Back to Journals » Open Access Journal of Sports Medicine » Volume 15
Short-Term Intermittent Normobaric Hypoxia Combined with Light Exercise Improves Acclimatization of Cardiorespiratory Function in Inactive Adults
Authors Aljaloud KS
Received 13 September 2024
Accepted for publication 13 December 2024
Published 17 December 2024 Volume 2024:15 Pages 229—237
DOI https://doi.org/10.2147/OAJSM.S492820
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Andreas Imhoff
Khalid S Aljaloud
Department of Exercise Physiology, College of Sport Sciences and Physical Activity, King Saud University, Riyadh, Saudi Arabia
Correspondence: Khalid S Aljaloud, Department of Exercise Physiology, College of Sport Sciences and Physical Activity, King Saud University, P O Box 2454, Riyadh, Saudi Arabia, Tel +966-8063100, Email [email protected]
Background: Un-acclimatized individuals may experience acute altitude illness. Thus, the current study investigated the impact of short-term intermittent normobaric hypoxia (NH) combined with light exercise on the acclimatization of cardiorespiratory function to altitude in inactive adults.
Methods: This quasi-experimental study recruited 10 inactive university students (age: 26.3 ± 2.53 years). All participants were instructed to perform light exercise while exposed to intermittent NH (15%) (2 h/d) for 2 weeks continuously. The heart rate (HR), relative oxygen consumption (VO2 mL/kg/min), minute ventilation (VE), VO2/HR, and respiratory frequency (RF) were measured.
Results: Results illustrated a significant improvement in participants’ cardiorespiratory functions by 10 days after exposure to NH, as compared to day 1 of exposure, based on their HR, RF, and VE responses at rest and HR, RF, VE, VO2, VO2/kg, and VO2/HR during light exercise. Resting-state values had returned to the pre-NH exposure levels after 10 days of intermittent NH exposure. Furthermore, values measured during light exercise were significantly decreased on days 10 and 14 as compared to day 1 of NH exposure.
Conclusion: This study concluded that as few as 10 days of exposure to intermittent NH (pO2 = 15%) combined with light exercise may improve the acclimation to NH of 15% pO2 in inactive adults.
Keywords: altitude, acclamation, oxygen consumption, health-related fitness, training, sedentary
Introduction
Moving to altitude, ie, 1500 m or higher above sea level, leads to several physiological changes that reduce physical performance.1–3 Due to the lower atmospheric pressure, individuals demonstrate a significant reduction in blood oxygen saturation, alveolar partial pressure of oxygen, and arteriovenous oxygen difference in the first few days after arrival at such altitudes, which leads to a decreased of oxygen delivery to tissues.4,5 Consequently, a substantial reduction in cardiorespiratory function results in increased resting heart rate, breathing rate, and loss of body water. Consequently, a significant reduction in aerobic fitness markers, such as oxygen consumption, cardiac output, lactate concentration, and ventilatory capacity, has been reported.6,7
Oxygen consumption capacity (VO2) reflects cardiorespiratory fitness, including aerobic endurance capacity, which can be improved by endurance training.8,9 Sufficient levels of blood hemoglobin (HB) and hematocrit (Hct) improve the ability of red blood cells to transport oxygen to the working tissues, which enhances aerobic exercise performance. Higher levels of HB generally indicate better oxygen transport and higher aerobic endurance.10 Numerous studies have reported elevated HB and Hct concentrations in high-altitude populations.11,12
People who move to higher altitudes for leisure, sports, or tourism may find that it requires additional physical effort to perform the same physical activity they usually perform at sea level. Un-acclimatized individuals may experience acute altitude illness within a few hours of hypoxic exposure above 2500 m13, which affects their cardiovascular and respiratory functions.14,15 Moreover, tourists and mountaineers usually experience some illness symptoms or acute mountain sickness (AMS) at high altitudes.16 AMS is characterized by headache, dizziness, vomiting, anorexia, fatigue, and insomnia a few hours after reaching a high altitude17. Tourists and people who plan to visit high-altitude areas are recommended to prepare for AMS.18 The available evidence indicates that spending 1–2 days at an altitude of 2200 m or higher may help reduce AMS and improve acclimatization and that physical performance is improved after spending 6 days at the higher altitude.19 Thus, acclimatizing to a higher altitude environment is time-consuming and usually requires travel expenses, a special geographical location, and special tools and equipment.
One strategy for acclimatizing to altitude is exposure to a hypoxic environment. Such a strategy allows humans to acclimatize to altitudes, improve physical performance, and reduce altitude illness.20 To assist athletes who may need to perform sports at higher altitudes than that to which they are accustomed, different training modes have been applied to simulate hypoxic environments. Simulated environmental chambers are usually used to acclimatize athletes to altitude.4,21,22 Short-term intermittent hypoxic training (STIHT) is a common mode of exposure to normobaric hypoxia (NH) to simulate altitude acclimatization.22 According to some studies, STIHT can improve physical performance, particularly endurance capacity, in athletes.23 They concluded that due to the limitations in the quality of studies, the positive effects on improving exercisers’ VO2max and HB concentration should be approached with caution and need to be verified by further high-quality research. In a previous study, Bonetti and Hopkins reported that intermittent hypoxic training may enhance the performance of professional or recreational athletes at sea level.15
However, the effects of short-term intermittent hypoxia combined with light-intensity exercise on cardiorespiratory fitness in inactive adults are not clear. Therefore, this study examined the impact of a combination of 14 days of intermittent exposure to NH in a simulated altitude chamber and light physical activity on cardiorespiratory fitness biomarkers in inactive adults.
Materials and Methods
Study Design
This study used a quasi-experimental design, as used in similar previous studies,21,24 to evaluate the effect of short-term intermittent hypoxia combined with light-intensity physical activity on cardiorespiratory fitness in inactive adults, by explicitly measuring the dependent variables including hypoxia (pO2 =15%).
Participants
Ten apparently healthy, inactive male adults (aged 26.3 ± 2.53 years) were recruited randomly from the university students. All participants had lived at about 600 m or less above sea level over the past 6 months. All participants underwent medical examinations by a certified physician from King Saud University prior to starting the experiments. We included apparently healthy, non-smoking, inactive adults without any injury, lung or respiratory health problems, cardiovascular diseases, or any bodily or mental illness. All included participants were deemed inactive as they did not meet the recommended international physical activity guidelines.25 Participants with any of these health conditions, who were active, or who were living at ≥600 m above sea level, were excluded.26
Ethical approval for this study was obtained from the Institutional Review Board of King Saud University. Each participant was informed about the study process and signed a consent form. Each participant was informed that he could withdraw from study participation at any time without giving a formal excuse. All participants were asked not to perform exercise outside the study environment during the course of the experiment, particularly not involving moderate-to-vigorous-intensity physical activity.
An environmental chamber (6 m × 6 m × 3 m) from Weiss Technik (Loughborough, UK) was used throughout the present study. A portable indirect calorimetry system (METAMAX 3B, Cortex Biotechnic GmbH, Regensburg, Germany) was used to evaluate cardiorespiratory fitness markers, including respiratory frequency (RF), oxygen consumption (VO2), minute ventilation (VE), respiratory exchange ratio (RER), and tidal volume (VT), VO2/heart rate (HR), VE/VO2, and VE/carbon dioxide production (VCO2).
Procedures
Participants performed light physical exercise in the environmental chamber during acclimatization for 2 h per day for 14 consecutive days.27 The chamber was maintained at a temperature of 23°C and a relative humidity of 60%. On Day 1, each participant had a chance to familiarize themselves with using the chamber at an oxygen concentration of 15% which equivalent to approximately 2500 meters above sea level. The participants trained at an oxygen concentration of 15% for the next 13 days.
The participants were instructed to perform light exercise for two sessions. Each session last in 40 min with 15 min rest following each 40 min. They were asked to repeat the exercises sequentially. The first exercise included a standing floor-touch, in which the participant bent his trunk to touch the floor with his hands while keeping his knees straight, for 10s, in three sets. The second exercise was a sitting toe-touch, in which the participant sat on the floor with extended legs, and reached out to touch first one foot and then the other with his hands, 10 times. The third exercise was the alternate toe-touch, in which the participant stood with his feet apart, bent at the waist, and reached out to touch his left toe with his right hand, coming up, and then touching his right toe with his left hand. To assess spinal stretching, each participant was instructed to stand on hands and knees with his back first arched, and then to lower his chest toward the ground. For back rotation, each participant was instructed to sit on the floor with his legs extended, while holding a rod over his shoulders with his arms. He then rotated his upper body in counterclockwise and clockwise directions alternately. In general, exercise intensity was controlled using heart rate within ~55-60% of HRmax.
All procedures were performed at a self-paced rate. All variables were measured at rest for 5 min on the day before NH exposure and on days 1, 10, and 14 of the study period.28,29
Statistical Analysis
The Shapiro–Wilk test was performed to evaluate the normality of the data. Repeated-measures analysis of variance was used to assess the effects of the independent variable on the dependent variables. Tukey’s test was used to determine the significance of the effects of independent variables on dependent variables. The dependent variables were compared for both resting and exercise states. All differences with P < 0.05 were considered statistically significant. All statistical analyses were performed using the IBM Statistical Package for Social Sciences program (SPSS version 26, IBM, Armonk, NY USA).
Results
The aim of the present study was to examine the impact of short-term intermittent hypoxia with light-intensity physical activity on cardiorespiratory fitness in inactive adults. All participants were inactive adults as they did not meet the recommended physical activity guidelines.25 Although inactive, resting measurements of their physical characteristics and physiological variables, shown in Table 1, demonstrate that the participants were apparently healthy young adults.
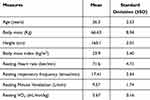 |
Table 1 Physical and Physiological Characteristics of the Participants, at Rest (n=10) |
Resting-state data from the 1st day before starting the experiment (pre-hypoxia) were compared with those of the first day, the 10th day, and the 14th day. The resting HR was significantly higher on the first day of exposure to hypoxia (84.30 ± 6.85 bpm) as compared to pre-hypoxia exposure (71.60 ± 4.71) (P < 0.001). Figure 1 illustrates the significant decrease in resting HR after 10 days (72.86 ± 4.69) and 14 days (71.81 ± 3.88) of exposure to hypoxia, as compared to the first day (all P < 0.001).
Similar results were observed for resting RF and resting VE. In Figure 2, resting RF increased significantly on the first day of exposure to hypoxia (23.24 ± 2.71 time/min) as compared to pre-exposure to hypoxia (17.41 ± 2.54 times/min), but the RF value returned to the pre-hypoxia exposure level on day 10 (18.36 ± 2.65 times/min) and day 14 (17.75 ± 2.82 times/min) (all P < 0.001).
Furthermore, Figure 3 also illustrates that resting VE significantly increased on the first day of exposure to hypoxia (12.17 ± 2.40 L/min) as compared to the day before exposure to hypoxia (9.57 ± 1.74 L/min) and then returned to the pre-hypoxia exposure level on day 10 (9.83 ± 1.31 L/min) and day 14 (9.58 ± 2.38 L/min) (all P < 0.001).
Table 2 illustrates that all physiological variables measured during light exercise were significantly decreased on days 10 and 14 as compared to day 1.
 |
Table 2 Comparison of the Mean of the Physiological Measurements During Light Exercise at Low Oxygen Partial Pressure (pO2 = 15%) on Days 10 and 14 with That of Day 1 (n = 10) |
Discussion
The main aim of the current study was to examine the effects of exposure to NH (low oxygen partial pressure at pO2 = 15%) combined with light physical activity on acclimatization in inactive young adults. Hypoxic acclimatization was defined as the hypoxia tolerance threshold.30 An NH method was used in the hypoxic chamber by decreasing the inspired oxygen content to pO2 = 15% in the chamber atmosphere, while maintaining a regular and constant barometric pressure. We showed that exposure to intermittent NH under these conditions had acclimatizing effects on all measured cardiorespiratory variables during both resting and exercise states over a period of 10 days.
The extent of acclimatization to NH was between 10.70% and 33.49% in the present study. For instance, resting HR decreased significantly by day 10 and day 14, by 13.57% and 14.82%, respectively, relative to day 1 of exposure to NH. Furthermore, HR decreased significantly during light exercise by both days 10 and day 14, by 10.70% and 11.69%, respectively, as compared to day 1 of exposure to NH (P <0.05). NH is a practical and safe method, and is less costly than hypobaric hypoxia (HH) for improving acclimatization of physical fitness components. A recent study found no significant differences in resting (P = 0.397) and exercise (P = 0.790) HR between HH and NH.31 Moreover, a significant reduction in HR recovery (calculated as the difference between the peak HR and the resting HR after a 2-min rest) was seen in both the HH and NH groups across a training program (P < 0.05).32
Some hematological changes occur during exposure to altitude or a simulated environment, such as an NH chamber, including an increase in Hb and a decrease in Hb–O2 affinity.33,34 The initial increased in Hb is due to the reduction in plasma volume. After a couple of weeks, the Hb concentration increases with red blood cell production. The reduced pO2 of inspired air reduces the pO2 of the arterial blood (PaO2). The low level of O2 in the blood is countered by increasing the cardiac output and/or blood–O2 capacitance coefficient, which requires an increase in HR, therefore in cardiac output.35 The current study protocol improved the participants’ resting HR resulting in acclimatization within 10 days. The elevation in Hb and Hct levels begins within a few days (3–4 days) after initial exposure to hypoxia, which may lead to an increase in the PaO2 and O2 content of the blood.36 The increase in HR and cardiac output during the first few days after exposure to hypoxia, combined with increasing RF and VE, meets the demand for O2 in body tissues.18
The present study reported a significant improvement in the RF during rest and light exercise. Resting RF decreased significantly by 21.01% and 23.62%, respectively, by days 10 and 14, as compared to day 1 of exposure to hypoxia. Moreover, RF during light exercise was reduced by 17.39% and 17.44% on days 10 and 14, respectively, as compared to the first day of exposure to hypoxia. Although a few studies have investigated RF acclimatization to hypoxia, some have not found significant changes in RF between normoxia and NH in healthy men.37 However, these studies used short periods (ie, 10 min) of exposure to NH (pO2 = 10%).38 Our study showed that young individuals, even if they have inactive lifestyles, may acclimatize to hypoxia within 10–14 days if light physical activity is performed.
Resting VE in the current study decreased by 19.23% and 21.28% by days 10 and 14, respectively, as compared to day 1 of exposure to NH. Similarly, during light exercise sessions, VE decreased by 29.06% and 30.68%, respectively, by days 10 and 14 as compared to the first day of exposure to NH. In a previous study,39 investigators measured VE during 10 hours of exposure to simulated altitude (normobaric hypoxia and normoxic hypobaria). They found that VE was not significantly different between normobaric hypoxia and normoxic hypobaria. However, after 3 hours, normobaric hypoxia was higher than altitude by 39% and higher than normoxic hypobaria by 41% (P<0.01).
Ventura et al investigated the physiological responses to short-term intermittent exposure to hypoxia at a simulated altitude of 4000 m, which progressively increased to 5500 m over 17 days, in a study that included low-intensity exercise over 7 days to acclimatize to altitude.40 All participants experienced a significant increase in maximal pulmonary ventilation within a few days (P < 0.05). Using a protocol based on exposure to 6000 m for 5 h/day on 3 consecutive days, followed by exposure to 8000 m for 1 h/day in trained adults, they found increased ventilation and PaO2, and decreased PaCO2, without significant changes in red blood cell counts.41 On the other hand, our study demonstrated that exposure to NH (pO2 = 15%) for only 2 h/day for 10 days may help acclimatization to altitude by improving physiological parameters, such as pulmonary capacity and VE.
The results of the current study showed a significant increase in VO2 during light exercise, with an improvement by 28.21% and 30.65% on days 10 and day 14, respectively (both P < 0.01), as compared to the first day of exposure to hypoxia. No significant differences between the reported VO2 on days 10 and 14 were found compared with the same workload in normal ambient air (normoxia) (P = 0.29). Furthermore, oxygen pulse (VO2/HR) also improved by 23.13% and 22.80% on days 10 and day 14, respectively (both P < 0.01), as compared to the first day of exposure to hypoxia. Eroglu and Aydin examined the impact of intermittent hypoxic interventions on the aerobic and anaerobic performance of elite athletes. They concluded that no significant changes in performance occurred, including VO2, in the hypoxic group. The differences in the study findings may be due to the methods used, as the hypoxia group in their study was exposed to hypoxia for 4 weeks, 3 days/week. Each session lasted 60 min/day; thus, participants were exposed to normal ambient air (normoxia) for 5 min, followed by 5 min of hypoxia (pO2 = 15%).42 Furthermore, differences in the study findings may be partly related to the participants’ fitness levels, as all of the participants in the previous study were elite athletes. In the present study, hematological blood parameters, such as Hb or Hct, were not measured. However, the reported improvement in VO2 and VO2/HR in the present study could be attributed to the significant increase in Hb concentration as well as the improvement in the stroke volume induced by enhanced contractility during light exercise.40
Although the findings of the present study were consistent with those of previous studies, which reported that hypoxic exposure significantly improved some physiological parameters,7,21,22,43 cautions should be taken as some similar findings may refer to different factors. Moreover, the present study was not randomized control trial (RCT). Thus, more studies are recommended using RCT protocol to enhance more precise findings.
Study Limitations
The current study was a quasi-experimental study, and did not use a control group to compare their data with the experimental group. In addition, the sample size was small, as the nature of the study protocol, which included exposure to hypoxia, made it difficult to recruit participants. The current study did not measure some important physiological parameters, including hematological and cardiovascular variables, which may help to explain some of the reported results. The study is not placebo controlled. There were no measurements done during exercise in normoxia.
Conclusion
In conclusion, whereas research on acclimatization during rest and light exercise has not been well studied, this study revealed that combining light exercise with intermittent exposure to NH (pO2 = 15%) for as little as 2 h per day for 10 days may improve some important cardiovascular capacities in inactive adults. The protocol used in this study may help to improve acclimatization in adults when they visit high altitudes (approximately 2500 m above sea level). This may help untrained adults or tourists who would like to visit such places to use this protocol. Further research is required to examine the impact of similar protocols on different populations.
Data Sharing Statement
The data presented in the current study have not been deposited into public repositories but may be available upon request from the corresponding author.
Ethics Approval and Consent to Participate
Ethical approval has been obtained from the Institutional Review Board at King Saud University (E-19-3752). The present study complies with the Declaration of Helsinki.
Acknowledgment
The author would like to extend their gratitude to the Researchers Supporting Project number (RSP2024R263), King Saud University, Riyadh, Saudi Arabia.
Funding
This research received no external funding.
Disclosure
The author declares no conflict of interest.
References
1. Saunders PU, Pyne DB, Gore CJ. Endurance training at altitude. High Alt Med Biol. 2009;10(2):135–148. doi:10.1089/ham.2008.1092
2. West JB. High-altitude medicine. Am J Respir Crit Care Med. 2012;186(12):1229–1237. doi:10.1164/rccm.201207-1323CI
3. Burtscher M, Millet GP, Burtscher J. Hypoxia conditioning for high-altitude pre-acclimatization. J Sci Sport Exercise. 2022;2022:1–15.
4. Bhaumik G, Dass D, Lama H, Chauhan S. Maximum exercise responses of men and women mountaineering trainees on induction to high altitude (4350 m) by trekking. Wilderness Env Med. 2008;19(3):151–156. doi:10.1580/07-WEME-OR-121.1
5. Brutsaert TD. Do high-altitude natives have enhanced exercise performance at altitude? Appl Physiol Nutr Metab. 2008;33(3):582–592. doi:10.1139/H08-009
6. Mazzeo RS, Bender PR, Brooks GA, et al. Arterial catecholamine responses during exercise with acute and chronic high-altitude exposure. Am J Physiol Endocrinol Metab. 1991;261(4):E419–E424. doi:10.1152/ajpendo.1991.261.4.E419
7. Álvarez-Herms J, Julià-Sánchez S, Gatterer H, et al. Anaerobic training in hypoxia: a new approach to stimulate the rating of effort perception. Physiol Behav. 2016;163:37–42. doi:10.1016/j.physbeh.2016.04.035
8. Ranković G, Mutavdžić V, Toskić D, et al. Aerobic capacity as an indicator in different kinds of sports. Bosnian J Basic Med Sci. 2010;10(1):44. doi:10.17305/bjbms.2010.2734
9. Abut F, Akay MF, George J. Developing new VO2max prediction models from maximal, submaximal and questionnaire variables using support vector machines combined with feature selection. Comput Biol Med. 2016;79:182–192. doi:10.1016/j.compbiomed.2016.10.018
10. Warburton DE, Gledhill N, Quinney HA. Blood volume, aerobic power, and endurance performance: potential ergogenic effect of volume loading. Clin J Sport Med. 2000;10(1):59–66. doi:10.1097/00042752-200001000-00011
11. Stembridge M, Williams AM, Gasho C, et al. The overlooked significance of plasma volume for successful adaptation to high altitude in Sherpa and Andean natives. Proc Nat Acad Sci. 2019;116(33):16177–16179.
12. Beall CM, Brittenham GM, Strohl KP, et al. Hemoglobin concentration of high‐altitude Tibetans and Bolivian Aymara. Am J Phys Anthropol. 1998;106(3):385–400. doi:10.1002/(SICI)1096-8644(199807)106:3<385::AID-AJPA10>3.0.CO;2-X
13. Imray C, Booth A, Wright A, Bradwell A. Acute altitude illnesses. BMJ. 2011;2011:343.
14. Powell FL, Garcia N. Physiological effects of intermittent hypoxia. High Alt Med Biol. 2000;1(2):125–136. doi:10.1089/15270290050074279
15. Bonetti DL, Hopkins WG, Kilding AE. High-intensity kayak performance after adaptation to intermittent hypoxia. Int J Sports Physiol Perform. 2006;1(3):246–260. doi:10.1123/ijspp.1.3.246
16. Butler GJ, Al-Waili N, Passano D, et al. Altitude mountain sickness among tourist populations: a review and pathophysiology supporting management with hyperbaric oxygen. J Med Eng Technol. 2011;35(3–4):197–207. doi:10.3109/03091902.2010.497890
17. Luks AM, Beidleman BA, Freer L, et al. Wilderness medical society clinical practice guidelines for the prevention, diagnosis, and treatment of acute altitude illness: 2024 update. Wilderness Env Med. 2024;35(1_suppl):2S–19S. doi:10.1016/j.wem.2023.05.013
18. Gonggalanzi L, Nafstad P, Nafstad P, et al. Acute mountain sickness among tourists visiting the high-altitude city of Lhasa at 3658 m above sea level: a cross-sectional study. Arch Public Health. 2016;74:1–7. doi:10.1186/s13690-016-0134-z
19. Muza SR, Beidleman BA, Fulco CS. Altitude preexposure recommendations for inducing acclimatization. High Alt Med Biol. 2010;11(2):87–92. doi:10.1089/ham.2010.1006
20. Majumdar D. Performance enhancement through physical activity at high altitudes. In: Management of High Altitude Pathophysiology. Elsevier; 2018:279–306.
21. Ambroży T, Maciejczyk M, Klimek AT, et al. The effects of intermittent hypoxic training on anaerobic and aerobic power in boxers. Int J Environ Res Public Health. 2020;17(24):9361. doi:10.3390/ijerph17249361
22. Huang Z, Yang S, Li C, Xie X, Wang Y. The effects of intermittent hypoxic training on the aerobic capacity of exercisers: a systemic review and meta-analysis. BMC Sports Sci Med Rehab. 2023;15(1):174. doi:10.1186/s13102-023-00784-3
23. Levine BD. Intermittent hypoxic training: fact and fancy. High Alt Med Biol. 2002;3(2):177–193. doi:10.1089/15270290260131911
24. Hendriksen IJ, Meeuwsen T. The effect of intermittent training in hypobaric hypoxia on sea-level exercise: a cross-over study in humans. Eur J Appl Physiol. 2003;88(4):396–403. doi:10.1007/s00421-002-0708-z
25. Ross R, Chaput J-P, Giangregorio LM, et al. Canadian 24-hour movement guidelines for adults aged 18–64 years and adults aged 65 years or older: an integration of physical activity, sedentary behaviour, and sleep. Appl Physiol Nutr Metab. 2020;45(10):S57–S102. doi:10.1139/apnm-2020-0467
26. Apte CV, Rao KS. The maximum expiratory flow-volume loop in natives of Ladakh and acclimatized lowlanders. High Alt Med Biol. 2005;6(3):209–214. doi:10.1089/ham.2005.6.209
27. Ricart A, Casas H, Casas M, et al. Acclimatization near home? Early respiratory changes after short-term intermittent exposure to simulated altitude. Wilderness Env Med. 2000;11(2):84–88. doi:10.1580/1080-6032(2000)011[0084:ANHERC]2.3.CO;2
28. Ramadan MZ. Effects of Task and Environment-Related Variables on Individuals’ Lifting Capabilities While Wearing Protective Clothing. West Virginia University; 1988.
29. Khalaf TM, Ramadan MZ, Al-Ashaikh RA. How many days are required for workers to acclimatize to heat? Work. 2017;56(2):285–289. doi:10.3233/WOR-162485
30. Remen M, Oppedal F, Imsland AK, Olsen RE, Torgersen T. Hypoxia tolerance thresholds for post-smolt Atlantic salmon: dependency of temperature and hypoxia acclimation. Aquaculture. 2013;416:41–47. doi:10.1016/j.aquaculture.2013.08.024
31. Rosales AM, Shute RJ, Hailes WS, Collins CW, Ruby BC, Slivka DR. Independent effects of acute normobaric hypoxia and hypobaric hypoxia on human physiology. Sci Rep. 2022;12(1):19570. doi:10.1038/s41598-022-23698-5
32. Rodríguez-Zamora L, Benavente C, Petrer I, et al. Hypoxia matters: comparison of external and internal training load markers during an 8-week resistance training program in normoxia, normobaric hypoxia and hypobaric hypoxia. Eur J Appl Physiol. 2024;2024:1–11.
33. Ivy CM, Scott GR. Control of breathing and the circulation in high-altitude mammals and birds. Comp Biochem Physiol A. 2015;186:66–74. doi:10.1016/j.cbpa.2014.10.009
34. Storz JF, Scott GR. Life ascending: mechanism and process in physiological adaptation to high-altitude hypoxia. Annu Rev Ecol Evol Syst. 2019;50(1):503–526. doi:10.1146/annurev-ecolsys-110218-025014
35. Storz JF, Bautista NM. Altitude acclimatization, hemoglobin-oxygen affinity, and circulatory oxygen transport in hypoxia. Mol Aspect Med. 2022;84:101052. doi:10.1016/j.mam.2021.101052
36. Hahn AG, Gore CJ. The effect of altitude on cycling performance. Sports Med. 2001;31(7):533–557. doi:10.2165/00007256-200131070-00008
37. Neuls F, Krejci J, Jakubec A, Botek M, Valenta M. Vagal threshold determination during incremental stepwise exercise in normoxia and normobaric hypoxia. Int J Environ Res Public Health. 2020;17(20):7579. doi:10.3390/ijerph17207579
38. Melnikov V, Divert V, Komlyagina T, Consedine N, Krivoschekov S. Baseline values of cardiovascular and respiratory parameters predict response to acute hypoxia in young healthy men. Physiol Res. 2017;66(3):467–479. doi:10.33549/physiolres.933328
39. Loeppky J, Icenogle M, Scotto P, Robergs R, Hinghofer-Szalkay H, Roach R. Ventilation during simulated altitude, normobaric hypoxia and normoxic hypobaria. Respiration Physiol. 1997;107(3):231–239. doi:10.1016/S0034-5687(97)02523-1
40. Ventura M, Jordi I, Ferran A. Intermittent hypobaric hypoxia induces altitude acclimation and improves the lactate threshold. Aviat Space Environ Med. 2000;71(2):125–130.
41. Nagasaka T, Satake T Changes of pulmonary and cardiovascular functions in subjects confined intermittently in a low-pressure chamber for 3 consecutive days.
42. Eroğlu A, Aydın T. Effect of intermittent hypoxic intervention on aerobic and anaerobic performance of the elite athletes. Med Sc Disc. 2021;8(8):460–464. doi:10.36472/msd.v8i8.580
43. Gao YX, Li P, Jiang CH, et al. Psychological and cognitive impairment of long‐term migrators to high altitudes and the relationship to physiological and biochemical changes. Eur J Neurol. 2015;22(10):1363–1369. doi:10.1111/ene.12507
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




