Back to Journals » Neuropsychiatric Disease and Treatment » Volume 21
The 4977 Bp Deletion of Mitochondrial DNA as a Potential Trait Marker for Major Depressive Disorder
Authors He Y , Yang X, Li Z, Liu W, Tang J, Chen X
Received 27 November 2024
Accepted for publication 27 March 2025
Published 13 April 2025 Volume 2025:21 Pages 867—873
DOI https://doi.org/10.2147/NDT.S509050
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yu-Ping Ning
Ying He,1,* Xinbo Yang,1,* Zongchang Li,1 Weiqing Liu,2,3 Jinsong Tang,4 Xiaogang Chen1
1Department of Psychiatry, National Clinical Research Center for Mental Disorders, and National Center for Mental Disorders, The Second Xiangya Hospital of Central South University, Changsha, Hunan, 410011, People’s Republic of China; 2Clinical Research Center for Mental Disorders, Shanghai Pudong New Area Mental Health Center, School of Medicine, Tongji University, Shanghai, 200122, People’s Republic of China; 3Laboratory for Molecular Mechanisms of Brain Development, Center for Brain Science (CBS), RIKEN, Wako, Saitama, Japan; 4Department of Psychiatry, Zhejiang University School of Medicine Sir Run Run Shaw Hospital, Hangzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ying He, Email [email protected]
Background: Major depressive disorder (MDD) is significantly influenced by genetic factors. The present study aims to examine the potential correlation between the 4977 bp deletion of mitochondrial DNA (mtDNA) and MDD.
Methods: The 4977 bp deletion of mtDNA was detected in the peripheral blood of 253 MDD patients and 257 healthy controls, with depression assessed by the Hamilton Depression Rating scale and functioning by the Global Assessment of Function Scale.
Results: MDD patients had a higher incidence of the 4977 bp deletion, unaffected by demographic or clinical factors.
Conclusion: The 4977 bp deletion may be a trait marker for MDD.
Keywords: major depressive disorder, mitochondrial DNA deletion, mtDNA deletion, 4977 bp deletion
Introduction
Major depressive disorder (MDD), a disorder that affects the energy-sensitive brain, is characterized by the lack of motivation and loss of interest in daily activities. Clinical signs and symptoms of MDD include persistently poor mood, loss of interest, major weight changes, sleep difficulties, decreased energy, low self-esteem, difficulty concentrating, suicidal thoughts, physical agitation or retardation, and thoughts of death. These are defined by the DSM.1 These symptoms need to be present for varying lengths of time and significantly disrupt everyday living or cause discomfort. As the brain’s energy production relies heavily on mitochondria, there have been evidences supporting the “mitochondrial psychiatry” model of depression 2. Postmortem studies have revealed a decrease in the expression of mitochondrial DNA (mtDNA) products in the frontal cortex 3 and cerebellum4 of individuals with MDD. In animal models of MDD, the suppression of the mitochondrial respiratory chain has also been found.5 Genetic studies have been indicated an increased frequency of mtDNA deletions in MDD,6,7 and shared mtDNA mutations between mitochondrial disorders and MDD.8 There are also studies suggesting that mitochondrial dysfunction may be the cellular and biological basis for synaptic changes in the brain of depression.9 These findings strongly suggest a link between MDD and mtDNA abnormalities.
The majority of studies on depression concentrated on mtDNA mutations, ignoring more catastrophic flaws that are essential to the quantity and quality of mtDNA, such as mtDNA copy number variation and 4977 bp deletion.10,11 Our previous research did not establish a significant correlation between mtDNA copy number and MDD.12 As importantly, the 4977 bp deletion in mtDNA is the most common damage to human mtDNA (due to the presence of two 13 bp forward repeat regions between 8470–8482 bp and 13447–13459 bp, which have identical sequences: 5′-ACCTCCCTCACC-3′. Since the sequences near this region are rich in AT, the DNA molecule configuration tends to form bends here, and the bent DNA molecule is not only susceptible to oxidative damage but can also combine with topoisomerase, leading to abnormal DNA replication and resulting in a 4977 bp deletion between 8470 bp to 13447 bp or 8482 bp to 13459 bp). It is also the most severe damage because the deleted fragment is not only large in scope but also encodes many key enzymes in the oxidative phosphorylation pathway (such as four subunits in Complex I: MT-ND3, MT-ND4, MT-ND4L, and MT-ND5; MT-CO3 in Complex IV; MT-ATP8 and MT-ATP6 in Complex V; and five tRNA genes: MT-TG, MT-TR, MT-TH, MT-TS2, MT-TL2), and thus is considered a biomarker of mtDNA damage, reflecting the quality of mtDNA.13,14 In the present study, we aim to investigate the association between the 4977 bp deletion of mtDNA and MDD in a case-control study.
Methods
Participants
The study adhered to the Declaration of Helsinki, with all participants providing informed consent after being informed about risks and benefits. For minors or those unable to consent, legal guardians provided written consent. The study was approved by the ethical committee of the Second Xiangya Hospital at Central South University.
In this study, 253 MDD patients and 257 matched healthy controls (HC) were enrolled through the Second Xiangya Hospital’s Outpatient Department. Meeting DSM-IV-TR criteria, being between the ages of 17 and 45, and comprehending the survey’s content are prerequisites for participation in the severe depression group. Schizophrenia, substance or alcohol abuse, neurological abnormalities, severe illnesses, abnormal blood or organ function, pregnancy, and breastfeeding are among the exclusion factors. HC must be between the ages of 17 and 45, have signed consent, and match in age and gender. Mental disorders, serious illnesses, brain injury, substance misuse, and a family history of mental or epilepsy issues are excluded.
Depression and Function Assessment
General information about MDD patients was collected, such as age, gender, age at onset, marital status, occupation, degree of education, medication, and number of prior episodes. The Hamilton-17 Depression Rating Scale (HDRS-17) was utilized to evaluate the intensity of depression.15 The Global Assessment of Function Scale (GAF) was used to evaluate the psychological, social, and occupational function.16
Detection of mtDNA 4977 Bp Deletion
MtDNA Extraction
The extraction of mtDNA from peripheral blood leukocytes can be referred to our previous research.12 The sample for detecting 4977 bp deletion of mtDNA was diluted to 50 ng/μL using sterile deionized water and stored in a refrigerator at 4°C for later use. Primers were designed based on the method reported by Aral et al in 2010.17 Primer design and evaluation were strictly conducted using Primer 5.0 according to the principles of primer design to confirm no additional matches. The primers were synthesized by Beijing Dingguo Changsheng Biotechnology Co., Ltd. in PAGE purity grade (see Table 1).
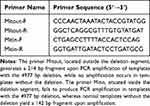 |
Table 1 The Primer Sequences |
Amplification of Target Fragments
The primers were centrifuged for 10 minutes and then diluted with sterile deionized water to a final concentration of 100 μmol/L. The diluted primer mixture was thoroughly mixed and centrifuged for 20 seconds before storage at 4°C.
For the PCR reaction, 10 ng of DNA was mixed with 5 mL Taq PCR Green Mix (provided by Thermo Scientific, Inc.) and 4 pmol of each primer in a final volume of 10 mL. The PCR conditions were as follows: initial denaturation at 95°C for 5 minutes, followed by 35 cycles of denaturation at 95°C for 30s, annealing at 60°C for 30s, and extension at 72°C for 30s. The reaction was then incubated at 72°C for 2 minutes.
Agarose Gel Electrophoresis
After amplification of DNA samples using regular PCR, the resulting amplification products were subjected to electrophoresis on a 2% agarose gel (provided by Biowest, a company based in Spain). Subsequently, the gel was placed in the EpiChemi3 Darkroom and imaged using an image analysis system (see Figure 1).
Confirmation of the 4977 bp Deletion
To prepare the agarose gel for electrophoresis, agarose powder was diluted in 0.5× TBE buffer, heated until clear, and mixed with GelRed DNA dye (supplied by Biotium, Inc). The solution was cooled before pouring into a gel tray. After solidification, PCR products were loaded and electrophoresis run at 150V. To confirm the presence of the desired 4977 bp deletion in the amplified fragments, five PCR products with bands at 214 bp were selected for sequencing analysis conducted by Nanjing GenScript Biotech Co., Ltd. (see supplementary material 1). The obtained nucleotide sequences were subsequently compared with the theoretically predicted sequence that would result from a 4977 bp deletion (see supplementary material 2).
Statistical Analysis
Statistical analyses were conducted with SPSS 17.0. Group results are presented as mean ± S.D. The usual threshold of significance (p) was fixed at 0.05 for two-tailed tests. The count data was analyzed using a chi-square test and presented as percentages. Levene’s test was used to confirm the homogeneity of variances between the groups. Relationships between variables were evaluated with the Spearman’s rank correlation test.
Result
Both groups were well matched for age and gender (see Table 2). The MDD patients had a mean age of onset of 33.0 (±11.67), with 145 individuals (57.31%) reporting a history of medication use.
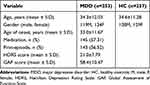 |
Table 2 General Characteristics of the Recruited Subjects |
Among the 253 cases of MDD, 124 cases (49.0%) were found to have the 4977 bp deletion of mtDNA. In comparison, only 72 out of 257 cases (28.0%) exhibited the same deletion in the HC group (χ2 = 23.753, p = 0.000 < 0.05) (see Figure 2). Univariate analysis revealed no significant connection between the 4977 bp deletion of mtDNA and demographic factors or depression severity in the MDD group. (see Table 3). Likewise, the 4977 bp deletion of mtDNA was not significantly correlated with age (t = −1.030, p = 0.304 > 0.05) or gender (χ2 = 1.150, p = 0.284 > 0.05) in the HC group, according to univariate analysis.
 |
Table 3 Univariate Analysis of 4977 Bp Deletion of mtDNA in Major Depressive Disorder |
Discussion
The present study indicates that the frequency of 4977 bp deletion of mtDNA in leukocytes is significantly higher in patients compared to healthy controls, suggesting poorer mtDNA quality in MDD. However, there is no correlation between the frequency of 4977 bp deletion and age, age of onset, marital status, education level, or medication history.
Numerous neurodegenerative diseases are linked to both changes in the copy number and quality of mtDNA, also known as mtDNA mutations.18 One of the earliest kinds of mtDNA mutations thought to cause human diseases is a large mtDNA deletion. The 4977 bp deletion is the most frequent of these large deletions and may indicate alterations in the quality of mtDNA because it impacts three of the five complexes that make up the respiratory chain (Complex I, Complex Ⅳ, and Complex Ⅴ).19,20 The role of mitochondria and mtDNA in the development of MDD has been explored over the years, but the exact molecular mechanisms by which mtDNA segmental deletions contribute to the pathogenesis of MDD remain unclear. The 4977 bp region of mtDNA contains the MT-ATP8 and MT-ATP6 genes, which, when absent, impede electron transport chain Complex V and further damaging the cellular respiration and ATP synthesis.21 Reports associated with mutations in MT-ATP8 and MT-ATP6 genes primarily manifest as intellectual disability, central and peripheral nerve damage, language impairments, and motor disorders.22,23 Therefore, the 4977 bp deletion of mtDNA may also play a critical role in the development of MDD.
Early detection of this loss during the diagnostic procedure may result in more individualized treatment regimens and earlier action. In patients with MDD, a number of intriguing intervention techniques have demonstrated possible antidepressant effects in recent years. Deep transcranial magnetic stimulation, for example, has become a non-invasive method for regulating brain activity and reducing symptoms of depression.24 Another cutting-edge strategy to lessen the intensity of depression is continuous theta burst stimulation, which targets particular brain circuits.25 Furthermore, Stanford’s neuromodulation therapy enhances brain plasticity and elevates mood by combining electrical stimulation with cognitive training.26 These methods, along with the early discovery of the 4977 bp deletion, may open the door to more focused and efficient treatments, giving MDD sufferers who are trying to get rid of their crippling symptoms fresh hope. The lives of people with MDD could be greatly improved by incorporating these cutting-edge intervention techniques into therapeutic practice.
Currently, methodological limitations in the study of mtDNA and the multi-organ involvement and complex features of mitochondrial respiratory chain impairment hinder the precise understanding of the molecular mechanisms involved. However, further research will help reveal the association between mitochondrial dysfunction and MDD, providing important clues for early detection and intervention. Additionally, it is important to explore the intrinsic connections between mitochondrial dysfunction and various clinical manifestations of MDD.
Conclusion
There is a strong association between mtDNA 4977 bp deletion and the diagnosis of MDD, rather than severity, frequency of episodes, or medication status. This indicates that the 4977 bp deletion of mtDNA reflects more of a trait marker rather than a state indicator in MDD, which is crucial for selecting disease biomarkers. The prospective identification of the 4977 bp deletion of mtDNA as a diagnostic biomarker for MDD has promise for facilitating early diagnosis and the discovery of therapeutic targets.
Funding
The work was supported by the National Natural Science Foundation of China (No. 82401769), the National Key Research and Development Program of China (No. 2021YFE0191400), and the Scientific Research Launch Project for new employees of the Second Xiangya Hospital of Central South University.
Disclosure
All authors state that there is no conflict of interest in this work.
References
1. Association AP. Diagnostic and Statistical Manual of Mental Disorders. Diagnostic and Statistical Manual of Mental Disorders.
2. Cardon I, Grobecker S, Jenne F, et al. Serotonin effects on human iPSC-derived neural cell functions: from mitochondria to depression. Mol Psychiatry. 2024;29(9):2689–2700. doi:10.1038/s41380-024-02538-0
3. Thorne BN, Ellenbroek BA, Day DJ. The serotonin reuptake transporter modulates mitochondrial copy number and mitochondrial respiratory complex gene expression in the frontal cortex and cerebellum in a sexually dimorphic manner. J Neurosci Res. 2022;100(3):869–879. doi:10.1002/jnr.25010
4. Reetz K, Lencer R, Steinlechner S, et al. Limbic and frontal cortical degeneration is associated with psychiatric symptoms in PINK1 mutation carriers. Biol Psychiatry. 2008;64(3):241–247. doi:10.1016/j.biopsych.2007.12.010
5. Kolar D, Kleteckova L, Brozka H, Vales K. Mini-review: brain energy metabolism and its role in animal models of depression, bipolar disorder, schizophrenia and autism. Neurosci Lett. 2021;760:136003. doi:10.1016/j.neulet.2021.136003
6. Shao-bo LIU, Ting L-H, Yao GAO, Jun-sheng T, Xue-mei QIN. The key role of mitochondrial energy metabolism disorder in the pathogenesis of depression. Acta Pharma Sin. 2020;55(2):195–200. doi:10.16438/j.0513-4870.2019-0623
7. Visentin APV, Colombo R, Scotton E, et al. Targeting inflammatory-mitochondrial response in major depression: current evidence and further challenges. Oxid Med Cell Longev. 2020;2020:2972968. doi:10.1155/2020/2972968
8. Friedman AK, Walsh JJ, Juarez B, et al. Enhancing depression mechanisms in midbrain dopamine neurons achieves homeostatic resilience. Science. 2014;344(6181):313–319. doi:10.1126/science.1249240
9. Lu -J-J, Wu P-F, He J-G, et al. BNIP3L/NIX-mediated mitophagy alleviates passive stress-coping behaviors induced by tumor necrosis factor-α. Mol Psychiatry. 2023;28(12):5062–5076. doi:10.1038/s41380-023-02008-z
10. Karimian M, Babaei F. Large-scale mtDNA deletions as genetic biomarkers for susceptibility to male infertility: a systematic review and meta-analysis. Int J Biol Macromol. 2020;29(158):85–93. doi:10.1016/j.ijbiomac.2020.04.216
11. Picard M. Blood mitochondrial DNA copy number: what are we counting? Mitochondrion. 2021;60:1–11. doi:10.1016/j.mito.2021.06.010
12. He Y, Tang J, Li Z, et al. Leukocyte mitochondrial DNA copy number in blood is not associated with major depressive disorder in young adults. PLoS One. 2014;9(5):e96869. doi:10.1371/journal.pone.0096869
13. Li T, Lu Z, Wang J, Chen J, Fu H, Mao J. Growth retardation in the course of Fanconi syndrome caused by the 4977-bp mitochondrial DNA deletion: a case report. Children. 2021;8(10):887. doi:10.3390/children8100887
14. Saini SK, McDermott MM, Picca A, et al. Mitochondrial DNA damage in calf skeletal muscle and walking performance in people with peripheral artery disease. Free Radic Biol Med. 2020;160:680–689. doi:10.1016/j.freeradbiomed.2020.09.004
15. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62. doi:10.1136/jnnp.23.1.56
16. First MB. Diagnostic and statistical manual of mental disorders, 5th edition, and clinical utility. J Nerv Ment Dis. 2013;201(9):727–729. doi:10.1097/NMD.0b013e3182a2168a
17. Aral C, Akkiprik M, Kaya H, et al. Mitochondrial DNA common deletion is not associated with thyroid, breast and colorectal tumors in Turkish patients. Genet Mol Biol. 2010;33(1):1–4. doi:10.1590/s1415-47572009005000102
18. Wallace DC, Shoffner JM, Trounce I, et al. Mitochondrial DNA mutations in human degenerative diseases and aging. Biochimica Et Biophysica Acta. 1995;1271(1):141–151. doi:10.1016/0925-4439(95)00021-U
19. Holt IJ, Harding AE, Morgan-Hughes JA. Deletions of muscle mitochondrial DNA in mitochondrial myopathies: sequence analysis and possible mechanisms. Nucleic Acids Res. 1989;17(12):4465–4469. doi:10.1093/nar/17.12.4465
20. Zeviani M, Moraes CT, DiMauro S, et al. Deletions of mitochondrial DNA in Kearns-Sayre syndrome. Neurology. 1998;51(6):1525and8pagesfollowing. doi:10.1212/wnl.51.6.1525-a
21. Celotto AM, Chiu WK, Van Voorhies WA, Palladino MJ. Modes of metabolic compensation during mitochondrial disease using the drosophila model of ATP6 dysfunction. PLoS One. 2011;6.
22. Jonckheere AI, Hogeveen M, Nijtmans LG, et al. A novel mitochondrial ATP8 gene mutation in a patient with apical hypertrophic cardiomyopathy and neuropathy. J Med Genet. 2008;45(3):129–133. doi:10.1136/jmg.2007.052084
23. Rucheton B, Jardel C, Filaut S, et al. Homoplasmic deleterious MT-ATP6/8 mutations in adult patients. Mitochondrion. 2020;55:64–77. doi:10.1016/j.mito.2020.08.004
24. Lan XJ, Yang XH, Mo Y, et al. Deep transcranial magnetic stimulation for treatment-resistant depression: a systematic review and meta-analysis of randomized controlled studies. Asian J Psychiatr. 2024;96:104032. doi:10.1016/j.ajp.2024.104032
25. Cai DB, Qin XD, Qin ZJ, et al. Adjunctive continuous theta burst stimulation for major depressive disorder or bipolar depression: a meta-analysis of randomized controlled studies. J Affect Disord. 2024;346:266–272. doi:10.1016/j.jad.2023.10.161
26. Lan XJ, Cai DB, Liu QM, et al. Stanford neuromodulation therapy for treatment-resistant depression: a systematic review. Front Psychiatry. 2023;14:1290364. doi:10.3389/fpsyt.2023.1290364
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



