Back to Journals » Cancer Management and Research » Volume 17
Successful Diagnosis and Management of Superior Orbital Fissure Syndrome Secondary to Lung Adenocarcinoma: A Case Report
Received 1 October 2024
Accepted for publication 9 January 2025
Published 15 January 2025 Volume 2025:17 Pages 57—63
DOI https://doi.org/10.2147/CMAR.S495207
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Bilikere Dwarakanath
Yufang Wang, Xiangrong Zhao
Department of Radiotherapy, Liaocheng Hospital Affiliated to Shandong First Medical University (Liaocheng People’s Hospital), Liaocheng, Shandong, People’s Republic of China
Correspondence: Xiangrong Zhao, Email [email protected]
Introduction: Superior orbital fissure syndrome (SOFS) is a rare condition that involves damage to multiple structures within the superior orbital fissure, often caused by trauma, inflammation, or tumors. Lung adenocarcinoma, known for its propensity to metastasize, can lead to orbital metastases, which can manifest as SOFS. This case underscores the diagnostic and therapeutic challenges associated with such rare metastatic presentations.
Case Presentation: A 60-year-old woman with a history of left lung adenocarcinoma presented with left eyelid ptosis and fixed eye position following hair dyeing. Despite initial treatments and imaging, her condition persisted. Subsequent imaging and thorough clinical evaluation revealed metastasis to the left superior orbital fissure. The patient was treated with volumetric modulated arc therapy (VMAT), leading to significant clinical improvement and reduction of the orbital mass.
Conclusion: This case highlights the critical role of comprehensive diagnostic evaluation and communication between specialists in managing rare metastatic conditions. It also demonstrates the efficacy of localized radiotherapy in treating such uncommon presentations of lung cancer metastasis.
Keywords: superior orbital fissure syndrome, lung adenocarcinoma, metastasis, radiotherapy, case report
Introduction
Superior orbital fissure syndrome (SOFS) is an uncommon neurological condition characterized by damage to the cranial nerves and vascular structures passing through the superior orbital fissure. This syndrome often results from trauma, inflammation, or neoplastic processes.1–3 Lung adenocarcinoma, a type of non-small cell lung cancer, is known for its potential to metastasize to various distant sites, most commonly to the brain and bones. However, metastasis specifically involving the superior orbital fissure is exceedingly rare.4 Traditionally, diagnosis of SOFS involves a combination of clinical evaluation and imaging studies. Given the complex anatomy of the superior orbital fissure and the rarity of metastasis to this area, misdiagnosis or delayed diagnosis is not uncommon. Effective management requires not only accurate diagnosis but also a tailored therapeutic approach. Recent advances in radiotherapy, such as volumetric modulated arc therapy (VMAT), offer promising options for localized treatment.
This case report presents a unique instance of lung adenocarcinoma metastasizing to the superior orbital fissure, leading to SOFS. The patient’s history, diagnostic journey, and response to targeted radiotherapy provide valuable insights into managing rare metastatic presentations and highlight the importance of interdisciplinary collaboration in optimizing patient outcomes.
Case Report
The patient is a 60-year-old woman diagnosed with left lung adenocarcinoma two years prior in Liaocheng people’s hospital. On February 16, 2024, she presented to our hospital for follow-up and was noted to have left eyelid ptosis. She reported that about two weeks earlier, following hair dyeing, she experienced drooping of the left eyelid. She had been treated with oral antihistamines (specific medication unknown) at a local clinic without notable improvement. Subsequently, she sought care at our ophthalmology clinic where she was initially diagnosed with “left ocular muscle paralysis” and was treated with mecobalamin 0.5 mg three times daily, citicoline 0.2 g three times daily, and vitamin B1 10 mg three times daily, but her symptoms persisted. The patient initially attributed her symptoms to an allergic reaction to the dye. Allergic reactions typically present with bilateral itching, photophobia, or increased discharge. However, upon further questioning, the patient reported only mild swelling of both eyelids and drooping of the left eyelid, without other allergic symptoms. Given her history of lung cancer and the nature of her symptoms, we suspected that the symptoms were caused by metastasis compressing the oculomotor and abducent nerves, rather than an allergic reaction.
“A further review of the medical history reveals that on December 20, 2021, the patient was diagnosed with left upper lobe adenocarcinoma, stage IV, with bone metastasis.” Pathological immunohistochemical results were as follows: TTF1(+), NapsinA(+), P53(+), Ki-67(40%+), Syn(-), CK7(+), CEA(+), P40(-), CyclinD1(-), P63(weak+). PD-L1 (22C3) testing revealed a tumor proportion score (TPS) of approximately 80% positive. Genetic testing identified an EGFR exon 19 deletion mutation. The patient’s initial treatment included osimertinib, which resulted in a partial response (PR). The progression-free survival (PFS) with osimertinib was approximately 8 months. However, in August 2022, follow-up imaging revealed progression of the pulmonary lesions, and osimertinib was discontinued. The patient then received four cycles of pemetrexed combined with cisplatin chemotherapy, which resulted in stable disease. The PFS with chemotherapy was approximately 6 months. In January 2023, new metastatic lesions were found in the thoracic and lumbar spine. The patient was treated with local radiation therapy (40Gy in 20 fractions over 4 weeks), which led to a partial response (PR). In June 2023, progression of the pulmonary lesions was noted, and a treatment adjustment was made to anlotinib combined with toripalimab. The patient’s condition remained stable until she missed subsequent follow-ups and treatments.
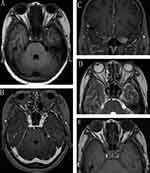
Upon admission, physical examination showed an Eastern Cooperative Oncology Group Performance Status (ECOG) score of 2, blood pressure of 130/70 mmHg, clear consciousness, fluent speech. Left eyelid ptosis required manual lifting for ophthalmic examination. The pupil diameter was approximately 5 mm, with the left eye fixed in position and absent light reflex. Ophthalmic examination is illustrated in Figures 1. On February 20, 2024, cranial Nuclear Magnetic Resonance Imaging (MRI) revealed: 1) Abnormal signal in the right occipital region, suggestive of metastatic tumor based on history. 2) Multiple small ischemic lesions in the brain. 3) Sinusitis. The initial imaging by the radiologist did not suggest any abnormalities in the orbital region. However, the patient’s persistent left eyelid ptosis prompted us to review the MRI more carefully, particularly focusing on the orbital area. During this process, we identified a small abnormal signal in the left superior orbital fissure (Figures 2A-D). This finding was surprising, as it correlated with the patient’s symptoms. After communicating with the radiology team, we decided to proceed with a more targeted orbital MRI. Repeated imaging provided clearer visualization of the lesion (Figure 2E), showing abnormal signals in the left orbital apex and the anterior edge of the left cavernous sinus, consistent with metastasis. Additionally, the left optic nerve and extraocular muscles appeared thinner compared to the right. Although we strongly suspected orbital metastasis, we recognized that ophthalmology expertise was crucial to confirming the diagnosis. Given the specialized nature of the eye, we could not be certain that the lesion was metastatic, so we consulted with ophthalmology specialists. After further discussions, we ruled out inflammatory or vascular diseases as potential causes. This collaborative effort led to the final diagnosis of left superior orbital fissure metastasis from lung adenocarcinoma, presenting as superior orbital fissure syndrome (SOFS). A contrast-enhanced chest and abdomen Computed Tomography (CT) scan conducted on February 17, 2024, demonstrated progression of the left lung tumor with associated atelectasis, enlargement of mediastinal and hilar lymph nodes, and newly developed metastatic tumors in the left adrenal gland, liver, and multiple bones.
 |
Figure 1 Photos of ophthalmologic examination before treatment (A) Left eyelid ptosis (B) Left eyeball fixed in position, with limited movement in all directions. |
The patient’s overall condition was stable, with no significant symptoms from bone or liver metastases; however, the left eyelid ptosis severely impacted her vision. After thorough discussion with the patient and her family, and obtaining consent, localized radiation therapy was planned for the left superior orbital fissure metastasis to alleviate symptoms (and to also address the right occipital metastasis).
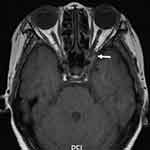
The radiotherapy was performed using Volumetric Modulated Arc Therapy (VMAT). The target areas included Gross Tumor Volume 1 (GTV1) (right occipital metastasis) and GTV2 (left superior orbital fissure metastasis). CT simulation images were fused with MRI to delineate the GTV target areas. GTV1 and GTV2 were expanded by 3 mm to create PGTV1 and PGTV2, with no expansion at the optic nerve (Figure 3). The radiation dose delivered was 45 Gy in 10 fractions over 2 weeks ensuring 95% coverage of PGTV1 and PGTV2. During the planning, critical structures, such as the left and right lenses, optic chiasm, pituitary gland, and brainstem, were contoured for protection. The dose distribution was well-conformed, and the maximum dose for the left lens was 560 cGy, for the right lens was 577 cGy, for the brainstem was 3483 cGy, for the optic chiasm was 3963 cGy, and for the pituitary gland was 3783 cGy. All doses to the critical structures were within their tolerance limits, and the treatment plan was approved. The patient completed treatment without significant side effects.
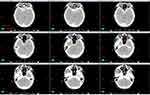 |
Figure 3 Target delineation diagram GTV2 as the mass in the superior orbital fissure, with a 3mm expansion to PGTV (excluding the optic nerve). |
After radiation therapy, the left eyelid ptosis was alleviated, and her visual field and eye movement improved significantly (Figure 4). The patient is very satisfied with the effect of the treatment. Follow-up MRI on April 16, 2024, demonstrated significant reduction in the metastasis (Figure 5). Radiotherapy was used to shrink the tumor and relieve compression on the oculomotor and abducent nerves, leading to significant improvement in eyelid ptosis. This demonstrates the effectiveness of localized radiation in treating nerve compression caused by metastasis in complex regions like the superior orbital fissure.
Discussion
This case underscores the critical importance of logical reasoning in differential diagnosis, especially when faced with atypical or misleading symptoms. The patient’s initial presentation, which coincided with a hair dyeing event, suggested an allergic reaction. However, through detailed history-taking and careful analysis of her symptoms—specifically the lack of typical allergic signs like itching, photophobia, or increased discharge—we were able to rule out an allergic etiology. This directed our focus towards a more serious underlying cause, ultimately leading to the suspicion of metastatic disease.
The diagnostic process was not straightforward. The initial cranial MRI on February 20, 2024, failed to detect a distinct lesion in the superior orbital fissure, which did not align with our clinical suspicion. Recognizing this discrepancy, we engaged in active communication with the radiology department, requesting a repeat MRI focused on the orbital region. This persistence led to the identification of a metastatic lesion in the left superior orbital fissure. This case highlights the necessity of integrating clinical assessment with imaging results and underscores the importance of thorough, interdisciplinary communication in complex cases.
In reviewing the literature, SOFS secondary to metastasis, particularly from lung adenocarcinoma, is exceedingly rare. Rarely documented cases of orbital metastases from lung cancer have typically involved more extensive areas of the orbit, such as orbital apex syndrome, with virtually no reports specifically describing metastasis to the superior orbital fissure.5,6 The complex anatomy of the superior orbital fissure, densely packed with nerves and blood vessels, makes it a challenging site for both diagnosis and treatment. This case is unique in that it illustrates the successful application of VMAT in treating a metastatic lesion in this area, resulting in significant symptomatic relief and partial remission, as confirmed by follow-up imaging.
Moreover, this case emphasizes the importance of consulting the latest literature and recognizing rare clinical presentations to ensure that even the most unusual cases are managed effectively. Our approach, which combined logical diagnostic reasoning, careful patient history analysis, effective interdisciplinary communication, and the use of advanced radiotherapy techniques, led to a favorable outcome. This underscores the value of a structured and methodical approach in clinical practice, particularly in cases involving rare and complex conditions.
In conclusion, this case contributes to the existing literature by documenting a rare instance of SOFS caused by lung adenocarcinoma metastasis. It highlights the need for vigilance in diagnosis, the importance of considering a broad differential diagnosis, and the efficacy of VMAT in treating metastatic lesions in challenging anatomical regions. These insights are valuable for clinicians managing similar cases and underscore the importance of comprehensive, patient-centered care in achieving optimal outcomes.
Data Sharing Statement
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the author.
Statement of Ethics
Ethical approval is not required to publish the case details in accordance with local or national guidelines.
Acknowledgments
We would like to thank Shuhua Li for providing and interpreting the imaging data, and Hongying Wang for her contributions in dose calculation and radiotherapy planning.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Consent for Publication
Written informed consent has been obtained from the patient for publication of this paper and accompanying images.
Funding
There is no funding to report.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
1. Rohrich RJ, Hackney FL, Parikh RS. Superior orbital fissure syndrome: current management concepts. J Craniomaxillofac Trauma. 1995;1(2):44–48. PMID: 11951462
2. Fujiwara T, Matsuda K, Kubo T, et al. Superior orbital fissure syndrome after repair of maxillary and naso-orbito-ethmoid fractures: a case study. J Plast Reconstr Aesthet Surg. 2009;62(12):e565–e569. doi:10.1016/j.bjps.2008.11.052
3. Reymond J, Kwiatkowski J, Wysocki J. Clinical anatomy of the superior orbital fissure and the orbital apex. J Craniomaxillofac Surg. 2008;36(6):346–353. doi:10.1016/j.jcms.2008.02.004
4. Riely GJ, Wood DE, Ettinger DS, et al. Non-small cell lung cancer, version 4.2024, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2024;22(4):249–274. doi:10.6004/jnccn.2204.0023
5. Linxi H, Jie W, Mingxing Z, et al. One case of orbital apex syndrome caused by metastasis of lung cancer. Chin J Neuromedicine. 2019;18(2):3.
6. Xu L, Yu M, Chen X, et al. One case of orbital apex syndrome caused by small cell lung cancer metastasis. Rev Neurol. 2021;177(8):1032–1035. doi:10.1016/j.neurol.2020.11.010
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Evaluation of the Clinical Efficacy of Intensity-Modulated Radiotherapy Combined with Transcatheter Arterial Chemoembolization for Hepatocellular Carcinoma with Extrahepatic Oligometastasis and Prognostic Factors for Patient Survival
Luo Y, Huang X, Chen J, Zhang S
International Journal of General Medicine 2023, 16:1271-1278
Published Date: 12 April 2023