Back to Journals » International Journal of Nanomedicine » Volume 20
Research and Application Prospect of Nanomedicine in Kidney Disease: A Bibliometric Analysis From 2003 to 2024
Authors Meng Y , Sui L, Xu T , Zhao H, Yuan Q, Sun L
Received 3 December 2024
Accepted for publication 21 February 2025
Published 12 March 2025 Volume 2025:20 Pages 3007—3030
DOI https://doi.org/10.2147/IJN.S510016
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Eng San Thian
Yilin Meng,1,* Lu Sui,1,* Tianhua Xu,1,* Hainan Zhao,2 Quan Yuan,3 Li Sun1
1Department of Nephrology, The First Hospital of China Medical University, Shenyang 110001, People’s Republic of China; 2Department of Nephrology, The First Affiliated Hospital of Jinzhou Medical University, Jinzhou 121001, People’s Republic of China; 3Department of Orthopedics, Shengjing Hospital of China Medical University, Shenyang, 110004, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Sun, The First Hospital of China Medical University, Nanjing North Street 155#, Heping District, Shenyang, Liaoning, 110001, People’s Republic of China, Tel +86-13940593292, Email [email protected] Quan Yuan, Shengjing Hospital of China Medical University, Sanhao Street 36#, Heping District, Shenyang, Liaoning, 110004, People’s Republic of China, Email [email protected]
Abstract: Kidney disease is a major public health concern that has a significant effect on a patient’s life span and quality of life. However, effective treatment for most kidney diseases is lacking. Nanotechnology mainly explores the design, characterization, production, and applications of objects in the nanoscale range and has been widely used in the medical field. To date, there has been an increasing amount of research on the application of nanotechnology in kidney disease. However, systematic bibliometric studies remain rare. In this review, data collected from the Web of Science Core Collection database until December 31, 2024, were subjected to a bibliometric analysis. A total of 1179 articles and reviews were included. The publication trends, countries, institutions, authors, co-authorship, co-citations, journals, keywords, and references pertaining to this topic were examined. The results showed that nanotechnology research in kidney disease is increasing. The leading country, organization, and author were China, Sichuan University, and Professor Peng Huang, respectively. ACS APPLIED MATERIALS & INTERFACES was the top journal among the 464 journals in which articles on nanotechnology in kidney disease were published. KIDNEY INTERNATIONAL was the most cited journal in the field. The most significant increases were shown for “acute kidney disease”, “drug delivery”, “oxidative stress”, “diabetic nephropathy”, and “chronic kidney disease”, indicating the current research hotspots. Furthermore, the development prospects and challenges of nanotechnology in kidney disease were discussed in this review. How to achieve precise drug delivery to render kidney-targeting therapy a reality may be problematic in future studies.
Keywords: nanomedicine, kidney disease, bibliometric analysis, drug delivery, diagnosis, therapy
Graphical Abstract:

Introduction
The kidney is an organ that excretes metabolite and keeps the balance of water and electrolyte. It is composed of nephrons, periglomerular organs, interstitium, blood vessels, and nerves. Nephrons, including glomeruli, renal tubules, and renal sacs, are the most primary structural and functional units of the kidney and responsible for filtration, reabsorption, and secretion to ensure body homeostasis. In kidney disease, the above structures and functions are damaged, resulting in internal environment disorders, proteinuria, hematuria, oliguria, edema, hypertension, and other symptoms. Eventually, kidney function is impaired, which can affect other organs and, in severe cases, lead to death.
 |
Figure 1 The process of publications’ filtration. |
Kidney disease has been a significant public health concern globally, affecting roughly 10% of the global population, and its prevalence is increasing yearly. In 2019, 1.4 million people died from chronic kidney disease (CKD) and the number of deaths has increased by 30% in the past 10 years.1 Approximately 10–15% of patients in hospitals suffer from acute kidney injury (AKI) and half are in intensive care units.2 It has been reported that the mortality rate of AKI was greater than CKD and surpassed the combined rates of diabetes, heart failure, prostate cancer, and breast cancer.3 In addition, patients’ quality of life is seriously affected by kidney disease. In patients 50–74 years of age, CKD was the eighth leading cause of disability-adjusted life years (DALYs) worldwide.4 Patients with end-stage renal disease (ESRD) usually depend on dialysis, which both decreases their quality of life and imposes a significant financial burden on their families and countries.5 In particular, kidney disease increases the mortality risk of other diseases such as cardiovascular disease.6 However, there are few effective treatments for kidney disease, and many drugs have poor therapeutic effects due to low bioavailability, short residence time in the kidney, and significant adverse effects. Therefore, developing kidney targeting drugs and improving their bioavailability are of great importance for delaying the progression of kidney disease.
Nanotechnology, which was proposed in 1959, is the engineering and manufacturing of materials at the atomic and molecular scales.7 In its strictest definition from the National Nanotechnology Initiative, nanotechnology refers to structures roughly in the 1–100 nm size regime in at least one dimension. Despite this size restriction, nanotechnology commonly refers to structures that are up to several hundred nanometers in size and that are developed by top-down or bottom-up engineering of individual components.8 The study of nanotechnology is based on various subjects such as macrophysics, computer technology, quantum mechanics, and biology. The size of many biological molecules is within the nano or subnano range, thus, nanotechnology is widely applied in biology. The term “nanomedicine” appeared around 2000 and pertains to the use of nanotechnology in maintaining health and improving diseases.9 Nano-Drug Delivery System (NDDS) refers to a novel approach in the pharmaceutical field, harnessing the potential of nanotechnology for drug delivery. According to the carrier materials and structures used, NDDS are divided into different categories, including nanosuspensions, nanoliposomes, micelles, microemulsions/self-microemulsions, nanocapsules, and solid lipid nanoparticles.10 These NDDS can enhance drug stability, increase bioavailability and half-life, improve drug distribution, and reduce adverse reactions by using nanotechnology to deliver drugs.11 For example, pegylated liposomal doxorubicin (Doxil), the first nanodrug, was approved in 1995 by the United States Food and Drug Administration (FDA).12 Doxil showed lower heart cardiotoxicity and a longer half-life than doxorubicin alone.13 In the past decade, the funding for nanomedicine has increased, and nanomedicine has shown significant potential in treating diseases, especially cancer.14
Currently, most kidney diseases cannot be cured completely, and some drugs used clinically, especially immunosuppressants, have numerous adverse reactions. For example, glucocorticoids and immunosuppressants are commonly used to treat kidney disease. However, long-term use of glucocorticoids can lead to obesity, necrosis of the femoral head, and even fatal infections. Some immunosuppressants, such as cyclophosphamide, inhibit the hematopoietic system or lead to impaired liver function. These severely limit the clinical application of drugs and bring great trouble to clinicians and patients. Nanotechnology may be effective in solving these problems. Nanoparticles (NPs) are the molecules and atoms engineered by nanotechnology with specific properties that can change drug pharmacokinetics and pharmacodynamics so as to target certain organs or even certain cells.15,16 Several NPs have shown a potential curative effect in kidney disease mouse models.14 For example, researchers created myofibroblast-targeting NPs with the antineoplastic agent Sorafenib, which can reduce renal fibrosis in mouse models.17 For hereditary kidney disease, DNA or RNA may be delivered to target cells by nanogene carriers and provide a therapeutic benefit.18–20 Ferumoxytol, a superparamagnetic iron oxide nanoparticle coated with a semi-synthetic carbohydrate shell, had a better effect on renal anemia than oral iron in phase III trials, and has been approved by the FDA.21,22 Nanotechnology can also be used to improve dialysis membranes and adsorbents. It can reduce the size of devices and aid in monitoring blood ion concentration using nanosensors.23,24 In addition, nanotechnology can aid in the early diagnosis of kidney disease, which is important for improving prognosis. Researchers found microRNA(miR)-21 highly expressed in early-onset AKI.25 A new type of nanoantenna has been synthesized that can detect miR-21 and diagnose AKI earlier in mice.26
As a new interdisciplinary subject, nanotechnology has been paid more and more attention to its application in kidney disease. Although there have been numerous reviews on the study of nanomedicine, many of them lack objective visualized data support and mainly rely on researchers’ subjective understanding of the field. Bibliometrics, created by James McKeen Cattell, is a method to count the information of publications and analyze the current state and trend of research.27,28 Professor Chaomei Chen transformed the statistical results into various visualization maps to simplify comprehension.29 Bibliometrics can objectively show the development status, research hotspots, and future prospects of a research field through statistical analysis of various characteristics of publications. At present, systematic bibliometric analysis studies on nanotechnology in kidney disease are rare. In this paper, bibliometrics analysis was used to visualize the landscape of publications, countries, organizations, authors, journals, keywords, and references on the topic of nanotechnology in kidney disease to display the research progress of nanotechnology in the diagnosis and treatment of kidney disease over the past 21 years. In addition, the existing problems and potential future research directions were proposed, serving as a valuable resource for scholars new to the field.
Materials and Methods
Data Collection
First, the Web of Science Core Collection (WoSCC) database, which is widely used for bibliometric analysis was searched. The database is comprised of several indices including the Science Citation Index-Expanded (SCIE), Social Sciences Citation Index (SSCI), and Arts & Humanities Citation Index (A&HCI).30–32 The search terms were
TI=x OR AB=x OR AK=x (‘TI’, ‘AB’, and ‘AK’ represent the field tag of ‘title’, ‘abstract’, and ‘author keywords’, respectively), x=((nanomedicine OR nanoparticle* OR nanotube* OR ‘nano drug*’ OR nanomaterial* OR nanocomposite*) AND (‘Kidney disease*’ OR nephropath* OR ‘renal disease*’ OR nephrosis OR ‘renal insufficiency’ OR ‘renal dysfunction’ OR ‘kidney dysfunction’ OR ‘kidney insufficiency’ OR ‘renal failure’ OR ‘kidney failure’ OR uremia OR ‘kidney injury’ OR ‘renal injury’ OR ‘renal impairment’ OR ‘kidney impairment’ OR ‘CKD’ OR ‘end-stage renal disease’ OR ‘ESRD’ OR ‘end-stage kidney disease’ OR ‘ESKD’ OR ‘hemodialysis’ OR ‘peritoneal dialysis’ OR ‘renal replacement therapy’ OR ‘kidney transplant’ OR ‘AKI’ OR ‘nephrotic syndrome’ OR ‘glomerulonephritides’ OR ‘glomerulonephritis’ OR ‘nephritis’) NOT (cancer OR carcinoma OR tumor OR neopla*)).
In total, 1243 publications were found.
Data Filtration
The filtering shown in Figure 1 and the search were performed on the same day (January 8, 2025). Only peer-reviewed reviews and articles published in English before January 1, 2025, were included. Other types of publications or those not written in English or published after January 1, 2025, were excluded. The filtered publication information was then exported as Excel and Plain text files for later analysis using bibliometrics visual analysis software. Finally, the publications were checked for duplication using CiteSpace 6.3.1 Basic. A total of 1179 publications were ultimately included in this study (Supplementary Table 1). Two authors independently completed the work.
Data Analysis
Various bibliometric visualization software was used in the analysis. The VOSviewer 1.6.18 was used for co-authorship analysis of countries, authors, organizations, co-citation analysis of cited authors, and citation analysis of journals.33 R 4.3.2 with the R package bibliometrix was used for mapping three fields plot, author keywords evolution paths, and finding the core journals based on Bradford’s Law.34 Burst detection, cluster analysis, timeline view, co-occurrence of keywords, and co-cited analysis of references were performed with CiteSpace 6.3.1 Basic.29 Microsoft Excel 2016 was used for descriptive statistics and producing polynomial trend lines, tables, and figures.
Results
The Number of Publications and Citations
This review included 1179 publications on nanotechnology in kidney disease: 1022 articles and 157 reviews. The earliest paper was published in 2003. It explored the influence of different functional groups on latex nanoparticles’ surfaces on the protein adsorption from human serum, and the conclusion was useful for the design of hemodialysis devices.35 The number of publications increased overall from 2003 to 2024 (Figure 2A) and the annual growth rate was 29.42%. Nearly half of the publications were published in the past 3 years. The number of publications was fitted using a polynomial curve (y = 0.0413×3 - 0.5607×2 + 2.5506x + 1, R² = 0.9934) which predicted the future growing trend. These publications were cited a total of 26567 times (average 22.53) prior to our search. The number of citations increased yearly from 2003 to 2024.
Distribution
A total of 76 countries made contributions to this field. China was the largest contributor with 456 publications, followed by the United States (210), India (109), Egypt (56), and Iran (52). In the top 10 (Table 1), 6 countries were from Asia, 2 from Europe, 1 from Africa, and 1 from North America. The top 10 countries published 1085 publications in all, accounting for 92.02% of the total and the proportion is shown in Figure 2B. The United States led the field prior to 2016 and China led thereafter. In addition, China had the most citations (9327). The country with the highest average number of citations was Denmark (80.667). The collocation between countries is shown in Figure 2C. The node color represents the average publication year of all publications on the topic from the country, the node size represents the number of publications from the country, and the thickness of links represents the frequency of cooperation between countries. The United States had the highest total link strength (118) and collaborated closely with other countries, including China, India, Germany, and England.
All literature was from 1643 organizations. The Sichuan University from China contributed the most with 32 publications. All the top 10 organizations (Table 2) were from China. The publications from Zhejiang University were cited the most (1645). The National Institute of Biomedical Imaging and Bioengineering in the USA and Wuxi People’s Hospital in China tied for first place of the average citations because they co-published 1 paper that received 548 citations. Figure 3A shows the cooperation among organizations. Taif University from Saudi Arabia had the highest total link strength (57).
 |
Table 1 The Top 10 Countries by Number of Publications |
 |
Table 2 The Top 10 Organizations by Number of Publications |
Authors
In total, 6888 authors contributed to writing the articles. Only 22 authors produced more than 5 papers in the field (Table 3). Among these authors, 9 were from China. Professor Peng Huang had the most publications (10) and most citations (653). All authors were classified into 4 clusters by the VOSviewer and were distinguished by colors in the overlay visualization map (Figure 3B). The authors in the same cluster cooperated more, possibly because the authors in the same cluster were usually from the same organization (Supplementary Table 2). The relationship of leading countries, organizations, and authors is shown in Figure 3C.
A co-citation analysis of the cited authors was performed. Table 4 includes a list of the top 20 writers based on citation count. Compared with Table 3, there were 5 cited authors (Ryan M. Williams, Edward R. Smith, Dawei Jiang, Mengxiao Yu, and Dong-Yang Zhang) who wrote more than 5 publications. Rm Williams was the leading author in the references, and his papers were cited 145 times. The co-citation analysis results are shown in Figure 4A. The node size indicates the number of times the author has been cited, and the thickness of the line between authors indicates the number of times that both authors were cited in the same article. The co-citations between cited authors were very common.
 |
Table 3 Authors With Over 5 Publications |
 |
Table 4 The Top 20 Cited Authors by Citations |
Journals
The 1179 articles in the field were published in 464 journals. The journal in which most of the articles were published was the ACS APPLIED MATERIALS & INTERFACES, with an impact factor of 8.5. Among the top 10 journals (Table 5), chemistry and nanoscience & nanotechnology were the major areas of interest. Bradford’s Law is an important law in bibliometrics. According to the law, journals are divided into three zones: core, middle, and tail. The law is used to estimate the exponentially diminishing returns of searching for references in science journals. For example, when journals in a field are sorted by number of articles into the three zones, each with approximately one-third of all articles, then the number of journals in each zone will be proportional to 1:n:n2 (n > 1).36 Based on Bradford’s Law (Table 6), 34 journals were included in the core journals (Supplementary Table 3). As shown in Figure 4B, the articles in the CHEMICAL ENGINEERING JOURNAL were mainly published in recent years. The links in Figure 4B represent the citations between journals. Furthermore, KIDNEY INTERNATIONAL was the most cited journal in the field, which was cited 1605 times in total.
 |
Table 5 The Top 10 Journals by the Number of Publications |
 |
Table 6 According to Bradford’s Law, the Journals Were Divided Into Three Zones, and the Journals in Zone 1 Were the Core |
Keywords
The 1179 publications contained 5403 keywords in total, including 2924 Keywords Plus, which were the keywords from the analysis of the WoSCC database, and 2964 author keywords, which were keywords written by the authors. In the co-occurrence analysis of author keywords, 288 were included (selection criteria: g-index (k = 14), LRF = 3.0, L/N = 10, LBY = 5, e = 1.0). The top 20 are shown in Table 7 based on frequency. “Acute kidney injury” (124) occurred the most and “chronic kidney disease” had the highest centrality (0.27) which represented the extent of interaction between nodes. The higher the centrality of keywords is, the more important the keywords are in the topic. Additionally, both “acute kidney injury” and “oxidative stress” had centrality higher than 0.1. “Magnetic resonance imaging” had the highest sigma values of 1.42, which reflected the novelty. The 295 keywords were divided into numerous clusters using CiteSpace. The major 8 clusters are shown in Figure 5A. The time when the keywords first appeared is indicated by the node position on the horizontal axis, the color represents the time of occurrence, and the purple outline of nodes represents the centrality higher than 0.1. The keywords commonly used in the last few years were included in clusters #1, #2, #3, #4, and #7. In burst detection, only one keyword, “magnetic resonance imaging”, displayed burst (the red nodes in Figure 5A). It burst from 2008 to 2015 and was also the keywords with the highest sigma values. The evolution of author keywords from 2003 to 2024 is shown in Figure 5B. NP, diabetes nephropathy, and AKI were the persistent hotspots. In addition, the research on CKD, dialysis, and kidney transplantation has increased in recent years.
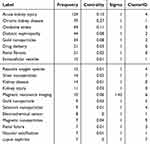 |
Table 7 The Top 20 Author Keywords by Frequency |
References
The co-citation analysis of references was conducted using CiteSpace and 293 references that met the selection criteria (g-index (k = 3), LRF = 3.0, L/N = 10, LBY = 5, e = 1.0) were included in the analysis. The references with the top 10 citations are listed in Table 8. Among the top 10 citations, 7 were original articles regarding loading certain medications on NPs that could alleviate AKI or renal fibrosis in mice. The 2 reviews by JA. Kellum and C. Ronco, respectively, both comprehensively reviewed the research on AKI.37,38 In the fifth paper, the safety of mesoscale NPs in mice was proven and was shown to accumulate more markedly in the kidney than in other organs, with a specific target to the proximal tubular epithelial cells.39 The reference titled “ROS-responsive nano-drug delivery system combining mitochondria-targeting ceria nanoparticles with atorvastatin for acute kidney injury” and “Selective Nanoparticle Targeting of the Renal Tubules” had the highest centrality (0.02).
 |
Table 8 The Top 10 References by Citations |
Figure 5C shows the three major clusters of references and the tendency over time. All of the top 10 references belonged to #1 and #4. The connections between various clusters were minimal. The burstness of 22 references was determined (Figure 5D). The main content of references that have burst until 2024 was as follows: some NPs, selenium-doped carbon quantum dots, and l-serine-modified chitosan with D-Arg-dimethylTyr-Lys-Phe-NH2 (SS-31), could selectively accumulate in the kidney and inhibit oxidative stress to alleviate AKI in mice model; a review about AKI; a review about the influence of nanoparticle physicochemical properties on kidney target; the NP with a selective Toll-like receptor 9 (TLR9) antagonist could target renal tubular and attenuate ischemic acute kidney injury in mice.38,40,44,47,48
Discussion
General Information
A general understanding exists on the topic of nanomedicine in kidney disease as shown in the above-mentioned analyses. The topic originated in 2003 and shows a noticeable upward tendency to date. The researchers from China and the United States made significant contributions with considerable cooperation between the 2 countries. In addition, organizations in the 2 countries significantly contributed. Notably, although China produced the most publications, the United States had the highest average citations of the top ten countries is vital for this field, having advantages in academia. The leading organization was the Sichuan University in China. Based on the co-authorship analysis of authors and co-citation analysis of cited authors, Professor Peng Huang was the leading author, and 22 authors published more than 5 papers. Rm Williams, J Wang, and Y Wang were always cited, so they contributed significantly to the study of nanotechnology in kidney disease. Furthermore, the research was focused on the chemistry, and nanoscience & nanotechnology fields instead of clinical application based on the analysis results from journals’ category.
Nanotechnology Facilitates Drug Delivery to the Kidney
Drug delivery is a significant field of nanotechnology in kidney disease (Figure 6). In the analysis of keywords as well as references, drug delivery was the leading field. “Drug delivery” was the sixth most frequent keyword and the label of reference cluster #4. Meanwhile, the keyword “gold nanoparticles” was the fifth most frequent keyword and the labels of keyword clusters #3, #5, and #7 were all NP. In addition, drug delivery was the main topic among the leading references and the references burst in recent years. Initially, JJ. Marty et al designed NPs as a drug delivery system in the 1970s.49 Subsequently, the issues regarding how NPs are delivered to the kidney have attracted attention.
 |
Figure 6 Nanoparticles loading drugs could accumulate in the special location of the kidney. |
The ability of NPs to target the kidneys depends on physicochemical properties.48 The size of NPs plays an important role in renal targeting. Researchers found that gold (AU)-based NPs of 75 ± 25 nm in diameter could sufficiently accumulate in the kidney mesangium.50 Materials can pass through the glomerular filtration barrier and be excreted in the urine if their effective radius is smaller than 4.2 nm. However, AU-based NPs smaller than 1 nm showed less renal clearance because they were trapped by endothelial glycocalyx of the glomerulus.51 NPs larger than 100 nm could be excreted through secretion instead of filtration.52 The NPs greater than 250nm, called mesoscale nanoparticles (MNPs), possess special kidney-targeting capacity and slow-release properties. They can specifically accumulate in proximal tubular epithelial cells by endocytosis of the endothelial cells of peritubular capillaries, thereby realizing kidney-targeting therapy.53 The glomerular filtration barrier also repels the negatively charged particles because the barrier is negatively charged. Therefore, more negatively charged NPs typically accumulate more in the kidneys than positively charged NPs.54,55 In addition, the neutral surface charge and zwitterionic coating prevent the opsonin and formation of protein corona, which could prevent NPs from penetrating.55 The drug delivery is also affected by the shape. Researchers proved that short rod NPs and spherical NPs were initially more distributed in the kidney than long rod NPs; however, a few days later, the results were reversed.56 The NPs with high molecular weight and high aspect ratio could also penetrate the glomerular filtration barrier, which was important for delivering small interfering RNA (siRNA) to the kidney.57,58 Furthermore, NPs were made of various materials, like lipid, polymer, protein, nucleic acid, and inorganics, various materials showed different renal accumulations with density being a key factor.59 NPs made of high-density materials usually accumulated more in the kidney and had lower clearance than low-density materials.48 However, the above-mentioned studies were based on healthy kidneys. Patients may have a different distribution of NPs because kidney disease can damage the glomerular filtration barrier.
In addition to passive delivery, the ligands including peptides and antibodies in the surface layer of NPs could act as active pathways.60 For example, the peptide amphiphile micelles assembled with a type of zwitterionic peptide ligand (KKEEE)3K, which bound to the megalin on proximal tubule cells, adequately targeted the kidneys in a mouse model.55,61 The α8 integrin was shown expressed in mesangial cells.62 Using the anti-α8 integrin antibody, liposomes were used to target kidneys in both normal and nephritis mice.63
In summary, NPs produced based on nanotechnology could facilitate drug delivery through active or passive methods, and the efficacy of passive delivery was related to the physicochemical properties of NPs such as the size, charge, shape, and density.
Nanotechnology in AKI
“Acute kidney injury” was the most common keyword and the label of keywords clusters #4 in Figure 5A. Additionally, AKI was the label of reference cluster #1 in Figure 5C and the main content of the top 10 references. AKI was defined as a 50% rise in serum creatinine from baseline level within 7 days, or an increase in creatinine greater than or equal to 0.3 mg/dL during 48 hours, or oliguria for 6 hours.64 It is well known that the pathogenesis of AKI is related to oxidative stress, inflammation, and mitochondrial dysfunction.65,66 However, the current management of AKI mainly focuses on symptomatic management, such as removal of induction, correction of ion disorders, hemodynamic management, prohibition of nephrotoxic drugs, and dialysis. Kidney-targeting drugs or methods for causal treatment are quite limited.
Nanotechnology can aid drugs targeting the kidney and reduce adverse reactions of the agents. To date, various NPs have shown kidney benefits in AKI animal models based on different mechanisms. Oxidative stress can aggravate AKI, and several antioxidant drugs have been tried to treat or prevent AKI. Resveratrol is a natural antioxidant; however, its water solubility and bioavailability are low. When it was loaded by NPs, its inhibitory effect on oxidative stress damage became much better than that of resveratrol alone in vivo.67 The accumulation and activation of macrophages in the kidney were important to the inflammatory reaction in AKI induced by severe acute pancreatitis (SAP). Clodronate, able to reduce macrophage in the tissue, has low cytomembrane permeability and a short half-life. Dang et al created superparamagnetic iron oxide (SPIO)-clodronate-liposomes, which could induce apoptosis and decrease the release of inflammatory mediators to improve the AKI induced by SAP.68 Mitochondrial dysfunction induces cell apoptosis and takes part in the AKI advance.15 Formoterol, a type of long-acting β-agonist, can promote mitochondrial biogenesis and has a desirable effect in vitro. However, the efficacy in vivo was limited because of the renal distribution and adverse reaction, NPs could solve those problems and increase the therapeutic effect.69
Nanotechnology can also be combined with other therapies to improve AKI, such as stem cell-based therapy and gene therapy.70 Mesenchymal stem cells (MSCs) participate in the repair process during AKI, and the extracellular vesicles (EVs) from MSCs are essential.71,72 EVs with a diameter of nanometers participate in cell–cell communication in almost all physiological processes. In addition, EVs from MSCs can be used as a type of nanomedicine and transport biological active molecules such as proteins, lipids, and nucleic acids to target cells.73 IL-10 mRNA was discovered in vesicles. Human-derived proximal tubule epithelial cells could synthesize IL-10 when co-cultured with EVs, thereby reducing the inflammatory response, fibrosis, and cell death.72,74 However, the efficacy in clinical trials was not satisfactory due to low bioavailability and kidney accumulation.75,76 Zhang et al developed Arg-Gly-Asp peptide nanofibers, which could enhance the stability of EVs and improve the therapeutic effect in mouse AKI model.77 Several other RNAs also participate in the pathogenesis of AKI.78,79 Researchers have successfully transfected long non-coding RNA (lncRNA)-OIP5-AS1 with the assistance of NPs to inhibit renal ischemic reperfusion injury in mice.80 Arginase-2 (Arg-2) leads to tubular injury in contrast-induced AK, and Arg-2 siRNA can inhibit the transcription and translation, thereby alleviating the renal injury. However, the uptake efficiency of siRNA is poor, which limits its renoprotection in vivo.81,82 The layer-by-layer assembly of renal-targeted polymeric NPs could solve the above problems and had a protective effect in the contrast-induced AKI mice model.83 Another RNA, miR-5100, has a low expression in AKI and may be a novel biomarker.84 Researchers successfully induced miR-5100 overexpression by injecting miR-5100-mimic conjugated with polyethylenimine NPs in the AKI mice and finally achieved the effect of prevention and treatment of AKI.84
Furthermore, nanotechnology may be helpful in the early diagnosis and monitoring of AKI. Based on nanotechnology, the detection of biomarkers can be simple and fast. For example, approximately only 5 minutes was necessary to detect neutrophil gelatinase-associated lipocalin in urine using an ultrarapid nanoconfinement-enhanced fluorescence clinical detection platform.85 NPs also assist in the imageological examination. The SPIO mentioned earlier, can be used as a tracer in MRI and has the potential to detect renal damage in mice.68 Recently, a nanosystem, platelet membranes-ICG-SS31-poly lactic-co-glycolic acid (PLGA), was developed that could target kidney lesion areas in mice models and be detected by near-infrared rays to aid in early detection and monitoring of AKI.86 Vesicles can be used for the treatment of AKI and also for the prediction of AKI. It was proven that the lower levels of podocalyxin-like protein 1-positive EVs in urine before surgery, the more serious AKI patients suffered after cardiac surgery.87
Nanotechnology in CKD
According to the latest KDIGO guideline, CKD is defined as abnormalities of kidney structure or function, present for a minimum of 3 months, with implications for health.88 CKD can be classified into 5 stages based on eGFR. At present, most CKD patients are not diagnosed in time, and the treatment effect is slow or even poor. In particular, effective therapy for advanced-stage CKD is quite limited. While nanotechnology is helpful for the diagnosis and treatment of CKD.
In renal dysfunction, several abnormal metabolites are present in patients and can be excreted through exhalation. Polyaniline NPs can detect ammonia in human breath to provide a cost-effective and noninvasive method for monitoring renal function.89 Recently, Luo et al created pentiptycene metallopolymer/single-walled carbon nanotube complexes that can more sensitively detect ammonia of CKD patients.90 Glutathione-coated AU NPs as imaging contrast agents were used to evaluate renal function, which was highly sensitive and noninvasive and could evaluate the unilateral renal function in mice models.91 Nanotechnology can also improve the detection methods for urinary albumin.92
Celastrol (CLT) is the major active component of the herb tripterygium wilfordii widely used for the treatment of certain CKDs. However, the toxicity of CLT limits its effect. Wu et al designed peptides coupled with CLT-phospholipid NPs to deliver CLT to endothelial cells and podocytes in the glomerulus and obtained satisfactory anti-inflammatory and kidney-beneficial effects in mouse CKD model.93 NPs can not only reduce the toxicity but also prolong the duration of drug efficacy. Emodin enema delays the progression of CKD, however, the short retention time and low solubility limit the application. With the polymer NP, better colon adhesion and persistent effects were reached than emodin alone.94 The EVs from MSCs mentioned above assist in renal repair after AKI and have therapeutic potential for CKD. Recently, Li et al discovered that MSC-derived EVs could ameliorate lupus nephritis by regulating the proportion of T cell subsets, reducing plasma cells and pro-inflammatory cytokines in vivo; however, the exact mechanism remained unclear.95 In a single-center, randomized, placebo-controlled clinical trial, EV injection was proven to improve the renal function of stage 3–4 CKD patients by regulating inflammatory reactions.96 With the increasing number of diabetic patients, diabetic nephropathy is gradually replacing primary glomerulonephritis as the major cause of CKD. A nanometal-organic framework containing chromium or selenium and zinc was proven to increase creatinine clearance and decrease urinary albumin in the diabetic nephropathy mouse model.97,98 In addition to diabetic nephropathy, nanotechnology can also assist in the treatment of other CKDs. For example, lupus nephritis is caused by the immune reaction of anti-dsDNA antibody which can be inhibited by D-form modified ALW peptide.99 The polyethylene glycol (PEG)-PLGA NP could improve the stability of ALW peptide and reduce the IgG and C3 deposition in the kidney.100 Renal fibrosis, the final pathology change of ESRD, was potentially relieved by NPs. It was proven that folic acid-conjugated gold NPs selectively accumulated in the renal tubules of the fibrotic kidney in unilateral ureteral obstruction mice and inhibited the p38α mitogen-activated protein kinase leading to the relief of tubulointerstitial fibrosis.101
Furthermore, nanomedicine can help alleviate complications of CKD. Hyperphosphatemia is a severe and common complication of CKD and may lead to secondary hyperparathyroidism and even increase the risk of mortality. Ma et al synthesized nano-lanthanum hydroxide, which had a higher specific surface area and thus a better phosphorus-binding rate. The safety and efficacy of the synthesized nano-lanthanum hydroxide were also proven in mouse models.102
In general, given the unique physicochemical properties, nanomedicine can achieve continuous release and long-lasting efficacy, thereby owing to a broad therapeutic prospect in CKD.
Nanotechnology and Oxidative Stress
“Oxidative stress” is the third frequency keyword and also the main topic of many references above. Five of the top 10 references indicated nanotechnology could improve AKI through antioxidative effects,40–43,46 showing that oxidative stress is an important field of nanotechnology in kidney disease. Oxidative stress is caused by the high production of reactive oxygen species (ROS), which can lead to the destruction of proteins, DNA, cytomembranes, and other substances, thereby resulting in cell death and kidney disease.103–105 Therefore, anti-ROS is an important therapeutic strategy for kidney disease. The application of nanotechnology in anti-ROS therapy mainly manifests in two aspects: inhibition of ROS generation and scavenging excess ROS. It has been reported that H2O2-responsive nanoparticles loaded with vanillyl alcohol could target ROS over-production sites and inhibit production.106 Lozano et al designed PLGA nanoparticles encapsulating quercetin, which could maintain the integrity of mitochondrial electron transfer chains, and then reduce ROS production.107 PLGA nanoparticles combined with Cyclosporin A, an immunosuppressant commonly used in kidney disease, were designed to inhibit mitochondrial permeability transition pore opening, thus reducing ROS damage.108 Besides inhibiting ROS production, it is equally important to eliminate existing ROS. Nanozymes are enzyme-mimicking nanomaterials with properties of low cost, high stability, and catalytic ability. It has been demonstrated that iron oxide NPs, a kind of metallic nano-enzyme, could mimic peroxidase and scavenge ROS in vivo. Nanotechnology can also deliver antioxidants.109 The efficacy of antioxidants in clinical treatment is still uncertain. Factors such as low bioavailability and instability may affect its effectiveness. Nano-delivery systems have been a promising solution. For example, researchers have prepared lactate protein-based polylactic acid NPs for the delivery of natural antioxidants. The NPs could improve the water solubility and bioavailability of curcumin and reduce its biotoxicity.110 Yu et al utilized ROS-responsive nanocapsules to deliver drugs to the kidney in diabetic kidney disease models.111 In addition, DNA can also play a therapeutic role with nanotechnology aiding. It has been reported that DNA with the origami nanostructure could eliminate ROS and accumulate preferentially in the kidneys.45 More importantly, the anti-complement component 5a could be loaded into the DNA nanostructure, enabling dual-target therapy.112 These studies indicate that nanotechnology has broad application prospects in anti-oxidative stress.
Other Kidney Diseases
Nanomedicine also shows potential for the treatment of hereditary nephropathy. A prevalent hereditary nephropathy is polycystic kidney disease (PKD), which is primarily an autosomal dominant inheritance. Research indicated that folate-conjugated PLGA-PEG NPs loading rapamycin and antioxidants could better control cystic development in vivo than rapamycin alone.113 In addition to drug loading, NPs can load nucleic acids, which may cure hereditary nephropathy at the genetic level in the future.18,19 However, the application of nanotechnology in genetic kidney disease involves ethics and supervision, and relevant systems and laws need to be continuously improved for the further development of nanomedicine.
The safety of certain NPs or medications connected to nanotechnology was proven in clinical trials, and several are currently on the market.114–117 For example, the polymeric NPs with erythropoiesis-stimulating agents have been approved for renal anemia treatment.117 A clinical study of domestic polysaccharide SPIO NP injection for renal contrast-enhanced MRI to evaluate renal blood vessels and renal function is currently underway.118
Immune response also plays a critical role in the pathogenesis of kidney diseases, particularly in the use of immunosuppressants for the treatment of CKD. However, the application of some immunosuppressants commonly used at present, such as glucocorticoids, is often limited because of obvious side effects. Therefore, it is of great clinical significance to further explore the role of nanomedicines in immune regulation. Several relevant literatures have been reported. For example, dexamethasone (DXM)-loaded IFN-γ-treated MHC class I deficient cancer membrane-coated NPs (IM-MNPs/DXM) were fabricated which could utilize the immunosuppressive power of tumor cells for the treatment of lupus nephritis. These particles could evade immune clearance and accumulate in inflammatory organs. The sustained release of DXM can inhibit the production of proinflammatory cytokines in the inflammatory microenvironment, exhibiting significant therapeutic efficacy in ameliorating lupus nephritis as well as decreasing side effects in vivo.119 It has been found that calcium calmodulin kinase IV is increased in podocytes of patients with focal segmental glomerulosclerosis and in mice injected with doxorubicin. Using NPs loaded with a small drug inhibitor of calcium calmodulin kinase IV and tagged with antibodies directed to CD4 can inhibit autoimmunity, thereby alleviating kidney damage.120 Therefore, developing nanomaterials with immunomodulatory properties could offer new therapeutic approaches for treating immune-mediated kidney diseases.
However, there are still some problems of nanotechnology used in kidney diseases, limiting the wide application of nanomedicine. For instance, commonly used metal NPs may be deposited in other organs, like the liver, spleen, or even the brain, and cause metal poisoning.121 Although the accelerating degradation rate of nano-drugs can improve the safety, the efficacy may be reduced.122,123 Doping, a widely used and effective strategy for inorganic NPs, seems to be a method to reduce inorganic NPs’ toxicity. It can prevent NPs from dissolution and binding with oxygen.124,125 However, whether doping may affect the efficacy of NPs still needs to be further explored. Therefore, to keep the balance between effectiveness and safety is necessary.122 Furthermore, a systematic and detailed safety evaluation as well as a regulatory system for nanomedicine are lacking, and the effects on long-term exposure to nanomedicine remain unclear. Therefore, the long-term observation of the side effects and safety of nanomedicine are essential.125
Conclusion and Future Perspective
In this review, bibliometric methods were used to comprehensively collect and analyze global publications on nanotechnology in kidney disease. The development trend of nanotechnology, high-yield authors and institutions, important literature, and research hotspots were summarized. The results are essential to fully understand the current status of nanotechnology in kidney disease, adjust future research directions, and explore unknown areas. Based on the results of this study, many questions and challenges remain to be solved in this fast-growing field.
First, drug delivery is a significant advantage of nanotechnology and is currently a hot research topic. However, the kidney structure is complex, including various cell types and tissue components. How to achieve precise delivery, such as cell-specific or tissue-specific, to render accurate targeted therapy into reality may be problematic.
Secondly, the current research on the application of nanomedicine in kidney disease is mainly focused on AKI. AKI was the most common keyword in all publications analyzed. In addition, among the 10 most-cited references, 9 were on AKI. Fewer studies were on CKD than AKI. CKD presents as a slowly progressing disease, and the continuity of drug therapy and the persistence of drug effects are important in clinical application. Therefore, the development of sustained- or controlled-release technology in nanomedicine is essential for the treatment of CKD.
Thirdly, the results of this analysis showed that the mechanism of nanomaterials in the treatment of kidney disease is mainly through antioxidative effects. “Oxidative stress” was the third most common among the top 10 keywords. The immune response is also important in the pathogenesis of kidney disease, and immunosuppressive agents are often administered in CKD treatment. Therefore, the development of nanomedicine with immunosuppressive effects should be further investigated.
Finally, the potential side effects and bioaccumulation issues associated with the long-term use of nanomedicines require more attention. These concerns are critical for clinical applications and may become significant research directions in the future. Monitoring the long-term safety and efficacy of nanomedicine has been a great challenge.
In conclusion, due to the continuous progress of nanotechnology and the rapid development of artificial intelligence, early diagnosis, precise treatment, and the possibility of curing kidney disease is becoming a reality based on multi-disciplinary cooperation.
Abbreviations
CKD, chronic kidney disease; AKI, acute kidney injury; DALYs, disability-adjusted life years; ESRD, end-stage renal disease; NDDS, nanodrug delivery system; FDA, United States Food and Drug Administration; NPs, nanoparticles; miR, microRNA; WoSCC, the Web of Science Core Collection; SCIE, the Science Citation Index-Expanded; SSCI, the Social Sciences Citation Index; A&HCI, the Arts & Humanities Citation Index; TI, title; AB, abstract; AK, author keywords; TLR9, Toll-like receptor 9; AU, gold; MNP, mesoscale nanoparticle; SAP, severe acute pancreatitis; SPIO, superparamagnetic iron oxide; MSCs, mesenchymal stem cells; EVs, extracellular vesicles; lncRNA, long non-coding RNA; Arg-2, arginase-2 ; siRNA, small interfering RNA, PLGA, poly lactic-co-glycolic acid; CLT, celastrol; PEG, polyethylene glycol; ROS, reactive oxygen species; PKD, polycystic kidney disease; DXM, dexamethasone.
Data availability statement
The data presented in this article are available on the WoSCC database using the search query listed in the “Materials and methods” section, further inquiries can be directed to the corresponding authors.
Acknowledgments
We would like to express our thanks to the authors of some images in the graphical abstract and Figure 6 for providing the images. They are brgfx, katemangostar, rawpixel.com, barudakvisual, macrovector, jemastock and upklyak on Freepik, Freepik itself, Servier, and Pinclipart.
Funding
This study was supported by grants from the National Natural Science Foundation of China (No.81870505, No.82270778).
Disclosure
The authors report no conflicts of interest in this work.
References
1. GBD Results. Institute for health metrics and evaluation. Accessed March. 2024;2. https://vizhub.healthdata.org/gbd-results.
2. Lameire NH, Bagga A, Cruz D, et al. Acute kidney injury: an increasing global concern. Lancet. 2013;382(9887):170–179. doi:10.1016/S0140-6736(13)60647-9
3. Lewington AJP, Cerdá J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013;84(3):457–467. doi:10.1038/ki.2013.153
4. GBD. 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
5. Woo KT, Choong HL, Wong KS, Tan HB, Chan CM. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2012;81(10):1044–1045. doi:10.1038/ki.2012.39
6. Provenzano M, Coppolino G, Faga T, Garofalo C, Serra R, Andreucci M. Epidemiology of cardiovascular risk in chronic kidney disease patients: the real silent killer. Rev Cardiovasc Med. 2019;20(4):209–220. doi:10.31083/j.rcm.2019.04.548
7. Hochella MF. There’s plenty of room at the bottom: nanoscience in geochemistry. Geochim Cosmochim Acta. 2002;66(5):735–743. doi:10.1016/S0016-7037(01)00868-7
8. Farokhzad OC, Langer R. Impact of nanotechnology on drug delivery. ACS Nano. 2009;3(1):16–20. doi:10.1021/nn900002m
9. Kostarelos K Establishing nanomedicine. Nanomedicine. Available from: https://www.tandfonline.com/doi/abs/10.2217/17435889.1.3.259.
10. Null A, Saraf S. Applications of novel drug delivery system for herbal formulations. Fitoterapia. 2010;81(7):680–689. doi:10.1016/j.fitote.2010.05.001
11. Huang L, Huang XH, Yang X, et al. Novel nano-drug delivery system for natural products and their application. Pharmacol Res. 2024;201:107100. doi:10.1016/j.phrs.2024.107100
12. Zingg R, Fischer M. The consolidation of nanomedicine. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2019;11(6):e1569. doi:10.1002/wnan.1569
13. Rivankar S. An overview of doxorubicin formulations in cancer therapy. J Cancer Res Ther. 2014;10(4):853. doi:10.4103/0973-1482.139267
14. Wang J, Zhao W, Zhang Z, et al.. A journey of challenges and victories: a bibliometric worldview of nanomedicine since the 21st century. Adv. Mater. 2308915. doi:10.1002/adma.202308915
15. Bishop B, Sharma S, Scott EA. Nanomedicine in kidney disease. Curr Opin Nephrol Hypertens. 2023;32(4):366–376. doi:10.1097/MNH.0000000000000897
16. Sabiu G, Kasinath V, Jung S, Li X, Tsokos GC, Abdi R. Targeted nanotherapy for kidney diseases: a comprehensive review. Nephrol Dial Transplant. 2022;38(6):1385–1396. doi:10.1093/ndt/gfac233
17. Cheng HT, Huang HC, Lee TY, et al. Delivery of sorafenib by myofibroblast-targeted nanoparticles for the treatment of renal fibrosis. J Control Release. 2022;346:169–179. doi:10.1016/j.jconrel.2022.04.004
18. Trac N, Ashraf A, Giblin J, Prakash S, Mitragotri S, Chung EJ. Spotlight on genetic kidney diseases: a call for drug delivery and nanomedicine solutions. ACS Nano. 2023;17(7):6165–6177. doi:10.1021/acsnano.2c12140
19. Mathew AP, Uthaman S, Bae EH, Lee JY, Park IK. Vimentin targeted nano-gene carrier for treatment of renal diseases. J Korean Med Sci. 2021;36(49):e333. doi:10.3346/jkms.2021.36.e333
20. Oroojalian F, Rezayan AH, Mehrnejad F, et al. Efficient megalin targeted delivery to renal proximal tubular cells mediated by modified-polymyxin B-polyethylenimine based nano-gene-carriers. Mater Sci Eng C Mater Biol Appl. 2017;79:770–782. doi:10.1016/j.msec.2017.05.068
21. McCormack PL. Ferumoxytol. Drugs. 2012;72(15):2013–2022. doi:10.2165/11209880-000000000-00000
22. Lu M, Cohen MH, Rieves D, Pazdur R. FDA report: ferumoxytol for intravenous iron therapy in adult patients with chronic kidney disease. Am J Hematol. 2010;85(5):315–319. doi:10.1002/ajh.21656
23. Smith AF, Zhao B, You M, Jiménez JM. Microfluidic DNA-based potassium nanosensors for improved dialysis treatment. Biomed Eng Online. 2019;18(1):73. doi:10.1186/s12938-019-0692-8
24. Kanno Y, Miki N. Development of a nanotechnology-based dialysis device. Contrib Nephrol. 2012;177:178–183. doi:10.1159/000337052
25. Saikumar J, Hoffmann D, Kim TM, et al. Expression, circulation, and excretion profile of microRNA-21, −155, and −18a following acute kidney injury. Toxicol Sci. 2012;129(2):256–267. doi:10.1093/toxsci/kfs210
26. Xu Y, Zhang Q, Chen R, et al. NIR-II photoacoustic-active DNA origami nanoantenna for early diagnosis and smart therapy of acute kidney injury. J Am Chem Soc. 2022;144(51):23522–23533. doi:10.1021/jacs.2c10323
27. Ninkov A, Frank JR, Maggio LA. Bibliometrics: methods for studying academic publishing. Perspect Med Educ. 2022;11(3):173–176. doi:10.1007/s40037-021-00695-4
28. Godin B. On the origins of bibliometrics. Scientometrics. 2006;68(1):109–133. doi:10.1007/s11192-006-0086-0
29. Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;101(Suppl 1):5303–5310. doi:10.1073/pnas.0307513100
30. Zou H, Zhang X, Chen W, et al. Vascular endothelium is the basic way for stem cells to treat erectile dysfunction: a bibliometric study. Cell Death Discov. 2023;9(1):143. doi:10.1038/s41420-023-01443-9
31. Pan D, Xu L, Shi D, Guo M. Knowledge mapping of mitochondrial calcium uniporter from 2011 to 2022: a bibliometric analysis. Front Physiol. 2023;14:1107328. doi:10.3389/fphys.2023.1107328
32. Wang J, Liu X, Pan D, Cai X, Xue Y, Huang J. Chronic kidney disease in the shadow of COVID-19: insights from the bibliometric analysis. Int Urol Nephrol. 2023;56:683–697. doi:10.1007/s11255-023-03706-x
33. van Eck NJ, Waltman L. Software survey: vOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84(2):523–538. doi:10.1007/s11192-009-0146-3
34. Aria M, Cuccurullo C. bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetrics. 2017;11(4):959–975. doi:10.1016/j.joi.2017.08.007
35. Gessner A, Lieske A, Paulke BR, Müller RH. Functional groups on polystyrene model nanoparticles:: influence on protein adsorption. J Biomed Mater Res Part A. 2003;65A(3):319–326. doi:10.1002/jbm.a.10371
36. Brookes BC. Bradford’s law and the bibliography of science. Nature. 1969;224(5223):953–956. doi:10.1038/224953a0
37. Kellum JA, Romagnani P, Ashuntantang G, Ronco C, Zarbock A, Anders HJ. Acute kidney injury. Nat Rev Dis Primers. 2021;7(1):52. doi:10.1038/s41572-021-00284-z
38. Ronco C, Bellomo R, Kellum JA. Acute kidney injury. Lancet. 2019;394(10212):1949–1964. doi:10.1016/S0140-6736(19)32563-2
39. Williams RM, Shah J, Tian HS, et al. Selective nanoparticle targeting of the renal tubules. Hypertension. 2018;71(1):87–94. doi:10.1161/HYPERTENSIONAHA.117.09843
40. Liu D, Shu G, Jin F, et al. ROS-responsive chitosan-SS31 prodrug for AKI therapy via rapid distribution in the kidney and long-term retention in the renal tubule. Sci Adv. 2020;6(41):eabb7422. doi:10.1126/sciadv.abb7422
41. Yu H, Jin F, Liu D, et al. ROS-responsive nano-drug delivery system combining mitochondria-targeting ceria nanoparticles with atorvastatin for acute kidney injury. Theranostics. 2020;10(5):2342–2357. doi:10.7150/thno.40395
42. Yu H, Lin T, Chen W, et al. Size and temporal-dependent efficacy of oltipraz-loaded PLGA nanoparticles for treatment of acute kidney injury and fibrosis. Biomaterials. 2019;219:119368. doi:10.1016/j.biomaterials.2019.119368
43. Ni D, Jiang D, Kutyreff CJ, et al. Molybdenum-based nanoclusters act as antioxidants and ameliorate acute kidney injury in mice. Nat Commun. 2018;9(1):5421. doi:10.1038/s41467-018-07890-8
44. Han SJ, Williams RM, D’Agati V, Jaimes EA, Heller DA, Lee HT. Selective nanoparticle-mediated targeting of renal tubular Toll-like receptor 9 attenuates ischemic acute kidney injury. Kidney Int. 2020;98(1):76–87. doi:10.1016/j.kint.2020.01.036
45. Jiang D, Ge Z, Im HJ, et al. DNA origami nanostructures can exhibit preferential renal uptake and alleviate acute kidney injury. Nat Biomed Eng. 2018;2(11):865–877. doi:10.1038/s41551-018-0317-8
46. Sun T, Jiang D, Rosenkrans ZT, et al. A melanin-based natural antioxidant defense nanosystem for theranostic application in acute kidney injury. Adv Funct Mater. 2019;29(48). doi:10.1002/adfm.201904833
47. Rosenkrans ZT, Sun T, Jiang D, et al. Selenium-doped carbon quantum dots act as broad-spectrum antioxidants for acute kidney injury management. Adv Sci. 2020;7(12):2000420. doi:10.1002/advs.202000420
48. Huang Y, Wang J, Jiang K, Chung EJ. Improving kidney targeting: the influence of nanoparticle physicochemical properties on kidney interactions. J Control Release. 2021;334:127–137. doi:10.1016/j.jconrel.2021.04.016
49. Nanoparticles--a new colloidal drug delivery system.-all databases. Available from: https://webofscience.clarivate.cn/wos/alldb/full-record/MEDLINE:643885.
50. Choi CHJ, Zuckerman JE, Webster P, Davis ME. Targeting kidney mesangium by nanoparticles of defined size. Proc Natl Acad Sci U S A. 2011;108(16):6656–6661. doi:10.1073/pnas.1103573108
51. Du B, Jiang X, Das A, et al. Glomerular barrier behaves as an atomically precise bandpass filter in a sub-nanometer regime. Nat Nanotechnol. 2017;12(11):1096–1102. doi:10.1038/nnano.2017.170
52. Wyss PP, Lamichhane SP, Abed A, et al. Renal clearance of polymeric nanoparticles by mimicry of glycan surface of viruses. Biomaterials. 2020;230:119643. doi:10.1016/j.biomaterials.2019.119643
53. Williams RM, Shah J, Ng BD, et al. Mesoscale nanoparticles selectively target the renal proximal tubule epithelium. Nano Lett. 2015;15(4):2358–2364. doi:10.1021/nl504610d
54. Liang X, Wang H, Zhu Y, et al. Short- and long-term tracking of anionic ultrasmall nanoparticles in kidney. ACS Nano. 2016;10(1):387–395. doi:10.1021/acsnano.5b05066
55. Huang Y, Jiang K, Zhang X, Chung EJ. The effect of size, charge, and peptide ligand length on kidney targeting by small, organic nanoparticles. Bioeng Transl Med. 2020;5(3):e10173. doi:10.1002/btm2.10173
56. Zhao Y, Wang Y, Ran F, et al. A comparison between sphere and rod nanoparticles regarding their in vivo biological behavior and pharmacokinetics. Sci Rep. 2017;7:4131. doi:10.1038/s41598-017-03834-2
57. Ruggiero A, Villa CH, Bander E, et al. Paradoxical glomerular filtration of carbon nanotubes. Proc Natl Acad Sci U S A. 2010;107(27):12369–12374. doi:10.1073/pnas.0913667107
58. Alidori S, Akhavein N, Thorek DLJ, et al. Targeted fibrillar nanocarbon RNAi treatment of acute kidney injury. Sci Transl Med. 2016;8(331):331ra39. doi:10.1126/scitranslmed.aac9647
59. Vasylaki A, Ghosh P, Jaimes EA, Williams RM. Targeting the kidneys at the nanoscale: nanotechnology in nephrology. Kidney360. 2024;5(4):618. doi:10.34067/KID.0000000000000400
60. Wang J, Masehi-Lano JJ, Chung EJ. Peptide and antibody ligands for renal targeting: nanomedicine strategies for kidney disease. Biomater Sci. 2017;5(8):1450–1459. doi:10.1039/c7bm00271h
61. Wischnjow A, Sarko D, Janzer M, et al. Renal targeting: peptide-based drug delivery to proximal tubule cells. Bioconjug Chem. 2016;27(4):1050–1057. doi:10.1021/acs.bioconjchem.6b00057
62. Schnapp LM, Breuss JM, Ramos DM, Sheppard D, Pytela R. Sequence and tissue distribution of the human integrin alpha 8 subunit: a beta 1-associated alpha subunit expressed in smooth muscle cells. J Cell Sci. 1995;108(Pt 2):537–544. doi:10.1242/jcs.108.2.537
63. Scindia Y, Deshmukh U, Thimmalapura PR, Bagavant H. Anti-alpha 8 integrin immunoliposomes: a novel system for delivery of therapeutic agents to the renal glomerulus in systemic lupus erythematosus. Arthritis Rheum. 2008;58(12):3884–3891. doi:10.1002/art.24026
64. Lameire NH, Levin A, Kellum JA, et al. Harmonizing acute and chronic kidney disease definition and classification: report of a kidney disease: improving global outcomes (Kdigo) consensus conference. Kidney Int. 2021;100(3):516–526. doi:10.1016/j.kint.2021.06.028
65. Yeh TH, Tu KC, Wang HY, Chen JY. From acute to chronic: unraveling the pathophysiological mechanisms of the progression from acute kidney injury to acute kidney disease to chronic kidney disease. Int J mol Sci. 2024;25(3):1755. doi:10.3390/ijms25031755
66. Ding Y, Zheng Y, Huang J, et al. UCP2 ameliorates mitochondrial dysfunction, inflammation, and oxidative stress in lipopolysaccharide-induced acute kidney injury. Int Immunopharmacol. 2019;71:336–349. doi:10.1016/j.intimp.2019.03.043
67. Nie Y, Wang L, Liu S, et al. Natural ursolic acid based self-therapeutic polymer as nanocarrier to deliver natural resveratrol for natural therapy of acute kidney injury. J Nanobiotechnology. 2023;21:484. doi:10.1186/s12951-023-02254-x
68. chun DS, hua ZY, jiang WP, et al. Clodronate-superparamagnetic iron oxide-containing liposomes attenuate renal injury in rats with severe acute pancreatitis. J Zhejiang Univ Sci B. 2014;15(6):556–565. doi:10.1631/jzus.B1300244
69. Vallorz EL, Blohm-Mangone K, Schnellmann RG, Mansour HM. Formoterol PLGA-PEG nanoparticles induce mitochondrial biogenesis in renal proximal tubules. AAPS J. 2021;23(4):88. doi:10.1208/s12248-021-00619-4
70. Zhao Y, Pu M, Wang Y, Yu L, Song X, He Z. Application of nanotechnology in acute kidney injury: from diagnosis to therapeutic implications. J Control Release. 2021;336:233–251. doi:10.1016/j.jconrel.2021.06.026
71. Cantley LG. Adult stem cells in the repair of the injured renal tubule. Nat Clin Pract Nephrol. 2005;1(1):22–32. doi:10.1038/ncpneph0021
72. Ragni E, Banfi F, Barilani M, et al. Extracellular vesicle-shuttled mRNA in mesenchymal stem cell communication. Stem Cells. 2017;35(4):1093–1105. doi:10.1002/stem.2557
73. Yáñez-Mó M, Siljander PRM, Andreu Z, et al. Biological properties of extracellular vesicles and their physiological functions. J Extracell Vesicles. 2015;4:27066. doi:10.3402/jev.v4.27066
74. Soranno DE, Rodell CB, Altmann C, et al. Delivery of interleukin-10 via injectable hydrogels improves renal outcomes and reduces systemic inflammation following ischemic acute kidney injury in mice. Am J Physiol Renal Physiol. 2016;311(2):F362–372. doi:10.1152/ajprenal.00579.2015
75. Aghajani Nargesi A, Lerman LO, Eirin A. Mesenchymal stem cell-derived extracellular vesicles for kidney repair: current status and looming challenges. Stem Cell Res Ther. 2017;8:273. doi:10.1186/s13287-017-0727-7
76. Kosanović M, Milutinović B, Kutzner TJ, Mouloud Y, Bozic M. Clinical prospect of mesenchymal stromal/stem cell-derived extracellular vesicles in kidney disease: challenges and the way forward. Pharmaceutics. 2023;15(7):1911. doi:10.3390/pharmaceutics15071911
77. Zhang C, Shang Y, Chen X, et al. Supramolecular nanofibers containing arginine-glycine-aspartate (RGD) peptides boost therapeutic efficacy of extracellular vesicles in kidney repair. ACS Nano. 2020;14(9):12133–12147. doi:10.1021/acsnano.0c05681
78. Ramanathan K, Fekadie M, Padmanabhan G, Gulilat H. Long noncoding RNA: an emerging diagnostic and therapeutic target in kidney diseases. Cell Biochem Funct. 2024;42(1):e3901. doi:10.1002/cbf.3901
79. Sabet Sarvestani F, Afshari A, Azarpira N. The role of non-protein-coding RNAs in ischemic acute kidney injury. Front Immunol. 2024;15:1230742. doi:10.3389/fimmu.2024.1230742
80. Zhang R, Zhang X, Zhu X, et al. Nanoparticles transfected with plasmid-encoded lncRNA-OIP5-AS1 inhibit renal ischemia-reperfusion injury in mice via the miR-410-3p/Nrf2 axis. Ren Fail. 2024;46(1):2319327. doi:10.1080/0886022X.2024.2319327
81. Zhou LY, Liu K, Yin WJ, et al. Arginase2 mediates contrast-induced acute kidney injury via facilitating nitrosative stress in tubular cells. Redox Biol. 2023;67:102929. doi:10.1016/j.redox.2023.102929
82. Hu B, Zhong L, Weng Y, et al. Therapeutic siRNA: state of the art. Signal Transduct Target Ther. 2020;5(1):101. doi:10.1038/s41392-020-0207-x
83. rui GX, Fan TY, Liu Z, et al. Layer-by-layer assembly of renal-targeted polymeric nanoparticles for robust arginase-2 Knockdown and contrast-induced acute kidney injury prevention. Adv Healthcare Mater. 2024;13(20):2304675. doi:10.1002/adhm.202304675
84. Aomatsu A, Kaneko S, Yanai K, et al. MicroRNA expression profiling in acute kidney injury. Transl Res. 2022;244:1–31. doi:10.1016/j.trsl.2021.11.010
85. Yu M, Ye R, Zeng T, et al. Constructing an ultra-rapid nanoconfinement-enhanced fluorescence clinical detection platform by using machine learning and tunable DNA xerogel “probe. Anal Chem. 2023;95(42):15690–15699. doi:10.1021/acs.analchem.3c02955
86. Yao S, Wu D, Hu X. Platelet membrane-coated bio-nanoparticles of indocyanine green/elamipretide for NIR diagnosis and antioxidant therapy in acute kidney injury. Acta Biomater. 2024;173:482–494. doi:10.1016/j.actbio.2023.11.010
87. Miller D, Eagle-Hemming B, Sheikh S, et al. Urinary extracellular vesicles and micro-RNA as markers of acute kidney injury after cardiac surgery. Sci Rep. 2022;12(1):10402. doi:10.1038/s41598-022-13849-z
88. Stevens PE, Ahmed SB, Carrero JJ, et al. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. 2024;105(4):S117–S314. doi:10.1016/j.kint.2023.10.018
89. Hibbard T, Crowley K, Kelly F, et al. Point of care monitoring of hemodialysis patients with a breath ammonia measurement device based on printed polyaniline nanoparticle sensors. Anal Chem. 2013;85(24):12158–12165. doi:10.1021/ac403472d
90. Luo SXL, Swager TM. Wireless detection of trace ammonia: a chronic kidney disease biomarker. ACS Nano. 2024;18(1):364–372. doi:10.1021/acsnano.3c07325
91. Yu M, Zhou J, Du B, et al. Noninvasive staging of kidney dysfunction enabled by renal-clearable luminescent gold nanoparticles. Angew Chem Int Ed Engl. 2016;55(8):2787–2791. doi:10.1002/anie.201511148
92. Yang K, Shang Y, Yang N, Pan S, Jin J, He Q. Application of nanoparticles in the diagnosis and treatment of chronic kidney disease. Front Med. 2023;10:1132355. doi:10.3389/fmed.2023.1132355
93. Wu Q, Wang J, Wang Y, et al. Targeted delivery of celastrol to glomerular endothelium and podocytes for chronic kidney disease treatment. Nano Res. 2022;15(4):3556–3568. doi:10.1007/s12274-021-3894-x
94. Lu Z, Ji C, Luo X, et al. Nanoparticle-mediated delivery of emodin via colonic irrigation attenuates renal injury in 5/6 nephrectomized rats. Front Pharmacol. 2021;11:606227. doi:10.3389/fphar.2020.606227
95. Li C, Wu F, Mao J, et al. Mesenchymal stem cells-derived extracellular vesicles ameliorate lupus nephritis by regulating T and B cell responses. Stem Cell Res Ther. 2024;15(1):216. doi:10.1186/s13287-024-03834-w
96. Nassar W, El-Ansary M, Sabry D, et al. Umbilical cord mesenchymal stem cells derived extracellular vesicles can safely ameliorate the progression of chronic kidney diseases. Biomater Res. 2016;20:21. doi:10.1186/s40824-016-0068-0
97. Fakharzadeh S, Argani H, Torbati PM, et al. DIBc nano metal-organic framework improves biochemical and pathological parameters of experimental chronic kidney disease. J Trace Elem Med Biol. 2020;61:126547. doi:10.1016/j.jtemb.2020.126547
98. Fakharzadeh S, Kalanaky S, Argani H, et al. Ameliorative effect of a nano chromium metal-organic framework on experimental diabetic chronic kidney disease. Drug Dev Res. 2021;82(3):393–403. doi:10.1002/ddr.21759
99. Xia Y, Eryilmaz E, Der E, et al. A peptide mimic blocks the cross-reaction of anti-DNA antibodies with glomerular antigens. Clin Exp Immunol. 2016;183(3):369–379. doi:10.1111/cei.12734
100. Wang Y, Wang S, Liu W, et al. Anti-DNA antibody-targeted D-peptide nanoparticles ameliorate lupus nephritis in MRL/lpr mice. J Autoimmun. 2024;145:103205. doi:10.1016/j.jaut.2024.103205
101. Chan CKW, Szeto CC, Lee LKC, et al. A sub-10-nm, folic acid-conjugated gold nanoparticle as self-therapeutic treatment of tubulointerstitial fibrosis. Proc Natl Acad Sci U S A. 2023;120(42):e2305662120. doi:10.1073/pnas.2305662120
102. Ma Z, Yu T, Wu Y, et al. Nano-lanthanum hydroxide, a novel phosphate binder, for treating hyperphosphatemia: a preclinical study. Biomed Pharmacother. 2019;111:909–916. doi:10.1016/j.biopha.2018.12.107
103. Thomas K, Zondler L, Ludwig N, et al. Glutamine prevents acute kidney injury by modulating oxidative stress and apoptosis in tubular epithelial cells. JCI Insight. 2022;7(21):e163161. doi:10.1172/jci.insight.163161
104. Terawaki H, Yoshimura K, Hasegawa T, et al. Oxidative stress is enhanced in correlation with renal dysfunction: examination with the redox state of albumin. Kidney Int. 2004;66(5):1988–1993. doi:10.1111/j.1523-1755.2004.00969.x
105. Daehn IS, Ekperikpe US, Stadler K. Redox regulation in diabetic kidney disease. Am J Physiol Renal Physiol. 2023;325(2):F135–F149. doi:10.1152/ajprenal.00047.2023
106. Bae S, Park M, Kang C, et al. Hydrogen peroxide-responsive nanoparticle reduces myocardial ischemia/reperfusion injury. J Am Heart Assoc. 2016;5(11):e003697. doi:10.1161/JAHA.116.003697
107. L O, La A, Sp C, et al. Nanoencapsulated quercetin improves cardioprotection during hypoxia-reoxygenation injury through preservation of mitochondrial function. Oxid Med Cell Longev. 2019. doi:10.1155/2019/7683051
108. Zhang CX, Cheng Y, Liu DZ, et al. Mitochondria-targeted cyclosporin A delivery system to treat myocardial ischemia reperfusion injury of rats. J Nanobiotechnology. 2019;17(1):18. doi:10.1186/s12951-019-0451-9
109. Xiong F, Wang H, Feng Y, et al. Cardioprotective activity of iron oxide nanoparticles. Sci Rep. 2015;5:8579. doi:10.1038/srep08579
110. Nabofa WEE, Alashe OO, Oyeyemi OT, et al. Cardioprotective effects of curcumin-nisin based poly lactic acid nanoparticle on myocardial infarction in guinea pigs. Sci Rep. 2018;8(1):16649. doi:10.1038/s41598-018-35145-5
111. Yu M, Wang D, Zhong D, Xie W, Luo J. Adropin carried by reactive oxygen species-responsive nanocapsules ameliorates renal lipid toxicity in diabetic mice. ACS Appl Mater Interfaces. 2022;14(33):37330–37344. doi:10.1021/acsami.2c06957
112. Chen Q, Ding F, Zhang S, et al. Sequential therapy of acute kidney injury with a DNA nanodevice. Nano Lett. 2021;21(10):4394–4402. doi:10.1021/acs.nanolett.1c01044
113. Pala R, Barui AK, Mohieldin AM, Zhou J, Nauli SM. Folate conjugated nanomedicines for selective inhibition of mTOR signaling in polycystic kidneys at clinically relevant doses. Biomaterials. 2023;302:122329. doi:10.1016/j.biomaterials.2023.122329
114. Jiang H, Li Q, Chen B, et al. Phase I study of cisplatin and nanoparticle albumin-bound-paclitaxel combined with concurrent radiotherapy in locally advanced esophageal squamous cell carcinoma. Cancer Med. 2023;12(14):15187–15198. doi:10.1002/cam4.6205
115. Keefe SM, Hoffman-Censits J, Cohen RB, et al. Efficacy of the nanoparticle-drug conjugate CRLX101 in combination with bevacizumab in metastatic renal cell carcinoma: results of an investigator-initiated phase I-IIa clinical trial. Ann Oncol. 2016;27(8):1579–1585. doi:10.1093/annonc/mdw188
116. Miauton A, Audran R, Besson J, et al. Safety and immunogenicity of a synthetic nanoparticle-based, T cell priming peptide vaccine against dengue in healthy adults in Switzerland: a double-blind, randomized, vehicle-controlled, phase 1 study. EBioMedicine. 2024;99:104922. doi:10.1016/j.ebiom.2023.104922
117. Namiot ED, Sokolov AV, Chubarev VN, Tarasov SHB VV, Schiöth HB. Nanoparticles in clinical trials: analysis of clinical trials, fda approvals and use for COVID-19 vaccines. Int J mol Sci. 2023;24(1):787. doi:10.3390/ijms24010787
118. Li C Clinical Study of Domestic Polysaccharide Superparamagnetic Iron Oxide Nanoparticle Injection for Renal Contrast-Enhanced Magnetic Resonance Imaging clinicaltrials.gov. 2023. Available from: https://clinicaltrials.gov/study/NCT05045872.
119. Guo Q, Chen C, Wu Z, et al. Engineered PD-1/TIGIT dual-activating cell-membrane nanoparticles with dexamethasone act synergistically to shape the effector T cell/Treg balance and alleviate systemic lupus erythematosus. Biomaterials. 2022;285:121517. doi:10.1016/j.biomaterials.2022.121517
120. Tsokos GC, Tsokos MG. TARGETING TARGETED TREATMENT FOR IMMUNE AND NON-IMMUNE KIDNEY DISEASES. Trans Am Clin Climatol Assoc. 2019;130:88–99.
121. Liao C, Li Y, Tjong SC. Bactericidal and cytotoxic properties of silver nanoparticles. Int J mol Sci. 2019;20(2):449. doi:10.3390/ijms20020449
122. Li L, Shen Y, Tang Z, et al. Engineered nanodrug targeting oxidative stress for treatment of acute kidney injury. Exploration. 2023;3(6):20220148. doi:10.1002/EXP.20220148
123. Simpson CA, Salleng KJ, Cliffel DE, Feldheim DL. In vivo toxicity, biodistribution, and clearance of glutathione-coated gold nanoparticles. Nanomedicine. 2013;9(2):257–263. doi:10.1016/j.nano.2012.06.002
124. Naatz H, Lin S, Li R, et al. Safe-by-design cuO nanoparticles via Fe-Doping, Cu-O bond length variation, and biological assessment in cells and zebrafish embryos. ACS Nano. 2017;11(1):501–515. doi:10.1021/acsnano.6b06495
125. Najahi-Missaoui W, Arnold RD, Cummings BS. safe nanoparticles: are we there yet?. Int J mol Sci. 2020;22(1):385. doi:10.3390/ijms22010385
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
A Mini-Review of Diagnostic and Therapeutic Nano-Tools for Pancreatitis

Zhang Q, Li S, Yu Y, Zhu Y, Tong R
International Journal of Nanomedicine 2022, 17:4367-4381
Published Date: 19 September 2022
An Integrated Analysis of Inflammatory Endotypes and Clinical Characteristics in Chronic Rhinosinusitis with Nasal Polyps
Hao D, Wu Y, Li P, Li C, Jiang T, Zhang Q, Liu S, Shi L
Journal of Inflammation Research 2022, 15:5557-5565
Published Date: 24 September 2022
Extracellular Vesicles in Idiopathic Pulmonary Fibrosis: Pathogenesis, Biomarkers and Innovative Therapeutic Strategies

Yang Y, Lv M, Xu Q, Wang X, Fang Z
International Journal of Nanomedicine 2024, 19:12593-12614
Published Date: 25 November 2024
Polyethylene Glycols Stimulate Ca2+ Signaling, Cytokine Production, and the Formation of Neutrophil Extracellular Traps
Hinz A, Stankiewicz S, Litewka JJ, Ferdek PE, Sochalska M, Bzowska M
International Journal of Nanomedicine 2024, 19:13165-13181
Published Date: 7 December 2024
Drug Delivery System Targeting Cancer-Associated Fibroblast for Improving Immunotherapy
Zhang Z, Wang R, Chen L
International Journal of Nanomedicine 2025, 20:483-503
Published Date: 11 January 2025





