Back to Journals » Journal of Pain Research » Volume 18
Suzetrigine, a Non-Opioid NaV1.8 Inhibitor With Broad Applicability for Moderate-to-Severe Acute Pain: A Phase 3 Single-Arm Study for Surgical or Non-Surgical Acute Pain
Authors McCoun J, Winkle P, Solanki D , Urban J, Bertoch T, Oswald J, Swisher MW, Taber LA, Healey T, Jazic I, Correll DJ, Negulescu PA, Bozic C, Weiner SG
Received 8 December 2024
Accepted for publication 8 March 2025
Published 25 March 2025 Volume 2025:18 Pages 1569—1576
DOI https://doi.org/10.2147/JPR.S509144
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Karina Gritsenko
Jessica McCoun,1 Peter Winkle,2 Daneshvari Solanki,3 Joshua Urban,4 Todd Bertoch,5 Jessica Oswald,6,7 Matthew W Swisher,7 Louise Anne Taber,8 Tiffany Healey,9 Ina Jazic,10 Darin J Correll,11 Paul A Negulescu,12 Carmen Bozic,13 Scott G Weiner14 On behalf of the VX-548-107 Study Team
1Cenexel Georgia, Atlanta, GA, USA; 2Anaheim Clinical Trials, Anaheim, CA, USA; 3Clinical Investigation, HD Research, LLC, Bellaire, TX, USA; 4Orthopedic Surgery, OrthoNebraska, Omaha, NE, USA; 5CenExel JBR Clinical Research, Salt Lake City, UT, USA; 6Department of Emergency Medicine, UC San Diego Health, San Diego, CA, USA; 7Department of Anesthesiology, Center for Pain Medicine, UC San Diego, San Diego, CA, USA; 8Arizona Research Center, Phoenix, AZ, USA; 9Global Patient Safety, Vertex Pharmaceuticals, Boston, MA, USA; 10Biostatistics, Vertex Pharmaceuticals, Boston, MA, USA; 11Clinical Development, Vertex Pharmaceuticals, Boston, MA, USA; 12Research, Vertex Pharmaceuticals, Boston, MA, USA; 13Global Medicines Development and Affairs, Vertex Pharmaceuticals, Boston, MA, USA; 14Emergency Medicine, Brigham and Women’s Hospital, Boston, MA, USA
Correspondence: Carmen Bozic, Vertex Pharmaceuticals, 50 Northern Avenue, Boston, MA, 02210, USA, Email [email protected]
Background: Many patients experience inadequate pain control due to limited options that are both efficacious and safe for treating moderate-to-severe acute pain; therefore, opioids are still frequently prescribed for their effectiveness despite known tolerability issues and safety concerns. Suzetrigine, an oral, non-opioid, offers a promising alternative by selectively inhibiting the voltage-gated sodium channel 1.8 (NaV 1.8), a novel therapeutic target for pain management. Given the high selectivity of suzetrigine for NaV 1.8 (does not bind to other sodium channels/receptors with CNS activity), suzetrigine does not have CNS side effects or addictive potential associated with opioids. In the largest randomized, controlled phase 3 trials in established acute pain models, suzetrigine monotherapy demonstrated statistically significant and clinically meaningful reduction in moderate-to-severe acute pain compared to placebo.
Methods: To evaluate the safety and effectiveness of suzetrigine for the treatment of moderate-to-severe-acute surgical and non-surgical pain conditions, we conducted a phase 3, single-arm study in adults with moderate or severe acute pain on the verbal categorical rating scale and ≥ 4 on the numeric pain rating scale following surgical procedures or after presenting to a medical facility with moderate or severe acute pain of new origin. Participants received suzetrigine (100mg then 50mg every 12hrs) for 14 days or pain resolution, whichever came first. The primary endpoint was safety. The secondary endpoint was participant perception of suzetrigine’s effectiveness in treating acute pain at the end of treatment using a patient global assessment.
Results: Suzetrigine was generally safe and well-tolerated in participants (N=256) with a range of surgical and non-surgical acute pain conditions; the maximum severity for most participants who had adverse events was mild (71 participants; 27.7%) or moderate (21 participants; 8.2%). Most participants (213 participants; 83.2%) rated suzetrigine’s effectiveness for treating pain on a patient global assessment as good, very good, or excellent.
Conclusion: Suzetrigine provides a safe and effective non-opioid, non-addictive treatment with broad applicability for moderate-to-severe acute pain.
Clinicaltrials.gov Registration: NCT05661734.
Keywords: suzetrigine, VX-548, non-opioid, NaV1.8 inhibitor, moderate-to-severe acute pain, surgical/nonsurgical acute pain
Introduction
There are limited therapeutic options for moderate-to-severe acute pain that are both efficacious and safe. As a result, patients and clinicians often rely on opioids for effective pain management despite known tolerability issues and safety concerns, including addictive potential.1 Suzetrigine (VX-548) is an oral, small molecule, non-opioid pain signal inhibitor with potential to overcome the shortcomings of current standard-of-care based on its mechanism of action. Suzetrigine selectively and potently inhibits the voltage gated sodium channel 1.8 (NaV1.8),2 a novel therapeutic target for pain. NaV1.8 has a critical role in transmitting nociceptive signals, has selective expression on nociceptors within peripheral sensory nerves and dorsal root ganglia, and is not present in the human brain.3–6 In addition, there is no evidence that suzetrigine has addictive potential based on its mechanism of action, preclinical in vivo data, and clinical adverse event data from participants with moderate-to-severe acute pain.2,7 In two Phase 2 and two phase 3, randomized, active- and placebo-controlled trials, suzetrigine demonstrated statistically significant and clinically meaningful reductions in pain following abdominoplasty and bunionectomy, established models of acute pain.8,9 In the two phase 3 trials, the primary endpoint of the least squares mean difference in the time-weighted sum of the pain intensity difference for suzetrigine compared to placebo from 0 to 48 hours (SPID48) was 48.4 (95% CI: 33.6, 63.1; P<0.0001) after abdominoplasty and 29.3 (95% CI: 14.0, 44.6; P=0.0002) after bunionectomy.8,9 Suzetrigine was safe and well tolerated; there were no serious adverse events considered by the investigators to be related to suzetrigine. Based on these findings, we hypothesized that suzetrigine may offer broad applicability to treat acute pain. To expand on these findings, we evaluated the safety and effectiveness of suzetrigine in moderate-to-severe acute pain resulting from a variety of surgical and non-surgical conditions.
Methods
We conducted a phase 3, single-arm study to evaluate the safety and effectiveness of suzetrigine in treating acute pain resulting from a wide range of surgical and non-surgical conditions between January 2023 and December 2023 across the United States (clinicaltrials.gov registration: NCT05661734, principal investigator Peter Winkle, first participant consented on January 9, 2023, https://clinicaltrials.gov/study/NCT05661734). A list of investigators who enrolled participants in our study and their site’s location are provided in Supplementary Information 1. The study protocol was approved by a central institutional review board (ADVARRA, United States; ethics approval number 00023875) and conducted in accordance with the International Council for Harmonization Good Clinical Practice guidelines and the principles of the Declaration of Helsinki. All participants provided written informed consent before screening.
Study Design and Participants
An overview of the study design is provided in Supplementary Information 3 (Supplementary Figure 1). Our study eligibility criteria permitted enrollment of adults, 18 to 80 years of age, with moderate or severe acute pain on the verbal categorical rating scale (VRS) and ≥4 on the numeric pain rating scale (NPRS; range 0–10) following surgical procedures or after presenting to a medical facility with non-surgical pain of new origin (prior 48 hours; not related to a prior known condition). Detailed study eligibility criteria for our study are provided in Supplementary Information 2. Participants requesting study drug for pain relief received suzetrigine (100 mg first dose, then 50 mg every 12 hours) for 14 days or until their pain resolved, whichever occurred first. Participants were permitted to use concomitant acetaminophen (650 mg) and ibuprofen (400 mg) every 6 hours (termed rescue medication), as needed for additional pain relief, in line with standard multimodal therapy; no other analgesic medications (eg, NSAIDs other than ibuprofen, opioids) were permitted during study drug treatment.
Outcomes
The primary endpoint was safety and tolerability based on treatment-emergent adverse events, laboratory test results, vital signs, and electrocardiograms. During the conduct of the study, participants were queried at each study visit, using nonleading questions, about the occurrence of any adverse events. The investigator determined and recorded the severity and causality for all adverse events.
The secondary endpoint was the participants’ perception of the effectiveness of suzetrigine in managing pain at the end of treatment assessed by the proportion of participants reporting good, very good, or excellent on a validated patient global assessment, using a 5-point Likert scale (poor, fair, good, very good, or excellent).10
Sample Size Calculation and Statistical Analysis
The probability of observing an adverse event with incidence r in at least one of n study participants was calculated as 1–(1–r)n. Approximately 250 participants were planned to be enrolled to provide a 92% probability of observing an adverse event in at least one participant if the true incidence was 1% and a 99% probability of observing an adverse event in at least one participant if the true incidence was 2%.
All analyses included participants who received at least one dose of suzetrigine. Safety and patient global assessment data were summarized descriptively. For the patient global assessment, the end of treatment was defined as either day 14 or within 24 hours after the last dose for participants who completed or discontinued suzetrigine. Missing patient global assessments at the end of treatment were imputed using the previous patient global assessment. Participants with no previous patient global assessments available were considered non-responders.
Results
Participants
A total of 256 participants (mean age (SD) of 43.9 (14.1) years) received at least one dose of suzetrigine: 173 (67.6%) participants were female with a mean (SD) age of 43.9 (14.1) years and 83 (32.4%) were male with a mean (SD) age of 44.0 (14.1) years (Table 1). Participants had pain at baseline that was either moderate (191 participants; 74.6%) or severe (65 participants; 25.4%) on the VRS with a mean NPRS score of 6.7. Most participants, 222 (86.7%) had pain from surgical procedures (Figure 1A) and the remaining 34 (13.3%) participants had non-surgical pain (Figure 1B). A total of 187 (73.0%) participants used multimodal therapy; use of (concomitant use of acetaminophen and ibuprofen) was higher for surgical participants (177 of 222 participants; 79.7%) than non-surgical participants (10 of 34 participants; 29.4%).
 |
Table 1 Demographics and Baseline Clinical Characteristics |
Disposition
A CONSORT diagram of study participation is provided in Supplementary Information 3 (Supplementary Figure 2). Most participants (242 participants; 94.5%) completed treatment with suzetrigine (Table 2); 137 (53.5%) before day 14 due to pain resolution, and 105 (41.0%) completed on day 14. Five (2.0%) participants discontinued suzetrigine because of adverse events and four (1.6%) participants discontinued suzetrigine because of perceived lack of efficacy.
 |
Table 2 Disposition |
Safety
Suzetrigine was generally safe and well-tolerated with most adverse events being mild or moderate in severity (Table 3). The most common adverse events (at least 2% of participants) were headache, constipation, nausea, fall, and rash. The only adverse event occurring in at least 5% of participants was headache (18 participants; 7.0%). There were two (0.8%) participants with serious adverse events, which were considered by the investigator as not related to suzetrigine: one participant had suicidal ideation, and one participant had cellulitis.
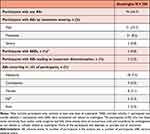 |
Table 3 Summary of Adverse Events |
Effectiveness
Overall, the proportion of participants with moderate-to-severe pain reporting good, very good, or excellent on the patient global assessment at the end of suzetrigine treatment was 83.2% (213 of 256 participants) (Figure 2A; Supplementary Information 4, Supplementary Table 1) with 82.0% reported among surgical participants (182 of 222 surgical participants) and 91.2% among non-surgical participants (31 of 34 non-surgical participants) (Figure 2B). The proportion of participants with moderate-to-severe pain reporting good, very good, or excellent on the patient global assessment at the end of suzetrigine treatment was similar between participants who took rescue medication (82.4%; 154 of 187 participants) and participants who did not take rescue medication (85.5%; 59 of 69 participants) (Supplementary Information 4, Supplementary Table 2).
Discussion
As a potent and highly selective NaV1.8 inhibitor,2 suzetrigine targets a critical underlying pain signaling mechanism in the peripheral nervous system, and as such, does not have addictive potential. This innovation has the potential to address the unmet need in moderate-to-severe acute pain management with a non-opioid, non-addictive analgesic.
Our study demonstrates that suzetrigine is both safe and effective for the treatment of a wide range of surgical and non-surgical acute pain conditions. Suzetrigine was generally well-tolerated, with adverse events consistent with those observed in individuals experiencing acute pain from similar conditions evaluated in our study. Regardless of the type of acute pain, a high proportion of participants (213 participants; 83.2%) reported good, very good, or excellent on the patient global assessment at the end of suzetrigine treatment with only four (1.6%) discontinuing suzetrigine due to lack of efficacy. This level of satisfaction was independent of whether the acute pain was surgical or non-surgical and supports the use of suzetrigine across a broad range of moderate-to-severe acute pain conditions. For context, in an open-label study of a moderate opioid tramadol administered intravenously in the hospital, 95% of patients rated their treatment as good, very good, or excellent at 48 hours.11 Thus, we find the strong response of suzetrigine important given that suzetrigine was orally administered in an outpatient setting over 14 days.
Our study demonstrated how suzetrigine can be used as either a monotherapy or with acetaminophen/ibuprofen as part of multimodal therapy, as practiced in clinical medicine. Participants were permitted to take additional multimodal therapy for pain relief, as needed, starting any time after the first dose of suzetrigine. Consistent with expectations, most patients used permissible concomitant medications supporting the utility of suzetrigine as part of a standard multimodal therapy regimen; however, additional studies may be needed to further assess the effectiveness of suzetrigine as a multimodal therapy regimen.
The results from our study further support the findings from two phase 22 and two phase 38,9 trials (all designed as randomized, double-blind, active- and placebo-controlled trials) that demonstrated that suzetrigine leads to a statistically significant and clinically meaningful reduction in moderate-to-severe acute pain in established models of acute pain.8,9 The totality of results across these five studies8,9 provides robust evidence of the effectiveness of suzetrigine for the treatment of broad acute pain conditions without addictive potential.2
Limitations
This was a single-arm study; therefore, the effectiveness of suzetrigine compared to placebo or an active control cannot be concluded. We did not conduct formal statistical hypothesis testing comparing suzetrigine effectiveness in surgical and non-surgical pain conditions; however, the results are generally consistent across these conditions and with findings from other suzetrigine acute pain trials.2,8,9
Conclusions
For the first time in over two decades, suzetrigine, a novel small molecule and highly selective NaV1.8 inhibitor, offers an effective and safe non-opioid, non-addictive treatment with broad applicability for the treatment of moderate-to-severe acute pain.
Acknowledgements
We thank the study participants, their families, and the site investigators. Medical writing support was provided by Allison K. Lord, Ph.D. (AKL) and Concetta G. Marfella, Ph.D. (CGM) under the guidance of the authors. AKL and CGM are employees of Vertex Pharmaceuticals and hold stock and/or options in the company.
Group Information
Trial investigators are listed in Supplemental Information 1.
Data Sharing Statement
Vertex is committed to advancing medical science. This includes the responsible sharing of data with qualified researchers. Proposals for the use of these data will be reviewed by a scientific board. Approvals are at the discretion of Vertex and will be dependent on the nature of the request, the merit of the research proposed, and the intended use of the data. Please contact [email protected] if you would like to submit a proposal or need more information.
Funding
This study was supported by Vertex Pharmaceuticals. Vertex Pharmaceuticals sponsored the design and conduct of the studies; collection, management, analysis, and interpretation of the data; preparation, review, and approval of the manuscript; and the decision to submit the manuscript for publication.
Disclosure
Drs. McCoun, Solanki, Urban, Bertoch, Oswald, Swisher, Taber, and Weiner have reported personal fees from Vertex Pharmaceuticals as members of the Acute Pain Steering Committee. Dr. Urban has reported personal fees and honoraria from Pacira Biosciences. Dr. Oswald participates on a Data Safety Monitoring Board for Salix Pharmaceuticals. Dr. Swisher reports funding paid to his institution from SPR Therapeutics, Infutronix, and Avanos Medical, during the conduct of the study. Drs. Healey, Jazic, Correll, Negulescu, and Bozic are employees of Vertex Pharmaceuticals and own stock and/or options in the company. Dr. Weiner reports personal fees from Cessation Therapeutics, Inc., outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Bruehl S, Apkarian AV, Ballantyne JC, et al. Personalized medicine and opioid analgesic prescribing for chronic pain: opportunities and challenges. J Pain. 2013;14(2):103–113. doi:10.1016/j.jpain.2012.10.016
2. Jones J, Correll DJ, Lechner SM, et al. Selective inhibition of Na(V)1.8 with VX-548 for acute pain. N Engl J Med. 2023;389(5):393–405. doi:10.1056/NEJMoa2209870
3. Shiers S, Klein RM, Price TJ. Quantitative differences in neuronal subpopulations between mouse and human dorsal root ganglia demonstrated with RNAscope in situ hybridization. Pain. 2020;161(10):2410–2424. doi:10.1097/j.pain.0000000000001973
4. Staedtler ES, Sapio MR, King DM, et al. The μ-opioid receptor differentiates two distinct human nociceptive populations relevant to clinical pain. Cell Rep Med. 2024;5(10):101788. doi:10.1016/j.xcrm.2024.101788
5. The GTEx Consortium. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science. 2020;369(6509):1318–1330. doi:10.1126/science.aaz1776
6. Han C, Huang J, Waxman SG. Sodium channel Nav1.8: emerging links to human disease. Neurology. 2016;86(5):473–483. doi:10.1212/WNL.0000000000002333
7. Osteen JD, Immani S, Tapley TL, et al. Pharmacology and mechanism of action of Suzetrigine, a potent and selective NaV1.8 pain signal inhibitor for the treatment of moderate to severe pain. Pain Therapy. 2025. doi:10.1007/s40122-024-00697-0
8. Bertoch T, D’Aunno D, McCoun J, et al. Suzetrigine, a non-opioid Na. Under J Rev. In Press 2025.
9. Bertoch T, D’Aunno D, McCoun J, et al. Randomized, placebo-controlled, phase 3 trials of Suzetrigine, a non-opioid, pain signal inhibitor for treatment of acute pain after abdominoplasty or bunionectomy. Journal-related Activities and Other Special Activities at the 2024 American Society of Anesthesiologists Meeting [abstract]. Anesthesiology. 2024;141(4):647.
10. Rothman M, Vallow S, Damaraju CV, Hewitt DJ. Using the patient global assessment of the method of pain control to assess new analgesic modalities in clinical trials. Curr Med Res Opin. 2009;25(6):1433–1443. doi:10.1185/03007990902862032
11. Avenue Therapeutics Inc. 15 February 2022. Sponsor briefing document for tramadol hydrochloride injection: NDA 213231. Available at: https://www.fda.gov/media/156139/download.
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



