Back to Journals » International Journal of Women's Health » Volume 17
Risk of Mental Disorders in Polycystic Ovary Syndrome: Retrospective Cohort Study of a Korean Nationwide Population-Based Cohort
Authors Kim Y , Chae K, Kim S, Kang S, Yoon H, Namkung J
Received 19 August 2024
Accepted for publication 24 January 2025
Published 5 March 2025 Volume 2025:17 Pages 627—638
DOI https://doi.org/10.2147/IJWH.S490673
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Youngjin Kim,1 Kyunghee Chae,1 Sukil Kim,1 Soyeon Kang,2 Hyonjee Yoon,2 Jeong Namkung2
1Department of Preventive Medicine and Public Health, College of Medicine, The Catholic University of Korea, Seoul, Korea; 2Department of Obstetrics and Gynecology, College of Medicine, The Catholic University of Korea, Seoul, Korea
Correspondence: Jeong Namkung, Department of Obstetrics and Gynecology, College of Medicine, The Catholic University of Korea, 17, Banpo-Daero 20-Gil, Seocho-Gu, Seoul, Korea, Email [email protected]
Purpose: Polycystic Ovary Syndrome (PCOS) is one of the most common gynecological endocrine conditions, affecting both the physical and mental health, and the quality of life of women. PCOS was associated with diverse mental disorders but studies in Korean populations were limited. This study aims to investigate the risk of mental disorders in PCOS patients in Korea.
Patients and Methods: We evaluated the risk of five mental disorders in PCOS patients using health insurance billing data from the National Health Insurance Corporation. We selected 188,973 PCOS patients and 412,022 control individuals. Prevalence, cumulative incidence, and Hazard ratios (HR) were calculated for each mental disorder.
Results: We found PCOS patients to have increased prevalence of depressive disorders (Odds ratios (OR) 1.208[1.185– 1.232]), bipolar disorders (OR 1.403[1.330– 1.479]), and anxiety disorders (OR 1.089[1.064– 1.114]); however, PCOS patients also had lower prevalence of schizophrenia (OR 0.686[0.638– 0.737]) and sleep disorder (OR 0.911[0.888– 0.935]). The PCOS patients exhibited a significantly greater HR in depressive disorder (adjusted HR 1.244[1.148– 1.347]), bipolar disorder (adjusted HR 1.502[1.139– 1.981]), anxiety disorder (adjusted HR 1.147[1.050– 1.252]), and sleep disorder (adjusted HR 1.228[1.112– 1.356]).
Conclusion: Our results suggest that PCOS patients have increased risk of depressive disorders, bipolar disorders, anxiety disorders, and sleep disorders. This study supports international PCOS guidelines that recommend screening for mental health disorders.
Keywords: depressive disorder, bipolar disorder, anxiety disorders, schizophrenia, sleep wake disorders
Introduction
Polycystic ovary syndrome (PCOS) is one of the most common hormonal disturbances, affecting an estimated 8–13% of women of reproductive age.1 PCOS is a multifaceted disease influenced by genetic, endocrine, environmental, and behavioral factors, resulting in a heterogeneous phenotype with reproductive, metabolic, and psychological effects on women’s health and quality of life throughout life.2 The Rotterdam Criteria, the most widely used diagnostic criteria for PCOS, requires at least two of three conditions be met to confirm the diagnosis: clinical or biochemical hyperandrogenism, evidence of oligo-anovulation, and/or polycystic appearing-ovarian morphology on ultrasound, with the exclusion of other relevant disorders.3
Mental disorders are a significant public health burden and are associated with, but not limited to, socioeconomic status, race/ethnicity, life events, genes, and stress.4 Mental and physical health conditions are common comorbidities5 and, affect each other both directly and indirectly.6 PCOS is related to mental disorders in several ways.7 Previous studies have demonstrated associations between PCOS and various mental disorders.8–13 Another study suggested that distinguishing PCOS and mental disorder could be challenging, given the significant overlap between the symptoms of PCOS and side effects of antipsychotic drugs (for example, menstrual irregularity, amenorrhea, weight gain).14 The 2023 International Evidence–Based Guideline for the Assessment and Management of Polycystic Ovary Syndrome recommends that all healthcare professionals be aware of common psychological features that are important components of PCOS.15
Previous studies have shown the prevalence of PCOS,16 of type 2 diabetes mellitus with PCOS,17 and of impairment of glucose tolerance in PCOS patients17 differs among ethnicities. These findings suggest that the associations between PCOS and mental disorders might differ among ethnicities; however, there have been few studies assessing the risk of mental disorders in PCOS patients in the Korean population. A previous study investigating the prevalence of PCOS in Korean women of reproductive age indicated the need to examine the psychological problems associated with PCOS.18 We could find only one retrospective cohort study of Korean PCOS patients, which only covered major depressive disorder.19
We aimed to evaluate the risk of schizophrenia, depressive disorder, bipolar disorder, anxiety disorder, and sleep disorder in PCOS patients using billing data from Korea. We intended to clarify the relationship between PCOS and mental disorders within the Korean population and to contribute to PCOS–related research worldwide.
Materials and Methods
Study Design
This was a retrospective cohort study that utilized a nationwide population-based database. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of the Catholic Medical Center (IRB number: PC22ZISI0075). Patient consent was waived because individual patients cannot be identified within the database.
Data Source
We used the Korean health insurance claims data provided by the National Health Insurance Corporation (NHIC) from 2002 to 2020 (Database number: NHIS-2023-1-012). International Classification of Diseases, 10th revision (ICD-10) was used to identify PCOS, mental disorders, and comorbidities from the data.
Study Population
The process of selecting the study population is depicted in Figure 1. Among 1,641,735 individuals, we identified individuals with a history of PCOS using ICD-10 code E.28.2 (n=328,347). We excluded individuals who were younger than 11 or older than 60 years of age at the initial PCOS diagnosis (N=365), initially diagnosed with PCOS before 2004 or after 2017 (N=109,069), or who had been diagnosed with Cushing’s syndrome (E24), hyperprolactinemia (E22.1), or adrenogenital disorders (E25.0) (N = 13,214).
 |
Figure 1 Flowchart of Included Participant. Abbreviations: NHIS, National Health Insurance Services; PCOS, polycystic ovary syndrome. |
Our exclusion criteria were to clarify the impact of PCOS on mental health and ensure data quality. Since such exclusions would inevitably result in data loss, we established criteria to ensure that minimal data could be excluded. We assumed that if the initial diagnosis age of PCOS was not between 11 and 60 years, it was likely to be a misdiagnosis or an outlier. Since the registered data were limited from 2002 to 2020, analysis of data beyond this range was not feasible. Hence, individuals initially diagnosed with PCOS from 2004 to 2017 were chosen for this study to ensure a minimum of two years of pre- and post-diagnosis medical history. For those initially diagnosed with PCOS in 2002 or 2003, verifying the accuracy of their initial diagnosis is challenging due to the inability to access past medical records. As the data only extended to 2020, our understanding of the post-diagnosis medical history was limited for those initially diagnosed after 2017. We excluded patients with hormonal diseases having symptoms similar to PCOS to study the impact of PCOS on mental health clearly.
The control group was randomly selected from individuals without PCOS and was matched 1:3 with PCOS patients using propensity matching according to age and index year. The index date for PCOS patients was their initial PCOS diagnosis, while that for the control group was the first medical record of the assigned index year. In conclusion, 188,973 PCOS patients and 412,022 control individuals were selected.
Baseline Characteristics
The follow-up duration for this study was the period between the index date and the day we stopped tracking, which is the date of death for individuals who died before 2021, or December 31, 2020 for individuals who did not die before 2021.
Baseline comorbidities evaluated in this study were dyslipidemia (ICD-10 code: E78), hypertension (I10–I15), and diabetes mellitus (E10–E14). To be counted as having comorbidity, at least one hospitalization or two outpatient visits due to such disease was required.
We used medical check-up records for the index year in the analyses. Individuals who were current or previous smokers on the date of medical check-up were classified as having a smoking history. Non-smokers were those who had never smoked at the time of medical check-up. Individuals who consumed alcohol three or more times per week were classified as consuming alcohol frequently. Individuals were categorized based on their body mass index (BMI): underweight (BMI < 18.5kg/m2), healthy weight (20kg/m2 <= BMI < 25kg/m2), healthy weight (25kg/m2 <= BMI < 30kg/m2), or obese (BMI >= 25kg/m2).
Definition of Mental Disorder
Schizophrenia (ICD-10 codes: F20), depressive disorder (F32, F33, F34.1), bipolar disorder (F30, F31), anxiety disorder (F40, F41, F42, F43.0, F43.1), and sleep disorders (F51, G47) were noted in the subjects of this study. For an individual to be identified as having a mental disorder, their medical records had to include at least one hospitalization or two outpatient visits due to such disorders. Mental disorders diagnosed one year or more after the individual’s index date were considered for incidence calculation.
Statistical Analysis
The characteristics of PCOS patients and controls were described using appropriate summary statistics. For continuous variables, the mean, standard deviation (SD), median, and quartiles were used. For categorical variables, frequencies and percentages were used.
Differences between PCOS patients and controls were assessed using appropriate statistics. For continuous variables, Student’s t-test was used. For categorical variables, Chi-square tests were performed, and odds ratios (OR) with 95% confidence intervals (CIs) were calculated. The cumulative incidence of each mental disorder was calculated using the Kaplan-Meier method and compared between the case and control groups. For each mental disorder, unadjusted hazard ratio (HR) and HR adjusted for factors including age, diabetes, hypertension, dyslipidemia, BMI, smoking history, and alcohol intake frequency were calculated using univariate and multivariate Cox proportional hazards regression. Additionally, we calculated and compared HRs between subgroups of the study population: obese and non-obese individuals; individuals aged less than 35 and aged 35 or older. For sensitivity analysis, we calculated HRs in absence of individuals having smoking history or taking alcohol frequently. All data analyses were performed using SAS software (version 9.4, SAS Institute Inc., Cary, NC). A p-value < 0.05 was considered statistically significant.
Results
Baseline Characteristics
Comparisons of the baseline characteristics of the PCOS patients and controls are presented in Table 1. The mean age was 26.36 (SD 6.11) years for PCOS patients and 35.02 (SD 6.89) years for the controls, while the median age was 26 (interquartile range 22 to 30) years for PCOS patients and 35 (interquartile range 30 to 39) years for the controls. Among the PCOS patients, those aged 20–29 years comprised the largest age group (n = 114,601, 60.64%), while that of the controls was 30–39 years (n = 226,071, 54.87%). The mean follow-up duration was 8.57 years (SD 3.91) for PCOS patients and 8.69 years (SD 3.81) for the controls.
 |
Table 1 Baseline Characteristics of PCOS Patients and Controls |
In both PCOS patients and controls, the most common comorbid conditions were dyslipidemia (n = 68,923 and n = 152,276, respectively), followed by diabetes mellitus (n = 29,318 and n = 58,314) and hypertension (n = 14,709 and n = 45,970).
The number of individuals with medical check-up records in the index year was 33,652 (17.81%) for PCOS patients and 98,167 (23.83%) for the controls. The number of individuals with a smoking history was 3,365 (10.07%) for PCOS patients and 7,300 (7.49%) for the controls. The number of individuals who consumed alcohol more than three times a week was 2,184 (6.52%) for PCOS patients and 5,775 (5.91%) for the control group. The mean BMI was 22.13 kg/m2 (SD 4.08) for PCOS patients and 22.15 kg/m2 (SD 3.48) for controls. In both PCOS patients and controls, most individuals were of healthy weight (n = 22,908 and n = 71,585, respectively). The differences between all laboratory test results of PCOS patients and controls were significant. The numbers and proportion of individuals in subgroups are shown in Supplementary Tables 1 and 2, and those of individuals with or without a history of smoking or frequent alcohol consumption are presented in Supplementary Table 3.
Prevalence of Mental Disorders in PCOS
The prevalence of mental disorders in the PCOS patients and controls is presented in Table 2 and Figure 2. The PCOS patients had significantly greater prevalence of depressive disorder (OR: 1.208, 95% CI = 1.185–1.232), bipolar disorder (OR: 1.403, 95% CI = 1.330–1.479), and anxiety disorder (OR: 1.089, 95% CI = 1.064–1.114) than controls; however, PCOS patients had a significantly lower prevalence of schizophrenia (OR: 0.686, 95% CI = 0.638–0.737) and sleep disorders (OR: 0.911, 95% CI = 0.888–0.935).
 |
Table 2 Prevalence of Mental Disorders Among PCOS Patients and Controls |
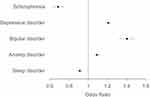 |
Figure 2 Hazard Ratios for Incidence of Mental Disorders in PCOS Patients. |
Cumulative Incidence of Mental Disorders in PCOS
The incidence of depressive disorders, bipolar disorders, anxiety disorders, and sleep disorders in PCOS patients was significantly greater than in controls (Figure 3, Log–rank test P–value < 0.05), while the incidence of schizophrenia did not differ significantly between PCOS patients and controls (Log–rank test P–value: 0.69).
 |
Figure 3 Cumulative Incidence of Mental Disorders in PCOS Patients and Controls: (A) Schizophrenia, (B) Depressive disorder, (C) Bipolar disorder, (D) Anxiety disorder, (E) Sleep disorder. |
Hazard Ratios for the Incidence of Mental Disorders in PCOS
The results of Cox proportional–hazards regression analyses are presented in Table 3 and Figure 4. The PCOS patients exhibited significantly greater HRs for depressive disorder (unadjusted HR: 1.443, 95% CI: 1.405–1.483; adjusted HR: 1.244, 95% CI: 1.148–1.347), bipolar disorder (unadjusted HR: 1.779, 95% CI: 1.651–1.916; adjusted HR: 1.502, 95% CI: 1.139–1.981), anxiety disorder (unadjusted HR: 1.228, 95% CI: 1.191–1.266; adjusted HR: 1.147, 95% CI: 1.050–1.252), and sleep disorder (unadjusted HR: 1.062, 95% CI: 1.026–1.099; adjusted HR: 1.228, 95% CI: 1.112–1.356). However, for schizophrenia, HRs were not significant (unadjusted HR: 0.974, 95% CI: 0.858–1.107; adjusted HR: 0.717, 95% CI: 0.427–1.204).
 |
Table 3 Hazard Ratios for Incidence of Mental Disorders in PCOS Patients |
In the subgroup analysis based on obesity, presented in Supplementary Table 4, non-obese PCOS patients exhibited higher HRs for the four mental disorders, excluding schizophrenia, which were similar to the HRs in the total study population. In contrast, all adjusted HRs for obese PCOS patients were insignificant. In the subgroup analysis based on age, presented in Supplementary Table 5, PCOS patients aged less than 35 showed higher HRs for the four mental disorders, excluding schizophrenia. However, PCOS patients aged 35 or older exhibited higher HRs only for depressive disorder and sleep disorder. Sensitivity analysis, presented in Supplementary Table 6, yielded results consistent with the main findings, showing that PCOS patients had significantly higher adjusted HRs for depressive disorder, bipolar disorder, anxiety disorder, and sleep disorder.
Discussion
In a regression model adjusted for age, diabetes mellitus, hypertension, dyslipidemia, BMI, smoking history, and alcohol intake frequency, PCOS patients had a 1.244–fold greater incidence of depressive disorder, 1.502–fold greater incidence of bipolar disorder, 1.147–fold greater incidence of anxiety disorder, and 1.228–fold greater incidence of sleep disorder than the general population. The prevalence of depressive disorder, bipolar disorder, and anxiety disorder was greater in PCOS patients than in the general population, while the prevalence of schizophrenia and sleep disorders was lower in PCOS patients than in the general population.
We adjusted several factors before calculating HR to clarify the association between PCOS and mental disorders. We considered three chronic medical conditions related to the common metabolic features of PCOS2 for calculation, as chronic medical conditions have been associated with mental disorders.4 DM was associated with various mental disorder, such as mood disorders,20,21 anxiety disorders,20,21 eating disorders,21 and severe mental illness.22 For dyslipidemia, people with severe mental illness had increased risk for hypertriglyceridemia and low high density lipoprotein cholesterol.23 However, reported association between mental health and blood pressure was mixed.24 We also considered lifestyle factors: alcohol consumption and smoking. PCOS international guideline recommends assessing alcohol consumption and smoking in regards of fertility15 and modifying alcohol consumption and smoking is important in long-term treatment of PCOS.25 Though the association between alcohol consumption and PCOS was controversial in previous studies,26 association between alcohol consumption and decreased mental health27,28 is well known. Smoking is a risk factor for PCOS26 and various psychiatric conditions.29 It is worth noting that PCOS exhibited a higher risk for several mental disorders, even after adjusting for these factors in the main analysis and excluding individuals with a history of frequent alcohol consumption or smoking in the sensitivity analysis.
There have been few previous studies of schizophrenia in PCOS patients, and the reported HRs vary. A previous study reported a greater prevalence in PCOS patients than in controls,12 which is not consistent with our results. In one study, the crude HR and adjusted HR of schizophrenia were greater in PCOS patients than in the general population,30 while several studies have reported nonsignificant crude HR for schizophrenia.9,13 In our study, the crude HR and adjusted HR were not significant. The small number of patients with schizophrenia may have influenced our results. An inverse relationship between testosterone level and severity of negative schizophrenia symptoms has been reported.31 Therefore, PCOS, which is characterized by hyperandrogenemia, and schizophrenia may be associated with each other; however, additional research is required to address this hypothesis.
The prevalence8,10,12,32,33 and HR9,34 of depressive disorder and odds of depressive symptoms35 have been reported to be greater in PCOS patients than in the general population. Our results were consistent with these earlier studies. PCOS has biochemical characteristics highly related to the occurrence of depression: the decrease in inhibitory neurotransmitters (serotonin, dopamine, gamma-aminobutyric acid, acetylcholine, etc.) that leads to hyperactivity of the hypothalamic-pituitary-adrenal axis,36 and high inflammatory markers.37 Also, neurotransmitters such as dopamine might affect the gut-brain axis and regulate appetite and satiety.38 Obesity is a common clinical characteristic in PCOS and depressive disorders.37,39 A previous study showed that depressed PCOS patients had higher BMIs than non-depressed PCOS patients,33 and another study reported PCOS patients with lower BMI to have slightly lower depression score.40 Also, weight loss induced by dietary interventions improved PCOS-related chronic inflammation.41 These findings suggested that obesity, PCOS, and depressive disorder should be considered altogether during treatment.
Several studies have reported that the prevalence of bipolar disorder is greater in PCOS patients than in the general population.10,12,34 Our results were similar to those of prior studies. However, the reported HRs for bipolar disorder among PCOS patients are not consistent. Two previous studies reported greater HRs for bipolar disorder in PCOS patients than controls34,42 as in our study, while another study found no significant association between the two diseases.9 Patients with PCOS or bipolar disorder share common endophenotypes with regard to insulin resistance, hyperlipidemia, and other metabolic abnormalities.43 Several studies have suggested that valproic acid, a drug commonly prescribed for bipolar disorder, might be associated with PCOS,44,45 and valproate–treated females more frequently exhibited menstrual abnormalities, features of hyperandrogenism, and other adverse metabolic parameters than lithium–treated females.46 The similarities between the two diseases described above might, in part, explain the greater prevalence and HR of bipolar disorder in PCOS patients.
Elevated anxiety scores40 and greater prevalence8,10,12,34 and HR9,34 of anxiety disorder in PCOS patients were reported in previous studies. Two systemic reviews reported increased prevalence of anxiety symptoms in PCOS patients,47,48 consistent with our results. The factors contributing to the development of anxiety disorder in PCOS patients are under investigation. Hormonal features, such as hypothalamic-pituitary-adrenal-axis49 or hyperandrogenism,48 may associated with anxiety in PCOS patients. The BMI might also be associated with anxiety,40,48 which may have a significant impact on PCOS patients, considering that one of the most common symptoms of PCOS is obesity.
Several studies have shown that PCOS patients are at high risk of obstructive sleep apnea50 and sleep disturbance,51,52 which is not consistent with our findings, as the PCOS patients in our study population had a lower prevalence of sleep disorders. This difference may have resulted from our study and the previous studies having had different research scopes. The sleep disorders we studied were not limited to sleep apnea or sleep disturbance. A study using a more similar definition of sleep disorder to ours showed higher HR of sleep disorder in PCOS patients compared with controls9 and aligned with our results. Common symptoms experienced by PCOS patients, like obesity and insulin resistance,50 could be contributing to sleep disorder or sleep disturbance. In addition, several studies suggested that treatment of obstructive sleep apnea could improve cardiometabolic functions.53,54 It seems likely that there is an association between sleep disorders and PCOS, but the degree of association may vary depending on the type of sleep disorder. Further research on this subject is needed.
The overlapping symptoms of PCOS and mental disorders suggest that the two conditions may be inter-related, and that treatment of one condition might help improve the other. However, a careful approach is needed, as some treatments for one condition may aggravate the other condition: for example, some antipsychotic drugs can have negative consequences on the symptoms of PCOS.14 Therefore, we encourage medical staff to more seriously consider the possibility that PCOS patients might have comorbid mental disorders and carefully to select the treatment options.
Our subgroup analysis revealed disparities in the risk of mental disorders among PCOS patients. These findings suggest that the need for mental disorder screening in PCOS patients may differ according to age and obesity status. Clinical and biochemical manifestations of PCOS change with age,55 and obesity was related to PCOS55 and mental health56 both. How to approach these complex relationships requires further research.
We checked the liver enzyme level of study populations as an indirect index of liver function because PCOS is associated with non-alcoholic fatty liver disease.57 While our results showed a statistically significant difference in liver enzyme levels between PCOS patients and controls, the clinical relevance of this finding was unclear. In previous studies, most POCS patients with elevated liver enzymes had a high BMI.58,59 This suggests that PCOS diagnosis alone was not enough to identify the association between liver function and PCOS.
This study had several limitations. The National Health Insurance Services (NHIS) database used in this study was subject to a few restrictions, as it consisted of billing records. We could not identify any treatments not covered by medical insurance. Misdiagnosis or misclassification of PCOS and mental disorders may have occurred. We did not consider other potential confounders, such as socioeconomic status or the effects of drugs related to PCOS or mental disorders, because they could not be identified in our database. A small percentage of individuals had a medical check-up record for the index year, possibly due to the biennial national health examination schedule. The initial population data we received already exhibited age differences between individuals with and without PCOS, even though we requested the age-matched individuals’ data from the NHIS database. We used the matching technique to overcome the imbalance, though we couldn’t eliminate it. The patients were not matched with controls for BMI, which could significantly affect mental health. Therefore, we adjusted age and BMI when calculating HR. We didn’t distinguish the patients based on the usage of psychiatric medications, like sodium valproate, as we aimed to describe the overall association between PCOS and mental disorders in the Korean population. Further study could explore the potential effect of drugs that patients had taken. Nevertheless, this study is meaningful as it shows insight into the relationships between PCOS and mental disorders in the Korean population.
Conclusion
We evaluated the risk of mental disorders in PCOS patients using a Korean nationwide population–based cohort. Our results suggest that PCOS patients have increased risks of depressive disorder, bipolar disorder, anxiety disorder, and sleep disorder. There are a few limitations in our study in that our database consisted of data claimed for a limited period. This study supports the current international PCOS guidelines, which recommend screening for mental health disorders.15 Therefore, our study advocates for more active screening of mental disorders in Korean PCOS patients, taking into account the changing needs based on individual factors such as age and obesity.
Data Availability Statement
Data sharing is not applicable to this article due to the principles and restrictions of NHIC.
Funding
The authors wish to acknowledge the financial support of Catholic Medical Center Research Foundation made in the program year of 2020.
Disclosure
Professor Jeong Namkung reports grants from Catholic Medical Center, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. World Health Organization. Polycystic ovary syndrome. World Health Organization: Available from: https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome.
2. Louwers YV, Laven JSE. Characteristics of polycystic ovary syndrome throughout life. Ther Adv Reprod Health. 2020;14:2633494120911038. doi:10.1177/2633494120911038.
3. Christ JP, Cedars MI. Current guidelines for diagnosing PCOS. Diagnostics. 2023;13(6):1113. doi:10.3390/diagnostics13061113
4. Eaton WW. Public Mental Health.
5. Doherty AM, Gaughran F. The interface of physical and mental health. Soc Psychiatry Psychiatr Epidemiol. 2014;49(5):673–682. doi:10.1007/s00127-014-0847-7
6. Ohrnberger J, Fichera E, Sutton M. The relationship between physical and mental health: a mediation analysis. Soc sci med. 2017;195:42–49. doi:10.1016/j.socscimed.2017.11.008
7. Almhmoud H, Alatassi L, Baddoura M, et al. Polycystic ovary syndrome and its multidimensional impacts on women’s mental health: a narrative review. Medicine. 2024;103(25):e38647. doi:10.1097/MD.0000000000038647
8. Yin X, Ji Y, Chan CLW, Chan CHY. The mental health of women with polycystic ovary syndrome: a systematic review and meta-analysis. Arch Womens Ment Health. 2021;24(1):11–27. doi:10.1007/s00737-020-01043-x
9. Hung JH, Hu LY, Tsai SJ, et al.. Risk of psychiatric disorders following polycystic ovary syndrome: a nationwide population-based cohort study. Franks S. editor. PLoS ONE 2014 Vol. 9;e97041. doi:10.1371/journal.pone.0097041
10. Brutocao C, Zaiem F, Alsawas M, Morrow AS, Murad MH, Javed A. Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine. 2018;62(2):318–325. doi:10.1007/s12020-018-1692-3
11. Rodriguez-Paris D, Remlinger-Molenda A, Kurzawa R, et al. Psychiatric disorders in women with polycystic ovary syndrome. Psychiatr Pol. 2019;53(4):955–966. doi:10.12740/PP/OnlineFirst/93105
12. Cesta CE, Månsson M, Palm C, Lichtenstein P, Iliadou AN, Landén M. Polycystic ovary syndrome and psychiatric disorders: co-morbidity and heritability in a nationwide Swedish cohort. Psychoneuroendocrinology. 2016;73:196–203. doi:10.1016/j.psyneuen.2016.08.005
13. Karjula S, Arffman RK, Morin-Papunen L, et al. A population-based follow-up study shows high psychosis risk in women with PCOS. Arch Womens Ment Health. 2022;25(2):301–311. doi:10.1007/s00737-021-01195-4
14. Doretto L, Mari FC, Chaves AC. Polycystic ovary syndrome and psychotic disorder. Front Psychiatry. 2020;11:543. doi:10.3389/fpsyt.2020.00543
15. Teede HJ, Tay CT, Laven JJE, et al.. Recommendations from the 2023 international evidence-based guideline for the assessment and management of polycystic ovary syndrome. J Clin Endocrinol Metab. 2023:dgad463. doi:10.1210/clinem/dgad463
16. Ding T, Hardiman PJ, Petersen I, Wang FF, Qu F, Baio G. The prevalence of polycystic ovary syndrome in reproductive-aged women of different ethnicity: a systematic review and meta-analysis. Oncotarget. 2017;8(56):96351–96358. doi:10.18632/oncotarget.19180
17. Kakoly NS, Khomami MB, Joham AE, et al. Ethnicity, obesity and the prevalence of impaired glucose tolerance and type 2 diabetes in PCOS: a systematic review and meta-regression. Hum Reprod. 2018;24(4):455–467. doi:10.1093/humupd/dmy007
18. Kim JH, Jung MH, Hong SH, Moon N, Kang DR. Age-adjusted prevalence and characteristics of women with polycystic ovarian syndrome in Korea: a Nationwide Population-Based Study (92010-2019). Yonsei Med J. 2022;63(8):794–798. doi:10.3349/ymj.2022.63.8.794
19. Lee IO, Kim JC, Seo JW, Pak HY, Chung JE. Risk of developing major depressive disorder in polycystic ovary syndrome: a retrospective cohort study. J Obstetrics Gynaecol. 2021;41(7):1157–1161. doi:10.1080/01443615.2020.1849071
20. Lin EHB, Korff MV. Mental disorders among persons with diabetes—results from the world mental health surveys. J Psychosom Res. 2008;65(6):571–580. doi:10.1016/j.jpsychores.2008.06.007
21. Ducat L, Philipson LH, Anderson BJ. The mental health comorbidities of diabetes. JAMA. 2014;312(7):691–692. doi:10.1001/jama.2014.8040
22. Holt RIG, Mitchell AJ. Diabetes mellitus and severe mental illness: mechanisms and clinical implications. Nat Rev Endocrinol. 2015;11(2):79–89. doi:10.1038/nrendo.2014.203
23. Vancampfort D, Stubbs B, Mitchell AJ, et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry. 2015;14(3):339–347. doi:10.1002/wps.20252
24. Schaare HL, Blöchl M, Kumral D, et al. Associations between mental health, blood pressure and the development of hypertension. Nat Commun. 2023;14(1):1953. doi:10.1038/s41467-023-37579-6
25. Norman RJ, Davies MJ, Lord J, Moran LJ. The role of lifestyle modification in polycystic ovary syndrome. Trends Endocrinol Metab. 2002;13(6):251–257. doi:10.1016/S1043-2760(02)00612-4
26. Cowan S, Lim S, Alycia C, et al. Lifestyle management in polycystic ovary syndrome – beyond diet and physical activity. BMC Endocr Disord. 2023;23:14. doi:10.1186/s12902-022-01208-y
27. Jane-Llopis E, Matytsina I. Mental health and alcohol, drugs and tobacco: a review of the comorbidity between mental disorders and the use of alcohol, tobacco and illicit drugs. Drug Alcohol Rev. 2006;25(6):515–536. doi:10.1080/09595230600944461
28. Puddephatt J, Irizar P, Jones A, Gage SH, Goodwin L. Associations of common mental disorder with alcohol use in the adult general population: a systematic review and meta‐analysis. ADDICTION. 2022;117(6):1543–1572. doi:10.1111/add.15735
29. Firth J, Solmi M, Wootton RE, et al. A meta‐review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatry. 2020;19(3):360–380. doi:10.1002/wps.20773
30. Chen SF, Yang YC, Hsu CY, Shen YC. Risk of schizophrenia in patients with polycystic ovary syndrome: a nationwide population-based cohort study from Taiwan. J Psychosomatic Obstet Gynecol. 2021;42(4):272–278. doi:10.1080/0167482X.2020.1735342
31. Markham JA. Sex steroids and schizophrenia. Rev Endocr Metab Disord. 2012;13(3):187–207. doi:10.1007/s11154-011-9184-2
32. Bhattacharya SM, Jha A. Prevalence and risk of depressive disorders in women with polycystic ovary syndrome (PCOS). Fertil Sterility. 2010;94(1):357–359. doi:10.1016/j.fertnstert.2009.09.025
33. Hollinrake E, Abreu A, Maifeld M, Van Voorhis BJ, Dokras A. Increased risk of depressive disorders in women with polycystic ovary syndrome. Fertil Sterility. 2007;87(6):1369–1376. doi:10.1016/j.fertnstert.2006.11.039
34. Berni TR, Morgan CL, Berni ER, Rees DA. Polycystic ovary syndrome is associated with adverse mental health and neurodevelopmental outcomes. J Clin Endocrinol Metab. 2018;103(6):2116–2125. doi:10.1210/jc.2017-02667
35. Alur-Gupta S, Dokras A, Cooney LG. Management of polycystic ovary syndrome must include assessment and treatment of mental health symptoms. Fertil Sterility. 2024;121(3):384–399. doi:10.1016/j.fertnstert.2024.01.018
36. Xing L, Xu J, Wei Y, et al.. Depression in polycystic ovary syndrome: focusing on pathogenesis and treatment. Front Psychiatry. 2022:13. doi:10.3389/fpsyt.2022.1001484
37. Kolhe JV, Chhipa AS, Butani S, Chavda V, Patel SS. PCOS and depression: common links and potential targets. Reprod Sci. 2022;29(11):3106–3123. doi:10.1007/s43032-021-00765-2
38. Sarkisian KI, Ho L, Yang J, Mandelbaum R, Stanczyk FZ. Neuroendocrine, neurotransmitter, and gut microbiota imbalance contributing to potential psychiatric disorder prevalence in polycystic ovarian syndrome. F S Rep. 2023;4(4):337–342. doi:10.1016/j.xfre.2023.08.009
39. Dokras A. Mood and anxiety disorders in women with PCOS. Steroids. 2012;77(4):338–341. doi:10.1016/j.steroids.2011.12.008
40. Barry JA, Kuczmierczyk AR, Hardiman PJ. Anxiety and depression in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2011;26(9):2442–2451. doi:10.1093/humrep/der197
41. Alenezi SA, Elkmeshi N, Alanazi A, Alanazi ST, Khan R, Amer S. the impact of diet-induced weight loss on inflammatory status and hyperandrogenism in women with polycystic ovarian syndrome (PCOS)-A systematic review and meta-analysis. J Clin Med. 2024;13(16):4934. doi:10.3390/jcm13164934
42. Chen SF, Yang YC, Hsu CY, Shen YC. Risk of bipolar disorder in patients with polycystic ovary syndrome: a nationwide population-based cohort study. J Affective Disorders. 2020;263:458–462. doi:10.1016/j.jad.2019.12.007
43. Jiang B, Kenna HA, Rasgon NL. Genetic overlap between polycystic ovary syndrome and bipolar disorder: the endophenotype hypothesis. Med Hypotheses. 2009;73(6):996–1004. doi:10.1016/j.mehy.2008.12.056
44. Bilo L, Meo R. Polycystic ovary syndrome in women using valproate: a review. Gynecological Endocrinol. 2008;24(10):562–570. doi:10.1080/09513590802288259
45. Himelein MJ, Thatcher SS. Polycystic ovary syndrome and mental health: a review. Obstetrical Gynecol Surv. 2006;61(11):723–732. doi:10.1097/01.ogx.0000243772.33357.84
46. McIntyre RS, Mancini DA, McCann S, Srinivasan J, Kennedy SH. Valproate, bipolar disorder and polycystic ovarian syndrome: bipolar disorder and polycystic ovarian syndrome. Bipolar Disorders. 2003;5(1):28–35. doi:10.1034/j.1399-5618.2003.00009.x
47. Cooney LG, Lee I, Sammel MD, Dokras A. High prevalence of moderate and severe depressive and anxiety symptoms in polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 2017;32(5):1075–1091. doi:10.1093/humrep/dex044
48. Dokras A, Clifton S, Futterweit W, Wild R. Increased prevalence of anxiety symptoms in women with polycystic ovary syndrome: systematic review and meta-analysis. Fertil Sterility. 2012;97(1):225–230.e2. doi:10.1016/j.fertnstert.2011.10.022
49. Annagür BB, Kerimoglu ÖS, Tazegül A, Gündüz Ş, Gençoglu BB. Psychiatric comorbidity in women with polycystic ovary syndrome: psychiatric comorbidity in PCOS. J Obstet Gynaecol Res. 2015;41(8):1229–1233. doi:10.1111/jog.12696
50. Helvaci N, Karabulut E, Demir AU, Yildiz BO. Polycystic ovary syndrome and the risk of obstructive sleep apnea: a meta-analysis and review of the literature. Endocr Connections. 2017;6(7):437–445. doi:10.1530/EC-17-0129
51. Mo L, Mansfield DR, Joham A, et al. Sleep disturbances in women with and without polycystic ovary syndrome in an Australian National Cohort. Clin Endocrinol. 2019;90(4):570–578. doi:10.1111/cen.13922
52. Moran LJ, March WA, Whitrow MJ, Giles LC, Davies MJ, Moore VM. Sleep disturbances in a community-based sample of women with polycystic ovary syndrome. Hum Reprod. 2015;30(2):466–472. doi:10.1093/humrep/deu318
53. Harsch IA, Schahin SP, Radespiel-Tröger M, et al. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2004;169(2):156–162. doi:10.1164/rccm.200302-206OC
54. Tasali E, Chapotot F, Leproult R, Whitmore H, Ehrmann DA. Treatment of obstructive sleep apnea improves cardiometabolic function in young obese women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2011;96(2):365–374. doi:10.1210/jc.2010-1187
55. Bellver J, Rodríguez-Tabernero L, Robles A, et al. Polycystic ovary syndrome throughout a woman’s life. J Assist Reprod Genet. 2018;35(1):25–39. doi:10.1007/s10815-017-1047-7
56. Avila C, Holloway AC, Hahn MK, et al. An overview of links between obesity and mental health. Curr Obes Rep. 2015;4(3):303–310. doi:10.1007/s13679-015-0164-9
57. Rocha ALL, Faria LC, Guimarães TCM, et al. Non-alcoholic fatty liver disease in women with polycystic ovary syndrome: systematic review and meta-analysis. J Endocrinol Invest. 2017;40(12):1279–1288. doi:10.1007/s40618-017-0708-9
58. Economou F, Xyrafis X, Livadas S, et al. In overweight/obese but not in normal-weight women, polycystic ovary syndrome is associated with elevated liver enzymes compared to controls. Hormones. 2009;8(3):199–206. doi:10.14310/horm.2002.1236
59. Minato S, Sakane N, Kotani K, et al. Prevalence and risk factors of elevated liver enzymes in Japanese women with polycystic ovary syndrome. J Clin Med Res. 2018;10(12):904–910. doi:10.14740/jocmr3639
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Minimal Effects of Cariprazine on Prolactin Levels in Bipolar Disorder and Schizophrenia
Culpepper L, Vieta E, Kelly DL, Patel MD, Szatmári B, Hankinson A, Earley WR
Neuropsychiatric Disease and Treatment 2022, 18:995-1011
Published Date: 12 May 2022
Seasonal Effects on Hospitalizations Due to Mood and Psychotic Disorders: A Nationwide 31-Year Register Study
Törmälehto S, Svirskis T, Partonen T, Isometsä E, Pirkola S, Virtanen M, Sund R
Clinical Epidemiology 2022, 14:1177-1191
Published Date: 21 October 2022
Environmental Factors in the Etiology of Mental Disorders in the Czech Republic
Hosak L, Hosakova K, Malekirad M, Kamaradova Koncelikova D, Zapletalova J, Latalova K
Neuropsychiatric Disease and Treatment 2023, 19:349-359
Published Date: 7 February 2023
Albumin and Associated Biomarkers in Severe Neuropsychiatric Disorders: Acute-Phase Schizophrenia and Bipolar Disorder
Xu H, Zheng L, Wang L, Gao H, Wei Y, Chen J
Neuropsychiatric Disease and Treatment 2023, 19:2027-2037
Published Date: 28 September 2023
Transdiagnostic Effects of Schizophrenia Polygenic Scores on Treatment Outcomes in Major Psychiatric Disorders

Serretti A, Baune BT
Neuropsychiatric Disease and Treatment 2025, 21:547-562
Published Date: 13 March 2025


