Back to Journals » Infection and Drug Resistance » Volume 18
Retrospective Analysis of Factors Influencing Clinical Outcomes of Revision Surgery for Periprosthetic Infection After Unicondylar Knee Arthroplasty
Authors Cao X, Zhao Z, Zhang C, Gao B, Dong R, Ma L
Received 14 January 2025
Accepted for publication 13 May 2025
Published 12 June 2025 Volume 2025:18 Pages 2977—2986
DOI https://doi.org/10.2147/IDR.S517567
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandip Patil
Xuyang Cao,1 Zizi Zhao,2 Cheng Zhang,3 Bo Gao,1 Ruifang Dong,2 Lijie Ma1
1Trauma Center, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, People’s Republic of China; 2Department of Orthopedics, North China Medical and Health Group Xingtai General Hospital, Xingtai, Hebei, People’s Republic of China; 3Department of Orthopedics, The First Central Hospital of Baoding City, Baoding, Hebei, People’s Republic of China
Correspondence: Lijie Ma, Trauma Center, The Third Hospital of Hebei Medical University, No. 102 Youyi North Street, Qiaoxi District, Shijiazhuang, Hebei, 050000, People’s Republic of China, Tel +86-17733299114, Email [email protected]
Objective: To identify factors influencing clinical outcomes of revision surgery for periprosthetic joint infection (PJI) after unicondylar knee arthroplasty (UKA).
Methods: This retrospective study included 40 patients who underwent UKA revision for PJI (May 2009–May 2023). Patients were divided into responders (n=27, favorable outcomes: no infection, KSS ≥ 80, HSS ≥ 85 at 6 months) and non-responders (n=13, suboptimal outcomes: persistent infection or KSS < 80/HSS < 85). Inflammatory markers (CRP, WBC), Knee Society Score (KSS), and Hospital for Special Surgery (HSS) score were assessed. Multivariate logistic regression identified predictors of success.
Results: Non-responders had higher rates of diabetes (46.2% vs 14.8%), smoking (30.8% vs 18.5%), alcohol use (23.1% vs 14.8%), Gram-positive infections (30.8% vs 11.1%), and deep infections (84.6% vs 22.2%, all P< 0.05). Key predictors of success included optimal antibiotic management (OR=1.33, 95% CI=1.02– 1.74), patient compliance (OR=1.44, 95% CI=1.08– 1.92), and absence of diabetes (OR=1.54, 95% CI=1.24– 1.98), smoking (OR=1.60, 95% CI=1.08– 2.37), or Gram-positive infections (OR=1.46, 95% CI=1.12– 1.90, all P< 0.05).
Conclusion: Diabetes, smoking, alcohol use, Gram-positive infections, deep infection, antibiotic management, and compliance significantly impact UKA revision outcomes. Smoking showed the strongest association (OR=1.60). Clinicians should prioritize preoperative optimization (glycemic control, smoking cessation) and protocol-driven antibiotic use. Findings are exploratory due to small sample size and require validation in larger cohorts.
Keywords: unicondylar knee arthroplasty, periprosthetic infection, revision surgery, clinical outcomes, influencing factors
Introduction
Unicondylar knee arthroplasty (UKA) is a widely utilized surgical procedure for the treatment of localized knee joint diseases, particularly in instances where osteoarthritis affects only one compartment of the knee. In comparison to total knee arthroplasty (TKA), UKA presents several benefits, such as minimally invasive techniques, accelerated recovery times, and enhanced preservation of the natural kinematics of the knee.1–3 Notably, while periprosthetic joint infection (PJI) is a recognized complication in both UKA and TKA, UKA-specific PJIs may differ in characteristics: UKA preserves more native joint structures and involves smaller incisions, which might alter infection pathways, pathogen distribution, or response to treatment compared to TKA, where the entire joint is replaced.4 Nevertheless, PJI continues to be a significant and debilitating complication subsequent to UKA, exerting substantial influence on patient outcomes and quality of life.5
PJI is an infrequent yet severe complication that requires intricate treatment strategies, encompassing prolonged antibiotic therapy and frequently necessitating revision surgery.6,7 Surgical revision of prosthetic joint infection (PJI) typically entails the removal of the infected prosthesis, meticulous debridement of infected tissues, and reimplantation of a new prosthesis, sometimes incorporating antibiotic-impregnated spacers to eradicate the infection.8–10 It is essential to comprehend the determinants that impact the success of these revision procedures in order to optimize treatment protocols and enhance patient prognoses.
Previous studies have identified numerous factors that may influence the outcome of revision surgeries for PJI, including the patient’s overall health status, comorbidities such as diabetes, smoking habits, specific surgical techniques employed, and postoperative care management, including antibiotic regimens.11,12 These findings are primarily derived from TKA or total hip arthroplasty (THA) cohorts,13 yet whether these factors apply to UKA remains unclear due to UKA’s distinct anatomical preservation, patient selection criteria (eg, younger patients with less comorbidity), and unique infection kinetics (eg, higher early postoperative infection rates but lower long-term recurrence compared to TKA).4 Significantly, individuals with diabetes face an elevated susceptibility to infections as a result of compromised immune responses and impaired wound healing associated with chronic hyperglycemia.14,15 Similarly, lifestyle factors such as tobacco use and alcohol consumption have been demonstrated to detrimentally impact surgical outcomes through the impairment of vascular function and immune response.16–18
We hypothesize that the clinical efficacy of revision surgery for UKA-associated PJI is influenced by a combination of infection-related factors (type/severity), antibiotic management, patient-related factors (underlying diabetes, smoking/drinking habits), and postoperative care (compliance, monitoring). This study aims to retrospectively analyze the outcomes of revision surgeries in patients who developed periprosthetic joint infection (PJI) after unicompartmental knee arthroplasty (UKA), with a focus on identifying key factors influencing clinical efficacy. Through the utilization of multivariate logistic regression analysis, we systematically assess the impact of infection type and severity, antibiotic management, patient compliance with medical advice, and postoperative care on the success of revision surgeries. While prior research has explored PJI revision factors in TKA,11,12 the unique anatomical and clinical characteristics of UKA (eg, preserved cruciate ligaments, smaller prosthetic volume) necessitate an independent evaluation of these factors in the UKA population. Thus, this study addresses an unmet need by providing UKA-specific evidence to guide tailored treatment strategies. The findings are anticipated to offer insights for developing more effective prevention and treatment strategies, ultimately enhancing postoperative prognosis. By elucidating these determinants, this research deepens understanding of postoperative management and underscores the importance of a comprehensive approach encompassing meticulous surgical technique, rigorous infection control, and proactive patient lifestyle management.
Materials and Methods
This study was conducted at Trauma Center, the Third Hospital of Hebei Medical University, and adhered to the Declaration of Helsinki. Ethical approval was obtained from the institutional review board (IRB No. 23-TJH-0226). Informed consent was waived because the research was retrospective and conducted on anonymized data.
General Information
Between May 2009 and May 2023, a total of 40 patients who experienced periprosthetic infection following unicondylar joint replacement and required revision surgery were enrolled as the study cohort. Given the retrospective nature of this study, patients were identified from the hospital’s electronic medical records, with inclusion restricted to those with complete clinical, laboratory, and imaging data. Subsequent to the surgical intervention, these patients were stratified into a “responders” (favorable revision outcomes, n=27) and a “non-responders” (suboptimal or persistent infection/functional limitations, n=13), based on predefined objective criteria (detailed in Section 1.2.3).
Admission Criteria
- Age range: 40 to 80 years, ensuring inclusion of patients within the typical age demographic for joint replacement;
- Patients with a history of unicondylar joint replacement;
- Revision surgery required for periprosthetic infection;
- A minimum of 6 months post-initial replacement procedure to exclude early postoperative complications (defined as infections occurring within 90 days of primary UKA, consistent with the Musculoskeletal Infection Society [MSIS] criteria).19
- For survival analysis, patients were censored at the time of the last follow-up if they had not experienced a failure event (eg, revision for recurrent PJI or persistent functional limitations) by the end of the study period.
Exclusion Criteria
- Patients with severe cardiovascular and cerebrovascular diseases, renal insufficiency, or other chronic conditions that may impact surgical safety and recovery;
- Patients with active infections in other areas (eg, lung or urinary system infections), which could potentially confound the assessment of infection treatment efficacy;
- Patients with immune compromised status (eg, HIV, chemotherapy);
- Patients with a history of prior revision surgery;
- Patients lacking capacity to comprehend the research content (excluded due to inability to provide informed consent or reliable self-reported outcomes, such as pain scores, critical for clinical assessments).
Methods
Observation of Postoperative Inflammatory Laboratory Indicators
(1) Following surgery, peripheral blood routine and C-reactive protein (CRP) levels were assessed. For the blood routine test, 3mL of fasting venous blood was collected from each subject using the Mindray CAL-8000 blood analysis assembly line instrument. Strict aseptic procedures were followed during sample collection, and the samples were placed into vacuum anticoagulant tubes for routine detection of white blood cell (WBC) count, neutrophil percentage, and platelet count. Additionally, 3mL of venous blood was collected for whole-blood CRP testing using the Mindray CAL-8000 via the latex-enhanced immune scattering turbidity method. Erythrocyte sedimentation rate (ESR) was also measured using the Westergren method to further assess infection severity.
(2) Postoperative monitoring included observation of body temperature changes, incision swelling, and signs of skin infection (eg, erythema, purulent discharge). Infection severity was classified based on MSIS criteria: probable PJI required ≥3 of the following: elevated CRP (>10 mg/L) or ESR (>30 mm/h), elevated WBC or neutrophil percentage, positive joint fluid culture, or sinus tract communication with the prosthesis.19
KSS and HSS Scores
The Knee Society Score (KSS)20 was used to estimate pain and functional status. KSS comprises two components: a function score (max 100, assessing walking distance and stair climbing) and a pain score (max 100, based on patient-reported pain). Higher scores indicate better function and less pain. The Hospital for Special Surgery (HSS)21 score evaluated overall recovery, incorporating pain, functional activity, muscle strength, and range of motion (total 100 points, higher scores indicating better recovery). Baseline KSS and HSS scores were collected preoperatively. Six months postoperatively, scores were assessed by two trained orthopedic surgeons (inter-rater reliability confirmed via κ=0.82 for KSS and κ=0.79 for HSS).
Clinical Treatment Effect Analysis
The primary outcome for regression analysis was revision success, defined as: (1) absence of clinical infection (no fever, no sinus tract, normal CRP/ESR) at 6 months; (2) KSS function score ≥80 and pain score ≥85; and (3) HSS score ≥85. Secondary outcomes included infection recurrence (≥1 positive culture or clinical signs of infection at 6 months) and functional improvement. Additional efficacy categories were defined as follows:
- Significant improvement: Pain scores reduced by >75%, functional scores increased by >50%, with no residual infection signs.
- Moderate improvement: Pain scores reduced by 50–75%, functional scores increased by 30–50%, with no active infection.
- Mild improvement: Pain scores reduced by 25–50%, functional scores increased by 10–30%, with controlled but not resolved infection.
- Failure: Pain scores reduced by <25%, functional scores increased by <10%, or persistent infection.
Causative organisms were identified via intraoperative synovial fluid cultures (aerobic, anaerobic, and fungal) during revision surgery. Antibiotic regimens were tailored to culture results: 27 patients received 4–6 weeks of intravenous (IV) antibiotics (eg, vancomycin 15 mg/kg q12h, cefazolin 2 g q8h) followed by 3 months of oral suppression (eg, ciprofloxacin 500 mg bid); 13 patients with multi-drug resistant (MDR) organisms (eg, methicillin-resistant Staphylococcus aureus [MRSA]) received extended IV therapy (6–8 weeks) with linezolid or daptomycin.22
All revision surgeries were performed by two senior orthopedic surgeons using a standardized two-stage protocol: stage 1 involved prosthesis removal, debridement, and placement of antibiotic-impregnated spacers; stage 2 (4–6 weeks later) involved reimplantation of a new prosthesis after infection resolution (normal CRP/ESR, negative cultures). One-stage revision was not performed in this cohort.
Statistical Analysis
A post-hoc power analysis was conducted using G*Power 3.1, assuming α=0.05, power=0.8, and a medium effect size (OR=2.0). With 40 patients (13 in the failure group), the study had 62% power to detect significant predictors, indicating potential underpowering. Categorical data were analyzed using χ² testing, and continuous data are presented as mean ± standard deviation (SD). Univariate analysis (t-test for continuous variables, Fisher’s exact test for categorical variables) was performed first, with variables showing P <0.10 included in multivariate logistic regression. Analysis was conducted using GraphPad Prism 9.0, with results reported as mean ± SEM. A significance level of P <0.05 was used for statistical inference.
Results
General Data Analysis
Patient ages ranged from 41 to 76 years, with a mean age of 62.45±7.33 years. There were 22 male and 18 female patients. In responders, the male-to-female ratio was 16:11 (59%:41%), with a mean age of 62.55±6.41 years and mean BMI of 22.35±1.88 kg/m². This group included 5 smokers (18.5%), 4 drinkers (14.8%), 9 hypertensive patients (33.3%), and 4 with diabetes (14.8%).
In non-responders, the male-to-female ratio was 6:7 (46%:54%), with a slightly lower mean age of 61.49±15.11 years and higher mean BMI of 23.67±2.12 kg/m². This group included 4 smokers (30.8%), 3 drinkers (23.1%), 4 hypertensive patients (30.8%), and 6 with diabetes (46.2%). Baseline characteristics (sex, age, BMI, hypertension) were comparable between groups (P>0.05), while non-responders had higher proportions of smoking, drinking, and diabetes (P<0.05). (Table 1)
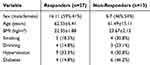 |
Table 1 Baseline Patient Characteristics |
Peripheral Blood Routine and C-Reactive Protein Postoperatively
Postoperative peripheral blood routine and CRP levels were significantly lower in non-responders compared to responders (P<0.05). Specifically, responders had higher mean CRP (25.17±2.14 mg/L vs 16.85±0.52 mg/L), neutrophil percentage (72.25±3.26% vs 62.82±2.12%), platelet count (259.36±12.87×109/L vs 181.63±10.35×109/L), and white blood cell count (17.35±1.46×109/L vs 12.54±0.87×109/L). (Table 2)
 |
Table 2 Postoperative Blood Markers |
Postoperative Body Temperature, Incision Swelling, and Skin Infection
Non-responders exhibited lower mean body temperature (37.12±0.35°C vs 38.65±0.59°C), reduced incision swelling (38.5% vs 74.1%), and fewer skin infections (23.1% vs 66.7%) compared to responders (P<0.05) (Table 3).
 |
Table 3 Postoperative Clinical Signs |
Knee Society Score (KSS)
Preoperative KSS scores were comparable between groups (P>0.05). Postoperatively, responders had significantly higher KSS scores (87.36±5.27 vs 74.59±4.35, P<0.05) (Table 4).
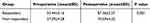 |
Table 4 Knee Society Score (KSS) |
Hospital for Special Surgery (HSS) Score
Preoperative HSS scores were similar between groups (P>0.05). Postoperatively, responders had significantly higher HSS scores (90.54±6.37 vs 77.32±5.45, P<0.05) (Table 5).
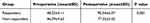 |
Table 5 Hospital for Special Surgery (HSS) Score |
Clinical Treatment Effect Analysis
Treatment efficacy was categorized as “significant”, “moderate”, “mild”, or “failure.” Responders showed 9 significant (33.3%), 14 moderate (51.9%), and 4 mild (14.8%) improvements, with no failures. Non-responders had 1 moderate (7.7%), 10 mild (76.9%), and 1 failure (7.7%), with significantly lower overall efficacy (P<0.05) (Table 6).
 |
Table 6 Clinical Treatment Efficacy |
Clinical Characteristics of Patients
Significant differences were observed between responders and non-responders in infection type (Gram-positive bacteria: 11.1% vs 30.8%; fungi: 7.4% vs 23.1%), infection depth (superficial: 77.8% vs 15.4%; deep: 22.2% vs 84.6%), antibiotic management (66.7% vs 38.5%), compliance (74.1% vs 46.2%), and postoperative monitoring (63.0% vs 23.1%) (P<0.05) (Table 7).
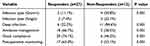 |
Table 7 Clinical Characteristics by Group |
Factors Affecting Postoperative Treatment Effect
Multivariate logistic regression analysis identified significant predictors of successful revision surgery (Table 8). Diabetes (OR=1.54, 95% CI=1.24–1.98, P=0.009), smoking (OR=1.60, 95% CI=1.08–2.37, P=0.026), alcohol use (OR=1.50, 95% CI=1.05–2.15, P=0.003), Gram-positive infections (OR=1.46, 95% CI=1.12–1.90, P=0.004), infection severity (OR=1.51, 95% CI=1.10–2.07, P=0.015), antibiotic management (OR=1.33, 95% CI=1.02–1.74, P=0.037), and patient compliance (OR=1.44, 95% CI=1.08–1.92, P=0.017) were significant predictors of treatment success (P<0.05). In contrast, postoperative monitoring (OR=1.40, 95% CI=0.95–2.06, P=0.083), elderly status (OR=1.39, 95% CI=0.88–2.20, P=0.160), and obesity (OR=1.42, 95% CI=0.92–2.19, P=0.112) showed no statistically significant association with treatment success, as their confidence intervals included 1.
 |
Table 8 Multivariate Logistic Regression: Predictors of Treatment Success |
Discussion
UKA offers substantial advantages in preserving knee function and expediting recovery compared to TKA.23–25 However, PJI remains a critical complication, significantly impacting postoperative recovery and quality of life.26 Our study identified key predictors of successful revision surgery for PJI after UKA, including patient-related factors (diabetes, smoking, alcohol use), infection characteristics (Gram-positive pathogens, deep infection), and clinical management (antibiotic use, patient compliance). Below, we contextualize these findings within existing literature, explore underlying mechanisms, and propose actionable clinical recommendations.
Patient-Related Factors: Diabetes, Smoking, and Alcohol Use
Non-responders (suboptimal outcomes) had higher proportions of diabetes (46.2% vs 14.8%, P<0.05), smoking (30.8% vs 18.5%, P<0.05), and alcohol use (23.1% vs 14.8%, P<0.05). Multivariate analysis confirmed these as significant predictors of failure: diabetes (OR=1.54, P=0.009), smoking (OR=1.60, P=0.026), and alcohol use (OR=1.50, P=0.003). These findings align with other reports where diabetes impairs immune function via chronic hyperglycemia and microvascular damage, with increased PJI risk.27 Smoking, which reduces tissue oxygenation by 20–30% and impairs neutrophil function,28 and alcohol use, which disrupts cytokine balance and macrophage activity,29 similarly elevate infection risk. Our results emphasize the need for preoperative optimization: strict glycemic control (HbA1c <7%), smoking cessation programs, and alcohol reduction counseling to mitigate these risks.
Infection Characteristics: Gram-Positive Pathogens and Deep Infection
Non-responders had higher rates of Gram-positive infections (30.8% vs 11.1%, P=0.001) and deep infections (84.6% vs 22.2%, P=0.001), with multivariate analysis linking both to failure (Gram-positive: OR=1.46, P=0.004; deep infection: OR=1.51, P=0.015). This mirrors TKA studies where Gram-positive bacteria (eg, Staphylococcus aureus) form biofilms resistant to antibiotics and host defenses,30 and deep PJI (involving bone/implant) evades debridement, increasing recurrence.31 Our results underscore the importance of early, aggressive intervention: synovial fluid culture to identify pathogens, imaging (eg, MRI) to assess infection depth, and biofilm-targeted debridement (eg, high-pressure irrigation) for deep infections.
Clinical Management: Antibiotic Use and Patient Compliance
Responders had better antibiotic management (66.7% vs 38.5%, P=0.001) and compliance (74.1% vs 46.2%, P=0.001), with multivariate analysis confirming these as success predictors (antibiotic management: OR=1.33, P=0.037; compliance: OR=1.44, P=0.017). These findings align with a recent TKA trial by Liu et al, where protocol-driven antibiotic use (targeted vancomycin based on local epidemiology, combined with cefazolin) reduced PJI recurrence from 7.89% to 3.13% (a 60.3% reduction), emphasizing the importance of tailoring antibiotics to culture results.32 Similarly, structured compliance programs, as shown by Han et al, improved functional outcomes by enhancing adherence to wound care and rehabilitation—patients with >15 supervised rehabilitation sessions had 18.5-fold higher odds of successful return to sport compared to non-adherent individuals, underscoring the value of structured protocols.33 Our data suggest that standardized antibiotic protocols (eg, 4–6 weeks of IV therapy followed by oral suppression) and patient education (eg, written care plans, follow-up reminders) are critical for success.
Postoperative Monitoring, Age, and Obesity: Non-Significant but Context-Dependent
While clinical characteristics showed responders had higher postoperative monitoring rates (63.0% vs 23.1%, P=0.001), multivariate analysis found no significant association (OR=1.40, P=0.083). This likely reflects small sample size (n=13 non-responders), limiting statistical power. Similarly, elderly status (OR=1.39, P=0.160) and obesity (OR=1.42, P=0.112) were not significant, possibly due to UKA’s selection bias toward younger, less obese patients—Thompson et al reported that UKA is often reserved for younger patients (<60 years) with lower BMI (<35 kg/m²), as higher BMI and older age correlate with poorer functional outcomes.34 These results caution against extrapolating TKA risk factors, where age and obesity are significant: Bonasia et al identified obesity (BMI > 30) as a key driver of TKA complications, including increased infection, loosening, and revision rates.35
Inflammatory Markers and Functional Outcomes: A Double-Edged Sword
Responders had higher postoperative CRP (25.17 vs 16.85 mg/L, P=0.001), neutrophil percentage (72.25% vs 62.82%, P=0.001), and WBC (17.35 vs 12.54×109/L, P=0.001). This may reflect more active infection at baseline, but responders’ better functional scores (KSS: 87.36 vs 74.59; HSS: 90.54 vs 77.32, P<0.05) suggest aggressive treatment (eg, targeted antibiotics, debridement) successfully controlled inflammation. These findings validate the utility of KSS and HSS scores in capturing clinically meaningful recovery, as demonstrated by Karaca et al in a UKA cohort: KSS improved from 65.2 to 91.4 (P<0.05), and HSS from 67.5 to 89.9 (P<0.05), confirming their sensitivity to postoperative improvements.36
Study Limitations and Future Directions
Our study has several limitations. The small sample size (n=40) and retrospective design limit generalizability and causal inference. Follow-up (6 months) may not capture late recurrence, and residual confounding (eg, unmeasured comorbidities) is possible. Future studies should use larger, prospective cohorts (eg, multi-center registries) to validate these predictors and explore mechanisms (eg, diabetes-related biofilm tolerance).
Conclusion
Successful revision surgery for PJI after UKA is influenced by patient-related factors (diabetes, smoking, alcohol), infection characteristics (Gram-positive pathogens, deep infection), and clinical management (antibiotic use, compliance). Actionable recommendations include : (1) preoperative optimization of diabetes (HbA1c < 7%), smoking cessation, and alcohol reduction; (2) routine synovial fluid culture and imaging to guide antibiotic selection and debridement depth; (3) structured compliance programs with written care plans and follow-up reminders; and (4) biofilm-targeted debridement for deep infections. These strategies may improve outcomes and patient quality of life.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study protocol was approved by the Ethics Committee of The Third Hospital of Hebei Medical University (NO. 23-TJH-0226), and the study was performed in accordance with the Helsinki II declaration. Informed consent was waived because the research was retrospective and conducted on anonymized data.
Funding
This study was supported by the Natural Science Foundation of Hebei Province (No. H2022206362).
Disclosure
The authors declare that they have no competing interests.
References
1. Jensen CB, Petersen PB, Jørgensen CC, et al. Length of stay and 90-day readmission/complication rates in unicompartmental versus total knee arthroplasty: a propensity-score-matched study of 10,494 procedures performed in a fast-track setup. JBJS. 2021;103(12):1063–1071. doi:10.2106/JBJS.20.01287
2. Tay ML, Monk A, Frampton CM, Hooper GJ, Young SW. A comparison of clinical thresholds for revision following total and unicompartmental knee arthroplasty: a retrospective study of propensity-matched patients from the New Zealand Joint Registry. The Bone & Joint Journal. 2023;105(3):269–276. doi:10.1302/0301-620X.105B3.BJJ-2022-0872.R2
3. Maritan G, Franceschi G, Nardacchione R, et al. Similar survivorship at the 5-year follow-up comparing robotic-assisted and conventional lateral unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2023;31(3):1063–1071. doi:10.1007/s00167-022-07218-6
4. Yamagami R, Inui H, Jo T, et al. Unicompartmental knee arthroplasty is associated with lower proportions of surgical site infection compared with total knee arthroplasty: a retrospective nationwide database study. The Knee. 2021;28:124–130. doi:10.1016/j.knee.2020.11.017
5. Chiu AK, Malyavko A, Das A, et al. Diagnostic and invasive colonoscopy are not risk factors for revision surgery due to periprosthetic joint infection. J Arthroplasty. 2023;38(8):1591–1596. doi:10.1016/j.arth.2023.02.019
6. Zambianchi F, Seracchioli S, Franceschi G, et al. Image-based robotic-arm assisted unicompartmental knee arthroplasty provides high survival and good-to-excellent clinical outcomes at minimum 10 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2023;31(12):5477–5484. doi:10.1007/s00167-023-07599-2
7. Zanirato A, Cavagnaro L, Chiarlone F, Quarto E, Formica M. Periprosthetic joint infection in unicompartmental knee arthroplasty: treatment options and outcomes. What is the current evidence in literature? Arch Orthop Trauma Surg. 2022;143(2):1031–1039. doi:10.1007/s00402-022-04414-4
8. Zambianchi F, Daffara V, Franceschi G, Banchelli F, Marcovigi A, Catani F. Robotic arm-assisted unicompartmental knee arthroplasty: high survivorship and good patient-related outcomes at a minimum five years of follow-up. Knee Surg Sports Traumatol Arthrosc. 2021;29:3316–3322. doi:10.1007/s00167-020-06198-9
9. Mohammad HR, Judge A, Murray DW. The influence of surgeon caseload and usage on the long-term outcomes of mobile-bearing unicompartmental knee arthroplasty: an analysis of data from the national joint registry for England, Wales, Northern Ireland, and the Isle of Man. J Arthroplasty. 2023;38(2):245–251. doi:10.1016/j.arth.2022.08.011
10. Tay ML, Matthews BG, Monk AP, Young SW. Disease progression, aseptic loosening and bearing dislocations are the main revision indications after lateral unicompartmental knee arthroplasty: a systematic review. J ISAKOS. 2022;7(5):132–141. doi:10.1016/j.jisako.2022.06.001
11. Slaven SE, Cody JP, Sershon RA, Ho H, Pper RH, Fricka KB. Alignment in medial fixed-bearing unicompartmental knee arthroplasty: the limb has a leg up on the component. J Arthroplasty. 2021;36(12):3883–3887. doi:10.1016/j.arth.2021.08.015
12. Salman LA, Abudalou A, Khatkar H, et al. Impact of age on unicompartmental knee arthroplasty outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2023;31(3):986–997. doi:10.1007/s00167-022-07132-x
13. Mekkawy KL, Rodriguez HC, Pannu TS, Rowland RJ, Roche MW, Corces A. Morbidly obese patients undergoing unicompartmental knee arthroplasty compared to total knee arthroplasty: a retrospective case-controlled analysis. J Arthroplasty. 2023;38(12):2510–2516.e2511. doi:10.1016/j.arth.2023.05.093
14. Cavagnaro L, Chiarlone F, Mosconi L, Zanirato A, Formica M, Burastero G. Two-stage revision for periprosthetic joint infection in unicompartmental knee arthroplasty: clinical and radiological results. Arch Orthop Trauma Surg. 2022;142(8):2031–2038. doi:10.1007/s00402-022-04464-8
15. Klasan A, Tay ML, Frampton C, Young SW. High usage of medial unicompartmental knee arthroplasty negatively influences total knee arthroplasty revision rate. Knee Surg Sports Traumatol Arthrosc. 2022;30(9):3199–3207. doi:10.1007/s00167-021-06650-4
16. D’Ambrosi R, Ursino C, Mariani I, Ursino N, Formica M, Chen AF. Clinical outcomes, complications, and survivorship for unicompartmental knee arthroplasty versus total knee arthroplasty in patients aged 80 years and older with isolated medial knee osteoarthritis: a matched cohort analysis. Arch Orthop Trauma Surg. 2023;143(10):6371–6379. doi:10.1007/s00402-023-04916-9
17. Alayane A, Moussa MK, Boushnak MO, Boulazaib I, Nicolas N. septic metallosis after unicompartmental knee replacement: a case report and literature review. J Orthop Case Rep. 2023;13(6):11. doi:10.13107/jocr.2023.v13.i06.3676
18. Kahan ME, Chen Z, Angerett NR, et al. Unicompartmental knee arthroplasty has lower infection, conversion, and complication rates compared to high tibial osteotomy. J Knee Surg. 2022;35(14):1518–1523. doi:10.1055/s-0042-1757597
19. Fillingham YA, Della Valle CJ, Suleiman LI. Definition of successful infection management and guidelines for reporting of outcomes after surgical treatment of periprosthetic joint infection: from the workgroup of the musculoskeletal infection society (MSIS). J Bone Joint Surg Am Vol. 2019;101(14):e69. doi:10.2106/JBJS.19.00062
20. Scuderi GR, Bourne RB, Noble PC, Benjamin JB, Lonner JH, Scott W. The new knee society knee scoring system. Clin Orthop Relat Res. 2012;470(1):3–19. doi:10.1007/s11999-011-2135-0
21. Narin S, Unver B, Bakirhan S, Bozan O, Karatosun V. Cross-cultural adaptation, reliability and validity of the Turkish version of the Hospital for Special Surgery (HSS) Knee Score. Acta orthopaedica et traumatologica turcica. 2014;48(3):241–248. doi:10.3944/AOTT.2014.3109
22. Ahmed SS, Begum F, Kayani B, Haddad FS. Risk factors, diagnosis and management of prosthetic joint infection after total Hip arthroplasty. Expert Rev Med Devices. 2019;16(12):1063–1070. doi:10.1080/17434440.2019.1696673
23. Craik JD, El Shafie SA, Singh VK, Twyman RS. Revision of unicompartmental knee arthroplasty versus primary total knee arthroplasty. J Arthroplasty. 2015;30(4):592–594. doi:10.1016/j.arth.2014.10.038
24. Plate J, Mofidi A, Bao B, et al. Unicompartmental knee arthroplasty: past, present, future. Reconstructive Rev. 2012;2(1). doi:10.15438/rr.v2i2.15
25. Bert JM, Hooper J, Moen S. Outpatient total joint arthroplasty. Curr rev musculoskeletal med. 2017;10:567–574. doi:10.1007/s12178-017-9451-2
26. Ren X, Ling L, Qi L, et al. Patients’ risk factors for periprosthetic joint infection in primary total Hip arthroplasty: a meta-analysis of 40 studies. BMC Musculoskelet Disord. 2021;22:1–17. doi:10.1186/s12891-021-04647-1
27. Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD. Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS One. 2016;11(3):e0150866. doi:10.1371/journal.pone.0150866
28. Jensen JA, Goodson WH, Hopf HW, Hunt TK. Cigarette smoking decreases tissue oxygen. Arch Surg. 1991;126(9):1131–1134. doi:10.1001/archsurg.1991.01410330093013
29. Mendenhall CL, Theus SA, Roselle GA, Grossman CJ, Rouster SD. Biphasic in vivo immune function after low- versus high-dose alcohol consumption. Alcohol. 1997;14(3):255–260. doi:10.1016/S0741-8329(96)00150-4
30. Guo Y, Song G, Sun M, Wang J, Wang Y. Prevalence and therapies of antibiotic-resistance in staphylococcus aureus. Front Cell Infect Microbiol. 2020;10(107). doi:10.3389/fcimb.2020.00107
31. Doub JB, Parmiter D, Brantner CA, et al. The location of biofilms on chronic prosthetic joint infections and the ramifications for clinical practice. Arthroplasty Today. 2024;25:101314. doi:10.1016/j.artd.2023.101314
32. Liu C, Kakis A, Nichols A, Ries MD, Vail TP, Bozic KJ. Targeted use of vancomycin as perioperative prophylaxis reduces periprosthetic joint infection in revision TKA. Clin Orthopaedics Related Res. 2014;472(1):227–231.
33. Han F, Banerjee A, Shen L, Krishna L. Increased compliance with supervised rehabilitation improves functional outcome and return to sport after anterior cruciate ligament reconstruction in recreational athletes. Orthop J Sports Med. 2015;3(12):2325967115620770. doi:10.1177/2325967115620770
34. Thompson SA, Liabaud B, Nellans KW, Geller JA. Factors associated with poor outcomes following unicompartmental knee arthroplasty: redefining the “classic” indications for surgery. J Arthroplasty. 2013;28(9):1561–1564. doi:10.1016/j.arth.2013.02.034
35. Bonasia DE, Palazzolo A, Cottino U, et al. Modifiable and nonmodifiable predictive factors associated with the outcomes of total knee arthroplasty. Joints. 2019;7(1):13–18. doi:10.1055/s-0039-1678563
36. Karaca S, Erdem MN, Oztermeli A, Bal E, Gogus A, Hamzaoglu A. Clinical and radiological results of oxford phase-3 medial unicompartmental knee arthroplasty. Cureus. 2019;11(11):e6070. doi:10.7759/cureus.6070
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

