Back to Journals » Nature and Science of Sleep » Volume 16
Survival and Risk Factors Associated with Mortality in Patients with Sleep Apnoea in Colombia: A Retrospective Cohort Study
Authors Tuta-Quintero E, Bastidas AR, Faizal-Gómez K , Torres-Riveros SG , Rodríguez-Barajas DA , Guezguan JA , Muñoz LD , Rojas AC, Hernández Calderón K , Ardila Velasco NV, Prieto P, Cuestas J, Camacho-Osorio J, Bonilla G, Collazos Bahamon E, Guardiola MA, Luna Salazar D , Fajardo LP, Rincón-Hernández J
Received 2 June 2024
Accepted for publication 9 August 2024
Published 9 October 2024 Volume 2024:16 Pages 1601—1610
DOI https://doi.org/10.2147/NSS.S481010
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Eduardo Tuta-Quintero,1 Alirio R Bastidas,1 Kamil Faizal-Gómez,1 Sergio Guillermo Torres-Riveros,2 Diego Alejandro Rodríguez-Barajas,2 Jonathan Alexander Guezguan,1 Laura D Muñoz,1 Ana Carolina Rojas,1 Katherine Hernández Calderón,1 Natalia Valentina Ardila Velasco,1 Paula Prieto,1 Juliana Cuestas,1 Julian Camacho-Osorio,1 Gabriela Bonilla,1 Estefania Collazos Bahamon,1 María Alejandra Guardiola,1 David Luna Salazar,1 Lina Paola Fajardo,1 Johan Rincón-Hernández1
1Facultad de Medicina, Universidad de La Sabana, Chía, Colombia; 2Residente de Medicina Interna, Facultad de Medicina, Universidad de La Sabana, Chía, Colombia
Correspondence: Alirio R Bastidas, School of Medicine, Universidad de La Sabana, Km 7, Autonorte de Bogota, Chía, Cundinamarca, 250001, Colombia, Email [email protected]
Background: Survival in patients with sleep apnoea (SA) can be reduced by variables such as age, sex, and comorbidities. However, survival data in patients with SA in Colombia remains scarce.
Methods: This is a retrospective cohort study of patients diagnosed with SA between 2005 and 2022. Five-year survival was assessed using the Kaplan-Meier method, and survival curves were stratified by age, sex, and cardiovascular disease. Risk factors associated with survival were evaluated using Hazard Ratio (HR) by adjusting for confounding variables with a Cox regression model. A minimum sample size of 1537 patients were estimated to be necessary to estimate a survival incidence rate with a 5% precision.
Results: The five-year survival rate in the general population was 94.6%, with lower survival in patients over 65 years (88.5% vs 97.9%; p < 0.001) and in patients with cardiovascular disease (89% vs 95.2%; p < 0.001) compared to the control group. In the Cox regression, age showed an HR of 1.05 (95% CI: 1.02– 1.07; p < 0.001). Male sex had an HR of 2.31 (95% CI: 1.25– 4.25; p = 0.007), congestive heart failure an HR of 4.00 (95% CI: 2.31– 6.94; p < 0.001), chronic obstructive pulmonary disease (COPD) an HR of 1.75 (95% CI: 1.04– 2.96; p = 0.035), chronic kidney disease (CKD) an HR of 2.23 (95% CI: 1.31– 3.78; p = 0.003), and metastatic cancer an HR of 4.96 (95% CI: 1.95– 12.60; p = 0.001).
Conclusion: The study showed a high five-year survival rate in patients with SA. The risk factors associated with decreased overall five-year survival were age, male sex, cardiovascular disease, COPD, CKD, and metastatic cancer.
Keywords: sleep apnoea, survival, risk factors
Introduction
Sleep apnoea (SA) is a chronic condition characterized by recurrent episodes of upper airway obstruction during sleep, leading to transient breathing interruptions and intermittent hypoxemia.1,2 This condition is significantly associated with reduced survival and an increased incidence of cardiovascular disease such as acute myocardial infarction, stroke, and cardiac arrhythmias.1,3 Worldwide epidemiological studies have documented a relationship between SA and increased mortality, highlighting the need for research to describe survival rates and identify factors influencing survival in this population.1–5
It is estimated that around one billion adults aged 30 to 69 worldwide suffer from SA, with a prevalence exceeding 50% in some countries.6–10 In South America, Tufik et al11 conducted 1042 polysomnographies in a population from São Paulo, finding a prevalence of 32.8% (95% CI, 29.6–36.3%) for SA. The variables associated with this prevalence were being male (OR = 4.1; 95% CI, 2.9–5.8; P < 0.001) and obesity (OR = 10.5; 95% CI, 7.1–15.7; P < 0.001).11 Young et al4 in a cohort of 1522 patients with an 18-year follow-up, identified a significant association between SA severity and mortality (HR 2.65; 95% CI, 1.82 to 3.85; p < 0.001). Similar data were described by “The Busselton Health Study”, a longitudinal study with an average follow-up of 13.4 years that included 380 patients.5 This study identified moderate to severe SA as an independent factor for a higher risk of all-cause mortality (HR = 6.24; 95% CI, 2.01 to 19.39) compared to those without SA (HR = 0.47; 95% CI, 0.17 to 1.29) (p < 0.008).
Pre-existing cardiovascular disease increases mortality in patients with SA.6,7 The study “Influence of Obstructive Sleep Apnea on Mortality in Patients With Heart Failure”, which followed 164 patients with a left ventricular ejection fraction <45% for up to 7.3 years, found a significant association between the presence of SA and a higher risk of mortality in patients with heart failure.6 Ge et al2 concluded that the presence of acute myocardial infarction (AMI) and a decreased LVEF increased mortality by 1.90 times (95% CI, 1.82–3.85) in patients with SA. These findings suggest that the severity of SA may be an important risk factor for cardiovascular mortality.6,7 Additionally, other conditions such as chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), collagen diseases, and type 2 diabetes have also been associated with increased mortality in these patients.8,9
SA is characterized by episodes of intermittent hypoxemia and sleep fragmentation, both factors associated with increased mortality through various pathophysiological mechanisms.12–14 Oxygen desaturation during apneas or hypopneas triggers nocturnal activation of the sympathetic nervous system and initiates an inflammatory cascade, including cellular oxidative stress.14,15 These mechanisms contribute to the accelerated development of cardiovascular diseases and the mortality associated with SA.15 Currently, it has been described that survival in patients with SA is influenced by variables such as age, sex, and comorbidities.6,8,9 However, data on survival in patients with SA, particularly in Latin American countries, remain scarce, necessitating the description of variables associated with outcomes in this population. The main objective of this study is to determine the factors associated with mortality and five-year survival in patients diagnosed with SA in Colombia.
Methods
A retrospective cohort study was conducted on subjects treated at the Clínica Universidad de La Sabana in Chía, Colombia, from 2005 to 2022. The main objective of the study was to evaluate the survival of patients diagnosed with SA and describe the factors associated with mortality.
Eligibility Criteria
Patients aged 18 years or older with a diagnosis of obstructive sleep apnea (OSA), defined by an apnoea-hypopnea index (AHI) greater than 5 events per hour of sleep, as confirmed by polysomnography (PSG) following American Academy of Sleep Medicine (AASM) criteria, were included.16 Eligible patients presented with symptoms such as chronic snoring, excessive daytime sleepiness, persistent fatigue, and sleep disturbances.16 Exclusion criteria included other sleep disorders or medical conditions with similar symptoms, as well as patients lacking follow-up survival data, and incomplete AHI information.
Variables and Data Collection
Variables analyzed included age, sex, race, marital status, anthropometric measures, and medical history of diseases such as congestive heart failure (CHF), atrial fibrillation (AF), cerebrovascular disease (CVE), CKD, COPD, AMI, and cancer. PSG variables analyzed included AHI, type of apnea, and the presence of restless legs syndrome. Regarding oxygen therapy prescription, the time from initiation, hours prescribed, hours used per day, and flow in liters were considered. Additionally, speech therapy indications and positive airway pressure system variables, such as Bi-Level Positive Airway Pressure (BPAP), Continuous Positive Airway Pressure (CPAP), and Automatic Continuous Positive Airway Pressure (AUTOCPAP) were considered. The outcome variable was survival, evaluated at 5 years.
Data evaluation and collection were performed using a database directly obtained from electronic medical records and diagnostic test results. To identify the follow-up status of patients, the general health system resource administrator (ADRES) was consulted to report the survival status. Precise eligibility criteria were established to mitigate selection bias. To reduce transcription bias, at least two team members reviewed the information, and in case of inconsistency, a third team member reviewed the information and made the final decision. Additionally, all variables were clearly defined, and the researchers responsible for data collection were previously trained.
Statistical Analysis
Data were transcribed into the Research Electronic Data Capture (REDCap) software version.17 Quantitative variables were summarized using measures of central tendency and dispersion, with means and standard deviations (SD) for normally distributed data, and medians and interquartile ranges (IQR) for non-normally distributed data. The Shapiro–Wilk test was used to assess normality. Qualitative variables were described as absolute and relative frequencies. Univariate analysis between study variables and the presence or absence of SA was performed using the chi-square test for qualitative variables and the Student’s t-test or Mann–Whitney U-test depending on the distribution of quantitative variables.
Five-year survival was assessed using survival tables, and the results were plotted using the Kaplan-Meier method.18 Survival curves were stratified by age, sex, and cardiovascular disease (AMI, CHF, AF, and CVE). Time to death was used as the dependent variable in the Cox regression model with variables selected for inclusion through bivariate analysis using a significance threshold of p < 0.2 and their biological plausibility in relation to the event in question. We built the covariate-adjusted model and created a series of directed acyclic graphs (DAGs) through an iterative process. Subsequently, we evaluated each covariate considered relevant for our analysis based on its association with the outcome using univariable Cox regressions with a significance level of α = 0.50. These covariates were considered for the multivariable model.18 Once the full model was fitted to the data, we used a stepwise backward regression method for variable selection. We started with a saturated model that included all possible variables and, at each step, removed the least significant variable until all remaining variables were significant according to adjustment criteria, such as the p-value, and based on clinical considerations.18 Regression coefficients and corresponding p-values were calculated for each independent variable.18 Hazard ratios (HR) for each variable were determined, with a significance level of p < 0.05 considered statistically relevant.
To determine the required sample size, we applied the Schoenfeld formula for survival analysis with an alpha level of 0.05 and 90% power.18,19 Based on this calculation, a minimum sample size of 1537 patients was estimated to achieve a 5% precision in estimating the survival incidence rate. This estimate considers the prevalence of significant comorbidities within our study setting.19 Data were analyzed using IBM SPSS software (version 26, IBM Corp., Chicago, IL, USA), which was licensed to the researchers’ university.
Results
General Characteristics of the Population
A total of 2,027 patients diagnosed with SA were included, with an average age of 57.4 years (SD 15.52) (Figure 1). Males constituted 73.5% (1,413/2,027) of the sample and had an average body mass index (BMI) of 29 kg/m² (SD 4.82) (Table 1). In the study population, 53.4% (1,083/2,027) had a history of systemic arterial hypertension, and 17.2% (348/2,027) had COPD. Among patients with COPD, 15.1% (291/1,922) survived, while 54.3% (57/105) died (p < 0.001).
 |
Table 1 General Characteristics of the Population |
 |
Figure 1 Flowchart of study. |
Polysomnography
The average AHI of the general population was 37.1 (SD 24.79), 36.7 (SD 24.65) in living patients, and 44.9 (SD 26.41) in deceased patients (p < 0.001). Positive pressure therapy was indicated for 80% (1,622/2,027) of the general population. CPAP usage was 79.5% (1,528/1,922) in living patients compared to 89.5% (94/105) in deceased patients (p = 0.012). The characteristics of the polysomnographies performed on the population are described in Table 2.
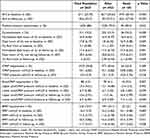 |
Table 2 Polysomnographic Characteristics |
Five-Year Survival
The five-year survival rate in the general population was 94.6% (Figure 2), with no significant differences between men (94.1%) and women (95.8%) (p = 0.144) (Figure 3). However, there was a significant decrease in survival in patients over 65 years old (88.5%) compared to those under 65 years old (97.9%) (p < 0.001) (Figure 4). Similarly, the presence of cardiovascular disease was associated with lower survival (89%) compared to patients without this comorbidity (95.2%) (p < 0.001) (Figure 5).
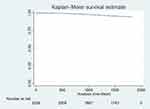 |
Figure 2 Survival at 5 years of follow-up. |
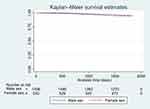 |
Figure 3 Survival at 5 years of follow-up stratified by sex. |
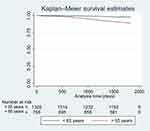 |
Figure 4 Survival at 5 years of follow-up stratified by age. |
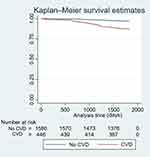 |
Figure 5 Survival at 5 years of follow-up stratified by cardiovascular disease. Abbreviation: CVD, Cardiovascular disease. |
In the Cox regression, age showed an HR of 1.05 (95% CI: 1.02–1.07; p < 0.001). Male sex had an HR of 2.31 (95% CI: 1.25–4.25; p = 0.007), CHF had an HR of 4.00 (95% CI: 2.31–6.94; p < 0.001), COPD had an HR of 1.75 (95% CI: 1.04–2.96; p = 0.035), connective tissue disease had an HR of 1.99 (95% CI: 0.96–4.10; p = 0.064), CKD had an HR of 2.23 (95% CI: 1.31–3.78; p = 0.003), and metastatic cancer had an HR of 4.96 (95% CI: 1.95–12.60; p = 0.001) (Table 3).
 |
Table 3 Cox Regression: Independently Associated Characteristics with Mortality |
Discussion
In this study, a high five-year survival rate was observed in the general population. Survival decreased in patients over 65 years old and those with cardiovascular disease. Multivariate analysis revealed that advanced age, male sex, CHF, COPD, CKD, and metastatic cancer were associated with an increased risk of mortality, highlighting the influence of these variables on survival. These findings are relevant for considering demographic factors and comorbidities in the prognostic evaluation of patients.
In a study conducted in four Latin American cities Mexico City (Mexico), Montevideo (Uruguay), Santiago (Chile), and Caracas (Venezuela)—Bouscoulet et al reported a high prevalence of SA.19 This prevalence ranged from 2.9% in subjects who did not report snoring, excessive daytime sleepiness, or observed apneas, to 23.5% in those who exhibited all three symptoms. Additionally, 60.2% (95% CI: 58.8% to 61.6%) of the participants reported snoring, 34.7% (95% CI: 33.3% to 36%) suffered from insomnia, 29.2% (95% CI: 27.7% to 30.6%) took daytime naps, and 3.4% (95% CI: 2.9% to 4%) presented with a combination of snoring, sleepiness, and observed apneas. In our study, we used a lower diagnostic threshold compared to that described by Bouscoulet et al, which may have increased the reported prevalence by including a greater number of patients with mild forms of the disease.19
Jara et al20 conducted a retrospective study on the survival of patients with SA and found that five-year survival is high. Factors such as CPAP use increased survival, with 76% without CPAP and 84% with CPAP (p < 0.001). In our study, higher survival was found in patients with SA (94.6%), and variables such as age over 65 and cardiovascular disease affect survival.20 In patients with SA, the interaction between intermittent hypoxemia and sleep fragmentation can amplify their individual effects, intensifying the inflammatory response and oxidative stress.12–15 This synergy contributes to a greater cardiovascular morbidity burden and an increased risk of mortality.14,15
In a retrospective cohort study, Jennum et al21 found that women with SA syndrome had lower mortality than men, even if they did not receive CPAP treatment. Factors such as younger age, being female, having a higher educational level, and low previous comorbidity, assessed using the Charlson comorbidity index for the last three years, were positively associated with survival. In contrast, being male, being 60 years or older, not receiving CPAP treatment, having a higher previous comorbidity burden, and a low educational level were identified as negative predictors of survival. According to our results and the literature, being male is a risk factor for increased mortality in patients diagnosed with SA, even when adjusted for confounding factors. Sex may influence mortality outcomes due to the limited number of women in studies, possibly because they are underdiagnosed. Regarding age, mortality was higher in patients over 65 years old. This finding is consistent with the study by Escrutinio et al,22 which identifies age as a crucial predictor of mortality in patients with SA (HR 1.08, 95% CI 1.07–1.09).
Multiple studies have described the association between SA and cardiovascular diseases.23,24 Albertsen et al25 estimated the risk of developing cardiovascular diseases in 20,240 patients aged ≤50 years, finding that 27.3% developed hypertension within 5 years compared to 15.0% of controls (RR: 1.84; 95% CI: 1.78–1.90). In our study, survival was lower in patients with SA and a history of AMI, CHF, AF, and stroke, with CHF being an independent risk factor for mortality. Heilbrunn et al,23 in a systematic review on the association between SA and the risk of mortality across 22 observational studies, found that SA is a significant risk factor for mortality from cardiovascular diseases (RR 1.94, 95% CI 1.39–2.70). Similar to the results of our study, the impact of cardiovascular disease can be explained by the regulation of the nervous system during the sleep cycle.26,27 Brunetti et al28 evaluated the association of SA and AF in patients with cardiovascular disease and found a correlation between the severity of SA and cardiovascular disease but not a causal association between SA and AF. In our study, patients with SA had a higher prevalence of cardiovascular disease risk factors, including CHF, AMI, and AF.
Ioachimescu et al8 reported an accumulated mortality rate of 52.8% (2630/4980) in patients diagnosed with COPD (29%), asthma (7%), and asthma/COPD overlap (15%). The median time to death was 2.7 years (IQR: 0.8–5.7). The mortality rate was significantly higher in men (62.8%) compared to women (34.4%) (p < 0.001). Beaudin et al7 described the prevalence and risk of CKD progression in 1,295 patients with SA. After stratification, 13.6% of the mild SA group, 28.9% of the moderate SA group, and 30.9% of the severe SA group had a moderate to very high risk of CKD progression (p < 0.001). Patients with moderate and severe SA have a higher risk of CKD progression independently of other confounding factors. This is explained by hypoxemia and sleep fragmentation, which activate the sympathetic nervous system and the renin-angiotensin-aldosterone system, favoring hypertension and glomerular hyperfiltration.
Seijo et al29 described a study with 302 patients who underwent SA screening and chest CT scans, finding an 8% higher prevalence of lung cancer in those with an AHI > 15. This difference was statistically significant, assessed using propensity score matching (p = 0.015) and nearest-neighbor matching (p = 0.041). After adjusting for potential confounding factors, a statistically significant association was found between AHI (p = 0.04), nocturnal hypoxemia (including time spent with oxyhemoglobin saturation below 90%, T90; p = 0.005), 3% oxygen desaturation index (p = 0.02), and lung cancer. Conversely, Theorell-Haglöw et al30 conducted a prospective study that did not find an association between SA and cancer mortality (HR 0.997, 95% CI 0.97–1.02, p = 0.85). Although the objective of our study was not to describe a causal association between SA and cancer development, a significant relationship was observed between chronic nocturnal hypoxemia and 5-year mortality in this population.29–31
SA in patients with COPD can be associated with a worse quality of life and greater deterioration in blood oxygen levels due to lung parenchyma impairment and chronic airflow obstruction; this results in disrupted ventilation perfusion and increased susceptibility to desaturation.32,33 Zhang et al32 reported a prevalence of SA of 44% among 73 COPD patients. The STOP-BANG questionnaire showed worse scores in patients with SA compared to the control group (3.9 vs 3.4; p=0.07), as did the COPD Assessment Test (18.4 vs 15.5; p=0.06). Additionally, nocturnal oximetry demonstrated good accuracy in identifying SA and was independently associated with the AHI in COPD patients.32
Limitations
Among the limitations of our study is its observational nature, with information obtained from clinical records, which may have omissions. However, measures were implemented to minimize information bias, such as continuous training of personnel responsible for data collection. The single-center nature of this research may limit the generalizability of the results. Nevertheless, we believe that the achieved sample size supports the conclusions drawn. Multicenter studies are recommended for a more comprehensive view of survival in SA patients, including a detailed evaluation of treatment adherence.
Conclusion
The study revealed high five-year survival rates, although survival rates were lower when stratified by sex and cardiovascular diseases. Factors associated with decreased overall five-year survival included age, male sex, cardiovascular disease, COPD, CKD, and metastatic cancer. While the single-center design of this research may limit the generalizability of the results, these findings are important for incorporating demographic factors and comorbidities into the prognostic evaluation of patients with SA.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was conducted in accordance with the principles of the current Helsinki Declaration, as well as local, regional, and international regulations pertaining to clinical research, including Colombian Law on Biomedical Research. Ethical approval was obtained from the Medical Ethics Committee of the Clínica Universidad de La Sabana (approval number: 202401). Prior to participating in the study, all participants provided written informed consent, and the confidentiality of their data was strictly maintained throughout the study.
Acknowledgments
The authors are most thankful for the Universidad de La Sabana.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Universidad de la Sabana Grant (MEDESP-5-2024).
Disclosure
The authors declare no competing interests.
References
1. Michael J, Sateia M. International classification of sleep disorders-third edition highlights and modifications. Chest. 2014;146(5):1387–1394.
2. Ge X, Han F, Huang Y, et al. Is Obstructive Sleep Apnea Associated with Cardiovascular and All-Cause Mortality? PLoS One. 2013;8(7):e69432. doi:10.1371/journal.pone.0069432
3. Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi:10.1093/aje/kws342
4. Young T, Finn L, Peppard P, et al. Sleep Disordered Breathing and Mortality: eighteen-Year Follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071–1078. doi:10.1002/14651858.CD001106.pub3
5. Marshall NS, Wong KKH, Liu PY, Cullen SRJ, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31(8):1079–1085.
6. Wang H, Parker JD, Newton GE, et al. Influence of Obstructive Sleep Apnea on Mortality in Patients With Heart Failure. J Am Coll Cardiol. 2007;49(15):1625–1631. doi:10.1016/j.jacc.2006.12.046
7. Beaudin AE, Raneri JK, Ahmed SB, et al. Risk of chronic kidney disease in patients with obstructive sleep apnea. Sleep. 2022;45(2):zsab267.
8. Ioachimescu OC, Janocko NJ, Ciavatta MM, Howard M, Warnock MV. Obstructive Lung Disease and Obstructive Sleep Apnea (OLDOSA) cohort study: 10-year assessment. J Clin Sleep Med. 2020;16(2):267–277. doi:10.5664/jcsm.8180
9. Meidan R, Elalouf O, Tauman R, et al. Systemic Lupus Erythematous and Obstructive Sleep Apnea: a Possible Association. Life. 2023;13(3):697. doi:10.3390/life13030697
10. Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687–698. doi:10.1016/S2213-2600(19)30198-5
11. Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo Epidemiologic Sleep Study. Sleep Med. 2010;11(5):441–446. doi:10.1016/j.sleep.2009.10.005
12. Kainulainen S, Töyräs J, Oksenberg A, et al. Severity of Desaturations Reflects OSA-Related Daytime Sleepiness Better Than AHI. J Clin Sleep Med. 2019;15(8):1135–1142. doi:10.5664/jcsm.7806
13. Martinez-Garcia MA, Sánchez-de-la-Torre M, White DP, Azarbarzin A. Hypoxic Burden in Obstructive Sleep Apnea: present and Future. Arch Bronconeumol. 2023;59(1):36–43. doi:10.1016/j.arbres.2022.08.005
14. Paschou SA, Bletsa E, Saltiki K, et al. Sleep Apnea and Cardiovascular Risk in Patients with Prediabetes and Type 2 Diabetes. Nutrients. 2022;14(23):4989. doi:10.3390/nu14234989
15. Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive Sleep Apnea and Cardiovascular Disease: a Scientific Statement From the American Heart Association. Circulation. 2021;144(3):e56–e67. doi:10.1161/CIR.0000000000000988
16. Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2017;13(3):479–504. doi:10.5664/jcsm.6506
17. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
18. Hosmer DW, Lemeshow S. Applied Logistic Regression.
19. Bouscoulet LT, Vázquez-García JC, Muiño A, et al. Prevalence of sleep related symptoms in four Latin American cities. J Clin Sleep Med. 2008;4(6):579–585. doi:10.5664/jcsm.27353
20. Jara SM, Phipps AI, Maynard C, Weaver EM. 0565 Long-Term Survival in Veterans with Sleep Apnea. Sleep. 2018;41(1):A210–A211. doi:10.1093/sleep/zsy061.564
21. Jennum P, Tønnesen P, Ibsen R, Kjellberg J. All-cause mortality from obstructive sleep apnea in male and female patients with and without continuous positive airway pressure treatment: a registry study with 10 years of follow-up. Nat Sci Sleep. 2015;7:43–50. doi:10.2147/NSS.S75166
22. Scrutinio D, Guida P, Aliani M, Castellana G, Guido P, Carone M. Age and comorbidities are crucial predictors of mortality in severe obstructive sleep apnoea syndrome. Eur J Intern Med. 2021;90:71–76. doi:10.1016/j.ejim.2021.04.018
23. Heilbrunn ES, Ssentongo P, Chinchilli VM, Oh J, Ssentongo AE. Sudden death in individuals with obstructive sleep apnoea: a systematic review and meta-analysis. BMJ Open Respir Res. 2021;8(1):e000656. doi:10.1136/bmjresp-2020-000656
24. Salari N, Khazaie H, Abolfathi M, et al. The effect of obstructive sleep apnea on the increased risk of cardiovascular disease: a systematic review and meta-analysis. Neurol Sci. 2022;43(1):219–231. doi:10.1007/s10072-021-05765-3
25. Albertsen IE, Bille J, Piazza G, Lip GYH, Nielsen PB. Cardiovascular Risk in Young Patients Diagnosed With Obstructive Sleep Apnea. J Am Heart Assoc. 2024;13(8):e033506. doi:10.1161/JAHA.123.033506
26. Zisapel N. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br J Pharmacol. 2018;175(16):3190–3199. doi:10.1111/bph.14116
27. Ishikawa O, Oks M. Central Sleep Apnea. Clin Geriatr Med. 2021;37(3):469–481. doi:10.1016/j.cger.2021.04.009
28. Brunetti V, Testani E, Losurdo A, et al. Association of Obstructive Sleep Apnea and Atrial Fibrillation in Acute Ischemic Stroke: a Cross-Sectional Study. J Pers Med. 2023;13(3):527. doi:10.3390/jpm13030527
29. Seijo LM, Pérez-Warnisher MT, Giraldo-Cadavid LF, et al. Obstructive sleep apnea and nocturnal hypoxemia are associated with an increased risk of lung cancer. Sleep Med. 2019;63:41–45. doi:10.1016/j.sleep.2019.05.011
30. Theorell-Haglöw J, Zhou X, Wittert G, et al. Does obstructive sleep apnea increase the risk of cancer and cancer mortality in combined community-based cohorts? J Sleep Res. 2023;33(4):e14089. doi:10.1111/jsr.14089
31. Nautiyal H, Roy D, Arya A, et al. Sleep Attributes Influencing Cardiovascular Morbidity Among Young Adults Pursuing Professional Courses in Dehradun, India: a Cross-Sectional Study. Cureus. 2024;16(1):e52647. doi:10.7759/cureus.52647
32. Zhang XL, Dai HP, Zhang H, et al. Obstructive Sleep Apnea in Patients With Fibrotic Interstitial Lung Disease and COPD. J Clin Sleep Med. 2019;15(12):1807–1815. doi:10.5664/jcsm.8090
33. Bouloukaki I, Fanaridis M, Testelmans D, Pataka A, Schiza S. Overlaps between obstructive sleep apnoea and other respiratory diseases, including COPD, asthma and interstitial lung disease. Breathe. 2022;18(3):220073. doi:10.1183/20734735.0073-2022
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

