Back to Journals » Journal of Pain Research » Volume 18
Risk Factors for Postoperative Pain in Pterygium Surgery Patients
Authors Yang G , Li Q , Tian M, Liu M, Zhang T, Guo W, Li Q
Received 24 December 2024
Accepted for publication 17 March 2025
Published 25 March 2025 Volume 2025:18 Pages 1607—1614
DOI https://doi.org/10.2147/JPR.S514070
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Karina Gritsenko
Guang Yang,1,* Qingyu Li,2,3,* Meiwen Tian,4,* Meimei Liu,4 Tinghui Zhang,4 Wenjun Guo,4 Qiang Li1
1School of Microelectronics, Tianjin University, Tianjin, 300072, People’s Republic of China; 2Department of Cataract, Tianjin Eye Hospital, Tianjin, 300020, People’s Republic of China; 3Tianjin Key Lab of Ophthalmology and Visual Science, Tianjin, 300020, People’s Republic of China; 4Shenzhen Eye Hospital, Shenzhen Eye Medical Center, Southern Medical University, Shenzhen, 518040, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Qiang Li, School of Microelectronics, Tianjin University, Tianjin, 300072, People’s Republic of China, Tel +8613820512683, Email [email protected] Wenjun Guo, Shenzhen Eye Hospital, Shenzhen Eye Medical Center, Southern Medical University, Shenzhen, 518040, People’s Republic of China, Tel +8613697406246, Email [email protected]
Purpose: Pterygium surgery is a common ophthalmological procedure, where effective management of postoperative pain is essential for ensuring patient satisfaction. This study aimed to investigate the risk factors for postoperative pain among Chinese patients undergoing pterygium excision surgery.
Patients and Methods: A total of 145 pterygium patients who underwent surgery from June 2020 to March 2021 at Shenzhen Eye Hospital were included. Anxiety levels were assessed using the Self-Rating Anxiety Scale before surgery, and pain levels were evaluated using the Numeric Rating Scale at various postoperative time points. Generalized linear model analysis was conducted with postoperative time-weighted average pain scores as the dependent variable and various potential risk factors as independent variables. These included traditional factors such as smoking history, alcohol history, ocular surgery history, and anxiety score as well as novel parameters like pterygium neck width, single- or double-headed pterygium, surgical corneal wound area, pterygium onset or recurrence, operating surgeon, congestion, pterygium invasion into the cornea, duration, graft conjunctival area, and preoperative pain score. We introduced the Shapley Additive exPlanations method to elucidate the contribution of these variables to time-weighted average pain scores.
Results: Among the 145 patients, 96 reported postoperative pain. No statistically significant differences were observed in baseline characteristics—such as age, sex, history of systemic diseases, smoking, alcohol use, and prior eye surgeries—between patients who experienced postoperative pain and those who did not. Anxiety scores, surgeon, pterygium neck widths, and preoperative pain scores were found to be significant risk factors for pain scores (p < 0.05).
Conclusion: Preoperative anxiety scores were positively correlated with pain scores. Significant differences in postoperative pain scores were observed among patients who underwent operations by different surgeons. Patients with wider pterygium neck widths experienced more severe postoperative pain. Higher preoperative pain scores were associated with more severe postoperative pain.
Keywords: pain management, preoperative anxiety, preoperative pain score
Introduction
Pterygium is a common ocular condition characterized by the growth of fibrovascular tissue originating from the conjunctiva on the cornea. Pterygium not only affects aesthetics but also leads to changes in corneal curvature and visual impairment.1 Severe cases of bilateral pterygium can result in blindness or loss of work capacity.2 The prevalence rate of pterygium ranges from 1.2% to 40% across different regions.3 The exact etiology of pterygium remains unclear, but factors such as ultraviolet radiation, tear film alterations, imbalances in cytokines and growth factors, immunological disorders, genetic mutations, and viral infections have been implicated.4 Risk factors for pterygium include old age, male sex, outdoor occupation, and rural living.5 Pterygium excision surgery is the primary treatment method for restoring visual acuity. Different surgical techniques are employed, including simple pterygium excision, pterygium excision with conjunctival grafting, pterygium excision with amniotic membrane transplantation, pterygium excision with the application of mitomycin C, and pterygium excision with limbal stem cell transplantation.6 Pterygium excision combined with conjunctival grafting significantly reduces the recurrence rate.1,7 In our study, we adopted pterygium excision combined with conjunctival transplantation to reduce the risk of postoperative pterygium recurrence. Corneal and conjunctival tissues are densely innervated with branches of the trigeminal nerve, making them highly sensitive.8 During surgery, local damage to the conjunctiva and cornea can result in varying degrees of postoperative pain, affecting patients’ quality of life and recovery. Pain is an unpleasant subjective sensation and emotional experience associated with actual or potential tissue damage.9 Postoperative pain can cause patient discomfort, and effective pain management is crucial for postoperative care. Currently, there is a lack of large-scale studies on postoperative pain assessment in patients who undergo pterygium surgery under local anesthesia. This study aimed to assess postoperative pain and associated risk factors in a large sample of pterygium patients receiving local anesthesia, thus providing insights for effective interventions. By identifying modifiable risk factors and analyzing their relative impact, this research highlighted actionable strategies for improving postoperative care. Furthermore, we utilized the Shapley Additive exPlanations (SHAP) interpretation tool to offer intuitive explanations for the factors influencing patients’ postoperative pain scores, enabling personalized pain management approaches to enhance patient outcomes and satisfaction.10
Materials and Methods
General Information
A total of 145 pterygium patients (51 males and 94 females) treated at Shenzhen Eye Hospital from June 2020 to March 2021 were included. The inclusion criteria were as follows: 1) aged ≥ 18 years, sex unspecified; and 2) diagnosed with pterygium in one or both eyes and planning to undergo pterygium excision under local anesthesia. This retrospective study adhered to the principles of the Helsinki Declaration and was approved by the Shenzhen Eye Hospital Medical Ethics Committee (Approval number: 2022-057-01). Informed consent was obtained from all participants. No stipend was provided.
Treatment Methods
Three days before surgery, patients started using levofloxacin eye drops (Huide Likang, Heze, Shandong, China, specification: 5 mL: 24.4 mg per vial) four times a day in both eyes. After routine disinfection and draping, we performed surface anesthesia using proparacaine hydrochloride eye drops (Youniter Nanjing Pharmaceutical Co., Ltd., Nanjing, Jiangsu, China, specification: 0.5%) in combination with subconjunctival injection of lidocaine hydrochloride (Hubei Tiansheng Pharmaceutical Co., Ltd., Chongqing, China, specification: 5 mL:0.1 g) at a volume of 0.5 mL for infiltration anesthesia at the pterygium neck and subconjunctival body. Depending on the degree of adhesion and thickness of the pterygium, we adopted corresponding surgical excision methods.7 We aligned the conjunctival flap with the corneal edge on the corneal edge side and sutured the conjunctival flap to the shallow sclera. After surgery, we applied tobramycin-dexamethasone ointment (S.A. Alcon-Couvreur n.v., Antwerp, Belgium, specification: 3.5 g, containing 10.5 mg tobramycin and 3.5 mg dexamethasone) to the operated eye and bandaged it. After surgery, patients were treated with tobramycin-dexamethasone eye drops (S.A. Alcon-Couvreur n.v., Antwerp, Belgium, specification: 5 mL), levofloxacin eye drops, and sodium hyaluronate eye drops (Shentian Pharmaceutical Co., Ltd., Suzhou, Jiangsu, China, specification: 5 mL:15 mg) in the operated eye four times a day for one month.
Observational Parameters
- Pain score: We used the Numeric Rating Scale, a scale from 0–10, where 0 represents no pain and 10 represents the most severe pain.11 We recorded preoperative pain levels and pain levels at 0 h, 1 h, 2 h, 4 h, 6 h, 8 h, 10 h, and 24 h after surgery. A time-weighted average pain score was used to estimate a patient’s mean 24 h postoperative pain score, taking into account the irregular time intervals of pain measurements.12
- Anxiety score: We evaluated patients’ preoperative anxiety using the Self-Rating Anxiety Scale (SAS).13 The Numeric Rating Scale and Self-Rating Anxiety Scale are widely used and publicly available tools, and no special permissions are required for their use in this study.
- Surgical factors: Information on the operating surgeon, and pterygium type (primary or recurrent) was recorded.
- Surgical parameters: Data on pterygium neck width, pterygium invasion into the cornea, surgical corneal wound area, graft conjunctival area, and whether the pterygium was single- or double-headed were collected.
- General Information: Patient age, sex, medical history, smoking history, alcohol history, and ocular surgery history were recorded.
Statistical Analysis
We used SPSS 26.0 or python 3.10.13 to conduct statistical analyses. A Mann–Whitney U-test or a chi-squared test was used to compare categorical data. We conducted a generalized linear model analysis with time-weighted average pain scores as the dependent variable and various independent variables as mentioned above. Python (SHAP) was utilized to generate SHAP plots illustrating the contribution of variables to the model. The model outcomes were interpreted by assessing the impact of different influential factors on the predicted results.14 A P value < 0.05 was considered to indicate statistical significance.
Results
Baseline Characteristics
A total of 145 patients participated in the study, 96 of whom reported postoperative pain. There were no statistically significant differences in baseline characteristics between patients who experienced postoperative pain and those who did not. The baseline data, including age, sex, history of systemic diseases, smoking, alcohol use, and prior eye surgeries, are shown in Table 1.
 |
Table 1 Descriptive Analysis of the Baseline Characteristics of 145 Patients with Pterygium |
Generalized Linear Model Analysis
A generalized linear model was constructed with the following independent variables: congestion, anxiety score, operating surgeon, pterygium onset or recurrence, single- or double-headed pterygium, pterygium neck width, pterygium invasion into the cornea, surgical corneal wound area, graft conjunctival area, duration, smoking history, alcohol history, ocular surgery history, and preoperative pain score. The model revealed that the factors affecting the pain scores were the anxiety score (P = 0.004), the operating surgeon (P = 0.001), the pterygium neck width (P = 0.046), and the preoperative pain score (P < 0.001). As illustrated in Table 2 and Table 3, preoperative anxiety scores were positively correlated with time-weighted average pain scores. The higher the preoperative anxiety score was, the more severe the postoperative pain. There were significant differences in time-weighted average pain scores among patients who underwent surgery performed by different surgeons. Patients with wider pterygium neck widths experienced more severe postoperative pain. As the preoperative pain score increased, the time-weighted average pain score became more pronounced, indicating a positive correlation between preoperative pain and postoperative pain. The ocular surgery history exhibited a near-significant impact (P = 0.053) on the postoperative pain score, implying a potential influence on postoperative pain levels (Table 2).
 |
Table 2 Generalized Linear Model Analysis |
 |
Table 3 Generalized Linear Model Analysis of Influencing Factors of Postoperative Pain in 145 Patients with Pterygium |
Model Interpretability
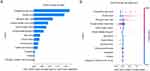
To visually elucidate the aforementioned variables, we utilized SHAP to illustrate their impact on the time-weighted average pain score. Given the multitude of surgeons performing pterygium surgeries, the SHAP chart encompassed 13 variables in addition to the surgeons to prevent overshadowing other pertinent factors. Notably, Figure 1A presented the ranking of these 13 variables based on their average absolute SHAP values, with the X-axis illustrating the SHAP values for predicting the model’s importance. In Figure 1B, each variable was depicted by a significant line, showcasing its effect on postoperative pain through differently colored dots—red denoting high-risk values and blue representing low-risk values. This visualization not only highlighted the direction of each variable’s impact but also conveyed the magnitude of influence, offering a clear explanation of how specific factors contribute to postoperative pain. Notably, Figure 1B highlighted that a higher preoperative pain score, elevated anxiety score, and wider neck width of pterygium contributed to an increased postoperative pain score.
Discussion
Pterygium surgery is a routine ophthalmological procedure, where effective management of postoperative pain is crucial for ensuring patient comfort and satisfaction. In our study, we aimed to identify factors influencing postoperative pain in pterygium surgery patients under local anesthesia, with the goal of offering insights into effective pain management strategies. Surgeon-related factors significantly influenced postoperative pain scores, likely due to differences in surgical techniques and perioperative management. Precise surgical maneuvers that minimize tissue trauma and individualized pain management strategies may reduce postoperative pain. This highlights the need for standardizing surgical protocols and promoting best practices to ensure consistent and optimal patient outcomes.
Interestingly, a wider pterygium neck width was associated with more severe postoperative pain. However, pterygium invasion into the cornea and surgical corneal wound area had no effect on postoperative pain. Loss of limbal stem cells occurred in the neck area of the pterygium.15 A pterygium with a wider neck may result in the loss of limbal stem cells, thereby affecting the speed and quality of eye tissue healing, and consequently influencing the perception of postoperative pain.
We observed that higher preoperative pain scores were linked to more severe postoperative pain. Studies have found that preoperative pain is a risk factor for postoperative pain.16 Patients with chronic pain have increased sensitivity to peripheral pain receptors due to increased release of inflammatory mediators such as prostaglandins and growth factors.17
We discovered that preoperative anxiety scores were positively correlated with postoperative pain scores. Anxiety is one of the most prevalent psychological reactions among patients before surgery. Higher levels of preoperative anxiety can result in adverse psychological and physiological effects, influencing anesthesia, postoperative care, and the therapeutic recovery process.18 Psychological factors such as depression and anxiety can increase the risk of high postoperative pain levels, prolonged opioid use, and chronic postoperative pain.19 Patients with severe preoperative anxiety can benefit from psychological counseling, or short-term use of anxiolytic medications to alleviate their anxiety. Preoperative anxiety in patients can be alleviated through cognitive therapy, music therapy, and relaxation techniques, which may, in turn, reduce postoperative pain.20,21
Interestingly, the ocular surgery history exhibited a near-significant impact on the postoperative pain scores. Patients with prior surgical experience may exhibit lower postoperative pain scores attributed to decreased anxiety and stress levels, resulting from their increased familiarity with the surgical process. Another plausible explanation was that individuals with prior eye surgeries may have developed a heightened tolerance for ocular discomfort, thereby perceiving the pain as less severe. However, further research is warranted to fully elucidate its effects.
We applied the SHAP method to the regression model to elucidate significant variables associated with postoperative pain. Overall, our study offers valuable insights into the factors influencing postoperative pain in pterygium surgery patients and underscores the significance of addressing preoperative anxiety. Tailoring pain management strategies based on individual patient profiles and ensuring consistent surgical techniques among different surgeons can significantly enhance postoperative comfort and satisfaction.
This study has several limitations. First, this was a single-center study, which may restrict the generalizability of the findings. Second, postoperative pain is subjective, and individual pain thresholds and perceptions can vary widely. Although we utilized standardized pain assessment tools, the subjective nature of pain reporting may introduce some bias. Third, while we identified factors associated with postoperative pain, preoperative pain was reported by 24.2% of participants. Additionally, we did not assess the long-term outcomes of pterygium surgery, such as recurrence rates, which could also influence patients’ postoperative experiences.
Conclusion
This study identified several key risk factors influencing postoperative pain in Chinese patients undergoing pterygium surgery. Preoperative anxiety levels were positively correlated with postoperative pain severity, highlighting the potential benefits of psychological interventions to alleviate anxiety and subsequently reduce postoperative pain. Practical strategies such as preoperative counseling, mindfulness training, or short-term use of anxiolytic medications could be considered to address anxiety effectively.
Surgeon-related factors significantly impacted postoperative pain scores, emphasizing the importance of standardizing and optimizing surgical techniques to minimize ocular tissue trauma. Training programs focusing on microsurgical skills and uniform surgical protocols may help reduce variability in outcomes among surgeons.
Additionally, patients with wider pterygium neck widths experienced more severe postoperative pain, possibly due to the loss of limbal stem cells in the neck area, which affects the speed and quality of tissue healing. For these patients, a more cautious surgical approach or enhanced postoperative care, such as the use of tissue-protective agents and closer follow-up, may help alleviate pain and promote recovery.
Furthermore, higher preoperative pain scores were associated with increased postoperative pain, likely due to heightened sensitivity to pain caused by chronic pain conditions. For such patients, preoperative identification and tailored pain management plans, including multimodal analgesia, could be beneficial.
Although our study offers valuable insights, it is limited by its single-center design, which may restrict the generalizability of the findings. The subjective nature of pain and individual variability in pain perception could introduce bias, despite the use of standardized pain assessment tools. Additionally, the study did not assess long-term outcomes, such as recurrence rates, which could also influence postoperative experiences.
This study underscores the importance of integrating psychological assessment into preoperative evaluations, adopting standardized surgical techniques, and tailoring pain management strategies to individual patient profiles. Implementing these measures could significantly enhance postoperative comfort and satisfaction. Future research should include multicenter studies to improve the generalizability of the findings and explore the impact of long-term outcomes on postoperative pain experiences.
Abbreviations
SHAP, Shapley Additive exPlanations; SAS, Self-Rating Anxiety Scale.
Data Sharing Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study adhered to the principles of the Helsinki Declaration and was approved by the Shenzhen Eye Hospital Medical Ethics Committee (Approval number: 2022-057-01). Informed consent was obtained from all participants.
Acknowledgment
We thank all members of the included studies for their contribution.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Tianjin Natural Science Foundation (Grant No. 22JCZDJC00220), the Foundation of State Key Laboratory of Ultrasound in Medicine and Engineering (Grant No. 2022KFKT004) and the Postgraduate Research Innovation Project of Tianjin, China under Grant No.2021YJSB118.
Disclosure
The author(s) report no conflicts of interest in this work.
References
1. Shahraki T, Arabi A, Feizi S. Pterygium: an update on pathophysiology, clinical features, and management. Therapeutic Adv Ophthalmol. 2021;13:25158414211020152. doi:10.1177/25158414211020152
2. Chu W, Choi H, Bhat A, Jhanji VJE. Pterygium: new insights. Eye. 2020;34(6):1047–1050. doi:10.1038/s41433-020-0786-3
3. Hashemi H, Khabazkhoob M, Yekta A, Jafarzadehpour E, Ostadimoghaddam H, Kangari H. The prevalence and determinants of pterygium in rural areas. J Curr Ophthalmol. 2017;29(3):194–198. doi:10.1016/j.joco.2016.09.002
4. Malozhen S, Trufanov S, Krakhmaleva D. Pterygium: etiology, pathogenesis, treatment. Vestnik oftalmologii. 2017;133(5):76–83. doi:10.17116/oftalma2017133576-83
5. Rezvan F, Khabazkhoob M, Hooshmand E, Yekta A, Saatchi M, Hashemi H. Prevalence and risk factors of pterygium: a systematic review and meta-analysis. Surv Ophthalmol. 2018;63(5):719–735. doi:10.1016/j.survophthal.2018.03.001
6. Patel ED, Rhee MK. Surgical techniques and adjuvants for the management of pterygium. Eye Contact Lens. 2022;48(1):3–13.
7. Palewski M, Budnik A, Konopińska J. Evaluating the efficacy and safety of different pterygium surgeries: a review of the literature. Int J Environ Res Public Health. 2022;19(18). doi:10.3390/ijerph191811357
8. Sacchetti M, Lambiase A. Neurotrophic factors and corneal nerve regeneration. Neural Regen Res. 2017;12(8):1220–1224. doi:10.4103/1673-5374.213534
9. Raja SN, Carr DB, Cohen M, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020;161(9):1976–1982. doi:10.1097/j.pain.0000000000001939
10. Lei T, Guo J, Wang P, et al. Establishment and validation of predictive model of Tophus in Gout Patients. J Clin Med. 2023;12(5):1755. doi:10.3390/jcm12051755
11. Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl 1):S17–24.
12. Ryu K, Michael GN, Kenneth CR, et al. Acute pain burden and opioid dose requirements after cesarean delivery in parturients with preexisting chronic back pain and migraine. Anesthesiol Research Practice. 2021;2021:3305579.
13. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. 1971;12(6):371–379. doi:10.1016/S0033-3182(71)71479-0
14. Lundberg SM, Lee S-I. A unified approach to interpreting model predictions.
15. Medical Advisory Secretariat. Limbal stem cell transplantation: an evidence-based analysis. Ontario Health Technol Assessment Series. 2008;8(7):1–58.
16. Yang MMH, Hartley RL, Leung AA, et al. Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ open. 2019;9(4):e025091. doi:10.1136/bmjopen-2018-025091
17. Gangadharan V, Kuner R. Pain hypersensitivity mechanisms at a glance. Dis Model Mech. 2013;6(4):889–895. doi:10.1242/dmm.011502
18. Zemła AJ, Nowicka-Sauer K, Jarmoszewicz K, Wera K, Batkiewicz S, Pietrzykowska M. Measures of preoperative anxiety. Anaesthesiol Intensive Ther. 2019;51:64–69. doi:10.5603/AIT.2019.0013
19. Doan LV, Blitz J. Preoperative assessment and management of patients with pain and anxiety disorders. Curr Anesthesiol Rep. 2020;10(1):28–34. doi:10.1007/s40140-020-00367-9
20. Stamenkovic D, Rancic N, Latas M, et al. Preoperative anxiety and implications on postoperative recovery: what can we do to change our history. Minerva anestesiologica. 2018;84(11):1307–1317. doi:10.23736/S0375-9393.18.12520-X
21. Armstrong AD, Hassenbein SE, Black S, Hollenbeak CS. Risk factors for increased postoperative pain and recommended orderset for postoperative analgesic usage. Clin J Pain. 2020;36(11):845–851. doi:10.1097/AJP.0000000000000876
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.