Back to Journals » Therapeutics and Clinical Risk Management » Volume 20
Risk Factors for Digital Replantation Failure: A Nomogram Prediction Model
Authors Guo T, Ma T, Gao R, Yu K, Bai J
Received 12 October 2024
Accepted for publication 11 December 2024
Published 27 December 2024 Volume 2024:20 Pages 929—937
DOI https://doi.org/10.2147/TCRM.S498528
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor De Yun Wang
Tianhao Guo,1 Tao Ma,2 Ruijiao Gao,3 Kunlun Yu,1 Jiangbo Bai1
1Department of Hand Surgery, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050051, People’s Republic of China; 2Department of Trauma Emergency Surgery,The First Affiliated Hospital of Hebei North University, Zhangjiakou, Hebei, 075000, People’s Republic of China; 3Department of Vascular Surgery, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050051, People’s Republic of China
Correspondence: Jiangbo Bai, Department of Hand Surgery, The Third Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050051, People’s Republic of China, Email [email protected]
Study Design: A Retrospective study.
Objective: Digital necrosis (DN) after replantation can cause some serious complication. Few articles focused on the risk factors of DN; therefore, we aim to investigate the risk factors of necrosis after multiple digital replantation.
Methods: We collected the data of patients receiving multiple digital replantation in our hospital between Jan. 2017 and Jan. 2024. Based on the necrosis or not after replantation, patients with DN were as necrosis group (NG), and patients without DN were as success group (SG). The demographics, comorbidities, and admission laboratory examinations of patients were computed by univariate analysis, logistic regression analysis, and receiver operating characteristic (ROC) curve analysis. We then construct a nomogram prediction model, plot ROC curves, calibration curves, and DCA decision curves using R language software.
Results: The survival rate in our study was 83.7% (278 of 332). Univariate analysis indicated that there were significant differences in the level of D-dimer, white blood cell, neutrophil, monocyte, monocyte-to-lymphocyte ratio, systemic immune-inflammation index, system inflammation response index, C-reactive protein (CRP), neutrophils/high density lipoprotein (HDL), monocytes/HDL were significantly higher in NG than in SG. However, logistic regression analysis showed that D-dimer and CRP were independent risk factors of DN, and we identified their cut-off values. Then, we constructed a nomogram prediction model with 0.7538 in AUC of the prediction model with good consistency in the correction curve and good clinical practicality by decision curve analysis.
Conclusion: The level of D-dimer and CRP was found to be closely related to DN. We constructed a nomogram prediction model that can effectively predict DN in patients with multiple digital replantation.
Keywords: necrosis, multiple digital replantation, D-dimer, CRP, risk factors
Introduction
Finger amputation is a common traumatic disorder, which may lead to catastrophic physical and psychosocial repercussions. Replantation was first reported by Malt et al1 to treat digital amputation with 70% to 90% survival rates based on previous studies.2,3 Replantation provides hope to numerous patients, because it can preserve digital length and nail, provide decent soft-tissue soft-tissue coverage, and maintain good joint motion, which improves patient satisfaction cosmetically and functionally in comparison with other methods, such as skin grafting.4,5 Recently, increasing evidence has been reported that injury mechanism, platelet count, smoking, preservation method of amputated part and the use of vein graft were closely related to digital necrosis (DN).6 Wojciech Dec7 found that patients with diabetes, smoking and crushing or avulsion injury were predictors for necrosis after replantation. Wang8 performed a retrospective study of 946 patients with replantation and first concluded that menstrual period, menopause, and the level of D-dimer were predictors of DN after digital replantation.
Ongoing literature is tried to investigate the relationship between inflammatory indicators in various diseases, such as ischemia-reperfusion injury.9,10 As we know, litter research explored the role of inflammatory indicators, such as the complete blood count and derived inflammatory indicators, in the prediction of DN after digital replantation. Although various studies focused on the predictors of DN, its predictors remain debated. Hence, we performed a nomogram prediction model to investigate predictors of DN. As far as we know, this is the first study to assess the relationship between derived inflammatory indicators and predictors for DN.
Materials and Methods
Ethics Statement
The study was approved by the Institutional Review Board of Third Hospital of Hebei Medical University in compliance with the Helsinki, and an exemption from the informed consent was obtained. All data were anonymized before the analysis to safeguard patient privacy (W2021-046-1).
Patients
We included 332 patients, including 54 patients with DN and 278 who were not, receiving multiple digital replantation from Jan. 2017 and Jan. 2024 in our hospital. The inclusion criteria: (1) multiple complete finger separation; (2) more than 18 years old. The exclusion criteria were as follows: (1) congenital finger deformity; (2) history of hand surgery. We obtained information of demographics (age, gender, BMI, injury mechanism, ischemia time, probe artery, injury hand), comorbidities (patients with a history of heart valve disease, heart failure, heart infarction, diabetes, or hypertension), and admission laboratory examinations, including prothrombin time (PT), international normalized ratio (INR), fibrinogen (FIB), activated partial thromboplastin time (APTT), thrombin time (TT), D-dimer, white blood cell (WBC), neutrophil (NEU), lymphocyte (LYM), monocyte (MON), red blood cell (RBC), platelet (PLT), neutrophil-to-lymphocyte ratio (neutrophils count/lymphocytes count, NLR), Monocyte-to-lymphocyte ratio (monocytes count/lymphocytes count, MLR), Platelet-to-lymphocyte ratio (platelets count/lymphocytes count, PLR), systemic immune-inflammation index (platelets count × neutrophils count)/lymphocytes count, SII), and system inflammation response index (monocyte count × neutrophils count)/lymphocytes count, SIRI), c-reactive protein (CRP), HDL=high-density lipoprotein; NHR=neutrophils/HDL; LHR=lymphocyte/HDL; MHR=monocytes/HDL; PHR=platelets/HDL.
All measurement data were presented as the mean ± SD. (standard deviation) when data satisfied the criteria for normality with p > 0.05. Since our data did not satisfy the criteria for normality and homogeneity of variance, statistical analysis between groups was performed using the rank sum test. For count data, chi-square test was used for data analysis. Statistical significance levels were considered to be p<0.05. All statistical analyses were carried out using SPSS, version 27.0 (SPSS Inc., Chicago, IL). To identify the best predictors of DN, univariate and multivariate analyses were computed. We choose the cut-off values for continuous variables by the maximum Youden index (sensitivity+specificity-1) in the ROC curve analysis. We used R language software to establish the nomogram prediction model for aDVT according to the multivariate logistic regression analysis results, and then we assessed the discriminative ability of the prediction model by AUC of ROC, and we evaluated the predicted and actual probabilities of this prediction model by calibration curve. The decision curve analysis is to evaluate the clinical application value of the prediction model.
Results
As shown in Tables 1 and 2, there were no significant differences in age, gender, BMI, injury mechanism, ischemia time, probe artery, injury hand, patients with a history of heart valve disease, heart failure, heart infarction, diabetes, or hypertension, PT, as well as the level INR, FIB, APTT, TT, LYM, RBC, PLT, NLR, PLR, HLD, LHR, and PHR between two groups by univariate analysis. However, we found that the level of D-dimer (p < 0.0001), WBC (p = 0.017), NEU (p = 0.025), MON (p = 0.002), MLR (p = 0.003), SII (p = 0.032), SIRI (p = 0.003), CRP (p < 0.0001), NHR (p = 0.019), and MHR (p = 0.001) were significantly higher in NG than in SG.
 |
Table 1 Possible Factors May Be Associated with Digital Necrosis After Replantation in Two Groups |
 |
Table 2 Laboratory Examinations May Be Associated with Digital Necrosis After Replantation in Two Groups |
Additionally, our findings showed that D-dimer [p = 0.012, OR = 1.859, 95% CI (1.145, 3.018)] and CRP [p = 0.005, OR = 1.009, 95% CI (1.003, 1.015)] were independent risk factors of DN by logistic regression analysis (Table 3). ROC curve analysis showed that the level of D-dimer (p < 0.0001, AUC area = 0.732, 95% CI (0.659,0.805)), and CRP (p < 0.0001, AUC area = 0.697, 95% CI (0.625,0.769)) were independent predictors of DN after replantation, and we identified that their cut-off values were 0.695 mg/L, and 30.985 mg/L, respectively (Table 4).
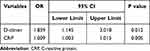 |
Table 3 Logistic Regression Analysis of Laboratory Variables Associated with Digital Necrosis After Replantation |
 |
Table 4 ROC Curve Analysis and Cut-Off Values Associated with Digital Necrosis After Replantation |
As shown in Figure 1, we conduct a nomogram prediction model according to the results of logistic regression analysis. The ROC curve of the nomogram suggested good discrimination ability [AUC = 0.7538, 95% CI(0.6966, 0.7929)] and the calibration curve of the nomogram with Hosmer Lemeshow goodness-of-fit test showed well calibrated (p > 0.05, Figures 2 and 3). Decision curve analysis implied the nomogram prediction model with good clinical benefits (Figure 4).
 |
Figure 1 The nomogram prediction model for digital necrosis in patients with replantation. |
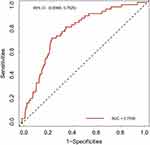 |
Figure 2 The receiver operating characteristic curves. |
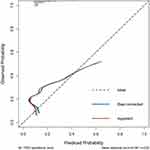 |
Figure 3 The calibration curve of nomogram. |
 |
Figure 4 The decision curve analysis of the nomogram. |
Discussion
DN after replantation is a serious complication that not only affects the digital appearance but also their function. Therefore, it is crucial to have a deep understanding of its risk factors and take timely measures to address them. Yu11 reviewed related studies and concluded that crush and avulsion injury, little finger, children and cold preservation were associated with DN after surgery, but ischemia time was not found to affect DN, which was different from the findings of Breahna4 that the timing of replantation and the ischemia time can impact the outcome of replantation. Wang8 conducted a comprehensive and in-depth analysis of 946 patients receiving digital replantation and first found that menstrual period, menopause, and the level of D-dimer were predictors of DN. Additionally, Wang8 also assessed the relationship between starting and finishing time of surgery and duration of surgery and DN and found that duration of surgery was identified as a predictor of DN.
In our study, the survival rate was 83.7% (278 of 332). Univariate analysis showed that the levels of D-dimer, WBC, NEU, MON, MLR, SII, SIRI, CRP, NHR, and MHR were related to DN. Furthermore, D-dimer and CRP were found to be the predictors for DN by logistic regression analysis, and we identified their cut-off values. The nomogram prediction model we performed has 0.7538 in the AUC of the prediction model, which implied good consistency in the correction curve and good clinical practicality by decision curve analysis.
Previous studies have reported that the survival rates of replantation to treat digital amputation ranged from 70% to 90%.2,3 Wang8 concluded a retrospective study of 946 patients with 78.8% survival rate in our study. In this study, the survival rate was 83.7% after multiple digital replantation, which was similar to prior research.2,3,8
D-dimer is widely used to evaluate venous thrombus in clinical practice.12 Recently, it has also been a predictor for other diseases, such as heart failure, coronary syndrome, pneumonia and cancer.3,5 Wang8 first reported the relationship D-dimer and DN and found that the level of D-dimer replantation played a crucial role in the assessment of DN. In our study, we found similar results showing that the level of D-dimer in FG was significantly higher than in SG, which was also demonstrated by logistic regression analysis. Above mentioned implied that patients with high D-dimer were more likely to suffer from replantation failure. As we know, replantation failure was mostly associated with the blockage of blood vessels in the hypercoagulable state resulting in microthrombus because D-dimer could originate from the formation and lysis of cross-linked fibrin, which can account for our and Wang’s findings. It is worth noting that Wang did not investigate the cut-off value of D-dimer to predictor DN after single digital replantation.8 Therefore, we used ROC curve analysis to identify 0.695 mg/L as the cut-off value of D-dimer to predictor DN.
Increasing literature has reported that inflammation contributed to the development of some traumatic disorders, such as ischemia-reperfusion injury.9,10 Inflammation can cause a hypercoagulable state by activating platelets, neutrophils, and endothelial cells, as well as by modulating the expression and function of coagulation factors and inhibitors. Recently, NLR, PLR, MLR, SII, and SIRI indexes have been reported that these indicators played an important role in many diseases because they can suggest a balance of systemic inflammation.13,14 To our knowledge, this is the first study assessing the relationship between inflammatory indicators and DN after digital replantation. In this study, the levels of D-dimer, WBC, NEU, MON, MLR, SII, SIRI, CRP, NHR, and MHR were found to be related to DN by univariate analysis. However, logistic regression analysis showed that CRP was an independent predictor of DN after replantation. CRP is a well-known biomarker for inflammation that binds to dead and damaged cells, which was used to screen various diseases, such as coronary heart disease and severe non-vascular diseases.15 Notably, CRP can improve the ability of the D-dimer and other fibrin degradation products to up-regulate interleukin-6 synthesis, which promotes CRP synthesis.16 We also used ROC curve analysis to identify the 30.985 mg/L as cut-off values of CRP.
According to the results of univariate and multivariate analyses in this study, we established a prediction model to evaluate DN after digital replantation. The ROC curve of the nomogram suggested good discrimination ability, and the calibration curve of the nomogram with Hosmer Lemeshow goodness-of-fit test showed well calibrated. Decision curve analysis showed that the nomogram prediction model has good clinical benefits.
Although our study offers some novel findings, it still has some limitations. First, this was a retrospective and single-center study, we need a large-scale cohort studies instead to validate the findings. Second, other factors that may related to necrosis, such as smoking history, were not fully included due to limited data in electronic medical records. Additionally, we did not perform external validation due to the limited sample size. Finally, although ten hand surgeons performed replantation in this study, they were hand surgeons with more than 5 years of experience.
In conclusion, we found that the level of D-dimer and CRP were closely related to DN by multivariate analysis, and we identified their cut-off value to predict DN. We also constructed a nomogram prediction model that can effectively predict DN in patients with multiple digital replantation. The purpose of this article is to share our experience in treating complete multiple digital amputation, which may help us take some preoperative measures to lower the incidence of DN.
Abbreviations
DN, digital necrosis; CRP, C-reactive protein; HDL, high-density lipoprotein; PT, prothrombin time; INR, international normalized ratio; FIB, fibrinogen; APTT, activated partial thromboplastin time; TT, thrombin time; WBC, white blood cell; NEU, neutrophil; LYM, lymphocyte; MON, monocyte; RBC, red blood cell; PLT, platelet; NLR, Neutrophil-to-lymphocyte ratio; MLR, Monocyte-to-lymphocyte ratio; PLR, Platelet-to-lymphocyte ratio; SII, systemic immune-inflammation index; SIRI, system inflammation response index; CRP, C-reactive protein; NHR, neutrophils/HDL; LHR, lymphocyte/HDL; MHR, monocytes/HDL; PHR, platelets/HDL; NG, necrosis group; SG, success group.
Ethical Statement
The study was approved by the Institutional Review Board of Third Hospital of Hebei Medical University in compliance with the Helsinki and an exemption from the informed consent was obtained. All data were anonymized before the analysis to safeguard patient privacy (W2021-046-1).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The present study was supported by a grant from the Key Project of Medical Research of Hebei Province (No. 20210561).
Disclosure
There are no competing interests.
References
1. Malt RA, McKhann C. Replantation of severed arms. JAMA. 1964;189:716–722. doi:10.1001/jama.1964.03070100010002
2. Barmparas G, Inaba K, Teixeira PG, et al. Epidemiology of post-traumatic limb amputation: a National Trauma Databank analysis. Am Surg. 2010;76(11):1214–1222. doi:10.1177/000313481007601120
3. Panagopoulou P, Antonopoulos CN, Dessypris N, et al. Epidemiological patterns and preventability of traumatic hand amputations among adults in Greece. Injury. 2013;44(4):475–480. doi:10.1016/j.injury.2012.10.008
4. Breahna A, Siddiqui A, Fitzgerald O’Connor E, et al. Replantation of digits: a review of predictive factors for survival. J Hand Surg Eur. 2016;41(7):753–757. doi:10.1177/1753193415624663
5. Bueno RA, Battiston B, Ciclamini D, et al. Replantation: current concepts and outcomes. Clin Plast Surg. 2014;41(3):385–395. doi:10.1016/j.cps.2014.03.010
6. Lima Jr JQ, Carli AD, Nakamoto HA, et al. Prognostic factors on survival rate of fingers replantation. Acta Ortop Bras. 2015;23(1):16–18. doi:10.1590/1413-78522015230101026
7. Dec W. A meta-analysis of success rates for digit replantation. Tech Hand Up Extrem Surg. 2006;10(3):124–129. PMID: 16974215. doi:10.1097/01.bth.0000225005.64605.17
8. Wang T, Xiong F, Tan JY, Qiu Y, Mi JY. Predictors for necrosis after single-digit replantation: a retrospective analysis of 946 patients. Plast Reconstr Surg. 2023;152(1):117–123. PMID: 36735820. doi:10.1097/PRS.0000000000010266
9. Zhang Z, Liu Y, Huang D, Huang Z. Single-cell WGCNA combined with transcriptome sequencing to study the molecular mechanisms of inflammation-related ferroptosis in myocardial ischemia-reperfusion injury. J Inflamm Res. 2024;17:6203–6227. PMID: 39281774; PMCID: PMC11397271. doi:10.2147/JIR.S476456
10. Bardallo RG, Chullo G, Alva N, et al. Mitigating cold ischemic injury: HTK, UW and IGL-2 solution’s role in enhancing antioxidant defence and reducing inflammation in steatotic livers. Int J Mol Sci. 2024;25(17):9318. PMID: 39273266; PMCID: PMC11394993. doi:10.3390/ijms25179318
11. Yu H, Wei L, Liang B, et al. Nonsurgical factors of digital replantation and survival rate: a meta-analysis. Indian J Orthop. 2015;49(3):265–271. doi:10.4103/0019-5413.156185
12. Kurklinsky AK, Kalsi H, Wysokinski WE, et al. Fibrin D-dimer concentration, deep vein thrombosis symptom duration, and venous thrombus volume. Angiology. 2011;62(3):253–256. PMID: 20834027. doi:10.1177/0003319710382416
13. Gok M, Kurtul A. A novel marker for predicting severity of acute pulmonary embolism: systemic immune-inflammation index. Scand Cardiovasc J. 2021;55(2):91–96. doi:10.1080/14017431.2020.1846774
14. Peng J, Wang H, Zhang L, et al. Construction and efficiency analysis of prediction model for venous thromboembolism risk in the elderly after hip fracture. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2021;46(2):142–148. doi:10.11817/j.issn.1672-7347.2021.190722
15. Gremmel T, Ay C, Seidinger D, et al. Soluble p-selectin, D-dimer, and high-sensitivity C-reactive protein after acute deep vein thrombosis of the lower limb. J Vasc Surg. 2011;54(6):48S–55S. doi:10.1016/j.jvs.2011.05.097
16. Rumley A, Emberson JR, Wannamethee SG, et al. Effects of older age on fibrin D-dimer, C-reactive protein, and other hemostatic and inflammatory variables in men aged 60-79 years. J Thromb Haemost. 2006;4:982–987. doi:10.1111/j.1538-7836.2006.01889.x
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Clinical Characteristics of Asymptomatic Thromboembolism in Psychiatric Inpatients: A Retrospective Study
Geng Y, Zhang P, Pan Y, Wang H, Chen Y, Lai J, Hu S
Neuropsychiatric Disease and Treatment 2024, 20:515-522
Published Date: 7 March 2024
D-Dimer Levels and NIHSS as Prognostic Predictors in Elderly Patients with Cerebral Infarction
Zheng Z
Clinical Interventions in Aging 2025, 20:505-511
Published Date: 26 April 2025

