumulated regarding the progression of frailty through cohort studies spanning several years.28,29,46–48 Most of these studies are epidemiological investigations involving large cohorts of elderly individuals in the general population. This study, however, focused on COPD patients, a population known for high dropout rates and substantial missing data in research, requiring careful attention during data analysis.49 To tackle these challenges, the analysis predominantly employed linear mixed models, enabling the filling in of missing data and facilitating strong statistical analysis.
One of the main limitations of this study is its observational, single-center design and the relatively small sample size, which prevented robust multivariate analyses from being conducted. This limitation restricted our ability to statistically adjust for baseline values of lung function and frailty, thus introducing the potential for regression to the mean, a well-known phenomenon that may affect longitudinal data interpretation. Additionally, the high dropout rate and missing data inherent in real-world clinical practice further limited statistical power. Therefore, the findings should be interpreted cautiously, and future studies with larger sample sizes and comprehensive multivariate approaches are necessary to confirm our observations. Despite these limitations, our study provides valuable insights reflecting the reality of clinical COPD management. Another major problem is that this study used the Kihon Checklist to assess frailty. This tool is only used in Japan, so international comparisons are difficult. In fact, one longitudinal epidemiological study on the progression of COPD and frailty was conducted using FI.20 Finally, this was an observational study, and therefore, causal relationships cannot be inferred; only associations can be discussed.
Conclusion
Three main conclusions can be drawn from our findings. First, in individuals with COPD, the probability of transitioning to a higher frailty category, such as from robust to pre-frail or from pre-frail to frail, was estimated to increase by 1.224 times annually. However, the GOLD categories, including GOLD 1 to GOLD 4, did not exhibit significant progression over the five-year study period. Second, the cohort as a whole demonstrated a significant annual change in FEV1 of −28.6 mL per year and an increase in the Kihon Checklist total score of 0.30 per year, as estimated by the linear mixed model. Third, the findings suggest that frailty progression may be one of the factors involved in the progression of COPD, which could be related to the frequent association observed between frailty and COPD.
Acknowledgments
This study was partly supported by the Research Funding for Longevity Sciences (22-7) from the National Center for Geriatrics and Gerontology, Japan.
Author Contributions
The authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors, take responsibility for the integrity of the work as a whole, contributed to the writing and reviewing of the manuscript, and have given final approval for the version to be published. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Janssens JP. Aging of the respiratory system: impact on pulmonary function tests and adaptation to exertion. Clin Chest Med. 2005;26(3):469–484, vi–vii. doi:10.1016/j.ccm.2005.05.004
2. Vaz Fragoso CA, Gill TM. Respiratory impairment and the aging lung: a novel paradigm for assessing pulmonary function. J Gerontol a Biol Sci Med Sci. 2012;67(3):264–275. doi:10.1093/gerona/glr198
3. MacNee W. Is chronic obstructive pulmonary disease an accelerated aging disease? Ann Am Thorac Soc. 2016;13(Supplement_5):S429–S437. doi:10.1513/AnnalsATS.201602-124AW
4. Ito K, Barnes PJ. COPD as a disease of accelerated lung aging. Chest. 2009;135(1):173–180. doi:10.1378/chest.08-1419
5. Antoniu SA, Boiculese LV, Prunoiu V. Frailty, a dimension of impaired functional status in advanced COPD: utility and clinical applicability. Medicina. 2021;57(5):474. doi:10.3390/medicina57050474
6. Guan C, Niu H. Frailty assessment in older adults with chronic obstructive respiratory diseases. Clin Interv Aging. 2018;13:1513–1524. doi:10.2147/CIA.S173239
7. Kusunose M, Oga T, Nakamura S, Hasegawa Y, Nishimura K. Frailty and patient-reported outcomes in subjects with chronic obstructive pulmonary disease: are they independent entities? BMJ Open Respir Res. 2017;4(1):e000196. doi:10.1136/bmjresp-2017-000196
8. Wang L, Zhang X, Liu X. Prevalence and clinical impact of frailty in COPD: a systematic review and meta-analysis. BMC Pulm Med. 2023;23(1):164. doi:10.1186/s12890-023-02454-z
9. Yan LC, Lu HY, Wang XY, et al. Prevalence and risk factors of frailty in patients with chronic obstructive pulmonary disease: systematic review and meta-analysis. Eur Geriatr Med. 2023;14(4):789–802. doi:10.1007/s41999-023-00800-2
10. Hanlon P, Lewsey J, Quint JK, et al. Frailty in COPD: an analysis of prevalence and clinical impact using UK Biobank. BMJ Open Respir Res. 2022;9(1). doi:10.1136/bmjresp-2022-001314
11. Kennedy CC, Novotny PJ, LeBrasseur NK, Wise RA, Sciurba FC, Benzo RP. Frailty and clinical outcomes in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2019;16(2):217–224. doi:10.1513/AnnalsATS.201803-175OC
12. Luo J, Zhang D, Tang W, Dou LY, Sun Y. Impact of frailty on the risk of exacerbations and all-cause mortality in elderly patients with stable chronic obstructive pulmonary disease. Clin Interv Aging. 2021;16:593–601. doi:10.2147/CIA.S303852
13. Zhang D, Tang W, Dou LY, Luo J, Sun Y. Four different frailty models predict health outcomes in older patients with stable chronic obstructive pulmonary disease. BMC Geriatr. 2022;22(1):57. doi:10.1186/s12877-022-02750-z
14. Nishimura K, Kusunose M, Sanda R, Shibayama A, Nakayasu K. Frailty and exacerbation of chronic obstructive pulmonary disease: is there any association? Int J Chron Obstruct Pulmon Dis. 2024;19:1131–1139. doi:10.2147/COPD.S455316
15. Brighton LJ, Nolan CM, Barker RE, et al. Frailty and mortality risk in COPD: a cohort study comparing the fried frailty phenotype and short physical performance battery. Int J Chron Obstruct Pulmon Dis. 2023;18:57–67. doi:10.2147/COPD.S375142
16. Galizia G, Cacciatore F, Testa G, et al. Role of clinical frailty on long-term mortality of elderly subjects with and without chronic obstructive pulmonary disease. Aging Clin Exp Res. 2011;23(2):118–125. doi:10.1007/BF03351076
17. Nishimura K, Kusunose M, Shibayama A, Nakayasu K. Is frailty a mortality predictor in subjects with chronic obstructive pulmonary disease? Int J Chron Obstruct Pulmon Dis. 2023;Volume 18:2955–2960. doi:10.2147/COPD.S439966
18. Scarlata S, Finamore P, Laudisio A, et al. Association between frailty index, lung function, and major clinical determinants in chronic obstructive pulmonary disease. Aging Clin Exp Res. 2021;33(8):2165–2173. doi:10.1007/s40520-021-01878-z
19. Cheng Z, Wu J, Xu C, Yan X. Exploring the causal relationship between frailty and chronic obstructive pulmonary disease: insights from bidirectional Mendelian randomization and mediation analysis. Int J Chron Obstruct Pulmon Dis. 2025;20:193–205. doi:10.2147/COPD.S501635
20. He D, Yan M, Zhou Y, et al. Preserved ratio impaired spirometry and COPD accelerate frailty progression: evidence from a prospective cohort study. Chest. 2024;165(3):573–582. doi:10.1016/j.chest.2023.07.020
21. Lee JS, Auyeung TW, Leung J, Kwok T, Woo J. Transitions in frailty states among community-living older adults and their associated factors. J Am Med Dir Assoc. 2014;15(4):281–286. doi:10.1016/j.jamda.2013.12.002
22. Marengoni A, Vetrano DL, Manes-Gravina E, Bernabei R, Onder G, Palmer K. The relationship between COPD and frailty: a systematic review and meta-analysis of observational studies. Chest. 2018;154(1):21–40. doi:10.1016/j.chest.2018.02.014
23. Wijnant SRA, Benz E, Luik AI, et al. Frailty transitions in older persons with lung function impairment: a population-based study. J Gerontol a Biol Sci Med Sci. 2023;78(2):349–356. doi:10.1093/gerona/glac202
24. Guo D, Huang K, Guan X, et al. Association between chronic respiratory diseases and frailty in Chinese elderly: a population-based longitudinal study. BMJ Open Respir Res. 2025;12(1). doi:10.1136/bmjresp-2023-002171
25. Burrows B, Bloom JW, Traver GA, Cline MG. The course and prognosis of different forms of chronic airways obstruction in a sample from the general population. N Engl J Med. 1987;317(21):1309–1314. doi:10.1056/NEJM198711193172103
26. Arai H, Satake S. English translation of the Kihon Checklist. Geriatr Gerontol Int. 2015;15(4):518–519. doi:10.1111/ggi.12397
27. Satake S, Senda K, Hong YJ, et al. Validity of the Kihon Checklist for assessing frailty status. Geriatr Gerontol Int. 2016;16(6):709–715. doi:10.1111/ggi.12543
28. Ohashi M, Yoda T, Imai N, et al. Five-year longitudinal study of frailty prevalence and course assessed using the Kihon Checklist among community-dwelling older adults in Japan. Sci Rep. 2021;11(1):12399. doi:10.1038/s41598-021-91979-6
29. Imai N, Yoda T, Horigome Y, et al. Determining factors that maintain physical function or increase frailty using the Kihon checklist among community-dwelling older adults: a six-year longitudinal study in Agano, Japan. BMC Geriatr. 2023;23(1):336. doi:10.1186/s12877-023-04055-1
30. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
31. Sasaki H, Nakamura M, Kida K, Kambe M, Takahashi K, Fujimura M. Reference values for spirogram and blood gas analysis in Japanese adults. J Jpn Respir Soc. 2001;39(5):S1–S17.
32. Sewo Sampaio PY, Sampaio RA, Yamada M, Arai H. Systematic review of the Kihon Checklist: is it a reliable assessment of frailty? Geriatr Gerontol Int. 2016;16(8):893–902. doi:10.1111/ggi.12833
33. Japanese Association on Sarcopenia and Fraility. Kihon Checklist. Available from: https://jssf.umin.jp/pdf/Kihon_Checklist_2022.pdf.
34. Bernabeu-Mora R, Oliveira-Sousa SL, Sanchez-Martinez MP, Garcia-Vidal JA, Gacto-Sanchez M, Medina-Mirapeix F. Frailty transitions and associated clinical outcomes in patients with stable COPD: a longitudinal study. PLoS One. 2020;15(4):e0230116. doi:10.1371/journal.pone.0230116
35. Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi:10.1164/rccm.201204-0596PP
36. Anthonisen NR, Connett JE, Enright PL, Manfreda J, Lung Health Study Research G. Hospitalizations and mortality in the lung health study. Am J Respir Crit Care Med. 2002;166(3):333–339. doi:10.1164/rccm.2110093
37. Anthonisen NR, Connett JE, Kiley JP, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The lung health study. JAMA. 1994;272(19):1497–1505. doi:10.1001/jama.1994.03520190043033
38. Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of lung health study participants after 11 years. Am J Respir Crit Care Med. 2002;166(5):675–679. doi:10.1164/rccm.2112096
39. Burge PS, Calverley PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. BMJ. 2000;320(7245):1297–1303. doi:10.1136/bmj.320.7245.1297
40. Calverley PM, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356(8):775–789. doi:10.1056/NEJMoa063070
41. Vestbo J, Edwards LD, Scanlon PD, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011;365(13):1184–1192. doi:10.1056/NEJMoa1105482
42. Finamore P, Scarlata S, Delussu AS, Traballesi M, Incalzi RA, Laudisio A. Frailty impact during and after pulmonary rehabilitation. COPD. 2021;18(5):518–524. doi:10.1080/15412555.2021.1967915
43. Maddocks M, Brighton LJ, Alison JA, et al. Rehabilitation for people with respiratory disease and frailty: an official American thoracic society workshop report. Ann Am Thorac Soc. 2023;20(6):767–780. doi:10.1513/AnnalsATS.202302-129ST
44. Maddocks M, Kon SS, Canavan JL, et al. Physical frailty and pulmonary rehabilitation in COPD: a prospective cohort study. Thorax. 2016;71(11):988–995. doi:10.1136/thoraxjnl-2016-208460
45. Wang Z, Hu X, Dai Q. Is it possible to reverse frailty in patients with chronic obstructive pulmonary disease? Clinics. 2020;75:e1778. doi:10.6061/clinics/2020/e1778
46. Gale CR, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: the English longitudinal study of ageing. Age Ageing. 2018;47(3):392–397. doi:10.1093/ageing/afx188
47. Tange C, Nishita Y, Tomida M, et al. Natural history trajectories of frailty in community-dwelling older Japanese adults. J Gerontol a Biol Sci Med Sci. 2022;77(10):2059–2067. doi:10.1093/gerona/glac130
48. Kaskirbayeva D, West R, Jaafari H, et al. Progression of frailty as measured by a cumulative deficit index: a systematic review. Ageing Res Rev. 2023;84:101789. doi:10.1016/j.arr.2022.101789
49. Calverley PM, Spencer S, Willits L, Burge PS, Jones PW, Group IS. Withdrawal from treatment as an outcome in the ISOLDE study of COPD. Chest. 2003;124(4):1350–1356. doi:10.1378/chest.124.4.1350
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.