Back to Journals » Infection and Drug Resistance » Volume 18
Retrospective Analysis of Factors Associated with a Prolonged Nucleic Acid Conversion Time in Patients with COVID-19 at Fangcang Shelter Hospital
Authors Li Y, Wei Y , Wang Y, Chen Q , Hou X
Received 17 February 2025
Accepted for publication 16 June 2025
Published 30 June 2025 Volume 2025:18 Pages 3219—3229
DOI https://doi.org/10.2147/IDR.S521808
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Oliver Planz
Yang Li,1,* Yang Wei,2,* Yu Wang,1 Qiuxia Chen,1,3 Xianhua Hou1,3
1Department of Neurology, The First Affiliated Hospital of Army Medical University, Chongqing, People’s Republic of China; 2Department of Vascular Surgery, The First Affiliated Hospital of Army Medical University, Chongqing, People’s Republic of China; 3Department of Neurology of Jiangbei Campus, The First Affiliated Hospital of Army Medical University, Chongqing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xianhua Hou, Department of Neurology, The First Affiliated Hospital of Army Medical University, No. 30 Gaotanyan Main St, Shapingba District, Chongqing, 400038, People’s Republic of China, Email [email protected] Qiuxia Chen, Department of Neurology of Jiangbei Campus, The First Affiliated Hospital of Army Medical University, No. 29 Jianxin East Road St, Jiangbei District, Chongqing, 400020, People’s Republic of China, Email [email protected]
Objective: The aim of this study was to explore the related factors for prolonged nucleic acid conversion time (NCT) in patients with SARS-CoV-2 Omicron variant, so as to help to prevent and control the epidemic.
Methods: This study retrospectively included 307 patients diagnosed with mild to moderate COVID-19 who were hospitalized in Shanghai International Exhibition Fangcang Shelter Hospital. Nucleic acid amplification detection method was used to detect 2019-nCoV nucleic acid in nasopharyngeal swab samples. Binary logistic regression models were developed to identify independent risk factors associated with the time to nucleic acid conversion, utilizing the Kaplan-Meier test for survival analysis.
Results: In total, 307 patients were included in the study, with the median of NCT was 8 (6, 10) days, ranging 2 to 24 days, by which patients were divided into early NCT (< 8 days) and late NCT (≥ 8 days). There was no difference between early and late NCT groups in gender, nationality, diabetes, previous sleep disorder, dyssomnia and depression (P = 0.222, 0.552, 0.118, 0.501, 0.133 and 0.603, respectively). There was a statistically significant difference between the two groups at different age levels, hypertension, anxiety (P=0.002, 0.001, 0.034). In the late NCT group, compared to early NCT, more patients with symptoms(37.5 vs 19.0%; P < 0.001), only cough and expectoration (29.4 vs 14.3; P=0.001), myodynia (13.8 vs 4.1; P=0.014) and fatigue (13.8 vs 4.1; P=0.003) were statistically different. There was no significant difference in the presence or absence of vaccination and the number of vaccination between the two groups(P=0.340 and 0.435).
Conclusion: Our study showed that age, hypertension, and anxiety were independent risk factors associated with the NCT in patients with COVID-19. Potential risk factors should be taken into consideration for the strategy of quarantining infected patients.
Keywords: COVID-19, SARS-CoV-2Viral, risk factors, negative conversion
Introduction
Coronavirus disease 2019(COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is spreading rapidly throughout the world and burdening health care systems across the globe.1 Cities have been particularly affected by the COVID-19 pandemic. At the end of February 2022, a wave of SARS-CoV-2 infection quickly emerged in Shanghai, China. Phylogenetic characterization of the SARS-CoV-2 viral genomes of 129 patients during this period and their relationship with the GISAID database revealed that all new viral genomes in Shanghai-infected individuals were clustered in the SARS-CoV-2BA.2.2 subline.2
In late 2021, the Omicron variant (B.1.1.529) of SARS-CoV-2 emerged in South Africa, causing a spike in COVID-19 cases. The World Health Organization labeled it a variant of concern on November 26, 2021. The previous study found Omicron to be 10 times more contagious than the original virus and twice as contagious as Delta, with double the immune evasion capability.2 The accumulation of mutations in the Spikes (S) gene specifically could alter the viral pathogenicity and immunogenicity. S gene mutations are also present in the highly transmissible South African variant.3 By February 2022, Shanghai, China, experienced a surge in infections, despite over 90% overall vaccination coverage. However, only 62% of those over 60 were vaccinated, and just 38% had booster shots.4 The main circulating Omicron sub-variants were BA1, BA2, and BA3, with all new cases in Shanghai linked to the BA.2.2 subline. Although vaccination continues worldwide, the impact of the vaccine on mutations in the SARS-CoV-2 genes is unclear. It has been suggested that combating covid-19 is to control its source-isolating patients.5
According to the current diagnosis and treatment plan for novel coronavirus pneumonia, a positive nucleic acid test for novel coronavirus is the primary criterion for diagnosis and release from isolation.6 Therefore, understanding RNA shedding dynamics could help inform preventing the spread of the disease, and intervening in the factors that prolong NCT can shorten the isolation time. At present, there have been many clinical studies of SARS-CoV-2 virus nucleic acid conversion to negative, but the results show that the NCT is very different.7 Age, hypertension, D-dimer level, bacterial co-infection and disease severity are associated with viral shedding time.8–11 However, data regarding the potential factors associated with the NCT in patients with COVID-19 caused by omicron are limited. In this study, we analyzed the situation in non-severe COVID-19 patients and explored the related factors prolonged NCT, so as to help to prevent and control the epidemic.
Method
Study Design
This study retrospectively included 307 patients diagnosed with COVID-19 who were hospitalized in Shanghai International Exhibition Fangcang Shelter Hospital from April 15, 2022 to May 21, 2022. According to the World Health Organization COVID-19 disease severity classification, mild disease is described as patients who meet the COVID-19 case definition but do not have viral pneumonia or hypoxia. Moderate disease is defined as clinical symptoms of pneumonia (fever, cough, dyspnea, and shortness of breath) and pulse oximetry (SpO2) ≥ 90% (in room air) but no symptoms of severe pneumonia (someone in the Clinical symptoms: respiratory rate >30/min, severe respiratory distress or SpO2 <90%, room air). This study was approved by the Ethics Committee of the First Affiliated Hospital of Army Military Medical University (approval no. (B)KY2022160), and was exempt from informed consent.
Although mild cases do not require hospitalization, all nucleic acid-positive patients require centralized isolation management, so all patients are from Fangcang shelter hospitals. Exclusion criteria included a previously diagnosed severe psychiatric illness (eg schizophrenia or bipolar disorder) or severe cognitive impairment, incomplete data records, and those vaccinated with adenovirus and recombinant vaccine.
Existing evidence shows that the diagnostic accuracy of Omicron is not affected by the PCR test routinely used in our country.6 At present, nucleic acid amplification detection methods are often used to detect new coronavirus nucleic acid in nasal, oropharyngeal swabs, sputum and other lower respiratory tract secretions, feces and other specimens. Therefore, in this study, the nucleic acid amplification detection method was used to detect the nucleic acid of novel coronavirus in nasopharyngeal swab samples. In instances where the values for positive, negative, and internal controls satisfied the established criteria, a cycle threshold (Ct) value of less than 35 was considered indicative of a positive result.
Measures and Data Collection
The electronic questionnaire was made through the questionnaire star platform. The participants scanned the quick response code of the questionnaire through their mobile phone to complete the questionnaire. The study questionnaire collected basic information including demographic characteristics (gender, age, nationality), admission number, previous sleep status, clinical symptoms (cough, expectoration, rhinobyon, fever, pharyngalgia, fatigue, loss of taste and smell, Myodynia, headache, dizziness, burning ribs).
The Chinese version of the Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality. The Chinese version of the PSQI has sufficient reliability, with an internal consistency Cronbach’s α of 0.77 to 0.84.12 The PSQI consists of 18 entries in 7 dimensions: sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disturbance, use of sleeping medications, and daytime dysfunction.13 Each item is scored from 0 to 3, with the total score ranging from 0 to 21. A higher score indicates a lower sleep quality. Poor sleep quality was defined as a total score >5.14 The Patient Health Questionnaire-9 (PHQ-9) and the General Anxiety Disorder-7(GAD-7) was used to evaluate the anxiety and depression. PHQ-9 consists of 9 items with a total score of 27. GAD-7 consists of 7 items with a maximum score of 21. Each item is scored from 0 to 3. Higher scores indicate a greater severity of depression / anxiety. A cut-off value of 10 was used to measure the binary outcomes of depression and anxiety.15
Obtain the participants’ admission number via the electronic questionnaire, and collect the participants’ case data, including hypertension, diabetes history, Ct value of SARS-CoV-2, and NCT. The Ct values included the first positive nucleic acid and the lowest open reading frames 1ab (ORF 1ab) gene values and nucleocapsid gene (N gene) values during hospitalization. NCT is defined as the duration from the first day of positive RT-PCR result till the first day showing negative on nucleic acid testing successively.16
Statistical Analysis
Statistical analysis was performed for all data using SPSS 17.0. Categorical variables and ranked data were described as the quantity (n) and percentage (%), non-normally distributed measurement data are represented as the median (M: P25, P75). The Mann–Whitney U-test was used to compare the differences between two groups for quantitative variables. In this study, negative conversion of viral RNA during the communicable period, as time-to-event data, was the outcome measure. Covariates with a p-value of less than 0.10 in the univariate analysis were subsequently included in the multivariate analysis. Binary logistic regression models were developed to identify independent risk factors associated with the time to nucleic acid conversion, utilizing the Kaplan-Meier test for survival analysis. p < 0.05 were considered statistically significant differences.
Results
Demographic Characteristics of Patients
In total, 307 patients were included in the study, with the median of NCT was 8 (6, 10) days, ranging 2 to 24 days, by which patients were divided into early NCT (<8 days) and late NCT (≥8 days). The median of early NCT was 6 (4, 7) days (47.88%, n=147). The median of late NCT was 10 (8, 13) days(52.12%, n=160). Of all patients, 211 were male (68.7%) and 96 were female (31.3%), 299 were Han (97.4%) and 8 were minority (2.6%). There was no difference between early and late NCT groups in gender and nationality (P = 0.222 and 0.552, respectively). There was a statistically significant difference between the two groups at different age levels (P=0.002). Detailed demographic characteristics of the patients included in this study are presented in Table 1.
 |
Table 1 Sociodemographic Characteristics |
Comorbidity, Sleep Quality, and Psychological Status
There was no difference between early and late NCT groups in diabetes, previous sleep disorder, dyssomnia and depression (P = 0.118, 0.501, 0.133 and 0.603, respectively). In the late NCT group, compared to early NCT, hypertension are more common (10.6 vs 1.4%; P = 0.001), and more patients with symptoms(37.5 vs 19.0%; P < 0.001).Anxiety was statistically significant in the early NCT and late NCT groups (3.4 vs 9.4%; P = 0.034) (Table 2).
 |
Table 2 Past History, Sleep Quality and Psychological Status in the Two Groups |
Clinical Symptom
The clinical symptoms of the patients mainly included 68 cases of cough and expectoration (22.1%), 30 cases of Myodynia (9.8%), 29 cases of fever (9.4%) and 28 cases (9.1%) of fatigue. In the late NCT group, compared to early NCT, only cough and expectoration (29.4 vs.14.3; P=0.001), Myodynia (13.8 vs 4.1; P=0.014) and fatigue (13.8 vs 4.1; P=0.003) were statistically different (Table 3).
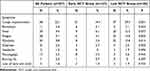 |
Table 3 Comparison of Clinical Symptoms |
Vaccination Status and Ct Value
In the late NCT group, compared with the early NCT group, the median of the first-time nucleic acid-positive ORF 1ab gene, the first-time nucleic acid-positive N gene, the minimum ORF 1ab gene and the minimum N gene were lower(28.02 vs 31.10, P =0.002; 26.22 vs. 29.38, P =0.001; 26.45 vs.29.31, P < 0.001; 24.57 vs. 27.60, P < 0.001).There was no significant difference in the presence or absence of vaccination and the number of vaccination between the two groups(P=0.340 and 0.435)(Table 4).
 |
Table 4 Comparison of Vaccination Status and Ct Values |
Sleep Quality
Among the sleep quality indicators, only hypnotics were statistically different in the two groups (P=0.039), with the median score of 0.00 (0.00, 0.00) in the overall patient, early NCT and late NCT groups (Table 5).
 |
Table 5 Comparison of Sleep Quality Indicators Between the Two Groups |
Covariate Screening Results
We used P < 0.10 to filter covariates, identifying age, hypertension, anxiety, clinical symptoms, cough, expectoration, fever, fatigue, muscle pain, hypnotic drugs, and CT value as factors linked to NCT (Table 1–5). Hypnotic drugs were excluded because they were one of the indicators for judging sleep quality, and the overall difference in sleep quality between the two groups was not statistically significant.
Multivariate Analysis of Independent Risk Factors Associated with the Prolonged NCT of SARS-CoV-2 RNA
Multivariate analysis revealed that older age (OR=1.325, 95% confidence interval [CI]: 1.072–1.636, P=0.009), hypertension(OR=5.571, 95% CI: 1.140–27.219, P=0.034), anxiety(OR=3.355, 95% CI: 1.043–10.791, P=0.042), anxiety(OR=3.355, 95% CI: 1.043–10.791, P=0.042), and fatigue(OR=5.039, 95% CI: 1.226–20.714, P=0.025) independently increase the risk of prolonged NCT. However, there was no significant difference in the clinical symptoms, cough and expectoration, fever, Myodynia and Ct values (Table 6).
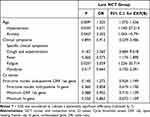 |
Table 6 Multivariate Analysis of the Independent Risk Factors for Advanced NCT |
Survival Analysis of Independent Risk Factors for Late NCT
The Kaplan Meier survival curves of 307 COVID-19 patients with SARS-CoV-2 RNA overall negative transformation revealed that the median time for SARS-CoV-2 RNA clearance was 8 days (Figure 1).
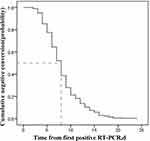 |
Figure 1 The Kaplan Meier survival curves of 307 COVID-19 patients with SARS-CoV-2 RNA overall negative transformation. |
We employed the Log rank test to evaluate the various factors on the duration of nucleic acid conversion in patients with COVID-19. The analysis revealed that age is associated with the rate of viral RNA clearance, with a p-value of 0.002 (refer to Figure 2A). Specifically, patients aged 17 years or younger exhibited the most rapid conversion to viral RNA negativity, with a median time of 6 days (95% CI: 4.717–7.283). In contrast, patients aged 41 to 50 years demonstrated the slowest conversion rate, with a median time of 9 days (95% CI: 8.324–9.676). Patients with a history of hypertension exhibited a significantly slower rate of viral RNA negative conversion, as indicated by a median duration of 12 days (95% CI: 9.939–14.061), compared to 7 days (95% CI: 6.562–7.438) for those without hypertension (P=0.004, Figure 2B). Anxiety also has been showed associated with the rate of viral RNA negative conversion, with a median duration of 9 days (95% CI: 7.569–10.431) for patients with anxiety, compared to 8 days (95% CI: 7.565–8.435) for those without anxiety (P=0.008, Figure 2C). In contrast, fatigue did not present a significant difference in the duration of SARS-CoV-2 RNA negative conversion (P=0.181, Figure 2D).
Discussion
Although COVID-19 has disseminated extensively worldwide, there remains considerable debate regarding the factors associated with the timing of viral clearance. It has been reported that increased NCT is an independent risk factor for long-term hospital stay.17 We hypothesize that intervention with factors that prolong NCT may shorten hospital stay. A nomogram based on predictors influencing persistent viral infection can be used as predictive tools to guide treatment and isolation strategies.18
Therefore, we performed a retrospective cohort study of 307 confirmed patients with SARS-CoV-2 at Shanghai International Exhibition Fangcang Shelter Hospital. Until now, there is no uniform international definition of NCT, and in this study the definition is consistent with that used in other high-quality studies as described in the Methods section.16 The median time to viral conversion observed in our study cohort was 8 days (IQR 6–10 days) from the first positive RT-PCR test, similar to the results of the study by Ling et al.19 Other studies have demonstrated a longer median duration of viral shedding of 12 days (IQR 10–14 days) and 15 days (IQR 12–18 days).20,21 The discrepancies might be attributed to the severity of disease, nucleic acid collection, and nucleic acid positive criteria in these studies.
In our study, 307 patients were included with a median of 8 (6,10) days of NCT ranging from 2 to 24 days. We divided the patients into early NCT group and late NCT group based on this median. The trough of ORF 1ab gene and N gene was lower in the late NCT group, and the trough of N gene and ORF 1ab gene was negatively correlated with the time of first negative transformation of the virus. Based on this, it is speculated that the lower the Ct value of N gene and ORF 1ab gene (ie the higher the viral load), the longer the time for the virus to turn negative for the first time. Our study showed that age, hypertension, and anxiety were independent risk factors associated with the NCT in patients with COVID-19, but not in terms of clinical symptoms, cough and expectoration, fever, Myodynia and Ct values.
Older individuals are the most vulnerable group in the pandemic.22 The Omicron-predominant wave led to a significant increase in mortality, particularly among the elderly population.23 Overall, older adults have a substantially higher case fatality rate as compared to younger individuals affected by COVID-19 (42% for those <65 vs 65% > 65 years).24 The results of this study showed that age was related to the duration of viral shedding. There was a significant positive correlation between disease duration and patient age in the asymptomatic group.25 It has been shown that nasopharyngeal/pharyngeal virus RNA shedding increases with age, whereas fecal virus RNA shedding decreases with age.26 These differences may be related to the age distribution of the included study population, and whether older age prolongs the NCT in covid-19 patients still needs further investigation.
Furthermore, at the time of a covid-19 outbreak, poor prognosis was related with having a comorbid factor. Hypertension is one of the most common risk factors for COVID-19 clinical progression. The possible key biological pathways include oxidative stress, ascorbate and aldarate metabolism, lipid metabolism, immune system and inflammation.27 Hypertension in our study was statistically different in the early NCT and late NCT group. By incorporating multivariate logistic regression equations with multivariate, we found hypertension was independent risk factor associated with the duration of SARS-COV-2 clearance. This is consistent with current studies.11,28
Participants who were infected with SARS-CoV-2 during the first year of the pandemic were more likely to experience poorer mental health.29 The prevalence of anxiety and depression is high among applicants in the Covid-19 pandemic.30 Interestingly, in this study, anxiety was associated with prolonged NCT, while depression was not. Recent studies have shown that pre-existing mental illness is a major risk factor for depression, anxiety and insomnia.31 Therefore, we suggest that while treating the respiratory symptoms of patients with new coronary pneumonia, attention should be paid to the patient’s mental health.
Furthermore, we analyzed Ct values for the first and lowest RT-PCR test (negatively associated with viral load). A high viral load at the time of first sampling was a predictor of severe infection and/or death in SARS-CoV-2 infected individuals of all age groups.32 Although we did not find the Ct value as an independent risk factor for prolonged NCT, the first nucleic acid ORF 1ab gene value and the N gene value were lower in the late NCT group compared with the early group (P =0.002, 0.001). This suggests that the higher the viral load, the longer the conversion time may be.
Our study has several limitations. First, this study was a single-center retrospective study, so the results may have been affected by population bias. Secondly, confounding factors were not controlled for in the subgroups of this study. Consequently, the findings of the study suggest an association between risk factors and prolonged NCT, but they do not provide unequivocal evidence to substantiate a causal relationship. Finally, some of the risk factors are not amenable to intervention. However, the real strength of this study lies in the sleep and mood studies conducted when examining clinical data in the Fangcang Shelter population.
Conclusions
This study demonstrated that age, hypertension, and anxiety were independent risk factors prolong the NCT in patients with COVID-19. Potential risk factors should be taken into consideration for the strategy of quarantining infected patients.
Ethical Approval
The authors confirm that all procedures undertaken in this study adhere to the ethical standards set by the appropriate national and institutional committees on human experimentation, as well as the Helsinki Declaration of 1975, with its 2008 revisions. The Ethics Committee of the Faculty of the First Affiliated Hospital of Army Military Medical University approved the protocol of this study(Approval number: (B)KY2022160). To maintain the principle of confidentiality, the data used were anonymized. A waiver of informed consent was granted as all anonymized data was collected retrospectively in accordance with the ethics approval.
Funding
There was no external funding for this article.
Disclosure
Qiuxia Chen and Xianhua Hou are co‐corresponding authors. We do not have any conflicts of interest associated with this publication. There was no significant financial support for this work that could have influenced its outcome.
References
1. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi:10.1016/S0140-6736(20)30627-9
2. Chen J, Wang R, Gilby NB, Wei GW. Omicron variant (B.1.1.529): infectivity, vaccine breakthrough, and antibody resistance. J Chem Inf Model. 2022;62(2):412–422. doi:10.1021/acs.jcim.1c01451
3. Tang JW, Toovey OTR, Harvey KN, Hui DDS. Introduction of the South African SARS-CoV-2 variant 501Y.V2 into the UK. J Infect. 2021;82(4):e8–e10. doi:10.1016/j.jinf.2021.01.007
4. Zhang X, Chen S, Zhang W. Shanghai’s life-saving efforts against the current omicron wave of the COVID-19 pandemic. Lancet. 2022;399(10340):2014.
5. Noureddine FY, Chakkour M, El Roz A, et al. The emergence of SARS-CoV-2 variant(s) and its impact on the prevalence of COVID-19 cases in the Nabatieh Region, Lebanon. Med Sci. 2021;9(2):40.
6. National Health Commission of the People’s Republic of China. Diagnostic and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 9). in chinese. 2022.
7. Fontana LM, Villamagna AH, Sikka MK, McGregor JC. Understanding viral shedding of severe acute respiratory coronavirus virus 2 (SARS-CoV-2): review of current literature. Infect Control Hosp Epidemiol. 2021;42(6):659–668. doi:10.1017/ice.2020.1273
8. Nadir Y, Kiran P. Risk factors for prolonged viral RNA shedding in patients with COVID-19; a nested case-control study. J Infect Dev Ctries. 2023;17(5):610–616. doi:10.3855/jidc.17508
9. Yu T, Dong J, Qi Q, et al. A nomogram for predicting delayed viral shedding in non-severe SARS-CoV-2 omicron infection. Infect Drug Resist. 2023;16:2487–2500. doi:10.2147/IDR.S407620
10. Arfijanto MV, Asmarawati TP, Bramantono B, et al. Duration of SARS-CoV-2 RNA shedding is significantly influenced by disease severity, bilateral pulmonary infiltrates, antibiotic treatment, and diabetic status: consideration for isolation period. Pathophysiology. 2023;30(2):186–198. doi:10.3390/pathophysiology30020016
11. Wen R, Li J, Chen F, et al. Effect of the renin-angiotensin-aldosterone system inhibitors on time to nucleic acid negative conversion in hypertensive patients with SARS-CoV-2 omicron infection: a propensity score matching study. Hypertens Res. 2025;48(1):273–283. doi:10.1038/s41440-024-01953-8
12. Zhu B, Xie M, Park CG, Kapella MC. Adaptation of the Pittsburgh sleep quality index in Chinese adults with type 2 diabetes. J Chin Med Assoc. 2018;81(3):242–247. doi:10.1016/j.jcma.2017.06.021
13. Soldatos CR, Paparrigopoulos TJ. Sleep physiology and pathology: pertinence to psychiatry. Int Rev Psychiatry. 2005;17(4):213–228. doi:10.1080/09540260500104565
14. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
15. Lin C, Tong Y, Bai Y, et al. Prevalence and correlates of depression and anxiety among Chinese international students in US colleges during the COVID-19 pandemic: a cross-sectional study. PLoS One. 2022;17(4):e0267081. doi:10.1371/journal.pone.0267081
16. Gao WJ, Li LM. Advances on presymptomatic or asymptomatic carrier transmission of COVID-19. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(4):485–488. doi:10.3760/cma.j.cn112338-20200228-00207
17. Lin P, Chen W, Huang H, et al. Delayed discharge is associated with higher complement C3 levels and a longer nucleic acid-negative conversion time in patients with COVID-19. Sci Rep. 2021;11(1):1233. doi:10.1038/s41598-021-81010-3
18. Gui H, Zhang Z, Chen B, et al. Development and validation of a nomogram to predict failure of 14-day negative nucleic acid conversion in adults with non-severe COVID-19 during the Omicron surge: a retrospective multicenter study. Infect Dis Poverty. 2023;12(1):7. doi:10.1186/s40249-023-01057-4
19. Liu W, Jin Y, Wu Y, et al. Factors influencing the time to COVID-19 antigen tests negative conversion among students at a Chinese university: a retrospective analysis. BMC Infect Dis. 2024;24(1):1443. doi:10.1186/s12879-024-10346-8
20. Yang Y, Liu Y, You Y, et al. Factors associated with negative conversion of viral RNA in hospitalized children infected with SARS-CoV-2 Omicron variant in Shanghai, China: a retrospective analysis. BMC Infect Dis. 2023;23(1):264. doi:10.1186/s12879-023-08223-x
21. Cai Y, Huang Z, Wu B, et al. Increased nutrition risk is associated with a prolonged negative conversion of viral RNA in children and adolescents with COVID-19. Nutr Clin Pract. 2023;38(5):1073–1081. doi:10.1002/ncp.10994
22. Gedik TE, Unal D, Suzan V, et al. The impact of COVID-19 pandemic on the geriatric inpatient unit. Curr Med Res Opin. 2023;39(2):259–265. doi:10.1080/03007995.2022.2148460
23. Miyashita K, Hozumi H, Furuhashi K, et al. Outcomes of COVID-19 in the Omicron-predominant wave: large-scale real-world data analysis with a comparison to influenza. Pneumonia. 2025;17(1):3. doi:10.1186/s41479-025-00158-y
24. Tisminetzky M, Delude C, Hebert T, Carr C, Goldberg RJ, Gurwitz JH. Age, multiple chronic conditions, and COVID-19: a literature review. J Gerontol a Biol Sci Med Sci. 2022;77(4):872–878. doi:10.1093/gerona/glaa320
25. Mori H, Obinata H, Murakami W, et al. Comparison of COVID-19 disease between young and elderly patients: hidden viral shedding of COVID-19. J Infect Chemother. 2021;27(1):70–75. doi:10.1016/j.jiac.2020.09.003
26. Vlaming-van Eijk LE, Ertugrul IA, Upasani V, et al. Temporal dynamics and (Para)clinical factors associated with (Long) viral RNA shedding in COVID-19 nonhospitalized individuals - The COVID-HOME study. J Med Virol. 2024;96(12):e70125. doi:10.1002/jmv.70125
27. Sánchez A, García-Pardo G, Martí A, et al. Omics for searching plasma biomarkers associated with unfavorable COVID-19 progression in hypertensive patients. Sci Rep. 2025;15(1):10343. doi:10.1038/s41598-025-94725-4
28. Zhang Y, Li Q, Duan H, et al. Machine learning based predictive modeling and risk factors for prolonged SARS-CoV-2 shedding. J Transl Med. 2024;22(1):1054. doi:10.1186/s12967-024-05872-7
29. Araújo N, Lopes C, Costa A, et al. Anxiety, depression, and poor sleep quality in two-year survivors of mild to severe SARS-CoV-2 infection and matched comparison groups. J Affect Disord. 2025;385:119344. doi:10.1016/j.jad.2025.05.004
30. Sensoy B, Gunes A, Ari S. Anxiety and depression levels in Covid-19 disease and their relation to hypertension. Clin Exp Hypertens. 2021;43(3):237–241. doi:10.1080/10641963.2020.1847132
31. Thaipisuttikul P, Awirutworakul T, Manatsathit M, Kaewpila W, Tiensuntisook S, Cheeveewat P. Depression, anxiety, insomnia, and quality of life in hospitalized COVID-19 patients. Acta Psychol. 2025;255:104935. doi:10.1016/j.actpsy.2025.104935
32. Ringlander J, Martner A, Huiqi L, et al. Influence of viral load on severity and mortality in COVID-19. Infect Dis. 2025:1–8. doi:10.1080/23744235.2025.2485274.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Pneumothorax in Critically Ill COVID-19 Patients: Prevalence, Analysis of Risk Factors and Clinical Outcomes
AlGhamdi Z, Alqahtani SY, AlDajani K, Alsaedi A, Al-Rubaish O, Alharbi A, Elbawab H
International Journal of General Medicine 2022, 15:8249-8256
Published Date: 21 November 2022
Pathogen Distribution, Drug Resistance Risk Factors, and Construction of Risk Prediction Model for Drug-Resistant Bacterial Infection in Hospitalized Patients at the Respiratory Department During the COVID-19 Pandemic
Wei XL, Zeng QL, Xie M, Bao Y
Infection and Drug Resistance 2023, 16:1107-1121
Published Date: 22 February 2023
Early Stage Risk Identification and Governance of Major Emerging Infectious Diseases: A Double-Case Study Based on the Chinese Context
Li X, Jiang H, Liang X
Risk Management and Healthcare Policy 2023, 16:635-653
Published Date: 7 April 2023
Perception and Impact of COVID-19 Pandemic in Psoriasis Patients: Data from the German PsoBest and the CoronaBest Registries
Valencia López MJ, Stephan B, Meineke A, Wolf S, Thaci D, Mrowietz U, Andrees V, Rustenbach SJ, Reich K, Thalmann L, Bogena H, Staubach P, von Kiedrowski RM, Augustin M
Psoriasis: Targets and Therapy 2024, 14:29-38
Published Date: 14 May 2024
Risk Factors and Nomogram Prediction Model for Healthcare-Associated Infections (HAIs) in COVID-19 Patients
Li Z, Li J, Zhu C, Jiao S
Infection and Drug Resistance 2024, 17:3309-3323
Published Date: 2 August 2024


