Back to Journals » Journal of Pain Research » Volume 18
Risk of Acute Pain in Obese Patients Undergoing Atrial Fibrillation Ablation
Authors Dong P, Wang H, Yan F, Zhang Z
Received 16 January 2025
Accepted for publication 29 April 2025
Published 20 May 2025 Volume 2025:18 Pages 2549—2557
DOI https://doi.org/10.2147/JPR.S517820
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Karina Gritsenko
Peiyu Dong, Hongbai Wang, Fuxia Yan, Zhe Zhang
Department of Anesthesiology, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China
Correspondence: Zhe Zhang, Department of Anesthesiology, Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, No. 167 Beilishi Road, Xicheng District, Beijing, 100037, People’s Republic of China, Email [email protected]
Background: Previous studies have indicated that obesity can lead to an increased pain sensitivity. However, the risk of acute pain in obese patients undergoing atrial fibrillation (AF) ablation remains unclear.
Methods: This was a case-control study. Clinical data of patients with AF who underwent percutaneous ablation at Fuwai Hospital between January and May 2019 were retrospectively collected. Numeric pain rating scale (NPRS) and Body mass index (BMI) were used to assess severity of intra-procedural pain and pre-procedural obesity, respectively. An intra-procedural NPRS score of 4 or higher indicated the presence of acute pain, and a pre-procedural BMI of 28 or greater was considered indicative of obesity. Multivariable logistic regression analysis was performed to explore the risk of intra-procedural acute pain in obese patients.
Results: A total of 333 eligible patients were divided into two groups based on presence of intra-procedural acute pain (case group: n=102 [30.6%] and control group: n=231 [69.4%]). Compared with control group, patients with intra-procedural acute pain showed higher percentage of obesity (40 [17.4%] vs 28 [27.5%]) and conscious sedation (96 [41.6%] vs 89 [87.3%]), lower percentage of diabetes history (38 [16.5%] vs 10 [9.8%]), and longer duration of procedure (median, 90 vs 110 min). The occurrence rates of acute pain during AF ablation were 41.2% for obese patients and 27.9% for non-obese patients. Obesity was independently associated with an increased risk of intra-procedural acute pain (adjusted odds ratio [OR], 2.29; 95% CI, 1.18– 4.43, P = 0.014). Sub-group analysis indicated a stronger risk of intra-procedural acute pain in obese patients under conscious sedation (adjusted OR, 2.48; 95% CI, 1.13– 5.42, P = 0.023).
Conclusion: Under conscious sedation, obesity is an independent risk factor for intra-procedural acute pain in adult patients undergoing AF ablation.
Keywords: obesity, acute pain, atrial fibrillation ablation, sedation, adult
Introduction
With the increase in global life expectancy, the prevalence of atrial fibrillation (AF) has tripled over the past 50 years.1 Currently, there are approximately 60 million cases of AF worldwide.2 The ablation therapy for AF has shown advantages over pharmacological treatments in psychological symptoms, quality of life, and cardiovascular morbidity.3–5 Therefore, the AF patients undergoing percutaneous interventional ablation therapy has increased annually.6,7 During AF ablation, a combination of local anesthesia and sedation is commonly used to alleviate intra-procedural pain. However, we have found that there are cases of inadequate pain control during the procedure in our hospital. If body movements occur due to acute pain during the procedure, it may adversely affect the ablation process and outcomes.8–10 Moreover, the experience of acute pain may have long-term negative effects on the patient’s mental and psychological condition.11–13
It is essential to explore and identify potential risk factors for acute pain during AF ablation. The occurrence of acute pain during the procedure could be minimized in the future by addressing risk factors or optimizing anesthesia techniques. In the clinical anesthesia practice of AF ablation, we have observed that obese patients appear to be more prone to experiencing acute pain in our hospital. However, through literature review, we found that clinical studies on acute pain during AF ablation in obese patients are lacking. Although some studies have found that obese individuals exhibit increased sensitivity to pain,14,15 there is still controversy among different studies regarding whether obesity actually leads to a lower pain threshold.16–18 Therefore, this study aims to explore the risk of acute pain in obese patients undergoing AF ablation.
Methods
Patient Screening
This study included adult patients who were hospitalized in arrhythmia center of Fuwai Hospital between January and May in 2019. The inclusion criteria were as follows: (1) primary diagnosis of AF, (2) underwent elective percutaneous interventional ablation for AF, and (3) intra-procedure pain assessment conducted by the anesthesia team. The exclusion criteria were as follows: (1) age < 18 years, (2) history of chronic pain treatment or currently medications for pain management, (3) cardiac electrophysiologists administered sedation independently, (4) concurrent treatments outside of AF ablation, (5) peri-procedure coma or cognitive dysfunction (e.g., delirium), and (6) incomplete data affecting statistical analysis.
Anesthesia Procedure
Cardiac electrophysiologists used lidocaine to perform local anesthesia at the puncture site, while the anesthesiologists performed sedation. The anesthesiologists selected either conscious sedation or deep sedation according to the requests of the electrophysiologists. Under conscious sedation, the patients did not require intervention to maintain airway patency and were able to purposefully respond to verbal commands, whether used alone or accompanied by light tactile stimulation. Under deep sedation, the patients’ spontaneous ventilation was possibly impaired, and they were aroused only by relatively strong painful stimulation. Conscious sedation primarily involved the use of midazolam (20μg/kg) and sufentanil (0.05μg/kg), whereas deep sedation involved the use of propofol (50μg/kg/min), dexmedetomidine (0.5μg/kg/h) and sufentanil (0.05μg/kg). Oxygen was administered via a mask or nasal cannula, and all patients received monitoring of pulse oxygen saturation, blood pressure, and electrocardiogram. Bispectral index (BIS) was monitored for patients under deep sedation.
Assessment of Obesity and Acute Pain
Pre-procedural obesity was assessed using body mass index (BMI), which was calculated as weight (kg) divided by height (m) squared. A BMI ≥ 28 on the day of procedure indicated obesity.19
After the patient was fully awake, intra-procedural pain severity was assessed using the numeric pain rating scale (NPRS), which ranged from 0 (no pain) to 10 (worst pain). An acute pain is identified if the highest intra-procedural NPRS score is ≥ 4.20 The main areas of acute pain were the chest and the puncture site.
Grouping and Sample Size Calculation
This was an unmatched case-control study. The eligible patients were divided into two groups based on whether intra-procedural acute pain occurred: cases were patients with acute pain, controls were patients without acute pain.
Based on a preliminary retrospective study that included data of patients who underwent AF ablation at Fuwai Hospital in May 2019, sample size calculation was performed using the PASS 15.0 software (NCSS Corp., Kaysville, UT, USA). The proportion of patients with obesity in the patients without acute pain was 15.0%; moreover, the expected Odds Ratio (OR) for the risk of acute pain in patients with obesity was 2.667. The minimum sample size in the case and control group were 67 and 214, respectively, with a power of 80% and a two-sided α of 0.05, calculated by PASS.
Statistical Analysis
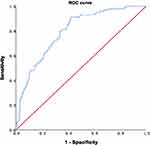
Data were analyzed using the IBM SPSS 26 software (IBM Corp., Armonk, NY, USA). Continuous data were expressed as median (lower quartile - upper quartile) [M(QL-QU)], with group comparisons conducted using the Mann–Whitney U-test. Categorical data are expressed as counts (percentage) [n (%)], with group comparisons using Pearson’s chi-square test. Multivariable logistic regression analysis was used to explore the risk of acute pain in patients with obesity. In multivariable regression model, pre-procedural obesity was defined as an independent variable, while intra-procedural acute pain was defined as the dependent variable. The model was adjusted with the following variables: sex, age (as a continuous variable), history of diabetes, depth of sedation, and duration of procedure (as a continuous variable). Patients without obesity were the reference category in the model. An area under curve (AUC) was generated from the receiver operating characteristic (ROC) curve to indicate the discrimination of the multivariable regression model. Hosmer-Lemeshow goodness of fit test was used to evaluate the calibration of the model. Statistical significance was set at P < 0.05.
Results
Patient Inclusion and Grouping
A total of 336 patients with AF hospitalized between January and May, 2019, were screened, and 3 were excluded based on the criteria. The remaining 333 eligible patients were included, of whom 68 (20.4%) had pre-procedural obesity and 265 (79.6%) did not. According to presence of intra-procedural acute pain, 102 patients (30.6%) were divided into case group, whereas 231 patients (69.4%) without acute pain were divided into control group (Figure 1).
 |
Figure 1 Flow chart of patients screening and grouping. Abbreviation: AF, atrial fibrillation. |
Clinical Characteristics
Table 1 presents the univariate analyses of the baseline characteristics and peri-procedural clinical data of the eligible patients. Compared with patients in control group, patients in case group showed higher percentage of obesity (40 [17.4%] vs 28 [27.5%]) and conscious sedation (96 [41.6%] vs 89 [87.3%]), lower percentage of diabetes (38 [16.5%] vs 10 [9.8%]), and longer duration of procedural (median, 90 vs 110 min). Univariate analysis indicated a statistically significant difference in the proportion of pre-procedural obesity between the two groups (χ² = 4.472, P = 0.034). The occurrence rates of acute pain during AF ablation were 41.2% for obese patients and 27.9% for non-obese patients.
 |
Table 1 Comparisons Between Patients with and Without Acute Pain |
Multivariable Logistic Regression Analysis
After adjusting for age, sex, diabetes history, depth of sedation, and duration of procedure, obesity was independently associated with an increased risk of intra-procedural acute pain (adjusted odds ratio [OR], 2.29; 95% CI, 1.18–4.43, P = 0.014) (Table 2).
 |
Table 2 Risk of Intra-Procedural Acute Pain in Obese Patients |
ROC curve analysis showed that the multivariable logistic regression model had a reasonable predictive ability for intra-procedural acute pain in AF patients who underwent percutaneous ablation (AUC: 0.796; 95% CI: 0.747 to 0.845; P < 0.001) (Figure 2). The accuracy of the estimated probabilities in the patients was ensured by the Hosmer-Lemeshow goodness of fit test of the multivariable logistic regression model (χ2: 7.035; P = 0.533).
Sub-Group Analysis
A total of 333 eligible patients were divided into two sub-groups according to different depth of sedation (conscious sedation or deep sedation). Univariate analysis showed that for the sub-group of conscious sedation, there was a statistical difference in the percentage of pre-procedural obesity between the case and the control group (χ² = 6.167, P = 0.013). After adjusting for age, sex, diabetes history, and duration of procedure, multivariable logistic regression analysis indicated that the risk of intra-procedural acute pain was further increased in patients with obesity (adjusted OR, 2.48; 95% CI, 1.13–5.42; P = 0.023) (Table 3). No statistical difference was observed in the sub-group of deep sedation (adjusted OR, 1.99; 95% CI, 0.50–7.84; P = 0.327).
 |
Table 3 Risk of Intra-Procedural Acute Pain Sub-Grouped by Depth of Sedation a |
Discussion
Our study indicates that obesity is associated with an increased risk of intra-procedural acute pain in patients undergoing percutaneous AF ablation, which is consistent with previous studies of non-cardiac populations.14,21–25 This association appears to be mainly attributable to a stronger increased risk of intra-procedural acute pain in obese patients under conscious sedation. Among these patients, obesity was associated with a 2.5-fold increased risk of intra-procedural acute pain compared with patients of normal BMI. In addition, the occurrence rate of intra-procedural acute pain of obese patients during AF ablation in our study was as high as 41.2%.
The possible mechanisms for increased pain sensitivity in populations with obesity include and inflammatory responses and poor sleep quality. Inflammation is one of the most common physiological mechanisms associated with obesity-related pain, and obesity is considered a state of chronic low-grade inflammation.26 Adipose tissue has endocrine functions and secretes anti-inflammatory cytokines under normal metabolic conditions.27 However, when excess fat is present, pro-inflammatory immune cells infiltrate adipose tissue, leading to the secretion of pro-inflammatory cytokines, which can affect neuronal activity in both peripheral and central nervous systems, increasing sensitivity to mechanical or thermal stimuli.28,29 Animal studies have shown that sleep deprivation significantly lowers pain thresholds, with increased adenosine activity enhancing pain sensitivity in sleep-deprived rats.30,31 Poor sleep quality are common in populations with obesity,32 and a correlation was found between poor sleep quality and increased peri-operative pain sensitivity.33–36
Obesity has become an increasing problem worldwide during the past few decades. According to a report, the overweight and obesity rates among adults in China are 34.3% and 16.4%, respectively.37 In our study, the proportion of obese patients with AF was 20.4%. And obesity was defined as BMI ≥28, based on the physical characteristics of Asian populations and the guidelines in China.19 BMI is affected by a variety of cultural, social, psychological, behavioural, pathophysiological and environmental influences. Although a lot of studies have shown that obesity has a negative effect on pain-related outcomes in different populations. There is, however, insufficient clinical evidence to suggest a clear positive effect of weight loss on acute pain. Therefore, whether the weight loss before AF ablation could be an effective method for attenuating intra-procedural pain still needs further research.
Although the advancements in ablation technology, acute pain that may occur during the procedure remains an issue that has not been effectively addressed and has long been overlooked. If patients experience acute pain during the procedure, psychological issues may arise, which is a common reason why patients refuse repeat ablation when atrial fibrillation recurs. After determining pre-procedural obesity as an independent risk factor of intra-procedural acute pain, we evaluated the clinical application value of the multivariable regression model. ROC curve analysis showed that the AUC is close to 0.8, indicating that the model has a reasonable predictive ability for patients in prediction of intra-procedural acute pain.38 Thus, we recommend assessing and predicting the risk of acute pain in patients undergoing AF ablation, as it holds the clinical significance. Firstly, it helps clinicians optimize intra-procedural sedation or anesthesia strategies in advance based on the risk of acute pain, thereby reducing the incidence of acute pain during AF ablation. Secondly, it may decrease complications during and after the procedure caused by acute pain and potentially improve patient outcomes. Thirdly, predicting the risk of acute pain can provide direction for researches into the mechanisms of intra-procedural acute pain and the development of pain management strategies.
According to this study, deep sedation can significantly reduce the incidence of intra-procedural acute pain in patients undergoing AF ablation. However, for obese patients, the choice of deep sedation requires balancing the benefits and risks, as it is necessary to assess the anesthesia risks. Obstructive sleep apnea (OSA) is very common among obese patients,39–41 and many cases of OSA remain unscreened and undiagnosed before ablation.42 Thus, obese patients receiving deep sedation are more likely to experience unexpected acute airway obstruction. There is currently no clear evidence on whether obese patients undergoing AF ablation should be placed under deep or conscious sedation. Anesthesiologists should make decisions based on clinical skills of cardiac electrophysiologists, clinical characteristics and preferences of patients, and pre-anesthetic evaluations. Pre-procedural OSA screening and a contingency plan to manage airway obstruction are crucial for obese patients scheduled for deep sedation.43,44
This study shows a wide age range among patients undergoing AF ablation (minimum age 25 years, maximum age 81 years), with a significant percentage of older patients (54.7%, aged 60 years and above) and a high prevalence of comorbidities (coronary heart disease and hypertension). For older patients, conscious sedation is recommended as the first choice, whereas deep sedation should be carefully controlled in terms of induction speed and drug dosage to minimize the risk of hypotension and delayed recovery. In the present study, the proportion of AF patients with hypertension was as high as 52%. For patients with moderate to severe hypertension or coronary artery disease, deep sedation may be preferred to prevent severe intra-procedural blood pressure fluctuations or angina triggered by acute pain. BIS monitoring is recommended during deep sedation to reduce the dosage of anesthetic agents and the recovery duration.45
The limitations of this study mainly stem from its retrospective design, which makes it impossible to eliminate all potential confounding factors that may influence the results. Additionally, data on patients’ sleep quality prior to the procedure was not available, leaving it as a possible source of confounding. Finally, the influence of intrinsic shortcomings of self-reported data on the results cannot be ruled out.
Conclusion
Our findings indicate that patients with a BMI of 28 or higher face a significantly elevated risk of acute pain under conscious sedation during the procedure. This heightened risk should be carefully considered when performing pre-anesthetic evaluations and determining the appropriate anesthesia. Further prospective studies are needed to establish a causal relationship between pre-procedural obesity and intra-procedural acute pain.
Abbreviation
AUC, Area under curve; AF, Atrial fibrillation; BIS, Bispectral Index; BMI, Body mass index; CI, Confidence interval; NPRS, Numerical pain rating scale; OSA, Obstructive sleep apnea; OR, Odds ratio; ROC, Receiver operating characteristic.
Ethics
This study was approved by the Ethics Committee of Fuwai Hospital and conducted in accordance with the Declaration of Helsinki. The Ethics Committee waived the need for patient consent owing to retrospective data collection. The patient records and information were anonymized and de-identified before analysis.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed on the journal to which the article will be submitted; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
Supported by CAMS Innovation Fund for Medical Sciences (CIFMS 2023-I2M-1-004).
Disclosure
All authors declared that the study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015;386(9989):154–162. doi:10.1016/S0140-6736(14)61774-8
2. Elliott AD, Middeldorp ME, Van Gelder IC, et al. Epidemiology and modifiable risk factors for atrial fibrillation. Nat Rev Cardiol. 2023;20(6):404–417. doi:10.1038/s41569-022-00820-8
3. Al-Kaisey AM, Parameswaran R, Bryant C, et al. Atrial fibrillation catheter ablation vs medical therapy and psychological distress: a randomized clinical trial. JAMA. 2023;330(10):925–933. doi:10.1001/jama.2023.14685
4. Mark DB, Anstrom KJ, Sheng S, et al. Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA. 2019;321(13):1275–1285. doi:10.1001/jama.2019.0692
5. Mahalleh M, Soleimani H, Pazoki M, et al. Heart failure with preserved ejection fraction and atrial fibrillation: catheter ablation vs. standard medical therapy - a systematic review and meta-analysis. Heart Fail Rev. 2025;30(1):1–15. doi:10.1007/s10741-024-10437-3
6. Kushnir A, Barbhaiya CR, Aizer A, et al. Temporal trends in atrial fibrillation ablation procedures at an academic medical center: 2011-2021. J Cardiovasc Electrophysiol. 2023;34(4):800–807. doi:10.1111/jce.15839
7. National Center for Cardiovascular Diseases. Summary of the China cardiovascular health and disease report 2023. Chin J Cir. 2024;39(7):625–660. doi:10.3969/j.issn.1000-3614.2024.07.001
8. Li KHC, Sang T, Chan C, et al. Anaesthesia use in catheter ablation for atrial fibrillation: a systematic review and meta-analysis of observational studies. Heart Asia. 2019;11(2):e011155. doi:10.1136/heartasia-2018-011155
9. Riis-Vestergaard LD, Tønnesen J, Ruwald MH, et al. General anaesthesia compared to conscious sedation for first-time atrial fibrillation catheter ablation-a Danish nationwide cohort study. Europace. 2024;26(8):euae203. doi:10.1093/europace/euae203
10. Ford P, Cheung AR, Khan MS, et al. Anesthetic techniques for ablation in atrial fibrillation: a comparative review. J Cardiothorac Vasc Anesth. 2024;38(11):2754–2760. doi:10.1053/j.jvca.2024.05.004
11. Fregoso G, Wang A, Tseng K, Wang J. Transition from acute to chronic pain: evaluating risk for chronic postsurgical pain. Pain Physician. 2019;22(5):479–488. doi:10.36076/ppj/2019.22.479
12. Ishida Y, Okada T, Kobayashi T, et al. Pain management of acute and chronic postoperative pain. Cureus. 2022;14(4):e23999. doi:10.7759/cureus.23999
13. Small C, Laycock H. Acute postoperative pain management. Br J Surg. 2020;107(2):e70–e80. doi:10.1002/bjs.11477
14. Pradalier A, Willer JC, Boureau F, et al. Relationship between pain and obesity: an electrophysiological study. Physiol Behav. 1981;27(6):961–964. doi:10.1016/0031-9384(81)90354-1
15. Marques Miranda C, de Lima Campos M, Leite-Almeida H. Diet, body weight and pain susceptibility - A systematic review of preclinical studies. Neurobiol Pain. 2021;10:100066. doi:10.1016/j.ynpai.2021.100066
16. Emerson NM, Nahman-Averbuch H, Peugh JL, et al. Pain sensitivity does not differ between obese and healthy weight individuals. Pain Rep. 2021;6(3):e942. doi:10.1097/PR9.0000000000000942
17. Torensma B, Thomassen I, van Velzen M, et al. Pain experience and perception in the obese subject systematic review (Revised Version). Obes Surg. 2016;26(3):631–639. doi:10.1007/s11695-015-2008-9
18. Okifuji A, Hare BD. The association between chronic pain and obesity. J Pain Res. 2015;8:399–408. doi:10.2147/JPR.S55598
19. National Health Commission of the People’s Republic of China. Guidelines for the diagnosis and treatment of obesity (2024 edition). Chin J Digest Surg. 2024;23(10):1237–1260. doi:10.3760/cma.j.cn115610-20241017-00455
20. Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10:390–392. doi:10.1197/aemj.10.4.390
21. McKendall MJ, Haier RJ. Pain sensitivity and obesity. Psychiatry Res. 1983;8:119–125. doi:10.1016/0165-1781(83)90099-9
22. Neumann L, Lerner E, Glazer Y, et al. A cross-sectional study of the relationship between body mass index and clinical characteristics, tenderness measures, quality of life, and physical functioning in fibromyalgia patients. Clin Rheumatol. 2008;27(12):1543–1547. doi:10.1007/s10067-008-0966-1
23. Zhang Y, Zhang S, Gao Y, et al. Factors associated with the pressure pain threshold in healthy Chinese men. Pain Med. 2013;14(9):1291–1300. doi:10.1111/pme.12158
24. Miscio G, Guastamacchia G, Brunani A, et al. Obesity and peripheral neuropathy risk: a dangerous liaison. J Peripher Nerv Syst. 2005;10(4):354–358. doi:10.1111/j.1085-9489.2005.00047.x
25. Okifuji A, Donaldson GW, Barck L, et al. Relationship between fibromyalgia and obesity in pain, function, mood, and sleep. J Pain. 2010;11(12):1329–1337. doi:10.1016/j.jpain.2010.03.006
26. Chin SH, Huang WL, Akter S, et al. Obesity and pain: a systematic review. Int J Obes. 2020;44(5):969–979. doi:10.1038/s41366-019-0505-y
27. Crissey JM, Jenkins NT, Lansford KA, et al. Adipose tissue and vascular phenotypic modulation by voluntary physical activity and dietary restriction in obese insulin-resistant OLETF rats. Am J Physiol Regul Integr Comp Physiol. 2014;306:R596–606. doi:10.1152/ajpregu.00493.2013
28. Han JM, Levings MK. Immune regulation in obesity-associated adipose inflammation. J Immunol. 2013;191:527–532. doi:10.4049/jimmunol.1301035
29. Ronti T, Lupattelli G, Mannarino E. The endocrine function of adipose tissue: an update. Clin Endocrinol. 2006;64:355–365. doi:10.1111/j.1365-2265.2006.02474.x
30. Xue J, Li H, Xu Z, et al. Paradoxical sleep deprivation aggravates and prolongs incision-induced pain hypersensitivity via BDNF signaling-mediated descending facilitation in rats. Neurochem Res. 2018;43:2353–2361. doi:10.1007/s11064-018-2660-2
31. Hambrecht-Wiedbusch VS, Gabel M, Liu LJ, et al. Preemptive caffeine administration blocks the increase in postoperative pain caused by previous sleep loss in the rat: a potential role for preoptic adenosine a2a receptors in sleep-pain interactions. Sleep. 2017;40(9):zsx116. doi:10.1093/sleep/zsx116
32. Badran M, Ayas N, Laher I. Insights into obstructive sleep apnea research. Sleep Med. 2014;15:485–495. doi:10.1016/j.sleep.2014.01.009
33. Wang JP, Lu SF, Guo LN, et al. Poor preoperative sleep quality is a risk factor for severe postoperative pain after breast cancer surgery: a prospective cohort study. Medicine. 2019;98:e17708. doi:10.1097/MD.0000000000017708
34. Orbach-Zinger S, Fireman S, Ben-Haroush A, et al. Preoperative sleep quality predicts postoperative pain after planned caesarean delivery. Eur J Pain. 2017;21:787–794. doi:10.1002/ejp.980
35. Luo ZY, Li LL, Wang D, et al. Preoperative sleep quality affects postoperative pain and function after total joint arthroplasty: a prospective cohort study. J Orthop Surg Res. 2019;14:378. doi:10.1186/s13018-019-1446-9
36. Zhang Z, Wang H, Wang Y, et al. Risk of postoperative hyperalgesia in adult patients with preoperative poor sleep quality undergoing open-heart valve surgery. J Pain Res. 2020;13:2553–2560. doi:10.2147/JPR.S272667
37. National Health Commission of the People’s Republic of China. Report on nutrition and chronic diseases of Chinese residents (2020). Acta Nutrimenta Sinica. 2020;42(6):521.
38. Hanley JA, McNeil BJ. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29–36. doi:10.1148/radiology.143.1.7063747
39. De Jong A, Verzilli D, Chanques G, et al. Preoperative risk and perioperative management of obese patients. Rev Mal Respir. 2019;36(8):985–1001. doi:10.1016/j.rmr.2019.01.009
40. Carron M, Safaee Fakhr B, Ieppariello G, et al. Perioperative care of the obese patient. Br J Surg. 2020;107(2):e39–e55. doi:10.1002/bjs.11447
41. Cha YM, Friedman PA, Asirvatham SJ, et al. Catheter ablation for atrial fibrillation in patients with obesity. Circulation. 2008;117(20):2583–2590. doi:10.1161/CIRCULATIONAHA.107.716712
42. Madhusudan P, Wong J, Prasad A, et al. An update on preoperative assessment and preparation of surgical patients with obstructive sleep apnea. Curr Opin Anaesthesiol. 2018;31(1):89–95. doi:10.1097/ACO.0000000000000539
43. Chung F, Memtsoudis SG, Ramachandran SK, et al. Society of anesthesia and sleep medicine guidelines on preoperative screening and assessment of adult patients with obstructive sleep apnea. Anesth Analg. 2016;123(2):452–473. doi:10.1213/ANE.0000000000001416
44. Willard CE, Rice AN, Broome ME, et al. Nasal ventilation mask for prevention of upper airway obstruction in patients with obesity or obstructive sleep apnea. AANA J. 2019;87(5):395–403.
45. Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014;6:CD003843. doi:10.1002/14651858.CD003843.pub3
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.