Back to Journals » Journal of Pain Research » Volume 18
Risk Factors for the Occurrence of Rebound Pain After Intercostal Nerves Block in Three-Port Thoracoscopic Surgery: A Case-Control Study
Authors Wan C, Kong M, Shen Q , Lu W, Shen X
Received 6 October 2024
Accepted for publication 13 January 2025
Published 23 January 2025 Volume 2025:18 Pages 381—390
DOI https://doi.org/10.2147/JPR.S494568
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jinlei Li
Chongyang Wan,1,2 Min Kong,2 Qihong Shen,2 Weina Lu,1,2 Xu Shen2
1Jiaxing University Master’s Degree Cultivation Base, Zhejiang Chinese Medical University, Jiaxing City, Zhejiang Province, People’s Republic of China; 2Department of Anesthesiology and Pain Research Center, The Affiliated Hospital of Jiaxing University, Jiaxing City, Zhejiang Province, People’s Republic of China
Correspondence: Xu Shen, Medical Center for Anesthesia and Pain, First Hospital of Jiaxing, 1882 Zhonghuan South Road, Nanhu District, Jiaxing City, Zhejiang Province, People’s Republic of China, Email [email protected]
Background and Objectives: Rebound pain (RP), characterised by an acute increase in pain levels, is usually observed after the effects of block anaesthesia have subsided. Severe RP can cause adverse effects, thus affecting patient prognosis. In this study, we investigated the incidence of RP and its risk factors after intercostal nerve block in three-port thoracoscopic surgery to provide a clinical basis for identifying high-risk patients and providing early intervention.
Methods: A single-centre retrospective study was conducted on 475 patients who underwent three-hole thoracoscopic surgery from September 2022 to September 2023 in Jiaxing First Hospital. Data were collected and compared between patients who developed RP and those who did not. IBM SPSS Statistics 25.0 software was used for statistical analysis.
Results: Data were collected from 700 patients. After applying the exclusion criteria, 475 cases were finally included and the incidence of RP was 23.8%. The results showed that the differences in body mass index (BMI), upper and lower chest diameters, anterior and posterior chest diameters, left and right chest diameters, and gender between patients with RP and those without RP were statistically significant (p < 0.05). In addition, the proportion of female patients with RP was significantly higher. BMI (advantage ratio [OR] = 0.835, 95% confidence interval [CI]: 0.375 ~ 1.859), upper and lower chest diameters (OR = 0.916, 95% CI: 0.827 ~ 1.014), anterior and posterior chest diameters (OR = 0.765, 95% CI: 0.635 ~ 0.921), left and right chest diameters (OR = 0.612, 95% CI: 0.421 ~ 0.891), and gender (OR = 1.170, 95% CI: 0.576 ~ 2.373).
Conclusion: The incidence of RP after three-hole thoracoscopic intercostal nerve block is high and associated with multiple risk factors. Early intervention is needed for patients at risk of RP to improve patient prognosis and satisfaction.
Keywords: intercostal nerve block, rebound pain, regional block anesthesia, thoracoscopic surgery
Introduction
With the introduction and implementation of the concept of enhanced recovery after surgery, peripheral nerve block (PNB), a crucial component of multimodal analgesia, has gained prominence because of its efficacy in reducing perioperative opioid consumption and shortening postoperative hospital stay. However, post-PNB rebound pain (RP) is commonly observed in patients when the analgesic effect wears off, thereby increasing the need for opioids, which reduces or negates the overall benefit of PNB.1 The incidence of severe RP after epidural analgesia for video-assisted thoracic surgery (VATS) is approximately 22%.2 In a large retrospective study, of the 972 outpatients receiving PNB, 482 experienced severe RP (approximately 50%).3 RP, that is, acute postoperative pain after the disappearance of regional block anesthesia effects, has recently garnered increasing research attention in terms of its exact definition, pathological mechanisms, associated risk factors, and preventive and curative measures.4 Several studies have attempted to define RP after regional block anesthesia.5 In 2019, based on the mechanism of RP occurrence, Dada et al (2019) defined RP as a nociceptive hypersensitivity state occurring 8–24 h after local block anesthesia.6 Belete et al defined RP as the change from good pain control at surgery to severe pain within 24 h of surgery.7 It is the sudden onset of substantial mechanosurgical pain induced by nonconfrontational injurious inputs after the regional nerve block effect has subsided.8 Many patients undergoing regional block anesthesia, either as the sole anesthetic technique or in combination with general anesthesia or sedation, experience severe pain after the sensory nerve block is released.9 This pain may reduce or even negate the overall benefit of PNB.6 Currently, domestic and international studies have investigated the incidence and risk factors associated with RP after abdominal surgery, spinal surgery, outpatient surgery combined with PNB, and VATS involving epidural analgesia. However, reports on the incidence of RP and the associated risk factors after intercostal nerve block in thoracic surgery are lacking.2,3,10,11
According to statistics, approximately 70% of thoracic surgeries are performed under VATS, with most performed under general anesthesia combined with regional block anesthesia. Chest drains are routinely left in place for drainage during the postoperative period.12 Postoperative analgesics routinely used in thoracic surgery by anesthesiology departments are thoracic epidural analgesia (TEA), thoracic paravertebral block, and intercostal nerve block.13 Most open-heart surgeries are compounded with TEA for controlling postoperative pain. Recently, intercostal nerve block has become increasingly common in VATS surgeries because of the ease of its execution. It is routinely combined with intercostal nerve block for analgesia in thoracic surgeries at our institution. Although intercostal nerve block may be associated with lower pain scores in the early postoperative period, the effects may persist for a limited duration. Fewer clinical studies have investigated the time and degree of gradual diminution of the effect of intercostal nerve block and whether RP has any risk or specificity, warranting more in-depth studies on this topic.
Materials and Methods
The study was approved by the local research ethics committee (reference number: 2023-KY-237). The clinical registration number was ChiCTR2400083935. This single-center, retrospective observational study was conducted in the Department of Anaesthesiology, Jiaxing University Hospital, Jiaxing, People’s Republic of China. We collected the electronic medical records of 700 patients who underwent three-port thoracoscopic surgery with intercostal nerve blocks at the First Hospital of Jiaxing from September 2022 to September 2023. Patients’ general information and that of their diagnostic history and treatment plan were obtained by searching their records. RP was defined as the change from good pain control at surgery to severe pain 24 h after surgery. Good pain control was defined as the last postanesthesia care unit (PACU) pain score recorded after PNB. However, if the patient was not in the PACU, the pain score was recorded immediately before leaving the operating room. The change to severe pain within 24 h after surgery was defined as the sudden onset of pain at 24 h after surgery that either interfered with the patients’ sleep or required them to seek surgeon’s support.
Inclusion and Exclusion Criteria
In this study, we included 18- to 75-year old patients who underwent elective thoracoscopic lung surgery with intercostal nerve block analgesia under general anesthesia in our hospital, whose complete clinical data were available, and who scored American Society of Anesthesiology (ASA) class I–III.
We excluded patients experiencing an imperfect analgesic effect of the intercostal nerve block; patients with mental illness or inability to correctly and effectively identify their feelings; patients with long-term chronic pain; those who changed the operation mode during the operation, such as thoracoscopic surgery was changed to open surgery; those who encountered severe complications after the operation and were admitted to the intensive care unit; those who withdrew or lost of follow-up visits; those who used other analgesic drugs during the study period; those who violated the analgesic protocol of this study; those who were taken out of service during the period of using analgesic pumps due to clogging of the line in the middle of the process; those who experienced malfunctioning of analgesic pumps; and those in whom the use of analgesic pumps had to be discontinued within 24 h of the occurrence of postoperative adverse reactions.
After applying the exclusion criteria, the data of 475 patients were finally included in the study. These patients were finally divided into two groups: those who experienced RP and those who did not.
Follow-Up
Eligible patients identified on the basis of the electronic inpatient medical record were followed up by telephone to obtain information about the occurrence of RP after surgery, such as incidence and time of occurrence.
Data Collection
Data were extracted from the hospital’s electronic database and from patients’ responses to the daily telephonic follow-up questionnaire. Regarding postoperative follow-up, all patients received follow-up telephone calls from the anesthetist daily, starting approximately 24 h after surgery. During this follow-up, relevant data regarding clinical pain and pain management measures were recorded.
Risk Factor Variables
Patients’ baseline data were collected, and potential risk factors were assessed (Table 1). Some of these risk factors were associated with postoperative pain, including patients’ age, body mass index (BMI), gender, comorbidities (hypertension/diabetes mellitus), duration of surgery, and thoracic size (anteroposterior diameters, right and left diameters, and upper and lower meridians). The operation time was calculated as the end time of the patient’s operation minus the start time of the operation, as noted in the anesthesia record sheet. The anteroposterior thoracic diameters were the maximum of the values measured from the anterior to posterior in the aortic plane on the affected side of the patient, as observed on the most recent preoperative computed tomography (CT) scan. The upper and lower thoracic diameters were the maximum of the values measured from the apex of the lungs to its base on the affected side of the patient, as observed on the most recent preoperative CT scan. The right and left thoracic diameters were half of the maximum of the values measured from the left to right in the aortic plane on the affected side of the patient, as observed on the most recent preoperative CT scan.
 |
Table 1 Basic Information of Respondents |
Outcome Variable
In this study, the primary outcome variable was the incidence of RP. RP was defined as a dramatic change from well-controlled pain within 12–24 h of nerve block release to pain 24 h after surgery. Although severe pain is sudden and severe after PNB subsides, no threshold RPS value was determined for patients with RP.8,14 In a study investigating factors associated with RP after PNB release following major outpatient surgery, the incidence of RP was measured by evaluating the change from mild pain (NRS pain score = 3) at the time of the last measurement of block onset to severe pain (NRS pain score = 7) within 24 h of PNB release.3 Considering that all the present study patients were inpatients and had used sufentanil (100 μg) + ondansetron (8 mg/100 mL), with no background dosage for postoperative analgesia, the incidence of RP was measured by evaluating the change from mild pain at the time of the last measurement of block onset (NRS pain score <3) to moderately severe pain (NRS pain score ≥ 4). All patients were free of residual numbness at 24-h follow-up. The discharge criterion for the PACU patients was adequate pain control (NRS < 3 or patient-reported satisfactory pain control).
Statistical Methods
Statistical analyses were performed using IBM SPSS Statistics 25.0 (IBM Corporation) software. Continuous variables are expressed as the mean [SD] or quartile. The two-sample t-test was employed to analyze normally distributed data, and the Mann–Whitney U-test was conducted to analyze data without normal distribution. Categorical variables are expressed as counts and percentages. Comparative analyses were performed using the chi-square test or Fisher’s exact probability method. RP-associated risk factors were analyzed through multifactorial logistic regression. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. A p value < 0.05 was considered statistically significant.
Results
Basic Patient Information
In this survey, we included a total of 475 patients, of which 113 had RP, accounting for 23.8% of the total. Among the 279 female patients included in the study, 79 (28.3%) experienced RP, whereas 34 of 196 male patients (17.3%) had RP. In the total study population, 43 of the 172 patients with hypertension experienced RP (25.0%); 70 of the 303 patients without hypertension had RP (23.1%); 17 of the 61 patients with diabetes had RP (27.9%); 96 of the 414 patients without diabetes had RP (23.8%); 17 of the 61 patients with pain experienced RP (27.9%); 101 of the 417 patients with ASAII had RP (24.1%); 12 of the 58 patients with ASAIII experienced RP (20.7%); 43 of the 200 patients in whom the left side was affected had RP (21.5%); 70 of the 275 patients in whom the affected side was the right side had RP (25.5%); 87 of the 348 patients aged age <66 years experienced RP (25.0%); 26 of the 127 patients aged ≥66 years experienced RP (20.5%); 105 of the 417 patients with preoperative blood glucose levels of ≤6.9 mmol/L had RP (25.2%); and three of the 28 patients with preoperative blood glucose levels of had RP (10.7%). Table 1 presents the basic characteristics of the patients.
Univariate Analysis of the Factors Affecting RP Occurrence
The chi-square test was used to analyze the difference between patients with and without RP in terms of seven indicators (Table 2). The two groups did not differ significantly in terms of hypertension, diabetes mellitus, gender, affected side, ASA grading, age, and preoperative blood glucose levels (p > 0.05). Among these factors, gender was found to be associated with the occurrence of RP (p < 0.05), and the percentage of female patients with RP was significantly higher than that of male patients with RP.
 |
Table 2 Univariate Analysis of Categorical Variables |
Ten indicators were analyzed using the independent samples t-test (Table 3). Height (t = 2.214, p < 0.05), weight (t = 3.615, p < 0.05), BMI (t = 2.868, p < 0.05), upper and lower thoracic diameters (t = 2.299, p < 0.05), anteroposterior diameters (t = 4.381, p < 0.05) (t = 4.381, p < 0.05), and left and right diameters (t = 5.089, p < 0.05) differed significantly between patients with and without RP. Other factors such as the length of hospital stay (t = −1.202, p = 0.230), age (t = 0.759, p = 0.448), length of surgery (min) (t = −0.389, p = 0.697), and preoperative blood glucose (mmol/L) (t = 1.555, p = 0.121) did not differ significantly between the two groups.
 |
Table 3 One-Way Analysis of Continuous Variables |
Logistic Regression Analysis
Considering the occurrence of RP as the outcome, the probability of RP after three-port thoracoscopic surgery following intercostal nerve block release was 23.8%. Seven significant factors identifying using the univariate analysis were selected and established as independent variables. The values of categorical variables were assigned as shown in Table 4. Incidence of RP was set as a dependent variable (0 = no RP, 1 = RP occurred). Logistic regression was adopted to analyze potential risk factors for RP incidence (Table 5).
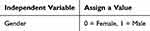 |
Table 4 Assignment of Factors Influencing Rebound Pain |
 |
Table 5 Multifactorial Logistic Regression Analysis of Factors Influencing Rebound Pain Incidence in Patients |
Forest plot of the multivariate logistic regression analysis of factors associated with the incidence of RP (Figure 1). The error bars represent 95% CIs; error bars to the left or right of the x = 1.0 axis indicate that a given factor protects against or is a risk factor for pain, respectively; error bars across the x = 1.0 axis indicate no significant difference between the factors for pain (no significant difference in the pain risk).
 |
Figure 1 Forest plot of the multivariate logistic regression analysis of factors associated with the incidence of RP. |
The results of the multifactorial analysis showed that the anteroposterior and left and right thoracic diameters were protective factors for pain. Each unit increase in the anteroposterior thoracic diameters decreased the probability of the RP by approximately 23.5%, and each unit increase in the left and right thoracic diameters decreased the probability of RP by approximately 38.8%.
Discussion
In this retrospective study, we found that RP occurred in approximately 23% patients who underwent thoracic surgery. One-way analysis of variance was conducted to examine variables with significant differences between the patients with and without RP, and logistic regression was used to further identify variables significantly associated with RP. The anteroposterior and left and right thoracic diameters were protective factors for the occurrence of RP. Each unit increase in anteroposterior thoracic diameters decreased the probability of RP by approximately 23.5%, and each unit increase in the left and right thoracic diameters decreased the probability of RP by approximately 38.8%. Additionally, the occurrence of RP differed significantly between male and female patients, indicating a close association between sex and RP incidence in patients, with the percentage of female patients experiencing RP being significantly higher than that of male patients with RP.
Compared with the recent large retrospective study in which the incidence of RP after a single PNB was approximately 50%,3 the incidence of RP after intercostal nerve block was 23% in the present study. In our hospital, postoperative analgesia is routinely provided using analgesic pumps on postoperative day 1. Moreover, surgeons routinely administer oral medications, such as ketorolac tromethamine BID or aminophenol hydrocodone TID, for postoperative analgesia. A significant increase in pain intensity and opioid requirements is frequently observed in patients experiencing RP at 24 h after postoperative analgesia. Despite adequate postoperative analgesic management, RP was noted in 20%–30% of the study patients, and postoperative analgesia with sufentanil 100 μg + ondansetron 8 mg/100 mL, a background-free dose, could not adequately control RP. Furthermore, an appropriate management strategy for RP after nerve block remains to be developed. The incidence and risk factors for RP after PCEA discontinuation have been evaluated in a previous study; however, the study involved thoracoscopic surgical patients who had undergone PCEA, and not patients receiving intercostal nerve blocks.
In the present study, the univariate analysis revealed that six factors, namely hypertension, diabetes mellitus, gender, affected side, ASA classification, age, and first intraoperative blood glucose levels did not differ significantly between the RP and non-RP groups. Other factors such as the length of hospital stay (t = −1.202, p = 0.230), age (t = 0.759, p = 0.448), duration of surgery (min) (t = −0.389, p = 0.697), and intraoperative first blood glucose (mmol/L) (t = 1.555, p = 0.121) also exhibited no significant association with RP incidence. By contrast, height (t = 2.214, p < 0.05), weight (t = 3.615, p < 0.05), BMI (t = 2.868, p < 0.05), upper and lower thoracic diameters (t = 2.299, p < 0.05), anteroposterior diameters (t = 4.381, p < 0.05), and left and right diameters (t = 5.089, p < 0.05) differed significantly between patients with and without RP. Seven factors exhibiting statistically significant differences between the two patient groups, as determined through the univariate analysis, were selected as independent variables. Logistic regression was performed to analyze the factors that might affect RP incidence. The anteroposterior and right and left thoracic diameters were protective factors for the occurrence of RP. The probability of RP reduced by approximately 23.5% for each unit increase in the anteroposterior thoracic diameters and by approximately 38.8% for each unit increase in the right and left thoracic diameters. This suggests that the anatomical size of the thorax is closely related to the occurrence of postoperative RP.
In addition, sex was identified as a significant factor for the occurrence of RP in this study, with the percentage of female patients with RP being significantly higher. Studies have identified three non-modifiable patient and surgical risk factors for RP, namely younger age, female gender, and bone surgery.3 Our finding indicating a significantly higher proportion of female patients with RP is consistent with those of previous studies. Female sex is an independent risk factor for RP development. In various surgical procedures, women are at an increased risk of experiencing postoperative pain.15,16 Gender differences in pain perception are related to complex psychosocial and biological factors, such as women’s greater willingness to communicate regarding their pain and subjective pain experiences. Although gender is an immutable risk factor for RP in the postoperative period, these characteristics remain crucial for optimizing pain management in the perioperative period in patients with relevant risk factors.
RP has recently been introduced as a term for describing acute pain that begins after the regional anesthesia-associated sensory block has worn off. RP has various definitions, and, to date, no consensus has been formed on a formal definition of RP.9 RP has not been universally accepted as a distinct pain phenomenon. One can argue that the sudden onset of typical injurious pain is a consequence of revealing inadequate multimodal analgesia.17 Multimodal analgesic approaches are currently used for postoperative pain management, including acetaminophen, nonsteroidal anti-inflammatory analgesics, opioids, and PNBs. PNB plays a crucial role in anesthesia and postoperative multimodal analgesia for extremity surgery.18 PNB offers multiple benefits in various surgeries, including good early analgesia, a high safety profile, reduced opioid consumption, better early postoperative pain control, and earlier discharge from the hospital.19,20 Current studies have suggested that regional block anesthesia is effective in the first 6–8 h after administration.3 However, after the anesthetic effects wear off, pain may rebound, and sometimes, this pain may be worse than that before the operation.21 This severe pain sets in rapidly, thus counteracting measures that offer adequate analgesia, such as non-opioid multimodal systemic and local analgesia.22 RP after regional block anesthesia, characterized by nociceptive hypersensitivity, occurs less frequently in the PACU, and it suddenly intensifies and become intolerable after the patient is shifted from the PACU to the ward, reducing the quality of postoperative recovery as well as patients’ satisfaction.23 The outcome of treatment of severe RP with conventional non-opioid medications is poor because of the different action mechanisms of drugs involved. Patients who experience severe RP during three-port thoracoscopic surgery usually exhibit various behavioral responses such as limb tremors, strong vocal responses, and attempts to remove the chest tube.2 These responses may increase the risk of postoperative complications, such as surgical incision splitting, bleeding from the surgical site, wound suture breakage, and dislodgement of various catheters. It may also lead to cardiovascular system complications such as elevated blood pressure, increased heart rate, and cardiac arrhythmias. Patient with RP may also agitate during the awakening period and experience postoperative delirium and increased pain, leading to a prolonged hospital stay. Moreover, in mostly elderly patients, lung masses10 are often combined with cardiopulmonary insufficiency, reduced arterial elasticity, myocardial and autonomic function, severe pain, and psychological burden. These can easily cause hemodynamic instability, and even cardiovascular and cerebrovascular accidents, thereby endangering health of the elderly patients.12 Therefore, anesthesiologists and surgeons should consider the cases of RP seriously, carefully weighing the pros and cons of nerve blocks before finalizing a treatment plan.
The characteristics of RP experienced by the patients were as follows: (1) acute in nature, (2) occurred after PNB effect had subsided, and (3) clinically significant in terms of intensity and impact on psychological well-being, quality of recovery, and activities of daily living.24 RP often occurs at night, but this may be because most single PNB injections last 8–12 h, and most elective surgeries are performed during the daytime.8 RP is also often described as “burning” in nature, but it lacks other neuropathic features such as anomalous pain, which typically occurs 12–24 h after the PNB is administered. However, sometimes, predicting the exact time at which the blocking effect wears off is difficult. RP intensity usually remains high for 2–6 h, but the subsequent pain trajectory is constant with the expected recovery and healing process after a surgical injury.25 Understandably, RP is a distressing situation, significantly affecting the total amount of analgesics used, patient satisfaction, and recovery.26 Severe RP can increase opioid requirements in patients, thereby increasing the risk of opioid-related adverse drug events.27 The possible pathophysiological mechanisms underlying the occurrence of RP after regional anesthesia are as follows: abnormal spontaneous overexcitation of specific nerve fibers, tissue injury-induced local inflammatory response, and surgical injury triggering abnormal sensory remodeling of the central nervous system.28,29 These proposed mechanisms remain hypothetical currently, warranting further studies to gain a deeper understanding.
Patients who develop RP postoperatively can be treated with a combination of pharmacological and psychotherapeutic interventions. Additionally, they should be informed preoperatively of the possibility of RP to avoid disputes.
Currently, specific treatments for RP are still insufficient. In order to reduce the occurrence of RP, a combination of preoperative education, multimodal combined analgesic strategies, and psychological interventions can be considered. Preoperative education can help patients understand the surgical and analgesic process, thus reducing postoperative anxiety and pain; multimodal analgesic strategies can improve the analgesic effect through the use of different analgesic drugs in combination with peripheral nerve block techniques; and psychological interventions can help patients to adjust their perception of and response to pain. Future research should focus on exploring the mechanism of rebound pain after nerve block in order to develop individualised treatment plans. There is also a need to explore new therapeutic tools, to promote the progress of clinical research, and to apply new technologies to improve the understanding of RP so that more specific and effective treatments and strategies can be provided.
Limitations
This study has some limitations. First, it was a single-center retrospective observational study. The reliability of the conclusions needs to be confirmed in a multicenter randomized-controlled trial. Second, the effect of unrecorded variables on the classification of postoperative pain trajectories could not be evaluated further because of the retrospective design of the study. Additionally, due to the lack of available data, the role of hormonal drugs during nerve block could not be assessed, as these drugs are rarely compounded during nerve block at our institution. Third, the sample size was small. Fourth, we examined only acute pain intensity and the effect of a single procedure at 24 h after the surgery.
Conclusions
Anteroposterior and left and right thoracic diameters are protective factors for pain, with each additional unit of anteroposterior and left and right thoracic diameters decreasing the probability of patient pain by approximately 23.5% and 38.8%, respectively. In addition, the proportion of female patients with RP was significantly higher than that of male patients with RP, indicating a strong association between sex and RP incidence. For patients who are likely to experience RP after intercostal nerve block release following three-port thoracoscopic surgery, advanced interventions must be considered to improve their prognosis and satisfaction.
Data Sharing Statement
Data supporting our findings are available from the corresponding author upon request. Data were not publicly available because of privacy or ethical restrictions.
Ethics Approval
This retrospective observational study was conducted at Jiaxing First Hospital, approved by the Institutional Ethics Committee (2023-LY-237), the full name of the Ethics Committee is the Medical Ethics Committee of Jiaxing First Hospital, and registered with the Chinese Clinical Trials Registry (registration number: ChiCTR2400083935, registration date: 2024-5-8). The study was carried out in accordance with the principles of the Declaration of Helsinki. Written informed consent has been obtained from all patients, and their anonymous information will be published in this article.
Acknowledgments
The authors would like to thank all the reviewers who participated in the Review.
Author Contributions
In this paper, Wan Chongyang was responsible for experimental scheme design, data collection and final writing. Kong Min and Shen Qihong are responsible for the design of the experimental scheme, and Lu Weina is responsible for helping to collect the data. Shen Xu is responsible for the final writing and revision. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the Department of Anesthesiology, Jiaxing First Hospital.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jia G. Research progress of rebound tenderness after peripheral nerve block. J Clin Anesthesiol. 2023;39(10):1093–1097.
2. Chang W-K, Li Y-S, Wu H-L, et al. Group-based trajectory analysis of postoperative pain in epidural analgesia for video-assisted thoracoscopic surgery and risk factors of rebound pain. J Chin Med Assoc. 2022;85(2):216–221. doi:10.1097/JCMA.0000000000000647
3. Barry GS, Bailey JG, Sardinha J, et al. Factors associated with rebound pain after peripheral nerve block for ambulatory surgery. Br J Anaesth. 2021;126(4):862–871. doi:10.1016/j.bja.2020.10.035
4. Zhu Y, Li Q, Liu G, et al. Effects of esketamine on postoperative rebound pain in patients undergoing unilateral total knee arthroplasty: a single-center, randomized, double-blind, placebo-controlled trial protocol. Front Neurol. 2023;14. doi:10.3389/fneur.2023.1179673
5. Luebbert E, Rosenblatt MA. Postoperative rebound pain: our current understanding about the role of regional anesthesia and multimodal approaches in prevention and treatment. Curr Pain Headache Report. 2023;27(9):449–454. doi:10.1007/s11916-023-01136-z
6. Dada O, Gonzalez Zacarias A, Ongaigui C, et al. Does rebound pain after peripheral nerve block for orthopedic surgery impact postoperative analgesia and opioid consumption? A narrative review. Int J Environ Res Public Health. 2019;16(18):3257. doi:10.3390/ijerph16183257
7. Admassie BM, Tegegne BA, Alemu WM, Getahun AB. Magnitude and severity of rebound pain after resolution of peripheral nerve block and associated factors among patients undergoes surgery at University of Gondar comprehensive specialized hospital northwest, Ethiopia, 2022. Longitudinal cross-sectional study. Ann Med Surg. 2022;84:104915.
8. Lavand’homme P. Rebound pain after regional anesthesia in the ambulatory patient. Curr Opin Anaesthesiol. 2018;31(6):679–684. doi:10.1097/ACO.0000000000000651
9. Hamilton DL. Rebound pain: distinct pain phenomenon or nonentity? Br J Anaesth. 2021;126(4):761–763. doi:10.1016/j.bja.2020.12.034
10. Kwon H-J, Kim YJ, Lee D, et al. Factors associated with rebound pain after patient-controlled epidural analgesia in patients undergoing major abdominal surgery. Clin J Pain. 2022;38(10):632–639. doi:10.1097/AJP.0000000000001067
11. Li Y-S, Chang KY, Lin SP, Chang MC, Chang WK. Group-based trajectory analysis of acute pain after spine surgery and risk factors for rebound pain. Front Med. 2022;9.
12. Chen-Yoshikawa TF, Fukui T, Nakamura S, et al. Current trends in thoracic surgery. Nagoya J Med Sci. 2020;82(2):161–174. doi:10.18999/nagjms.82.2.161
13. Van den Broek RJ, Koopman JS, Postema JM, et al. Continuous erector spinae plane block versus thoracic epidural analgesia in video-assisted thoracic surgery: a study protocol for a prospective randomized open label non-inferiority trial. Trials. 2021;22(1):321. doi:10.1186/s13063-021-05275-9
14. Williams BA, Bottegal MT, Kentor ML, et al. Rebound pain scores as a function of femoral nerve block duration after anterior cruciate ligament reconstruction: retrospective analysis of a prospective, randomized clinical trial. Reg Anesth Pain Med. 2007;32(3):186–192. doi:10.1016/j.rapm.2006.10.011
15. Terrie V, Wardhan R, Rashidi P, et al. Patient and procedural determinants of postoperative pain trajectories. Anesthesiology. 2021;134(3):421–434. doi:10.1097/ALN.0000000000003681
16. Thoracic DO, Sandner-Kiesling A, Strießnig A, et al. Is there an impact of sex on acute postthoracotomy pain? A retrospective analysis. Ann Thorac Surg. 2020;109(4):1104–1111. doi:10.1016/j.athoracsur.2019.11.016
17. Nobre LV, Cunha GP, Sousa PCCBD, et al. Bloqueio de nervos periféricos e dor rebote: revisão de literatura [Peripheral nerve block and rebound pain: literature review]. Braz J Anesthesiol. 2019;69(6):587–593. Portuguese. doi:10.1016/j.bjan.2019.05.001
18. Youm YS, Cho SD, Cho HY, et al. Preemptive femoral nerve block could reduce the rebound pain after periarticular injection in total knee arthroplasty. J Arthroplasty. 2016;31(8):1722–1726. doi:10.1016/j.arth.2016.02.006
19. Fang J, Shi Y, Du F, et al. The effect of perineural dexamethasone on rebound pain after ropivacaine single-injection nerve block: a randomized controlled trial. BMC Anesthesiol. 2021;21(1). doi:10.1186/s12871-021-01267-z
20. Sort R, Brorson S, Gögenur I, et al. Rebound pain following peripheral nerve block anaesthesia in acute ankle fracture surgery: an exploratory pilot study. Acta Anaesthesiologica Scandinavica. 2018;63(3):396–402. doi:10.1111/aas.13290
21. Zhang C, Li Z, Yu K, et al. A postoperative phenomenon of percutaneous endoscopic lumbar discectomy: rebound pain. Orthopaedic Surg. 2021;13(8):2196–2205. doi:10.1111/os.13088
22. Uppal V, Barry G, Ke JX, et al. Reducing rebound pain severity after arthroscopic shoulder surgery under general anesthesia and interscalene block: a two-centre randomized controlled trial of pre-emptive opioid treatment compared with placebo. Can J Anaesth. 2023;71(6):773–783.
23. Lee HJ. Intravenous versus perineural dexamethasone for reducing rebound pain after interscalene brachial plexus block: a randomized controlled trial. J Korean Med Sci. 2023;38(24).
24. Henningsen MJ, Sort R, Møller AM, Herling SF. Peripheral nerve block in ankle fracture surgery: a qualitative study of patients’ experiences. Anaesthesia. 2018;73(1):49–58. doi:10.1111/anae.14088
25. Muñoz-Leyva F, Cubillos J, Chin KJ. Managing rebound pain after regional anesthesia. Korean J Anesthesiol. 2020;73(5):372–383. doi:10.4097/kja.20436
26. Pradeep B, Rajasekhar M. Rebound pain: undesired, yet unexplored. J Anaesthesiol Clin Pharmacol. 2022;38(4):527–528. doi:10.4103/joacp.joacp_435_22
27. Schubert AK, Wiesmann T, Volberg C, et al. Rebound pain and postoperative pain profile following brachial plexus block compared to general anaesthesia—An observational study. Acta Anaesthesiologica Scandinavica. 2023;67(10):1414–1422. doi:10.1111/aas.14318
28. Streb T, Schneider A, Wiesmann T, et al. “Rebound pain” – von der Definition bis zur Therapie [‘Rebound pain” – from definition to therapy]. Die Anaesthesiologie. 2022;71(8):638–645. German. doi:10.1007/s00101-022-01120-z
29. Stone A, Lirk P, Vlassakov K. Rebound pain after peripheral nerve blockade—bad timing or rude awakening? Anesthesiology Clinics. 2022;40(3):445–454. doi:10.1016/j.anclin.2022.03.002
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Ultrasound-Guided Continuous Rhomboid Intercostal and Sub-Serratus Plane Block Comparison of Thoracoscopic Intercostal Nerve Block After Thoracoscopic Surgery: A Prospective Randomized Controlled Study
Wang S, Wang H, Chen X, Li M, Xu D
Journal of Pain Research 2024, 17:4471-4481
Published Date: 21 December 2024

