Back to Journals » Therapeutics and Clinical Risk Management » Volume 21
The Application of Opacification-Development Ratio Based on CT Scan for Diagnosing Pediatric Chronic Rhinosinusitis
Authors Zhang J , Yang A, Chen T , Cao Y, Lv Q, Xu Y, Liao Z , Chen X, Ye Z, Lai R, Hong H
Received 5 February 2025
Accepted for publication 7 June 2025
Published 13 June 2025 Volume 2025:21 Pages 895—904
DOI https://doi.org/10.2147/TCRM.S520879
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Jun Zhang,1,* Anni Yang,1,* Tengyu Chen,1,* Yufeng Cao,1 Qiliang Lv,1 Yingxiang Xu,1 Zhenpeng Liao,1 Xianzhen Chen,1 Zhongkang Ye,1 Renjie Lai,1 Haiyu Hong1,2
1Department of Otolaryngology, Head and Neck Surgery, The Fifth Affiliated Hospital of Sun Yat-Sen University, Zhuhai, Guangdong Province, People’s Republic of China; 2Allergy Center, the Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, Guangdong Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Haiyu Hong, Department of Otolaryngology, Head and Neck Surgery, Allergy Center, The Fifth Affiliated Hospital of Sun Yat-sen University, 52 of Meihua East Road, Zhuhai, Guangdong, 519000, People’s Republic of China, Tel +8607562528832; +8613823070089, Email [email protected]
Purpose: To investigate the diagnostic potency of the opacification-development ratio (ODR) for pediatric chronic rhinosinusitis based on CT scanning.
Patients and Methods: Children aged 0– 15 years who underwent nasal CT scanning from August 2011 through July 2021 were included in the research. The area under receiver operating characteristic curve (AUC) and predictive value were used to assess the diagnostic accuracy of the ODR and Lund-Mackay score based on CT scanning.
Results: A total of 1820 patients (217 in the positive symptom group and 1603 in the negative symptom group) who underwent CT scanning were included in the study. A significant positive correlation was observed between the ODR and the Lund-Mackay score in all age groups. In children aged 0– 15 years, the AUC of the ODR and the Lund-Mackay score were 0.7970 and 0.7719, respectively (p > 0.05). The optimal cut-off value for the ODR was 25.83, with a sensitivity of 57.14% and a specificity of 94.2%. In contrast, the optimal cut-off value for the Lund-Mackay score was 6.5, with a sensitivity of 6.5% and a specificity of 85.84%. Notably, the ODR score demonstrated significantly superior performance compared to the Lund-Mackay score in children aged 0– 4 years (p < 0.001).
Conclusion: In diagnosing pediatric chronic rhinosinusitis, the use of CT scans is associated with a higher rate of false positives when compared to clinical symptoms. The ODR score based on CT scanning is a valuable diagnostic tool for chronic rhinosinusitis in children aged 0– 11, particularly those aged 0– 4.
Keywords: chronic rhinosinusitis, children, Lund-Mackay score, retrospective study, CT imaging
Introduction
Pediatric rhinosinusitis is a common inflammatory disease of the sinuses during childhood development.1 From 2006 to 2016, the prevalence of acute pediatric rhinosinusitis ranged from 8.28% to 11.0%.2 A recent systematic review reported that the global prevalence of chronic rhinosinusitis in children was estimated at 5.54%.3 Another study found there were 3.7–7.5 million visits per year for chronic rhinosinusitis among patients aged 0 to 20 in the United States. Chronic rhinosinusitis visits were significantly more prevalent than those for acute rhinosinusitis.4 With a high morbidity rate, pediatric chronic rhinosinusitis has a great impact on children’s quality of life, growth, and development, posing a significant burden on public healthcare resources.5 Therefore, the accurate diagnosis of pediatric chronic rhinosinusitis is particularly important.
Endoscopy and CT imaging are important diagnostic tools for chronic rhinosinusitis in children, which are beneficial to the differential diagnosis and pre-operative evaluation.1 Nasal endoscopy has the advantages of visualization, simplicity, and no radiation, but it is hard to ensure all children show adequate compliance. CT scans can provide high-resolution images of bony structures and soft tissue to accurately evaluate the severity and location of sinonasal inflammation in children.6 However, CT scans have a high false-positive rate, as sinonasal mucosal edema is common in children due to respiratory tract infection. Previous studies have shown that more than half of asymptomatic children can also demonstrate increased density in the sinuses based on nasal CT scan imaging, with approximately 19% of patients being completely clinically asymptomatic and 59% being essentially clinically asymptomatic.7,8 If patients have an upper respiratory infection within two weeks, increased sinus density can be observed in up to 87% of patients.9 Quantitative scoring systems such as the Lund-Mackay (LM) score have been used by previous researchers as diagnostic tools to objectively quantify the severity of sinus turbidity.10,11 However, current applications of the LM score are mainly involved in adult subjects and few studies have been conducted on children. Given that the sphenoid and frontal sinuses might be undeveloped in children under 12 years old, it may not be the optimal diagnostic tool for diagnosing pediatric chronic rhinosinusitis.12
To avoid disturbances caused by sinus development in children, some researchers proposed the opacification-development ratio (ODR) for diagnosing pediatric chronic rhinosinusitis.13 The ODR assesses the development and the area of turbidity of sinuses separately, with the ostiomeatal complex and all sinuses considered paired. However, the diagnostic potency of the ODR for pediatric chronic rhinosinusitis has not yet been adequately validated in clinical practice. Thus, this study retrospectively analyzed the CT imaging of children aged 0–15 years, aiming to investigate the diagnostic potency of ODR in nasal CT scans for diagnosing chronic rhinosinusitis in children.
Materials and Methods
Inclusion Criteria
This retrospective study consecutively collected clinical data from children aged 0–15 years from August 1st 2011 to July 31st 2021, who underwent nasal CT scanning with complete clinical data. All children were collected from outpatient clinic in a tertiary hospital. The clinical history of the patients was collected including the patient’s gender, age, year of examination, symptoms, etc. If the child had multiple CT scans, only the first imaging scan was analyzed. Partially missing medical history information would be asked by telephone to the guardians of children. The study was performed in compliance with the principles of the Declaration of Helsinki.
Exclusion Criteria
Children who met at least one of the following criteria were excluded from the trial: 1) failure to provide a complete patient history for various reasons; 2) having functional endoscopic sinus surgery previously; 3) cancellation of the examination for any reason; 4) children with severe syndromes or malformations in nasal cavity and 5) lack of compliance or excessive CT image artifacts.
Outcomes
Patients who met the diagnostic criteria for chronic rhinosinusitis in children in European Position Paper on Rhinosinusitis and Nasal Polyps 2020 (EPOS 2020) were included in the positive symptom group and the rest in the negative symptom group. Specifically, it was defined as the presence of two or more symptoms one of which should be either nasal blockage / obstruction / congestion or nasal discharge for ≥ 12 weeks, which could be accompanied by facial pain/pressure or/and cough.1 Positive result in CT imaging was defined as 1) partially or completely opaque lesions in the nasal cavity and sinuses; 2) irregular thickening of the sinus mucosa; 3) the presence of air-liquid flatness in the sinus on CT images; and 4) intact sinus walls without bony destruction, which may be thickened or thinned. It is worth mentioning that participants in the negative symptom group might have suffered from other diseases, eg, traumatic head injury or nasal bone fracture, therefore receiving a CT scan. Clinical information and results were not available to the performers and assessors. For ODR scoring, each sinus is given a development score of three if it was present, and a score of zero if it was not present. If all sinuses are developed, the sum of the five sites (frontal, ethmoid, sphenoid, maxillary sinuses, and OMC) on each side can be scored up to 15 points (a total of 30 points). The area scored from zero to three based on the turbidity (normal = 0 points; < 2/3 = 1 point; ≥ 2/3 = 2 points; completely turbid = 3 points). If the OMC was normal it was scored as zero, and if the OMC was turbid it was scored as three. The ODR was calculated as “(sum of bilateral turbidity scores/sum of bilateral development scores) × 100”.
Statistical Analysis
The diagnostic potency of the LM score and ODR for the diagnosis of pediatric chronic rhinosinusitis was assessed using the receiver operating characteristic curve (ROC). The diagnostic potency of the LM score and ODR was assessed by area under receiver operating characteristic curve (AUC), where 0.50 < AUC ≤ 0.70 suggests low predictive value, 0.70 < AUC ≤ 0.90 moderate predictive value, and AUC > 0.90 high predictive value. The optimal cut-off value was calculated by choosing the maximum Youden index to predict whether the LM score and ODR could be used as the diagnostic criteria for diagnosing pediatric chronic rhinosinusitis. The study was statistically analyzed using SPSS 26.0 (SPSS Inc., Chicago, IL) and GraphPad Prism 8 (GraphPad, La Jolla, CA). Data were expressed as mean ± standard deviation. Unpaired Student’s t-test was used for two-group data. Categorical variables were analyzed using the square-chi test. All statistical methods were considered statistically significant when p < 0.05.
Results
Basic Characteristics of Included Patients
This study initially included 2021 patients. After excluding patients with incomplete medical history, a total of 1820 patients remained in this study. The distribution of age of patients is shown in Figure S1. There were 1265 (69.51%) male patients and 555 (30.49%) female patients, with no statistically significant difference in gender composition (p = 0.512). Among 1820 patients, a total of 217 (11.92%, 217/1820) met the diagnostic criteria for pediatric chronic rhinosinusitis according to EPOS 2020 and were included in the positive symptom group, while the remaining 1603 patients without nasal symptoms were included in the negative symptom group. There was a statistically significant difference in age between patients from these two groups (p < 0.001). There was no statistically significant difference in the percentage of patients in the positive symptom group and negative symptom group who demonstrated positive imaging on CT scan (p = 0.183) (Table 1).
 |
Table 1 The Demographic Features of Included Patients |
Diagnostic Rate of CT Scans
The sensitivity of CT scanning for diagnosing pediatric chronic rhinosinusitis is 67.28%, the specificity is 37.37%, the false-positive rate is 62.63%, and the false-negative rate is 32.72% (Table 2). The diagnosis rate of CT scans in different age groups was significantly higher than the pediatric chronic rhinosinusitis incidence rate (p < 0.001). The incidence rate of pediatric chronic rhinosinusitis gradually increased with age, while the diagnosis rate of CT scans gradually decreased with age. However, the diagnosis rate of CT scans was still significantly higher than the incidence rate of pediatric chronic rhinosinusitis in all age groups (p < 0.001) (Figure 1a). The incidence rate of pediatric chronic rhinosinusitis in each season was significantly lower than that of CT scan diagnosis (p < 0.001), and there was no statistically significant difference in the diagnosis rate of CT scan and incidence rate of pediatric chronic rhinosinusitis among different seasons (p > 0.05) (Figure 1b).
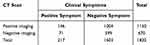 |
Table 2 Diagnosis of Pediatric Chronic Rhinosinusitis Based on Clinical Symptoms and CT Scan |
Lund-Mackay Score and ODR Based on Nasal CT Scan
The LM score was 8.39 ± 5.63 in the positive symptom group and 3.49 ± 3.01 in the negative symptom group. The LM score in the positive symptom group was statistically significantly higher than in the negative symptom group (p < 0.001) (Figure 2a). The difference in LM scores between the positive and negative symptom groups was statistically significant (p < 0.001) (Figure 2a). The ROC curve was used to explore the diagnostic potency of the CT scan-based LM score for the diagnosis of pediatric chronic rhinosinusitis. The AUC of the CT scan-based LM score was 0.7719 (95% CI: 0.7339–0.8100, p < 0.001). When its cut-off value is 6.5, the best diagnostic performance can be achieved, with a sensitivity of 59.91%, a specificity of 85.84%, and a Youden index of 0.4575 (Figure 2b).
The ODR of the positive and negative symptom groups were 29.84 ± 21.52 and 10.21 ± 8.80, respectively. The ODR of the positive symptom group was significantly higher than the negative symptom group, with a statistically significant difference (p < 0.001) (Figure 3a). The AUC of ODR based on CT scan was 0.7970 (95% CI: 0.7594–0.8347, p < 0.001), with an optimal cutoff value of 25.83, a sensitivity of 57.14%, a specificity of 94.2%, and a Youden index of 0.5134 (Figure 3b).
Diagnostic Accuracy in Different Age Groups
For children aged 0–4 years and 5–11 years, the diagnostic potency of the ODR was superior to that of the LM score statistically significantly (p < 0.05). For children aged 0–4 years, the ODR had the best diagnostic potency, with an AUC of 0.9109, a cutoff value of 25.83, a sensitivity of 84.85% and a specificity of 90.08%, and a Youden index of 0.7493. The AUC of the LM score was 0.7711, with a sensitivity of 78.79%, a specificity of 65.19%, and a Youden index of 0.4398. The diagnostic potency of the ODR was significantly better than that of the LM score statistically significantly (p < 0.001) (Table 3, Figure 4b, Figure 4c). For children aged 12–15 and 0–15, the diagnostic potency of ODR and LM score for pediatric chronic rhinosinusitis was not significantly different (p > 0.05) (Table 3, Figure 4a, Figure 4d).
 |
Table 3 Diagnostic Potency of ODR and Lund-Mackay Score in Children with Chronic Rhinosinusitis of All Ages |
Correlation Between ODR and Lund-Mackay Score in Different Age Groups
The ODR was positively correlated with the LM score significantly in the 0–15, 0–4, 5–11, and 12–15 age groups (r = 0.85, 0.80, 0.85, 0.90, respectively) (Table 4, Figure 5).
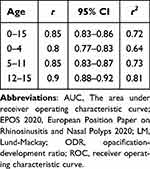 |
Table 4 Correlation Between ODR and Lund-Mackay Score in Different Age Groups |
Discussion
The LM scoring system is an objective method for quantifying CT-based sinus imaging, widely adopted for clinical assessment of the severity and therapeutic effects of rhinosinusitis.14 Studies have indicated that the LM scoring system may provide a more accurate assessment of disease severity than other scales.15–17 Bhattacharyya et al found when the cut-off value of the LM score was greater than two in the diagnosis of chronic rhinosinusitis, the sensitivity was 94%, and the specificity was 41%; when the cut-off value was greater than 4, the specificity increased to 59%.15,18 However, it should be noted that previous studies about the LM score are predominantly involved with adults rather than children. Some researchers have shown that in children, when the LM score cut-off value was greater than 5, the sensitivity would be 86% and the specificity 85%. A LM score of ≤ 2 is indicative of a favorable negative predictive value, while a score of ≥ 5 is associated with a favorable positive predictive value, strongly suggesting the diagnosis of pediatric chronic rhinosinusitis.18
In this study, it was found that among children aged 0–15 years, the LM score shows limited diagnostic potency for pediatric chronic rhinosinusitis. Given that LM scores are integers, a score of ≥ 7 is more likely indicative of a confirmed diagnosis of pediatric chronic rhinosinusitis. The limited diagnostic utility of the LM score for pediatric chronic rhinosinusitis in this study may be due to the scoring system’s assignment of a single point for any degree of opacification. This approach gives equal weight to the presence of fluid in sinuses and mucosal thickening, which are two distinct conditions that lead to divergent clinical outcomes. Moreover, previous research on the LM scoring system was predominantly conducted in adult populations, failing to consider the common lack of sphenoid and frontal sinus development in children under 12 years old.12 The LM scoring system, which relies on the cumulative score from each sinus, inherently reduces the score range from 24 to 16 points in the absence of developed sphenoid and frontal sinuses. This discrepancy may result in a systematic underestimation of disease severity, thereby introducing errors in the diagnostic assessment of pediatric chronic rhinosinusitis.
Araújo Neto et al have proposed the ODR scoring system to decrease the confounding effects of children’s sinus development.13 The ODR evaluates the percentage of the opacified area relative to the developmental area of the sinus. In comparison to the LM scoring system, the ODR is less susceptible to the quantity and extent of sinus development, potentially leading to enhanced accuracy in diagnosing and assessing the severity of pediatric chronic rhinosinusitis. However, the diagnostic potency of the ODR has not yet been fully validated in patients with pediatric chronic rhinosinusitis. In this study, the ODR demonstrated superior performance in terms of the Youden Index and specificity for pediatric chronic rhinosinusitis compared to the LM score in patients aged 0–15. However, its sensitivity was inferior to that of the LM scoring system, with no statistically significant difference between the two scores. These results may therefore indicate that the diagnostic potency of the ODR for pediatric chronic rhinosinusitis is not superior to that of the LM score for children aged 0–15. Previous related research indicates that the development of sinus groups has temporal characteristics, with certain heterogeneity in the development of sinus groups among children of different age groups, which might be an important reason for the results. Therefore, we further categorized patients into different age groups to compare the diagnostic potency of the ODR and the LM score for pediatric chronic rhinosinusitis among different age groups.
Studies have shown that the maxillary and ethmoid sinuses are developed at birth; in contrast, the frontal sinuses are not yet developed in children aged 0–4 years, while the ethmoid sinuses are gradually aerated by the age group of 1–4 years; sphenoid and frontal sinuses are fully aerated by the age of 12.19,20 Considering the impact of varying sinus development stages on the diagnosis of pediatric chronic rhinosinusitis, we divided patients into three age groups: 0–4 years, 5–11 years, and 12–15 years. Then, we compared and validated the ODR and LM scores among these age groups, analyzing their diagnostic potency in the clinical diagnosis of pediatric chronic rhinosinusitis across age ranges.
The diagnostic potency of the ODR is significantly higher than that of the LM score in children aged 0–4 years. Similar results were observed in the age group of 5–11 years. The specificity and sensitivity of the ODR are significantly higher than those of the LM score, indicating that in children aged 5–11 years, the diagnostic potency of the ODR is superior to that of the LM score. At the optimal cut-off value, the sensitivity of the ODR in children aged 5–11 years was comparable to that of the LM score, but the specificity of the ODR was markedly higher than that of the LM score. This suggests that an ODR of 21.67 or lower more strongly indicates a negative diagnosis of pediatric chronic rhinosinusitis. For children aged 12–15 years, the AUC of the ODR was 0.8001, which was slightly smaller than that of the LM score (0.8116), with no statistically significant difference. Compared to the LM score, the ODR exhibited greater sensitivity yet showed a reduction in specificity. However, the difference between the ODR and the LM score was not statistically significant. Therefore, the diagnostic potency of both scoring systems is comparable in children aged 12–15 years. As patient ages increase, the AUC for the LM score shows a corresponding increase. This trend reveals that the LM score is less effective in diagnosing pediatric chronic rhinosinusitis in younger patients and more effective in older individuals. The discrepancy in diagnostic potency between the ODR and the LM score for pediatric chronic rhinosinusitis among different ages can likely be attributed to the distinctive temporal patterns of sinus development. Specifically, children under the age of 12 possess underdeveloped sphenoid and frontal sinuses. Furthermore, the oversimplified method employed by the LM scoring system in evaluating sinus opacification could inadvertently underestimate the disease severity. The development process of pediatric sinuses plays a critical role in determining the accuracy of the diagnosis of pediatric chronic rhinosinusitis using the LM score. In contrast, the ODR, which calculates the percentage of opacified area relative to the total developed sinus area, is less susceptible to variations in the quantity of sinus development. Consequently, the findings indicate that for the age groups of 0–4 and 5–11 years, the diagnostic utility of the ODR is superior to that of the LM score. However, in children aged 12–15 years, the diagnostic potency of the two scoring systems proves to be similarly effective.
The findings of the present investigation demonstrate a consistent correlation between ODR and LM scores across diverse age groups. However, this correlation exhibits age-dependent variability, being weaker among younger cohorts and more pronounced in older ones, with the least strength observed in children aged 0–4 years. It can be concluded that the ODR may be a more viable diagnostic tool for younger children, whereas the LM score appears to be more suitable for older individuals. As young children are less able to describe their symptoms, the ODR can help clinicians identify children with suspected CRS earlier.
Although pediatric sinus staging systems have been reported previously, their scoring systems are complex, and further studies are required to validate the diagnostic potency of pediatric sinus staging systems.21 In clinical practice, a scoring system would be widely utilized when it is simple, clear, highly accurate, and easy to implement. This study demonstrates the accessibility of the ODR and its significant utility for the diagnosis of chronic rhinosinusitis in children aged 0–11 years, with a particularly pronounced diagnostic potency in children aged 0–4. Although we performed a single-center and low-sample-size study, future application of the ODR might further enhance the specificity and sensitivity of CT scan-based diagnoses of pediatric chronic rhinosinusitis.
This study retrospectively applied the ODR score to children who underwent CT imaging, aiming to enhance the diagnosis of chronic rhinosinusitis in children. However, it does not imply that CT imaging should be used for all children suspected of having pediatric chronic rhinosinusitis. The primary objective of this study is to identify occult chronic rhinosinusitis in young children who have undergone CT imaging for other reasons, ensuring they receive standardized treatment as early as possible. Clinicians find it more challenging to assess their symptoms, and the ODR based on CT imaging findings can aid in improving the diagnosis of pediatric chronic rhinosinusitis.
There are limitations in the study. Firstly, only children under the age of 15 were included in this study. Therefore, the conclusions might not be necessarily applicable to adolescents aged 15 to 18. Secondly, during the case screening, we followed up with parents of children with partially missing medical history information by telephone to ask about previous symptoms and to determine whether the child met the inclusion criteria. However, there were still a very small number of children whose parents could not be contacted. It might miss some potential patients who met the inclusion criteria, leading to a study bias. Additionally, a large age difference between the two groups might cause confounding bias for the results of the study. Furthermore, as a retrospective study, the results need to be further verified in prospective cohorts in the future. Finally, ODR is a score based on CT imaging features, which cannot directly reflect clinical symptoms. Therefore, it still needs to be combined with clinical symptoms to diagnose CRS.
Conclusion
The ODR based on CT scan is not only user-friendly but also shows substantial diagnostic potential for chronic rhinosinusitis in children aged 0–11 years. The utilization of the ODR significantly improves the diagnostic precision of chronic rhinosinusitis in the 0-4-year age range.
Data Sharing Statement
Further enquiries about original data can be directed to the corresponding author.
Ethics Approval and Informed Consent
Ethical approval for this study was obtained from the Ethics Committee of the Fifth Affiliated Hospital of Sun Yat-sen University (2021-K74-1). Due to the retrospective nature of the study and no identifying information in CT imaging, informed consent in this study was waived by the Ethics Committee of the Fifth Affiliated Hospital of Sun Yat-sen University.
Acknowledgments
We would acknowledge all the participants included in our study.
Funding
This study was supported by the National Natural Science Foundation of China (grant No. 82071018), Natural Science Foundation of Guangdong Province, China (grant No. 2025A1515012592), and Foundation of Science and Technology of Shenzhen City (JCYJ20210324112607020).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fokkens WJ, Lund VJ, Hopkins C, et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology. 2020;58(Suppl S29):1–464. doi:10.4193/Rhin20.401
2. Levy DA, Pecha PP, Nguyen SA, Schlosser RJ. Trends in complications of pediatric rhinosinusitis in the United States from 2006 to 2016. Int J Pediatr Otorhi. 2020;128:109695. doi:10.1016/j.ijporl.2019.109695
3. Min HK, Lee S, Kim S, et al. Global incidence and prevalence of chronic rhinosinusitis: a systematic review. Clin Exp Allergy. 2025;55(1):52–66. doi:10.1111/cea.14592
4. Gilani S, Shin JJ. The burden and visit prevalence of pediatric chronic rhinosinusitis. Otolaryng Head Neck. 2017;157(6):1048–1052. doi:10.1177/0194599817721177
5. Cheng BT, Smith SS, Fishbein AB. Functional burden and limitations in children with chronic sinusitis. Pediat Allerg Imm-Uk. 2020;31(1):103–105. doi:10.1111/pai.13121
6. Greguric T, Prokopakis E, Vlastos I, et al. Imaging in chronic rhinosinusitis: a systematic review of MRI and CT diagnostic accuracy and reliability in severity staging. J Neuroradiol. 2021;48(4):277–281. doi:10.1016/j.neurad.2021.01.010
7. Pransky SM, Low WS. Pediatric ethmoidectomy. Otolaryngol Clin North Am. 1996;29(1):131–142. doi:10.1016/S0030-6665(20)30421-7
8. Diament MJ, Senac MJ, Gilsanz V, Baker S, Gillespie T, Larsson S. Prevalence of incidental paranasal sinuses opacification in pediatric patients: a CT study. J Comput Assist Tomogr. 1987;11(3):426–431. doi:10.1097/00004728-198705000-00011
9. Lusk RP, McAlister B, El Fouley A. Anatomic variation in pediatric chronic sinusitis: a CT study. Otolaryng Clin N Am. 1996;29(1):75–91. doi:10.1016/S0030-6665(20)30417-5
10. Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg. 1997;117(3):. doi:10.1016/S0194-59989770005-6.
11. Okushi T, Nakayama T, Morimoto S, et al. A modified Lund-Mackay system for radiological evaluation of chronic rhinosinusitis. Auris Nasus Larynx. 2013;40(6):548–553. doi:10.1016/j.anl.2013.04.010
12. Hopkins C, Browne JP, Slack R, Lund V, Brown P. The Lund-Mackay staging system for chronic rhinosinusitis: how is it used and what does it predict? Otolaryng Head Neck. 2007;137(4):555–561. doi:10.1016/j.otohns.2007.02.004
13. Araújo Neto SAD, Baracat ECE, Felipe LF. A new score for tomographic opacification of paranasal sinuses in children. Braz J Otorhinolar. 2010;76(4):491–498. doi:10.1590/S1808-86942010000400014
14. Ashraf N, Bhattacharyya N. Determination of the “incidental” Lund score for the staging of chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2001;125(5):483–486. doi:10.1067/mhn.2001.119324
15. Chavan A, Maran R, Meena K. Diagnostic evaluation of chronic nasal obstruction based on nasal endoscopy and CT scan paranasal sinus. Indian J Otolaryngol Head Neck Surg. 2019;71(Suppl 3):1948–1952. doi:10.1007/s12070-018-1376-6
16. Bhattacharyya N. A comparison of symptom scores and radiographic staging systems in chronic rhinosinusitis. Ame J Rhinol. 2005;19(2):175–179. doi:10.1177/194589240501900210
17. Bhattacharyya N. Relationship between mucosal inflammation, computed tomography, and symptomatology in chronic rhinosinusitis without Polyposis. Ann Otol Rhinol Laryngol. 2008;117(7):517–522. doi:10.1177/000348940811700709
18. Bhattacharyya N, Fried MP. The accuracy of computed tomography in the diagnosis of chronic rhinosinusitis. Laryngoscope. 2003;113(1):125–129. doi:10.1097/00005537-200301000-00023
19. Goldman-Yassen AE, Meda K, Kadom N. Paranasal sinus development and implications for imaging. Pediatr Radiol. 2021;51(7):1134–1148. doi:10.1007/s00247-020-04859-y
20. Weiglein A, Anderhuber W, Wolf G. Radiologic anatomy of the paranasal sinuses in the child. Surg Radiol Anat. 1992;14(4):335–339. doi:10.1007/BF01794761
21. Melder K, Shaffer A, Govil N, Stapleton A. The pediatric sinus staging system: a computed tomography-based approach to grading pediatric sinus disease. Laryngoscope. 2021;131(2):E642–E648. doi:10.1002/lary.28752
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.