Back to Journals » Journal of Pain Research » Volume 18
Serious Adverse Drug Reactions to Long-Term Oral Liquid Morphine in Patients with Chronic Pain: A Cross-Sectional Survey in Palliative Care
Authors Duncan B , Natuhwera G , Nassuuna D , Katusabe R, Kasozi H, Acuda W
Received 21 January 2025
Accepted for publication 1 May 2025
Published 8 May 2025 Volume 2025:18 Pages 2361—2371
DOI https://doi.org/10.2147/JPR.S515028
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Timothy Atkinson
Barbara Duncan,1 Germanus Natuhwera,1,2 Doris Nassuuna,3 Roselight Katusabe,1 Hanif Kasozi,1 Wilson Acuda2
1Clinical Department, Hospice Africa Uganda, Kampala, Uganda; 2Education Department, Institute of Hospice and Palliative Care in Africa, Kampala, Uganda; 3Research Department, International Rescue Committee, Kampala, Uganda
Correspondence: Germanus Natuhwera, Email [email protected]; [email protected]
Background: Behaviour suggestive of addiction in some patients on long-term oral liquid morphine (OLM) caused concern amongst the Hospice Africa Uganda clinical team and prompted the survey. This survey aimed to identify serious adverse drug reactions to long-term OLM in patients with chronic pain receiving palliative care.
Methods: In Phase 1, the database of patients receiving palliative care at Hospice Africa Uganda was analyzed to find patients taking OLM from 12.7.2017 to 19.10.2017. A purposive review of their medical records was undertaken to identify those on long-term OLM. Phase 2 was conducted between 12.6.2018 and 23.10.2018. All patients on long-term OLM were offered biopsychosocial and spiritual assessment by a pain specialist (BD) to determine whether they were experiencing any serious adverse drug reactions. Phase 3 immediately followed phase 2 assessment. The pain specialist discussed with the participant any medication changes (including OLM) or other therapies to facilitate holistic management of pain for the individual.
Results: In phase 1, 653 patients on OLM were identified. Phase 2 identified 49 patients who were on long-term OLM. Thirty-four patients agreed to participate in the assessment with the pain specialist. Of the 34 participants, 24 had chronic non-cancer pain and two had chronic cancer pain. Eight cancer survivors had incidental chronic non-cancer pain. Serious adverse drug reactions were identified in four participants with chronic non-cancer pain. Two cases of addiction, one case of opioid hyperalgesia, and one probable diversion of morphine.
Conclusion: To our knowledge, the study identified the first documented cases of addiction to OLM in sub-Saharan Africa. Future research involving a larger multicenter sample, longitudinal, and qualitative designs is needed. Education of healthcare practitioners prescribing opioids should put equal emphasis on management of chronic non-cancer pain as do chronic cancer pain to minimize the risk of serious adverse reactions.
Keywords: chronic pain, opioids, oral liquid morphine, palliative care, serious adverse drug reactions
Introduction
Opioids are essential medicines for providing good pain relief and are safe and effective in treating moderate to severe cancer pain.1–3 In Uganda, holistic palliative care, including skillful titration of opioid analgesics for optimal pain control, started in 1993 with the establishment of Hospice Africa Uganda (HAU) by Anne Merriman.4,5 This model for provision of culturally sensitive, affordable, and accessible African palliative care introduced cheap, locally reconstituted oral liquid morphine (OLM) for treatment of moderate to severe pain. HAU’s model is consistent with the World Health Organization (WHO) public health model for development of palliative care.6
Pain is a common complaint reported by patients in clinical settings, with a prevalence rate of 44.5% for cancer pain.7 The prevalence of chronic non-cancer pain (CNCP) varies widely from 13% to 50% across the world.8–11 In clinical settings, pain may be so severe and/or complex that it warrants expertise, skillful use and titration of analgesics, including strong opioids to achieve optimal pain control. However, in low-resourced countries such as Uganda, this may be hampered by several barriers such as opiophobia caused by lack of, or inadequate, training and lack of experiential exposure among health professionals.12 Education of healthcare professionals and the public is needed to overcome opiophobia – fear of addiction, diversion and misuse.1,13 The belief that oral opioids could not lead to addiction compared to systemic opioids helped to overcome opiophobia in 1993 through a landmark introduction of OLM into Uganda, particularly for management of moderate to severe cancer pain and advanced HIV/AIDS.5 Noteworthy, to date, there is no documented study in Uganda and perhaps on the entire African continent about whether long-term OLM therapy for chronic pain could carry a risk of serious adverse drug reactions (ADRs). An ADR is a harmful, unintended result caused by taking medication. ADRs may occur following a single dose or prolonged administration of a drug.
An earlier study had indicated that there is a low risk of addiction to opioids for cancer pain with a prevalence of 0–7.7%.14 In 2005, an evaluation study of a morphine public health programme assessing the feasibility and safety of morphine for chronic pain in cancer, HIV/AIDS and sickle cell disease in the community in sub-Saharan Africa (SSA), including Uganda, did not find evidence of opioid use disorder (OUD).15 Sadly, lack of universal health coverage16 and integrated specialist pain management services in Uganda leaves many patients reliant on palliative and hospice care services, which are limited in number for treatment of pain. Globally, the scope of palliative care has widened to include all non-communicable diseases, creating a situation where patients with numerous causes and types of pain, other than cancer and HIV/AIDS, are accepted by HAU. Anecdotal observations indicate that there is general limited knowledge about management of CNCP and the risks of ADRs from long-term OLM in Ugandan palliative care.
In 2013, it became apparent in the developed countries that prescribing oral opioids for CNCP is unsafe and ineffective.17 A rapid increase in opioid prescription in the USA coincided with about 28,000 deaths in 2014. These deaths were associated with prescription or illicit use of opioids not intended for clinical use in pain control18 and served as a global warning of the dangers of long-term oral opioid use.17–19 It is important that Ugandan palliative care clinicians take note of this warning as increasing numbers of patients with CNCP are being referred to them. Previous research shows that opioid therapy for chronic pain is associated with increased risk of overdose, OUD and dependence.20 Literature further cites that prescription OUD and chronic pain commonly occur together.21 Literature also shows that long-term opioid use may cause cognitive disorders, suppression of the endocrine and immune systems and opioid-induced hyperalgesia (OIH); a heightened pain sensitivity caused by opioid use.22,23
In recent years, prior to this study, the HAU clinical team in Kampala has recognized concerning trends related to morphine prescriptions in patients with chronic pain. These included early attendance for medication refills, repeatedly sending a caregiver and insisting on or requesting high doses of opioids for unrelieved pain or its increasing severity. Similar presentations have previously been recognized elsewhere as indicators of addiction to opioids.23,24
Thus, the aim of this survey was to identify patients with chronic pain of all causes on long-term OLM and to assess whether they experienced any serious ADRs.
Methods
Study Design and Population
This cross-sectional survey was conducted in three phases on patients receiving long-term OLM for chronic pain attending the HAU palliative care service in Kampala. HAU4 is a specialised health facility providing holistic, culturally sensitive patient-centered palliative care for patients and families living with life-threatening and life-limiting illnesses using an affordable African palliative care model.
Definition of Key Terms
Chronic pain was defined as pain with a duration of six or more months.25
Long-term morphine use was defined as one prescription per month for six months or longer.23
Participant Sampling and Recruitment Criteria
Purposive sampling was utilised to identify eligible participants. In phase 1, a patient’s case file was eligible for selection if the patient was on OLM for pain of any cause. Furthermore, upon initial review, a participant was eligible for enrollment into phase 2 of the study if they were-: (i) on OLM with one prescription per month for six months or longer, (ii) had CCP or CNCP with duration of at least six months, (iii) aged 12 years and above, (iv) able to give informed written consent to be assessed, (v) able to communicate in English or Luganda and (vi) physically and psychologically well enough to participate. Participants gave written informed consent unless they were illiterate, in which case thumbprint signatures were confirmed by a witness.
A participant was ineligible for selection if they (i) declined assessment, (ii) were no longer taking morphine at the time of the study, (iii) died before could be assessed, (iv) were too unwell to participate and (v) lived far and were unable to attend face-to-face assessment.
Data Collection Procedures and Instruments
In phase 1 of the study, medical records of 653 patients on OLM who were receiving palliative care at the Kampala site of HAU were identified from the HAU Kampala database between 12.7.2017 and 19.10.2017. A purposive review of the 653 patients’ files was carried out by the third author (DN) who inspected each file for pain diagnosis, current dose and highest dose of OLM. Duration of pain and duration of pain treatment with OLM were documented. Forty-nine patients on long-term OLM for CNCP and chronic cancer pain (CCP) were identified. Of the 49 patients, 34 agreed to be assessed by the pain specialist in phase 2 of the study. The reasons for not participating were-: (i) two patients declined assessment, (ii) the carer refused access to one patient (iii) seven were no longer taking morphine, (iv) two died prior to the study, (v) one was too unwell to participate, and (vi) two were living too far to attend. Although we would have recruited anyone aged 12 years and above in phase 2 of the study, one patient aged 12–23 years declined to participate. Hence, minimum age recruited was 24 years.
Phase 2 was conducted between 12.6.2018 and 23.10.18 and involved face-to-face detailed biopsychosocial and spiritual assessment by a pain specialist (BD) of the identified 34 participants on long-term OLM. We acknowledge this is a small number of participants for a descriptive cross-sectional survey and limits the generalizability of the results and their interpretation. ADRs related to OLM were established during the assessment using a checklist and documented. A researcher-developed guide was based on a full clinical examination. It included a medical history with specific questions related to pain, medication, ADRs to OLM, maximum daily dose of OLM, a full neurological assessment, a social history (occupation, housing, finance, family and significant relationships), a mood assessment, and a spiritual assessment adapted from the African Palliative Care Association (APCA) African Palliative Care Outcome Scale (POS).26 The result was discussed with a consultant psychiatrist (WA) to establish whether a full psychiatric assessment was needed. The POS has two items reflecting spiritual well-being.27 These are: (i) over the past three days, have you felt that life was worthwhile? and (ii) over the past three days, have you felt at peace? Possible responses are rated on a 6-point Likert scale ranging from 0 to 5 with a zero-response denoting “not at all” and a 5-response denoting “yes, all the time”.
The research assistant (DN) was fluent in English and Luganda and acted as an interpreter during the assessment if it was needed. The lead author (BD) and a consultant psychiatrist (WA) discussed the assessment outcomes to determine if further psychiatric or psychosocial assessment by a social worker was needed as part of a holistic approach to pain management. Psychiatric assessment used the Mental State Examination, which is a structured, validated tool28,29 used to assess patient’s current mental state. It evaluates general appearance, behaviour, beliefs, mood and cognition. It is a most widely used instrument for assessing mental disorders internationally. Nine versus three participants met the criteria for further assessment by consultant psychiatrist and social worker respectively.
In phase 3, ADRs of OLM were discussed with individual participants. Appropriate individualized options and changes in pain management plan, including adjustment of OLM dosages, were discussed and implemented with each participant’s agreement. Participants were appropriately referred to the clinical palliative care team with advice for continued management. The consultant psychiatrist and pain specialist, or clinical services coordinator (RK), continued supporting the clinical team with follow-up and management of complex cases related to OUD and OIH that required further close expert attention.
SPSS v25 was used for descriptive data analysis to summarize the data mainly using frequencies and percentages. No data was missing from the 34 participants.
Results
All the 49 patients identified on long-term OLM were black Africans. Thirty-four participated in phase 2 and completed the biopsychosocial and spiritual assessment. Thirty-two (94%) of the participants (n=34) had CNCP, and eight of these participants had been successfully treated for cancer. Two participants had CCP. Twenty-three (68%) of the 34 participants were female.
The Age Range, Duration and Doses of Morphine Prescribed Can Be Seen in Table 1
Fifty-four causes of chronic pain were found in the 34 participants. Eleven categories of pain were identified (Table 2).
 |
Table 1 Age, Oral Liquid Morphine Duration and Doses Prescribed |
 |
Table 2 Categories of Pain in 34 Participants |
Expert Recommendation on Change in OLM Dose
Changes to pain medication were discussed with participants during Phase 3 assessment. Outcomes of discussion relating to OLM can be seen in Table 3 and Figure 1. Reasons for continuing same dose included introduction of other measures (eg psychological interventions) to manage pain before oral liquid morphine dose reduction.
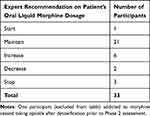 |
Table 3 Phase 2 – Change in Oral Liquid Morphine Dose as Recommended by the Pain Specialist (BD) and Consultant Psychiatrist (WA) |
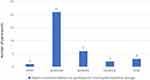 |
Figure 1 Showing number of participants against expert recommendation on participants’ oral liquid morphine dosage (n=33). |
Serious Adverse Drug Reactions to OLM
Three cases of OUD were identified in the 32 participants with CNCP. There were two cases of addiction and one case of probable diversion. One case of OIH was identified.
Of the nine participants referred to the consultant psychiatrist (WA) for expert psychiatric attention, three did not attend their appointment. Two participants received relaxation exercises to perform at home. One was advised to increase amitriptyline. Two received supportive psychotherapy, one of whom was also advised to increase amitriptyline. These expert interventions and therapies were beneficial. The ninth participant did not need any psychological treatment as his mood was normal. Three participants were referred to the HAU social worker for psychosocial supportive care, of whom two received bereavement counseling but the third rejected assistance.
Spiritual assessment revealed most participants (85%) were at peace and felt that life was worthwhile (74%) all or most of the time. None of the participants required referral for specialist spiritual care.
Case Histories of Four Patients with Severe CNCP are Described Below
The following case histories of serious ADRs to OLM demonstrate the importance of recognizing and managing them.
Sickle-Cell Disease and Addiction
Case 1
Patient A had Sickle Cell Disease and chronic pain caused by necrosis of the neck of femur. At presentation the patient was self-injecting intravenous (IV) pethidine for pain relief. IV pethidine was successfully substituted with OLM. After some time, it became apparent that IV pethidine was again being used alongside OLM. Despite extensive supportive psychotherapy and education about the harms of IV pethidine, the patient continued self-injection whilst also returning early for repeat OLM prescriptions. A diagnosis of opioid addiction was made. Although this patient agreed to assessment, she declined further management by the consultant psychiatrist. After some months, the patient moved out of the study area to her home area 250 kilometers away and became lost-to-follow up despite the team’s relentless efforts to follow her up. It was later learnt that she continued to receive palliative care from her local palliative care service.
Case 2: Addiction in Sickle Cell Disease
Participant B had been established on OLM at HAU for chronic pain caused by repeated sickling crises. A pattern of requests for early refills of OLM or sending a carer for a morphine prescription suggested the patient might have opioid dependence. Before participation in phase 2 of the study, the participant presented at HAU as an acute emergency with a withdrawal syndrome from morphine. There was immediate referral to a psychiatrist who transferred this participant to a private hospital where the participant underwent a detoxification programme. At the subsequent research assessment at HAU, the participant had symptoms of depression with suicidal ideation, and it became clear there were profoundly difficult psychosocial circumstances. She was referred to consultant psychiatrist (WA) for further expert psychiatric review and attention but failed to attend. Her haematologist managed further sickle cell crises by admitting her to hospital for intravenous paracetamol as analgesia and avoided prescribing opioids.
Case 3: Diversion of Morphine
Participant C with a diagnosis of chronic pancreatitis pain due to alcohol use disorder had been receiving OLM prescriptions of high dosages ie 5400 mg liquid oral morphine daily before a referral by a physician to HAU. Clinical assessment by a consultant psychiatrist (WA) confirmed alcohol dependence. In conjunction with weekly psychosocial support by psychiatrist and either a pain specialist (BD) or clinical services coordinator (RK), the dose of morphine was reduced gradually to 90 mg daily. It was suspected that morphine was used as substitute for alcohol and probably diverted as he repeatedly showed no features of OLM side effects despite taking a very high dose. He was referred to a specialist drug treatment service for management of alcohol dependence and had not returned to HAU by the end of this study.
Case 4: Opioid-Induced Hyperalgesia (OIH)
Participant C was referred to HAU by a gynaecologist for management of severe pelvic pain due to endometriosis. The participant had been on 300 mg of OLM and presented with symptoms of OIH, ie widespread pain with allodynia on gentle skin touch, particularly on the forearm. Assessment by the consultant psychiatrist (WA) revealed the participant was extremely anxious, distressed and depressed not only about the pain but also about the uncertain prospect of having children in future resulting from her awareness that endometriosis is associated with infertility.
The participant received weekly psychosocial intervention jointly by WA and BD or RK, which included psychoeducation about endometriosis and OIH and its management. In addition to relaxation training, amitriptyline was increased to 50 mg daily for about 3 months. The participant complied with the medical advice to reduce morphine from 300 mg to 1.25 mg daily. Her pain and mood dramatically improved, and she was discharged back to her gynaecologist for continued management of endometriosis.
Discussion
This study aimed to identify serious ADRs to long-term use of OLM among patients with chronic pain receiving palliative care at HAU. The study identified four serious ADRs: two cases of addiction (both in sickle cell disease) and one case of probable diversion and opioid-induced hyperalgesia (OIH) each.
However, it is not possible to determine the prevalence of ADRs accurately with this small sample size. Nevertheless, these remain noteworthy findings in a low resource setting where knowledge about management of CNCP and presentations of OUD and OIH are limited not only among palliative care clinicians but also general healthcare professionals. Pain management services in the developed world are more advanced and familiar with CNCP and problems of OUD and often work alongside addiction services. Lack of integrated pain management services in Uganda leaves all palliative care services facing this problem alone. Enough body of research evidence has shown that pain management in low- and middle-income countries is hampered by a number of barriers including lack of or limited trained healthcare professionals with knowledge of pain management, lack of integrated pain management services and limited expertise and awareness of the role of multidisciplinary pain clinics.30–33 As a result of this study, the Institute of Hospice and Palliative Care in Africa, the educational arm of HAU, introduced management of CNCP in all its courses to increase awareness of the risks of prescribing long-term OLM to this group of patients. This is the first study to document addiction to OLM in Uganda and possibly in SSA. Codeine misuse, dependence and lack of provision for its treatment have been reported in South Africa.34 Addiction to oral tramadol is widely recognized in North and West Africa.35,36 Our literature searches have not found any reference of addiction to OLM in SSA.
Noteworthy, the two cases of addiction identified in this study had sickle cell disease, suggesting that this group of patients maybe more likely to develop psychological disorder which may predispose them to developing OUD as reported in a UK study, which found that 46% of sickle cell disease patients in a London hospital met criteria for depression and anxiety.37 However, it is important to mention that some of the findings of this study need to be interpreted with caution. For example, regarding the two cases of addiction, participant (B) who became addicted to OLM had symptoms of depression when assessed which may have been as a result of psychosocial problems, while addiction in participant (A) could have been largely due to or precipitated by self-injecting with IV pethidine. We acknowledge that the cross-sectional design of this study had limitation in observing causal trends over time. Another study had reported that depressed patients with CNCP may use opioids for self-management of insomnia and/or depression, which may progress to long-term use.38
The probable case of diversion identified in this study occurred in a patient who was taking very high doses of OLM, was a known alcohol-dependent person and appeared to have no caregiver as he always attended HAU alone. A strong association between long-term opioid use and a clustering of addictive behaviours was found in one study.23 Six addictive behaviours were identified – daily smoking, high alcohol intake, illicit drug use in the past year, obesity and long-term use of benzodiazepines and benzodiazepine-related drugs. However, long-term and short-term opioid users were more likely to abstain from alcohol. Behaviours prior to taking opioids had not been studied. Opioids may reduce the need for alcohol. Patient C may have substituted OLM for alcohol and then continued to request higher doses to divert morphine to others.
One participant with endometriosis had Opioid Induced Hyperalgesia (OIH) (Case 4). Endometriosis is a condition in which cells lining the endometrium (the inner lining of the uterus) grow outside the uterus, often involving the pelvic tissues, including the ovaries, fallopian tubes and other organs. It is associated with infertility. It can cause severe pelvic pain, anxiety, distress and depression. OIH is a state characterized by paradoxical worsening of pain as opioid doses are increased and pain may be felt in other areas of the body. Management is by gradual reduction in the dose of opioid,22 which was successfully implemented in this participant who also required extensive psychosocial intervention and an increased dose of antidepressant. Improvement of pain on reducing opioid dose supports the hypothesis that increasing doses of morphine caused OIH but her improved mood could have contributed as well. The participant responded very well to intensive psychological intervention which included psychoeducation, relaxation training and an increased dose of antidepressant by the psychiatrist. The finding corroborates Jamison et al21 who reported that effective pain treatment is nearly impossible in the context of persistent depression. Depression is reported to be prevalent at 12–27% in studies of opioid overdose.39,40
Addiction to oral opioids has been reported in previous studies in the developed world,16,17, while other previous research contends that the risk of opioid addiction in CCP is low.14 Our study has salient findings that are worth noting. For example, the three cases of OUD, ie two cases of addiction and one probable diversion, were identified in patients with CNCP. Our study highlights the urgent need for creation of awareness of OUD in CNCP, remembering that even cancer survivors with incidental CNCP may be in need of continued analgesia which may prolong their use of opioids. Another earlier evaluation study of a morphine public health programme for cancer and AIDS pain relief in SSA found no evidence of OUD, including addiction, in Uganda.15
Finding of serious cases of OUD in this study should act as a call for clinicians to be alert and able to identify and manage cases of opioid use disorder in a timely manner. Education of morphine prescribers and all healthcare professionals in the recognition and management of opioid use disorder is essential. It is equally important to prevent opiophobia, which can unjustly deny opioids for patients who need opioid analgesia for relief of moderate to severe pain.1,13 The harm of inadequate analgesia must be balanced against harm of possible risk of addiction, diversion and misuse of prescription opioids.41
In several developed countries, eg UK, use of opioid analgesia in patients with CNCP is only recommended as a last resort, once all other appropriate treatments have been tried and they have proven to be ineffective or yielded suboptimal analgesia. The Faculty of Pain Medicine in UK19 advise a closely monitored two-to-four-week trial of an opioid at a maximum dose of 120mg/day morphine (or equivalent) because there is no evidence of efficacy of high doses of opioids in the long-term. If the pain has not responded to this dose, then the opioid should be gradually reduced and stopped.42
Finally, this study has highlighted the importance of psychosocial interventions in patients with CNCP, which was successfully applied in our participants with pancreatic pain and endometriosis. Pain causes psychological distress, anxiety and depression, and these can potentially intensify pain.43 Therefore, it is essential that all clinicians routinely assess for mood and psychosocial problems in patients with CNCP and address them appropriately and early enough to optimize pain relief and improve quality of life of patients.
Strengths and Limitations of the Study
First, this was the first study to examine serious ADRs among patients with CCP and CNCP on long-term OLM at HAU. Prior to this study, palliative care practitioners at HAU, in Uganda and perhaps elsewhere in Africa, were not aware of the possibility of serious ADRs, particularly OUD (addiction and probable diversion) and OIH which were uncovered by this study. Second, to our knowledge, based on findings of a rigorous review, our study is the first documentation of addiction to OLM in sub-Saharan Africa. This calls for vigilance from palliative care practitioners and other clinicians to prevent, identify and effectively manage serious ADRs as soon as they develop. Timely involvement of other expertise, eg in addiction, is useful to manage OUD and achieve better treatment outcomes. The study findings should increase clinicians’ awareness of the challenge of OUD.
The study has a few limitations to acknowledge. First, the sample size was small. Second, this was a single-center study. Thus, findings have limited representativeness and limited generalizability. Therefore, the findings should be interpreted with caution. Furthermore, the small sample size meant that data analysis was only descriptive using crude frequencies and percentages without performing further data analysis, eg inferential statistics, to identify other probable predictors of serious ADRs other than OLM. Future studies should recruit a large multicenter sample. Third, there is a possibility of survivor bias. For example, 15 patients were not assessed in phase 2, while other ADRs may have been missed in those who declined to participate or died before commencement of the study. Nonetheless, the study signposts clinicians to be aware, closely monitor and search for OUD in patients on long-term opioid treatment. Fourth, the cross-sectional design with its one-point data collection limits interpretation of causality ie could have potentially limited chances of identifying causal relationships and OUD cases that may develop over time. Follow-up studies including randomized-controlled trials are needed, as well as qualitative study designs to gain a more nuanced understanding of this topic of public health importance.
Conclusion
Four serious ADRs to OLM were found in this survey. Addiction was likely to be found amongst sickle cell disease patient population. Whereas one may argue that a prevalence of 6% of OUD identified in this study is low, we must be concerned about every single case of OUD. Education on management of CNCP is essential for all morphine prescribers in Uganda, bearing in mind that CNCP management is uniquely different compared to CCP. Furthermore, pain management should not only be limited to palliative care services but rather be widely integrated into Uganda’s healthcare system.
There is a need for similar multicenter studies in health facilities in Uganda where OLM is prescribed for CNCP and CCP. Forward, longitudinal, and qualitative studies are needed and would be able to elicit and identify OUD and their causal relationships, including manifestations and factors associated with their development among patients. It is also important that interdisciplinary team working with expertise in mental health and addiction services be prioritized and utilized to optimize assessment and management of OUD when detected or even suspected.
Abbreviations
ADRs, Adverse Drug Reactions; APCA, African Palliative Care Association; CCP, Chronic Cancer Pain; CNCP, Chronic Non-Cancer Pain; HAU, Hospice Africa Uganda; IV, Intravenous; OIH, Opioid Induced Hyperalgesia; OLM, Oral Liquid Morphine; OUD, Opioid Use Disorder; POS, Palliative care Outcome Scale; SD, Standard Deviation; SSA, sub-Saharan Africa; WHO, World Health Organization.
Data Sharing Statement
The datasets generated and/or analysed in this study are reported in this manuscript. Anonymized raw data are available from the corresponding author only on reasonable request: [email protected] or [email protected].
Ethics and Participant Consent Statement
Ethical approval was obtained from Hospice Africa Uganda Research Ethics Committee (Reference: HAUREC 036/17) and from Uganda National Council for Science and Technology (Reference: HS 2371). Permission to access the HAU patient care electronic medical records to retrieve patients’ medical records was granted by the HAU management. Whilst recruitment was considered from the age of 12 years, the minimum age recruited was 24 years. All medical notes of patients reviewed in phase 1 had written informed consent obtained from each individual patient at enrollment into care granting permission to HAU to use the patients’ data for research, advocacy and/ or fundraising. Furthermore, all participants who were found eligible for phase 2 recruitment gave written informed consent to participate and publish. All data collected and reported in the study were anonymized to ensure anonymity. The study was conducted and reported in accordance with guidelines for the conduct of ethical research in Uganda and Declaration of Helsinki.
Acknowledgement
The authors would like to thank the patients who agreed to participate in the study, and Ms. Beata Coffey, Information Specialist at the Royal Society of Medicine Library for her support with undertaking literature search on addiction to oral opioids in sub Saharan Africa which informed this study.
Author Contributions
All authors contributed substantially to the work; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure
The authors have no competing interests to declare.
References
1. O’Brien M, Mwangi-Powell F, Adewole I, et al. Improving access to analgesic drugs for patients with cancer in sub-Saharan Africa. Lancet Oncol. 2013;14(4):e176–e82. doi:10.1016/S1470-2045(12)70343-1
2. Wiffen PJ, Wee B, Moore RA. Oral morphine for cancer pain. Cochrane Database Syst Rev. 2016; 4: CD003868.
3. World Health Organization (WHO). Model list of essential medicines. Available from: https://apps.who.int/iris/bitstream/handle/10665/325771/WHO-MVP-EMP-IAU-2019.06-eng.pdf?ua=1.
4. Hospice Africa Uganda. Available from: www.hospice-africa.org.
5. Jagwe J, Merriman A. Delivering analgesia in Rural Africa: opioid availability and nurse prescribing. J Pain Symptom Manage. 2007;33(5):547–551. doi:10.1016/j.jpainsymman.2007.02.014
6. Stjernsward J, Foley K, Ferris F. The public health strategy for palliative care. J Pain Sympt Manage. 2007;33(5):486–493. doi:10.1016/j.jpainsymman.2007.02.016
7. Snijders RA, Brom L, Theunissen M, et al. Update on prevalence of pain in patients with cancer 2022: a systematic literature review and meta-analysis. Cancers. 2023;15(3):591. doi:10.3390/cancers15030591
8. Reid KJ, Harker J, Bala MM, et al. Epidemiology of chronic non-cancer pain in Europe: narrative review, pain treatments and pain impact. Curr Med Res Opin. 2011;27(2):449–462. doi:10.1185/03007995.2010.5843
9. Fayaz A, Croft P, Langford R, et al. Prevalence of chronic pain in the UK: a systematic review and meta-analysis of population studies. BMJ Open. 2016;6(6):e010364. doi:10.1136/bmjopen-2015-010364
10. Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273–e283. doi:10.1016/j.bja.2019.03.023
11. Ekholm O D, Davidsen M, Davidsen M, et al. Increasing prevalence of chronic non-cancer pain in Denmark from 2000-2017: a population-based survey. Eur J Pain. 2022;3(3):624–633. doi:10.1002/ejp.1886
12. Nchako E, Bussell S, Nesbeth C, Odoh C. Barriers to availability and accessibility of controlled medicines in Africa. International Health. 2018;10(2):71–77. doi:10.1093/inthealth/ihy002
13. Berterame S, Erthal J, Thomas J, et al. Use of and barriers to access to opioid analgesics: a worldwide, regional, and national study. Lancet. 2016;387(10028):1644–1656. doi:10.1016/S0140-6736(16)00161-6
14. Højsted J, Sjøgren P. Addiction to opioids in chronic pain patients: a literature review. Eur J Pain. 2007;11(5):490–518. doi:10.1016/j.ejpain.2006.08.004
15. Logie DE, Harding R. An evaluation of a morphine public health programme for cancer and AIDS pain relief in Sub-Saharan Africa. BMC Public Health. 2005;5(1):82. doi:10.1186/1471-2458-5-82
16. World Health Organization. Data: universal health coverage. 2023. Available from https://data.who.int/countries/800.
17. Stannard C. Where now for opioids in chronic pain? Drug Ther Bull. 2018;118–122. doi:10.1136/dtb.2018.10.000007
18. Knaul FM, Farmer PE, Krakauer EL, et al. Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the lancet commission report. Lancet. 2017.
19. Becker WC, Fiellin DA. Limited evidence, faulty reasoning, and potential for a global opioid crisis. Br Med J. 2017;358:j3115. doi:10.1136/bmj.j3115
20. Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a national institutes of health pathways to prevention workshop. Ann Intern Med. 2015;162(4):276–286. doi:10.7326/M14-2559
21. Jamison RN, Dorado K, Mei A, Edwards RR, Martel MO. Influence of opioid-related side effects on disability, mood, and opioid misuse risk among patients with chronic pain in primary care. PAIN Reports. 2017;2(2):e589. doi:10.1097/PR9.0000000000000589
22. Mao J. Opioid-induced hyperalgesia. Pain Clin Updates. 2008;XVI.
23. Hojsted J, Ekholm O, Kurita GP, Juel K, Sjogren P. Addictive behaviours related to opioid use for chronic pain: a population-based study. Pain. 2013;154(12):2677–2683. doi:10.1016/j.pain.2013.07.046
24. Ballantyne JC, Stannard C. New addiction criteria: diagnostic challenges persist in treating pain with opioids. PAIN Clinical Updates XXI. 2013;1:1–7.
25. Treede R-D, Rief W, Barke A, et al. A classification of chronic pain for ICD-11. Pain. 2015;156(6):1003–1007. doi:10.1097/j.pain.0000000000000160
26. Harding R, Selman L, Agupio G, et al. Validation of a core outcome measure for palliative care in Africa: the APCA African Palliative Outcome Scale. Health Qual Life Outcomes. 2010;8(1):10. doi:10.1186/1477-7525-8-10
27. Selman L, Speck P, Gysels M, et al. ‘Peace’ and ‘life worthwhile’ as measures of spiritual well-being in African palliative care: a mixed-methods study. Health Qual Life Outcomes. 2013;11(1):94. doi:10.1186/1477-7525-11-94
28. Soltan M, Girguis J. How to approach the mental state examination. BMJ. 2017;8(357):j1821. doi:10.1136/sbmj.j1821
29. Huline-Dickens S. The mental state examination. Adv Psychiatric Treat. 2013;19(2):97–98. doi:10.1192/apt.bp.112.010215
30. Morriss WW, Roques CJ. Pain management in low- and middle-income countries. BJA Educ. 2018;18(9):265–270. doi:10.1016/j.bjae.2018.05.006
31. Bond M. Pain education issues in developing countries and responses to them by the international association for the study of pain. Pain Res Manag. 2011;16(6):404–406. doi:10.1155/2011/654746
32. Marun GN, Morriss WW, Lim JS, Morriss JL, Goucke CR. Addressing the challenge of pain education in low-resource countries: essential pain management in Papua New Guinea. Anesth Analg. 2020;130(6):1608–1615. doi:10.1213/ANE.0000000000004742
33. Cardosa MS. Promoting multidisciplinary pain management in and achievements. Pain. 2024;165(11):S39–S49. doi:10.1097/j.pain.0000000000003369
34. Parry CDH, Rich E, Van Hout MC, Deluca P. Codeine misuse and dependence in South Africa: perspectives of addiction treatment providers. South Afr Med J. 2017;107(5):451–456. doi:10.7196/SAMJ.2017.v107i5.12242
35. Salm-Reifferscheidt L. Tramadol: Africa’s opioid crisis. Lancet. 2018;391(10134):1982–1983. doi:10.1016/S0140-6736(18)31073-0
36. Ajayi AI, Somefun OD. Recreational drug use among Nigerian university students: prevalence, correlates and frequency of use. PLoS One. 2020;15(5):e0232964. doi:10.1371/journal.pone.0232964
37. Bridges G, Forden G, Tsitsikas D. Unmet psychological need/support in patients with sickle cell disease. PO-125. Br J Haematol. 2017;176(Suppl 1):5–145.28.
38. Sullivan MD. Why does depression promote long-term opioid use? Pain. 2016;157(11):2395–2396. doi:10.1097/j.pain.0000000000000658
39. Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose. Ann Internal Med. 2010;152(2):85–92. doi:10.7326/0003-4819-152-2-201001190-00006
40. Braden JB, Russo J, Fan M-Y, et al. Emergency department visits among recipients of chronic opioid therapy. Arch Intern Med. 2010;170(16):1425–1432. doi:10.1001/archinternmed.2010.273
41. Lancet Oncology T, Lancet Oncology Editorial. Access to opioids: a balance of harms. Lancet Oncol. 2017;18(10):1285. doi:10.1016/S1470-2045(17)30704-0
42. Faculty of Pain Medicine of the Royal College of Anaesthetists (UK). Opioids for long term pain. n.d. Available from: https://fpm.ac.uk/opioids-aware-clinical-use-opioids/opioids-long-term-pain.
43. Castillo RC, Wegener ST, Heines SE, et al. Longitudinal relationship between anxiety, depression and pain: results of a two-year cohort study of patients with lower extremity pain. Pain. 2013;154(12):2860–2866. doi:10.1016/j.pain.2013.08.025
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

