Back to Journals » Infection and Drug Resistance » Volume 18
Risk Factors for Development and Mortality of Carbapenem-Resistant Pseudomonas aeruginosa Bloodstream Infection in a Chinese Teaching Hospital: A Seven-Year Retrospective Study
Authors Dong L, Huang Y, Zhang S, Xu B, Li B, Cao Y
Received 24 October 2024
Accepted for publication 30 January 2025
Published 18 February 2025 Volume 2025:18 Pages 979—991
DOI https://doi.org/10.2147/IDR.S495240
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Sandip Patil
Luyan Dong,1,* Yingbin Huang,2,3,* Shengcen Zhang,1 Binbin Xu,1 Bin Li,1 Yingping Cao1
1Department of Clinical Laboratory, Fujian Medical University Union Hospital, Fuzhou, 350001, People’s Republic of China; 2Department of Pharmacy, Fujian Medical University Union Hospital, Fuzhou, 350001, People’s Republic of China; 3The School of Pharmacy, Fujian Medical University, Fuzhou, 350004, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yingping Cao; Bin Li, Email [email protected]; [email protected]
Objective: Pseudomonas aeruginosa (P. aeruginosa) is a gram-negative opportunistic pathogen, which can cause acute and chronic infections, often resulting in high mortality. The aim of this study was to investigate the risk factors for the development and mortality of patients with carbapenem-resistant P. aeruginosa bloodstream infection (CRPA BSI).
Methods: A total of 112 patients with CRPA BSI and 112 patients with carbapenem-sensitive P. aeruginosa (CSPA) BSI were included from a Chinese teaching hospital from January 2017 to December 2023 in this retrospective cohort study. The detection rate, antimicrobial susceptibility of P. aeruginosa and clinical characteristics of these patients were investigated. Multivariable logistic regression analysis was used to identify risk factors for the development and outcomes of CRPA BSI.
Results: In the past 7 years, 7480 blood samples of P. aeruginosa were cultured in the hospital. The detection rates of CRPA, multidrug resistant P. aeruginosa (MDRPA), and difficult-to-treat resistant P. aeruginosa (DTRPA) BSI increased annually (26% to 47%, 10% to 36% and 5% to 15%, respectively). CRPA showed high resistance to conventional antibiotics. Chronic lung disease (OR 3.953, 95% CI 1.131– 13.812), transplantation (OR 2.837, 95% CI 1.036– 7.770), multi-organ failure (OR 4.815, 95% CI 1.949– 11.894), pre-infection within CRPA (OR 9.239, 95% CI 3.441– 24.803), and exposure to carbapenems within 90 days (OR 2.734, 95% CI 1.052 − 7.106) were independent risk factors for the development of CRPA bacteremia. Sepsis or septic shock (OR 8.774, 95% CI 3.140– 24.515, p = 0.001) were independent risk factors of mortality.
Conclusion: Chronic lung disease, transplantation, multi-organ failure, prior CRPA infection, and prior carbapenems exposure are independent risk factors for the development of CRPA bacteremia. Sepsis or septic shock increases 28-day mortality. To investigate the molecular mechanisms of carbapenem-resistance of P. aeruginosa, standardize antibiotic usage, and assess risk factors for the development and mortality of CRPA BSI are beneficial to control infection and reduce death.
Keywords: Pseudomonas aeruginosa, bloodstream infection, carbapenem-resistance, risk factors, mortality
Introduction
Pseudomonas aeruginosa (P. aeruginosa) is a gram-negative opportunistic pathogen that can cause acute and chronic infections in patients with cancer, cystic fibrosis, chronic obstructive pulmonary disease (COPD), burns, sepsis, trauma, or ventilator-associated pneumonia (VAP).1–3 The pathogenesis of P. aeruginosa is complex, there is evidence showing that P. aeruginosa can secrete a variety of virulence factors (including LPS, 6 type secretion systems, pyocyanin, elastases, alkaline protease, biofilms and others) to adapt to the unfavorable environment of the host, which is responsible for the development of infection and disease.4 In addition, host-pathogen interactions also play a role in the pathogenesis of disease. Of note, P. aeruginosa infection usually causes a high mortality and is an important cause of nosocomial infections.5
According to the China Antimicrobial Surveillance Network (CHINET) (http://www.chinets.com/) in 2023, P. aeruginosa ranks the fifth among clinically isolated pathogens following Escherichia coli, Klebsiella pneumoniae, Staphylococcus aureus, and Acinetobacter baumannii, accounting for 7.8%. To date, the treatment for P. aeruginosa infection has been a challenge because P. aeruginosa rapidly acquires resistance to antibiotics.6 Carbapenem was previously considered as the final resort for the treatment of P. aeruginosa infection. However, the widespread use of carbapenem has led to an increase in P. aeruginosa resistance, resulting in the emergence of carbapenem-resistant P. aeruginosa (CRPA). In 2017, the World Health Organization (WHO) designated CRPA as a priority pathogen.7 In recent years, multidrug resistance (MDR) has increased all over the world and has been considered a threat to public health. Some studies have8–11 reported the emergence of MDR pathogens of different origins, which increases the necessity of the proper use of antibiotics.
To date, few studies have reported the CRPA bloodstream infection (BSI) in Fujian, China. This study aimed to investigate the detection rate of CRPA BSI, antibiotic resistance, and risk factors for the development and mortality of CRPA BSI in a Chinese teaching hospital in Fujian in the past 7 years.
Materials and Methods
Patients and Study Setting
Our study was conducted at Fujian Medical University Union Hospital, a teaching hospital in Fuzhou, Fujian Province, China. It is renowned as one of the largest tertiary hospitals in China. The study was approved by the Ethics Committee of Fujian Medical University Union Hospital (2024KY138). We were dedicated to protecting patient data, and the confidentiality statement was outlined in the ethical review form. This study was a retrospective study, and did not disclose patients’ information, did not interfere with the treatment, and did not increase the risk of patients. Thus, informed consent was not obtained.
Inclusion criteria: Clinical information was collected from the medical record system of patients whose blood cultures were positive for P. aeruginosa between January 1, 2017 and December 31, 2023. For patients with multiple positive blood cultures, only the first positive culture was selected.
Exclusion criteria: (1) Outpatients and individuals with incomplete medical records were excluded from this study. (2) Patients with bacteremia caused by multiple microorganisms were excluded from this study. (3) Patients aged < 18 years were excluded from this study. (4) Patients with catheter-associated bloodstream infection were excluded from this study.
A total of 112 patients with CRPA BSI were included in the final analysis. We selected an equal number of patients with carbapenem-sensitive P. aeruginosa (CSPA) BSI in the same year as the control group. If the number of CSPA patients in that year was insufficient, cases in neighboring years that met inclusion criteria were randomly selected as controls. Therefore, 112 patients with CSPA BSI were included in this study as a control group (Figure 1). Based on the power analysis, the minimum sample size for both the CRPA BSI and CSPA BSI groups was determined to be 68 patients per group. Therefore, the sample size in this study satisfied the necessary requirements, as detailed in Supplementary Data 1.
Data Collection
The following data were obtained from the electronic medical records of 224 patients, including age, sex, length of stay, number of days from hospitalization to positive culture, antimicrobial susceptibility, ward, underlying diseases, conditions before BSI (such as prior invasive procedures and/or devices), exposure to antibiotics within 90 days, and conditions after BSI (including laboratory examinations, therapeutic medication and outcomes at 28-days after bacteremia). For variables with data missing < 15%, we process the missing data through multiple interpolations. For variables with data missing value > 15%, these variables were excluded from the analysis.
Definitions
According to Clinical and Laboratory Standards Institute (CLSI) guideline,12 CRPA was defined as resistance to imipenem or meropenem (minimum inhibitory concentration (MIC) ≥ 8μg/mL), while CSPA was defined as sensitivity to imipenem and meropenem (MIC ≤ 2μg/mL). Multidrug resistance (MDR) was defined as non-susceptibility to at least one agent among three or more antipseudomonal antimicrobials.13 Difficult-to-treat resistance (DTR) was defined as non-susceptibility to all of the following antimicrobials: meropenem, ciprofloxacin, levofloxacin, ceftazidime, cefepime, imipenem-cilastatin, piperacillin-tazobactam, and aztreonam.14 BSI was defined as the isolation of bacteria from blood in the presence of fever or other clinical symptoms consistent with infection.15 The date of BSI onset was defined as the time when the first positive blood culture was obtained. Neutropenia was defined as an absolute neutrophil count < 0.5×109 cells/L. Nosocomial acquisition of BSI was defined as BSI occurring 48 h after admission.16
Microbiological Examination
An automated microbial mass spectrometry system Autof ms1000 (Autobio, China) was used for the bacterial identification, and a VITEK 2 Compact automated system (biomerieux, France) was used for the test of sensitivity to routine antibiotics (including Aminoglycosides: amikacin, tobramycin, cephalosporins: ceftazidime, cefepime; fluoroquinolones: ciprofloxacin, levofloxacin; carbapenems: imipenem, meropenem; β-lactam and β-lactamase inhibitors: piperacillin-tazobactam). Microbroth dilution method was used to determine the minimum inhibitory concentration (MIC) of polymyxin B (BIO-KONT, China) and routine antibiotics. P. aeruginosa ATCC 27853 was used as a standard quality control strain. The susceptibility to ceftazidime-avibactam (OXOID, USA) and cefiderocol (Liofilchem, Italy) was evaluated using the disk diffusion method.
Statistical Analysis
All statistical analyses were performed using the IBM SPSS Statistics v.23.0. The T-test was used for the comparisons of continuous variables between groups, and the Chi-square test was used for categorical variables. For variables with non-normal distribution, Wilcoxon’s test was adopted. Variables with p < 0.05 in the univariate analysis were included in multivariate analyses. Multivariable logistic regression analysis was used to identify the risk factors for development and mortality of CRPA BSI. A value of p < 0.05 was considered statistically significant.
Results
To investigate the detection rate and antibiotic sensitivity of CRPA and other drug-resistant phenotype in Fuzhou is crucial for developing a rational treatment plan. Furthermore, this study aimed to evaluate risk factors associated with BSI and mortality among patients infected with CRPA, which may provide evidence to optimize treatment and reduce the risk of infection and death. Consequently, clinical data were collected from patients at a tertiary teaching hospital in Fujian Province over the past 7 years.
Detection Rates of P. aeruginosa With Different Antibiotic Resistance Phenotypes in Different years
A total of 15824 P. aeruginosa clinical samples were cultured between January 2017 and December 2023, and 7480 P. aeruginosa blood samples were cultured for 7 years. The detection rates for both clinical and blood culture samples of P. aeruginosa increased over year, with the first decline at the end of 2021, followed by a rapid increase (Figure 2A). The detection rate of CRPA in blood culture samples progressively increased from 26% in 2017 to 49% in 2020, subsequently declined to 29% in 2021, and then rapidly increased to 47% in 2023. The increased trends in MDRPA BSI and CRPA BSI were generally consistent, with the detection rate of MDRPA increasing from 10% in 2017 to 36% in 2023, and a similar significant reduction was observed in 2021. In addition, the detection rate of DTRPA BSI remained low until 2022, when it rose sharply to 15% in 2023 (Figure 2B).
Antimicrobial Susceptibility of P. aeruginosa Isolates
The antimicrobial susceptibilities of 224 P. aeruginosa isolates are listed in Table 1. Among the 112 CRPA blood isolates in this study, the rate of resistance to amikacin, tobramycin, ceftazidime, cefepime, ciprofloxacin, levofloxacin, imipenem, meropenem, piperacillin-tazobactam was 33.3%, 47.3%, 42.9%, 41.1%, 57.1%, 57.1%, 96.4%, 83.9% and 63.4%, respectively. The CRPA isolates showed significantly higher resistance to the nine conventional antibiotics than the CSPA isolates (p < 0.001). In addition, 76 MDRPA were identified in the CRPA isolates, while only 2 MDRPA were identified in the CSPA isolates, and the antimicrobial susceptibility to conventional antibiotics was further tested (Table 1). A total of 43 DTRPA isolates were identified (Table 2). Colistin sensitivity tests were not performed in our laboratory before 2021. Between 2022 and 2023, a total of 32 patients underwent polymyxin B susceptibility testing, and only one strain was drug-resistant, with the resistance rate of 3.1%. The drug sensitivity test of ceftazidime-avibactam and cefiderocol was performed on 13 strains of DTRPA isolated in 2023. The results indicated that all 13 isolates were sensitive to ceftazidime-avibactam and two strains were intermediately resistant to cefiderocol, with the resistance rate of 15.38%.
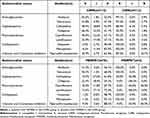 |
Table 1 Susceptibility of the 224 Pseudomonas Aeruginosa to Antimicrobial Agents From 2017 to 2023 |
 |
Table 2 Clinical Characteristics of Patients With CRPA and CSPA BSI |
Clinical Characteristics of Patients With P. aeruginosa BSI
The clinical features of 224 patients suffering from P. aeruginosa BSI are listed in Table 2. There were 159 males (71%), and the median age was 56.6 (45, 69) years. In addition, 180 (80.4%) patients had at least one hospitalization prior to the first positive culture, and the hospital-acquired infection was observed in 181 (78.5%) patients. The majority of patients were from the Department of Hematology (41.5%, n=93), Intensive Care Unit (ICU) (34.8%, n=78), and Department of General Surgery (15.6%, n=35).
For the underlying diseases, hematological diseases accounted for 46.4% (n=104), followed by hypertension (22.3%, n=50), multi-organ failure (19.2%, n=43), diabetes mellitus (18.8%, n=42), and cardiovascular diseases (13.8%, n=31). Compared with CRPA group (37.5%), the proportion of hematological diseases was significantly higher in patients with CSPA BSI (55.4%; p=0.007). There were no significant differences in other underlying diseases between CRPA group and CSPA group. In addition, 155 patients (69.2%) had antibiotics exposure within 90 days, and 42 (18.8%) patients had pre-infection within CRPA. Among 224 patients, the 28-day mortality rate of patients suffering from CRPA BSI was markedly higher than that of those with CSPA BSI (50.9% vs 21.4%, p < 0.001). The detection rates of MDRPA and DTRPA isolates were significantly higher in the CRPA group as compared to the CSPA group (67.9% vs 1.8%, p < 0.001 and 38.4% vs 0.0%, p < 0.001, Table 2). The majority of patients had invasive procedures before the BSI: 114 patients (50.9%) received peripherally inserted central catheters (PICC), 64 patients (28.6%) received central venous catheters (CVC) insertion, and 63 patients (28.1%) underwent endotracheal intubation. Additionally, 59 patients (26.3%) were managed with urinary catheters, 50 patients (22.3%) underwent puncture procedures, and 18 patients (8.1%) received arterial catheter placement. A total of 214 (95.5%) patients received active antimicrobial therapy. However, the utilization rate of ceftazidime-avibactam our study was relatively low, with only 7 out of 224 patients receiving this medication.
Risk Factors Associated With CRPA Bacteremia
Univariate analysis showed that more patients with CRPA were from the ICU, while patients with CSPA were more likely to be from the Department of Hematology. The most prevalent complications for patients suffering from CRPA BSI were chronic lung diseases, transplantation, multi-organ failure, and sepsis or septic shock. Patients infected with CRPA were more likely to receive a previous treatment in the ICU, pre-infection within CRPA, prolonged hospital stay, glucocorticoid therapy, immunosuppressive therapy, arterial catheterization and urinary catheterization, and lower albumin level (Table 2). Moreover, the disparity in antibiotic exposure between CRPA group and CSPA group within 90 days before BSI was predominantly attributed to carbapenems (25.9% vs 8.0%, p < 0.001), β-lactam and β-lactamase inhibitors (44.6% vs 29.5%, p = 0.019), and fluoroquinolones (32.1% vs 11.6%, p < 0.001). Multivariable logistic regression analysis indicated that, chronic lung disease (OR 3.953, 95% CI 1.131–13.812, p = 0.031), transplantation (OR 2.837, 95% CI 1.036–7.770, p = 0.043), multi-organ failure (OR 4.815, 95% CI 1.949–11.894, p = 0.001), pre-infection within CRPA (OR 9.239, 95% CI 3.441–24.803, p < 0.001), and exposure to carbapenems (OR 2.734, 95% CI 1.052–7.106, p = 0.039) within 90 days were independent risk factors associated with CRPA bacteremia (Table 3).
 |
Table 3 Multivariable Analysis of Factors Leading to the Development of CRPA BSI |
Risk Factors for 28-Day Mortality of CRPA BSI
In the 28-day follow-up, 57 (50.9%) patients infected with CRPA died, and 42 of 76 MDRPA-infected patients (55.3%) and 24 of 43 DTRPA-infected patients (55.8%) died. Eight patients died before the antibiotic sensitivity test were available, and 5 patients died after voluntarily giving up treatment. To identify the risk factors associated with 28-day mortality of patients infected with CRPA BSI, the demographics, clinical characteristics, and prior antibiotic exposure were compared between survivors and non-survivors.
Univariate analysis showed that patients who died within 28 days were more likely to be male, elderly, and from ICU, and mainly had hospital-acquired infections. Most non-survivors experienced unfavorable outcomes including multi-organ failure (p = 0.002) and sepsis/septic shock (p < 0.001) after BSI. Prior exposure to tigecycline and colistin within 90 days, previous invasive procedures and lower hemoglobin levels were associated with 28-day mortality (Table 4). There were no significant differences in antibiotic treatment regimens after BSI or other characteristics between survivors and non-survivors. (Supplementary Table S1).
 |
Table 4 Risk Factors for 28-Day Mortality in Patients With CRPA BSI |
In the multivariable logistic regression analysis, the use of colistin before infection (OR 4.890, 95% CI 1.003–23.846, p = 0.049) and sepsis or septic shock (OR 8.774, 95% CI 3.140–24.515, p = 0.001) were independent risk factors associated with 28-day mortality, whereas hemoglobin was found as a protective factor (OR 0.965, 95% CI 0.939–0.991, p = 0.010) (Table 5).
 |
Table 5 Multivariable Regression Analysis of Mortality in Patients With CRPA BSI |
Discussion
In this study, patients were included from one of the largest tertiary hospitals in Fujian Province. The patients admitted into this hospital were from all regions of Fujian Province and therefore representative. According to epidemiological statistics, the detection rate of CRPA worldwide shows an increasing trend, with the highest rate reaching 64.6% in Latin America.17 Lu et al18 carried out an 11-year, multi-center retrospective study in Hunan Province, China, and found that the rate of CRPA infections among patients with hematological malignancies (HM) increased significantly from 9.1% to 88.9%. A retrospective study conducted in Zhejiang Province, China, reported that the detection rate of CRPA BSI increased from 17% in 2012 to 60% in 2020.19 Our results indicated a consistent annual increase in the detection rates of CRPA BSI and MDRPA BSI from 2017 to 2020. However, the detection rates decreased significantly in 2021 and then increased from 2022. During the COVID-19 pandemic, the incidence of various diseases was reported to decline, which was attributed to the preventive and control measures during the epidemic. A retrospective study conducted across 70 countries and 457 stroke centers worldwide indicated that the COVID-19 pandemic was associated with a global reduction in the incidence of stroke.20 Our results may be related to the coincidence with the peak of the COVID-19 pandemic in China. In this period, widespread measures such as mask-wearing, enhanced disinfection protocols, and reduced public gatherings effectively protected vulnerable populations and reduced the spread of pathogenic bacteria. A study conducted in Wuhan, China, indicated that the detection rate of DTRPA exhibited a declining trend from 2013 to 2021.21 Similarly, our study indicated that the detection rate of DTRPA remained at a low level until 2021. However, the prevalence of drug-resistant phenotype showed a significant upward trend since 2022, warranting close attention. In addition, antibiotic classification management may be an effective way to reduce resistance. For instance, it is crucial to make rational choices regarding antibiotic therapy based on a thorough analysis of the infection site, severity of infection, bacterial drug resistance patterns, and the pathophysiological characteristics of patients. Secondly, minimizing unnecessary antibiotic usage represents another viable strategy.
P. aeruginosa can secrete some virulence factors, leading to a significant morbidity, which reduces the life expectancy, and elevates the mortality. For instance, the endotoxicity of lipid A LPS can induce tissue damage.22 Additionally, six types of secretion systems, including Type VI secretion system (associated with flagella), Type IV secretion system (associated with pili), and Type III secretion system (associated with multi-toxin components), contribute to the pathogenic process of P. aeruginosa.5 Many virulence factors are regulated by Quorum sensing (QS) system,23 and two-component systems24 and small non-coding regulatory RNAs also play important roles in the virulence regulation.25,26 Several virulence genes, including fimH, papC, lasB, rhlI, lasI, and toxA have been identified as the important factors related to the pathogenicity of P. aeruginosa.11 In response to diverse environmental challenges, bacteria have developed an array of resistance mechanisms. P. aeruginosa has acquired antibiotic resistance through multiple pathways, including outer membrane permeability, efflux system, and antibiotic inactivating enzyme.27 Resistance attributed to biofilm formation is associated with the presence of flagella and adhesins.28 The resistance of P. aeruginosa to carbapenem is mainly attributed to the absence or reduction of porin OprD, the excessive expression of AmpC, and the mediation of efflux pumps.29 The MDRPA or DTRPA frequently results from the interplay of multiple intricate resistance mechanisms.14 Molecular screening of antibiotic resistance genes is very important to investigate the resistance mechanism of P. aeruginosa.8,9 Our study indicated that the antibiotic resistance rate of CRPA in our hospital was different from that in other regions. Therefore, it is imperative to investigate the pathogenesis and antibiotic resistance mechanisms of CRPA, which may provide new strategies for the control of P. aeruginosa infection.
In accordance with previous findings,30–32 our results indicated that P. aeruginosa had the lowest rate of resistance to polymyxin B (~3.1%). Of note, the sample size was small in this study, and more studies with large sample size are warranted to further validate our findings. Studies have indicated that the resistance rate of CRPA to amikacin is very low, but the resistance rate of 112 CRPA to amikacin in our study was 33%, which was significantly higher than previously reported.33–36 This also suggests that local health-care providers should take caution to the empirical treatment of CRPA BSI infections with amikacin. CRPA strains often exhibit resistance to other antibiotics,37 which is consistent with our results. Moreover, our study indicated that CRPA showed the highest rate of resistance to piperacillin-tazobactam (63.4%). Clinical investigation shows that our hospital has a very high utilization rate of piperacillin-tazobactam, which may explain the resistance to this drug. The expert consensus on lower respiratory tract infections caused by P. aeruginosa in China recommends that ceftazidime-avibactam may serve as a first-line treatment alternative for CRPA infections when antibacterial susceptibility testing (AST) confirms the susceptibility to ceftazidime-avibactam.38 However, the utilization rate of ceftazidime-avibactam in this study was relatively low, which may limit its reference value. The definition of DTR emphasizes on the influence of antibiotic resistance on treatment choices and prognosis.39 The panel in United States strongly advocates that all microbiology laboratories conduct AST for MDRPA and DTRPA isolates against novel β-lactam drugs.14 Studies have shown that ceftazidime-avibactam is an effective option for the treatment of MDRPA and DTRPA,40,41 and cefiderocol has been proven to be effective in the treatment of severe infections caused by DTRPA.42,43 The 13 strains of DTRPA isolated in 2023 were evaluated for the sensitivity to ceftazidime-avibactam and cefiderocol, and the resistance rates were 0% and 15.4%, respectively. Although cefiderocol has not yet been approved for clinical use in China, resistant strains have already emerged. Therefore, investigating the mechanisms of cefiderocol resistance is of significant importance.
Our study showed a higher incidence of previous exposure to “carbapenems, β-lactam and β-lactamase inhibitors, and fluoroquinolone” in the CRPA group. Additionally, previous exposure to carbapenems was identified as an independent risk factor for CRPA BSI, which is in accordance with previously reported.19,30 Therefore, to understand the drug resistance pattern and the risk factors for CRPA BSI is crucial for providing rational treatment. Our results also indicated that ICU stay before BSI onset, prior CRPA infection, longer hospital stay, glucocorticoid therapy, immunosuppressive treatment, arterial catheter indwelling and urinary catheter indwelling and lower albumin levels were related to the development of CRPA BSI. In addition, chronic lung disease, multiple organ failure, transplantation, and prior CRPA infection were also found to be independent risk factors for the development of CRPA bacteremia in the present study. Damage to the mucous membranes of the respiratory tract in patients with chronic lung disease can lead to the invasion of colonized P. aeruginosa into the blood, resulting in BSI.44–46 Patients with multiple organ failure and those undergoing transplantation have compromised immune function, which inevitably increases the risk of P. aeruginosa BSI. Therefore, strictly controlling the use of carbapenem antibiotics, active management of high-risk complications, prudent use of immunosuppressants, and enhanced care for patients with prior ICU stay are essential for the management of CRPA BSI.
In this study, the 28-day mortality rate was 50.9% in 112 patients with CRPA, and the mortality rates were notably elevated in patients with MDRPA and DTRPA (55.3% and 55.8%, respectively), which was significantly higher than previously reported.19,35,36 Multivariable regression analysis revealed that prior exposure to colistin and sepsis or septic shock were independent risk factors for 28-day mortality, whereas hemoglobin was a protective factor. Colistin (polymyxin B or E) is recognized as a last-resort antibiotic for the treatment of CRPA infections,47 and it is typically employed when the infection is severe or other antibiotics have proven ineffective. Consequently, the mortality of patients may be more attributable to the severity and critical nature of their condition rather than the administration of polymyxins. Furthermore, our study appeared reasonable; however, the utilization rate of polymyxin in this study was notably low, with only 15 out of 112 CRPA patients with prior medication of polymyxin B. Therefore, studies with larger sample size are needed to further confirm the reliability of our findings. We recommend that clinicians can regularly evaluate risk factors associated with mortality and develop personalized treatments accordingly.
There were still limitations in this study. First, this was a single-center study in Fuzhou, China, and therefore, our findings are not representative of other regions across the country. Second, the condition of patients with CRPA is complex, and the regimen for antibiotic treatment should adjust accordingly throughout the course of treatment. For instance, some patients may have been prescribed more than 5 antibiotics, and thus it is difficult to assess the influence of antibiotic treatment regimen on the prognosis of patients. Therefore, more prospective studies are required to confirm our findings by controlling confounding factors. Third, this was a retrospective study, the absence of some data led to patient selection bias, which may have affected our results, and the mechanism of drug resistance was not investigated. Therefore, large samples or prospective studies are needed to further validate our conclusions, and investigate mechanisms underlying the antibiotic resistance, which is helpful for the development of novel strategies for the treatment of P. aeruginosa BSI.
Conclusions
Our study indicates the detection rates of CRPA, MDRPA, and DTRPA show an increasing trend in Fuzhou, China. Chronic lung disease, transplantation, multi-organ failure, prior CRPA infection, and prior carbapenems exposure are independent risk factors associated with the development of CRPA bacteremia. Additionally, sepsis or septic shock are independent risk factors for 28-day mortality in patients with CRPA BSI. More studies are needed to investigate the molecular mechanisms underlying the resistance of CRPA, standardize the use of antibiotics, and assess risk factors for development and mortality of CRPA BSI, which are beneficial to control P. aeruginosa infection and reduce its mortality.
Data Sharing Statement
The data presented in this study are available upon request from the corresponding author.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Fujian Medical University Union Hospital (2024KY138). As this study was retrospective, informed consent was waived by my ethics committee.
Funding
This study was supported by Fujian Medical University Union Hospital Key Disciplines Funding (2022YYZDXK11) and Fujian Research and Training Grants for Young and Middle-aged Leaders in Healthcare (to Bin Li).
Disclosure
The authors declare no conflict of interest.
References
1. Rossi E, La Rosa R, Bartell JA, et al. Pseudomonas aeruginosa adaptation and evolution in patients with cystic fibrosis. Nat Rev Microbiol. 2021;19(5):331–342. doi:10.1038/s41579-020-00477-5
2. Jurado-Martín I, Sainz-Mejías M, McClean S. Pseudomonas aeruginosa: an audacious pathogen with an adaptable arsenal of virulence factors. Int J mol Sci. 2021;22(6):3128. doi:10.3390/ijms22063128
3. Cendra MDM, Torrents E. Pseudomonas aeruginosa biofilms and their partners in crime. Biotechnol Adv. 2021;49:107734. doi:10.1016/j.biotechadv.2021.107734
4. Vidaillac C, Chotirmall SH. Pseudomonas aeruginosa in bronchiectasis: infection, inflammation, and therapies. Expert Rev Respir Med. 2021;15(5):649–662. doi:10.1080/17476348.2021.1906225
5. Qin S, Xiao W, Zhou C, et al. Pseudomonas aeruginosa: pathogenesis, virulence factors, antibiotic resistance, interaction with host, technology advances and emerging therapeutics. Signal Transduct Target Ther. 2022;7(1):199. doi:10.1038/s41392-022-01056-1
6. Blomquist KC, Nix DE. A critical evaluation of newer β-lactam antibiotics for treatment of Pseudomonas aeruginosa infections. Ann Pharmacother. 2021;55(8):1010–1024. doi:10.1177/1060028020974003
7. Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–327. doi:10.1016/S1473-3099(17)30753-3
8. Al-Kadmy IMS, Abid SA, Aziz SN, et al. The secrets of environmental Pseudomonas aeruginosa in slaughterhouses: antibiogram profile, virulence, and antibiotic resistance genes. Folia Microbiol. 2024;69(4):805–822. doi:10.1007/s12223-023-01116-1
9. Algammal AM, Eidaroos NH, Alfifi KJ, et al. oprL gene sequencing, resistance patterns, virulence genes, quorum sensing and antibiotic resistance genes of XDR Pseudomonas aeruginosa isolated from broiler chickens. Infect Drug Resist. 2023;16:853–867. doi:10.2147/IDR.S401473
10. Shafiq M, Zeng M, Permana B, et al. Coexistence of bla NDM-5 and tet(X4) in international high-risk Escherichia coli clone ST648 of human origin in China. Front Microbiol. 2022;13:1031688. doi:10.3389/fmicb.2022.1031688
11. Algammal AM, Alfifi KJ, Mabrok M, et al. Newly emerging MDR B. cereus in mugil seheli as the first report commonly harbor nhe, hbl, cytK, and pc-plc virulence genes and bla1, bla2, tetA, and ermA resistance genes. Infect Drug Resist. 2022;15:2167–2185. doi:10.2147/IDR.S365254
12. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing, M100, 31st Ed. Clinical and Laboratory Standards Institute; 2021.
13. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
14. Tamma PD, Aitken SL, Bonomo RA, et al. Infectious diseases society of America 2023 guidance on the treatment of antimicrobial resistant gram-negative infections. Clin Infect Dis. 2023:ciad428. doi:10.1093/cid/ciad428
15. Genga KR, Russell JA. Update of sepsis in the intensive care unit. J Innate Immun. 2017;9(5):441–455. doi:10.1159/000477419
16. Averbuch D, Orasch C, Cordonnier C, et al. European guidelines for empirical antibacterial therapy for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European conference on infections in leukemia. Haematologica. 2013;98(12):1826–1835. doi:10.3324/haematol.2013.091025
17. Nordmann P, Poirel L. Epidemiology and diagnostics of carbapenem resistance in gram-negative bacteria. Clin Infect Dis. 2019;69(Suppl 7):S521–S528. doi:10.1093/cid/ciz824
18. Lu L, Xu C, Tang Y, et al. The threat of carbapenem-resistant gram-negative bacteria in patients with hematological malignancies: unignorable respiratory non-fermentative bacteria-derived bloodstream infections. Infect Drug Resist. 2022;15:2901–2914. doi:10.2147/IDR.S359833
19. Yuan Q, Guo L, Li B, et al. Risk factors and outcomes of inpatients with carbapenem-resistant Pseudomonas aeruginosa bloodstream infections in China: a 9-year trend and multicenter cohort study. Front Microbiol. 2023;14:1137811. doi:10.3389/fmicb.2023.1137811
20. Nogueira RG, Qureshi MM, Abdalkader M, et al. Global impact of COVID-19 on stroke care and IV thrombolysis. Neurology. 2021;96(23):e2824–e2838. doi:10.1212/WNL.0000000000011885
21. Zhang Z, Tian L. Trends in DTR, CR, ECR, and FQR in four common gram-negative bacteria: a retrospective study from 2013 to 2021. Infect Drug Resist. 2022;15:2625–2631. doi:10.2147/IDR.S365139
22. Park WS, Lee J, Na G, et al. Benzyl isothiocyanate attenuates inflammasome activation in Pseudomonas aeruginosa LPS-stimulated THP-1 cells and exerts regulation through the MAPKs/NF-κB pathway. Int J mol Sci. 2022;23(3):1228. doi:10.3390/ijms23031228
23. Yang D, Hao S, Zhao L, et al. Paeonol attenuates quorum-sensing regulated virulence and biofilm formation in Pseudomonas aeruginosa. Front Microbiol. 2021;12:692474. doi:10.3389/fmicb.2021.692474
24. Gooderham WJ, Hancock REW. Regulation of virulence and antibiotic resistance by two-component regulatory systems in Pseudomonas aeruginosa. FEMS Microbiol Rev. 2009;33(2):279–294. doi:10.1111/j.1574-6976.2008.00135.x
25. Klein G, Raina S. Small regulatory bacterial RNAs regulating the envelope stress response. Biochem Soc Trans. 2017;45(2):417–425. doi:10.1042/BST20160367
26. Pita T, Feliciano JR, Leitão JH. Small noncoding regulatory RNAs from Pseudomonas aeruginosa and Burkholderia cepacia complex. Int J mol Sci. 2018;19(12):3759. doi:10.3390/ijms19123759
27. Breidenstein EBM, de la Fuente-Núñez C, Hancock REW. Pseudomonas aeruginosa: all roads lead to resistance. Trends Microbiol. 2011;19(8):419–426. doi:10.1016/j.tim.2011.04.005
28. Ozer E, Yaniv K, Chetrit E, et al. An inside look at a biofilm: pseudomonas aeruginosa flagella biotracking. Sci Adv. 2021;7(24):eabg8581. doi:10.1126/sciadv.abg8581
29. Horcajada JP, Montero M, Oliver A, et al. Epidemiology and treatment of multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa infections. Clin Microbiol Rev. 2019;32(4):e00031–19. doi:10.1128/CMR.00031-19
30. Wei X, Li L, Li M, et al. Risk factors and outcomes of patients with carbapenem-resistant Pseudomonas aeruginosa bloodstream infection. Infect Drug Resist. 2023;16:337–346. doi:10.2147/IDR.S396428
31. Jeong S, Jeon K, Lee N, et al. Changing genotypic distribution, antimicrobial susceptibilities, and risk factors of urinary tract infection caused by carbapenemase-producing Pseudomonas aeruginosa. Ann Lab Med. 2024;44(1):38–46. doi:10.3343/alm.2024.44.1.38
32. Benzaarate I, El Otmani F, Khazaz A, et al. Detection of carbapenemase encoding gene and resistance to cefiderocol in hospital and community eXtensive drug resistance and carbapenem-resistant Pseudomonas aeruginosa strains in morocco. Foodborne Pathog Dis. 2023;20(10):460–466. doi:10.1089/fpd.2023.0018
33. Yuan F, Xiao W, Wang X, et al. Clinical characteristics and prognosis of bloodstream infection with carbapenem-resistant Pseudomonas aeruginosa in patients with hematologic malignancies. Infect Drug Resist. 2023;16:4943–4952. doi:10.2147/IDR.S419064
34. Zhen S, Zhao Y, Chen Z, et al. Assessment of mortality-related risk factors and effective antimicrobial regimens for treatment of bloodstream infections caused by carbapenem-resistant Pseudomonas aeruginosa in patients with hematological diseases. Front Cell Infect Microbiol. 2023;13:1156651. doi:10.3389/fcimb.2023.1156651
35. Ioannou P, Alexakis K, Maraki S, et al. Pseudomonas bacteremia in a tertiary hospital and factors associated with mortality. Antibiotics (Basel). 2023;12(4):670. doi:10.3390/antibiotics12040670
36. Kang JS, Moon C, Mun SJ, et al. Antimicrobial susceptibility trends and risk factors for antimicrobial resistance in Pseudomonas aeruginosa bacteremia: 12-year experience in a tertiary hospital in Korea. J Korean Med Sci. 2021;36(43):e273. doi:10.3346/jkms.2021.36
37. Codjoe F, Donkor E. Carbapenem resistance: a review. Medical Sciences. 2017;6(1):1. doi:10.3390/medsci6010001
38. Bronchiectasis Expert Consensus Writing Group. Pulmonary infection assembly of Chinese thoracic society. Zhonghua Jie He He Hu Xi Za Zhi. 2022;45(8):739–752. doi:10.3760/cma.j.cn112147-20220407-00290
39. Huh K, Chung DR, Ha YE, et al. Impact of difficult-to-treat resistance in gram-negative bacteremia on mortality: retrospective analysis of nationwide surveillance data. Clin Infect Dis. 2020;71(9):e487–e496. doi:10.1093/cid/ciaa084
40. Vena A, Giacobbe DR, Castaldo N, et al. Clinical experience with ceftazidime-avibactam for the treatment of infections due to multidrug-resistant gram-negative bacteria other than carbapenem-resistant enterobacterales. Antibiotics. 2020;9(2):71. doi:10.3390/antibiotics9020071
41. Xu C, Zeng F, Huang Y, et al. Clinical efficacy of ceftazidime/avibactam combination therapy for severe hospital-acquired pulmonary infections caused by carbapenem-resistant and difficult-to-treat Pseudomonas aeruginosa. Int J Antimicrob Agents. 2024;63(1):107021. doi:10.1016/j.ijantimicag.2023.107021
42. Edgeworth JD, Merante D, Patel S, et al. Compassionate use of cefiderocol as adjunctive treatment of native aortic valve endocarditis due to extremely drug-resistant Pseudomonas aeruginosa. Clin Infect Dis. 2019;68(11):1932–1934. doi:10.1093/cid/ciy963
43. Stevens RW, Clancy M. Compassionate use of cefiderocol in the treatment of an intraabdominal infection due to multidrug-resistant Pseudomonas aeruginosa: a Case Report. Pharmacotherapy. 2019;39(11):1113–1118. doi:10.1002/phar.2334
44. Babich T, Naucler P, Valik JK, et al. Risk factors for mortality among patients with Pseudomonas aeruginosa bacteraemia: a retrospective multicentre study. Int J Antimicrob Agents. 2020;55(2):105847. doi:10.1016/j.ijantimicag.2019.11.004
45. Recio R, Viedma E, González-Bodí S, et al. Clinical and bacterial characteristics of Pseudomonas aeruginosa affecting the outcome of patients with bacteraemic pneumonia. Int J Antimicrob Agents. 2021;58(6):106450. doi:10.1016/j.ijantimicag.2021.106450
46. Teelucksingh K, Shaw E. Clinical characteristics, appropriateness of empiric antibiotic therapy, and outcome of Pseudomonas aeruginosa bacteremia across multiple community hospitals. Eur J Clin Microbiol Infect Dis. 2022;41(1):53–62. doi:10.1007/s10096-021-04342-y
47. Roch M, Sierra R, Andrey DO. Antibiotic heteroresistance in ESKAPE pathogens, from bench to bedside. Clin Microbiol Infect. 2023;29(3):320–325. doi:10.1016/j.cmi.2022.10.018
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



