Back to Journals » Vascular Health and Risk Management » Volume 21
The Association Between Sarcopenia Index and Aortic Valve Sclerosis in Coronary Artery Disease Patients: Insights from a Retrospective Cross-Sectional Analysis and Animal Models
Authors Zhang Y, Chen H, Chen Z, Du X, Chen J, Aikebaier M, Shan S, Yang L, Zhao A, Wang Y, Liu Y, Yang K
Received 4 February 2025
Accepted for publication 10 May 2025
Published 16 May 2025 Volume 2025:21 Pages 391—401
DOI https://doi.org/10.2147/VHRM.S520000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Daniel Duprez
Yifeng Zhang,1,* Hui Chen,2,* Zhongli Chen,3,* Xihao Du,4 Jiawei Chen,2 Mirenuer Aikebaier,1 Shuyao Shan,1 Ling Yang,2 Anqi Zhao,2 Yanping Wang,2 Yehong Liu,5 Ke Yang1
1Department of Cardiovascular Medicine, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People’s Republic of China; 2Department of Cardiology, Shanghai Ninth People’s Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, People’s Republic of China; 3State Key Laboratory of Cardiovascular Disease, Cardiac Arrhythmia Center, Fuwai Hospital, National Center for Cardiovascular Disease, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People’s Republic of China; 4Department of Epidemiology and Biostatistics, School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 5Department of Cardiology, Shanghai East Hospital Tongji University School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ke Yang, Department of Cardiovascular Medicine, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, No. 197 Ruijin second Road, Shanghai, 200025, People’s Republic of China, Email [email protected] Yehong Liu, Department of Cardiology, Shanghai East hospital Tongji University School of Medicine, No. 150 Jimo Road, Shanghai, 200120, People’s Republic of China, Email [email protected]
Background: The Sarcopenia Index (SI) is a recognized predictor of cardiovascular risk in patients with coronary artery disease (CAD), yet its association with aortic valve sclerosis (AVSc) remains insufficiently studied. This study aimed to examine the relationship between SI and AVSc in CAD patients.
Methods: In this retrospective study, 1056 CAD patients at Shanghai Ruijin Hospital underwent SI assessment and Doppler echocardiography. SI was calculated as [serum creatinine (mg/dL)/cystatin C (mg/L)] × 100. Logistic regression, subgroup analyses, and restricted cubic splines evaluated the SI-AVSc association. ROC curves determined SI’s diagnostic value and its addition to traditional AVSc factors. In parallel with clinical observations, aortic valve changes were analyzed in mice via hematoxylin and eosin, AlizarinRed S, and Masson’s trichrome to assess valve thickness, fibrosis and calcification.
Results: Patients with the lowest SI levels showed a higher prevalence of AVSc. Multivariate logistic regression revealed that SI was independently associated with AVSc (P< 0.001). The C-statistic for SI in identifying AVSc was 0.708 (95% CI: 0.671, 0.744), and it improved risk stratification when SI was added to traditional clinical models (C-statistic increased from 0.840 to 0.866). In the subgroup analysis, the discriminatory power of SI was enhanced among elderly patients. Findings from animal models supported these results, and Spearman correlation analyses revealed negative correlation between SI and peak systolic aortic valve flow velocity (Spearman’s rho=− 0.578, P=0.006). Histological analysis demonstrated that aortic valve leaflets in the low SI group were thicker and more fibrotic than those in the high SI group, and this complementary approach provided mechanistic insights into how sarcopenia may promote valve degeneration in elder mice.
Conclusion: Lower Sarcopenia Index is associated with the presence of AVSc in CAD patients. SI improves risk stratification and acts as a valuable associated marker for AVSc, emphasizing its potential clinical utility in enhancing patient management.
Keywords: sarcopenia index, aortic valve sclerosis, coronary artery disease
Introduction
Coronary artery disease (CAD) remains a leading cause of morbidity and mortality among older adults.1 Aortic valve sclerosis (AVSc), defined by thickening and/or calcification of the aortic valve without significant obstruction to blood flow, affects approximately 30% of individuals over the age of 65.2,3 Epidemiological studies have shown that the prevalence of AVSc increases with age and that it serves as a valuable marker of systemic atherosclerotic burden.4 Early detection of AVSc has important clinical implications, potentially improving disease management strategies in practice.5 However, aside from echocardiography, there are few biomarkers available for identifying AVSc.
Sarcopenia, a progressive condition characterized by the gradual loss of skeletal muscle mass and function, progresses at a rate of 0.5% to 1% per year starting in middle age, with acceleration beyond 60 years.6 Notably, CAD has been found to accelerate the progression of sarcopenia even in relatively young patients.7 The Sarcopenia Index (SI), calculated as [serum creatinine (mg/dL)/cystatin C (mg/L)] × 100, has been proposed as a novel marker for assessing sarcopenia.8 Recent studies have confirmed the prognostic value of SI in CAD patients undergoing invasive procedures.9 Given that AVSc and sarcopenia share key pathophysiological mechanisms driving their progression and increasing cardiovascular risk, the interplay between these conditions in the context of CAD represents a critical area of research.10,11 Understanding this interaction may provide promising opportunities for improving prognostic accuracy in CAD management.
Despite the recognized importance of AVSc and sarcopenia in CAD, most existing studies focus on their independent prognostic roles. However, there is a lack of research investigating the combined associated value of the SI for AVSc in CAD patients. This study aims to evaluate the prognostic significance of the SI in predicting the development of aortic valve sclerosis in patients with coronary artery disease. Specifically, it will assess the predictive value of SI for the presence of AVSc in CAD patients.
Methods
Study Design and Populations
In this retrospective study, 3053 patients diagnosed with CAD via coronary computed tomography angiography or conventional coronary angiography were recruited from the Department of Cardiovascular Medicine at Shanghai Ruijin Hospital between January 2020 and January 2021. Among these, 2852 patients underwent standard transthoracic echocardiography. The study excluded individuals based on the following criteria: absence of creatinine or cystatin C data (n=380), acute coronary syndrome (n=366), an estimated glomerular filtration rate (eGFR) below 30 mL/min per 1.73 m² (n=87), severe heart failure (New York Heart Association class III or IV, or left ventricular ejection fraction <30%) (n=281), rheumatic disease (n=96), valvular stenosis (n=59), congenital aortic valve malformation (n=52), prior aortic valve replacement (n=46), thyroid or parathyroid disorders (n=184), chronic immobilization (n=86), and cancer (n=124). Additionally, 35 patients declined participation. Consequently, 1056 patients were included in the final analysis (Figure 1). The study protocol was approved by the Ethics Committee of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, and all participants provided written informed consent. This study complies with the Declaration of Helsinki.
 |
Figure 1 Flowchart of patient enrollment. |
Definitions and Measurements
Function and morphology of aortic valve was measured by echocardiograph. Peak and mean velocity across the aortic valve were calculated using the modified Bernoulli equation, with continuous-wave Doppler.12 AVSc was characterized by the presence of aortic valve leaflets that showed localized areas of slight thickness or enhanced echogenicity, without any associated limitation in mobility or a peak flow velocity surpassing 2.0 m/s across the aortic valve.13,14 As ESC recommends, hypertension is defined as systolic blood pressure (SBP) of ≥140 mmHg and/or diastolic blood pressure (DBP) of ≥90 mmHg measured on at least three occasions in two separate places, or the use of any antihypertensive medication.15 Diabetes is characterized by a fasting blood glucose level equal to or greater than 7.0 mmol/L, or a post-load blood glucose level equal to or greater than 11.1 mmol/L, or the administration of antidiabetic medications.16 CAD was identified by the American College of Cardiology/American Heart Association lesion classification scheme, and involved a luminal diameter stenosis of at least 50% in one or more major epicardial coronary arteries.17 The calculation of the SI was performed utilizing the following formula: [Serum creatinine (mg/dL)/Cystatin C (mg/L)]×100.8
Animals and Experiments
The experimental and animal protocols adhered to the guidelines set forth by the Guide for the Care and Use of Laboratory Animals and received approval from the animal care and use committee at Shanghai Jiao Tong University, China. These protocols also complied with Directive 2010/63/EU from the European Parliament concerning the protection of animals used for scientific purposes.
Male SPF-grade C57BL/6 mice, aged six weeks, were procured from Beijing Vital River Laboratory Animal Products Co. Ltd., China. These mice were housed at a temperature of 25±1°C with 65±5% humidity, and under a 12-hour light/dark cycle in the animal facility of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine. All studies observed the 3R principles of reduce, reuse, and recycle.
During the experiments, 20 male C57BL/6 mice were conventionally fed for 78 weeks to simulate natural aging. At the end of the protocol, the mice fasted overnight for echocardiography assessment. A Vevo 2100 (FujiFilm Visual Sonics) with an MS-400 imaging transducer was employed for two-dimensional echocardiography of cardiac and aortic valve function. Following the echocardiogram, the mice were subjected to anesthesia and subsequently euthanized by inhaling isoflurane followed by an intraperitoneal injection of pentobarbital sodium at a dosage of 30 mg/kg of body weight. Hearts were collected, and blood samples were extracted to measure fasting glucose levels, blood lipid profile, C-reactive protein, creatinine, and blood calcium and phosphorus levels. Cystatin C concentration was measured by a commercial ELISA kit (Cat# KE10066, Proteintech, USA).
Immunohistochemistry
The harvested hearts were immersed in a 4% paraformaldehyde solution for 12 hours to ensure proper fixation, then embedded in a medium suitable for optimal cutting at low temperatures. The tissues were sectioned into 6 μm-thick slices for frozen section histology. For comprehensive histological examination, these sections were stained with hematoxylin and eosin, AlizarinRed S, and Masson’s trichrome. Images of the stained sections were captured using an Olympus BX61TRF microscope (Tokyo, Japan) and analyzed quantitatively with ImageJ software (National Institutes of Health, Bethesda, MD).
Statistical Analysis
Continuous variables are presented as means ± standard deviations (SD) for normally distributed data or as medians with interquartile ranges (IQRs) for non-normally distributed data, while categorical variables are expressed as proportions and frequencies. Comparative analyses of continuous variables were performed using the one-way analysis or Kruskal–Wallis test, and χ²-tests were used for categorical variables. In the logistic regression models, the SI was analyzed both as a continuous variable in 10-unit increments and as an ordinal variable divided into tertiles, with the lowest tertile serving as the reference category. A multivariable logistic regression analysis was conducted to evaluate the independent diagnostic significance of SI in identifying AVSc. Model 1 adjusted for demographic information including age and gender, model 2 adjusted for covariates that were significantly meaningful in the baseline table, model 3 adjusted for covariates, which may influence the process of AVSc in previous study.5,18,19 All variations were examined multicollinearity by calculating variance inflation factors (VIFs). Hosmer–Lemeshow test was used to test the goodness of fit metrics. Receiver operating characteristic (ROC) curves were generated to assess the effectiveness of SI in distinguishing AVSc across the study cohort, with the optimal SI cutoff determined by the highest Youden index (sensitivity + specificity – 1). C-statistics and their 95% confidence intervals (CIs) were reported. The incremental benefit of adding SI to the conventional diagnostic model was evaluated using C-statistics, net reclassification improvement (NRI) index, and integrated discrimination improvement (IDI) index. Additionally, restricted cubic splines were used to explore potential nonlinear associations between SI and AVSc, with knots placed at the 5th, 35th, 65th, and 95th percentiles of SI for a smoothly integrated graph. In animal studies, Spearman correlation analyses were conducted to examine the relationship between SI and peak systolic aortic valve flow velocity. All statistical analyses were performed using SPSS version 26.0 or R version 4.4.1, with statistical significance set at P < 0.05.
Results
Baseline Clinical Characteristics
This study involved 1056 stable CAD patients (Figure 1). The baseline characteristics of the participants are shown in Table 1. Patients with the lowest SI level tended to be older, included a smaller proportion of males, and had higher systolic blood pressure (all P<0.05). Additionally, patients with the lowest SI level had a higher prevalence of AVSc (Figure 2).
 |
Table 1 Baseline Characteristics of CAD Patients According to SI Levels |
 |
Figure 2 The proportion of AVSc among CAD patients divided by tertile of SI level. |
Association Between SI and AVSc
In logistic regression analysis, each 10-unit increase in SI was significantly associated with a reduced incidence of AVSc [OR = 0.598 (95% CI: 0.539, 0.664), P < 0.001, Table 2]. This inverse relationship remained consistent after adjusting for demographic, clinical, and laboratory confounders in Model 3 [OR = 0.580 (95% CI: 0.500, 0.673), P < 0.001, Table 2]. Moreover, when SI was divided into tertiles, patients in the second and third tertiles exhibited a lower incidence of AVSc compared to those in the first tertile after adjusting for the same confounders [Tertile 2: OR = 0.390 (95% CI: 0.253, 0.603), P < 0.001; Tertile 3: OR = 0.228 (95% CI: 0.139, 0.374), P < 0.001, Table 2]. Besides, all variations were examined multicollinearity by calculating variance inflation factors (VIFs), which were both less than 5 (Table S1), and the goodness of fit of logistic regression model was evaluated by Hosmer–Lemeshow test to ensure the accuracy of the estimated probabilities (p=0.644). To fully explored the potential residual impact of confounding factors, the role of SI in discriminating AVSc among different subgroups was performed (Figure 3). Notably, this association was particularly significant in individuals aged ≥65 years (p<0.001, p for interaction = 0.002).
 |
Table 2 Association Between SI Level and AVSc |
Performance of SI for Discrimination of AVSc
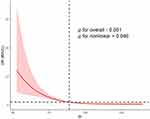
Restricted cubic spline analysis with a multivariate logistic regression model revealed an inverse relationship between the SI and the incidence of AVSc (P < 0.001 for overall association; P = 0.046 for nonlinear; Figure 4). To assess the discriminative ability of SI levels for AVSc, ROC analysis was conducted, yielding a C-statistic of 0.708 (95% CI: 0.671, 0.744) with an optimal cutoff value of 85.26 (Figure S1) (sensitivity: 0.697, specificity: 0.642, Table S2) across the total cohort. Moreover, incorporating SI into the clinical traditional model significantly improved AVSc discrimination, increasing the C-statistic from 0.840 (95% CI: 0.814, 0.866) to 0.866 (95% CI: 0.841, 0.892). This enhancement was further supported by a category-free net reclassification improvement (NRI) of 0.597 (95% CI: 0.466, 0.728, P < 0.001) and an integrated discrimination improvement (IDI) of 0.064 (95% CI: 0.048, 0.081, P < 0.001, Table 3). Subgroup analysis by age indicated that SI exhibited a discriminative power for AVSc in elder patients compared to younger ones, with C-statistics of 0.742 (95% CI: 0.700, 0.784) versus 0.583 (95% CI: 0.494, 0.672), respectively (Figure 5), and with high sensitivity of 0.724, specificity of 0.675 in elder group (Table S2).
 |
Table 3 Performance of SI in Improving Diagnosis of AVSc |
 |
Figure 5 Diagnostic value of SI for AVSc in different subgroups. Abbreviations: SI, sarcopenia index; AVSc, aortic valve sclerosis. |
Decreased SI Level Promoted Pathological Change of Aortic Valve Sclerosis in Mice
To investigate the role of SI in regulating aortic valve sclerosis, aged mouse model was developed. SI was measured in these mice, which were then categorized into high (n=10) and low (n=10) SI groups, with baseline information provided in Table S3. The study revealed a significant inverse relationship between SI levels and aortic valve sclerosis. Mice in the low SI group exhibited markedly higher peak systolic aortic valve flow velocity compared to the high SI group (Figure 6A and B). This relationship was further explored by a negative correlation between SI levels and peak systolic aortic valve flow velocity (Spearman’s rho=−0.578, P=0.006, Figure 6C). Histological analysis demonstrated that aortic valve leaflets in the low SI group were thicker and more fibrotic than those in the high SI group (Figure 6D and F). Moreover, calcification foci were observed exclusively in the low SI group (3 cases) and were absent in the high SI group (Figure 6G). These findings suggest that change of SI may influence the progression of aortic valve sclerosis and calcification in aged mice, potentially offering new insights into the pathogenesis and prevention of this condition.
Discussion
In this study, we examined the relationship between the SI and AVSc in patients with CAD. Our results indicated that a lower SI was associated with a higher prevalence of AVSc, independent of traditional risk factors. The SI exhibited discriminatory power for AVSc, and its addition in clinical traditional models improved risk prediction. Supporting these clinical findings, an aged mouse model demonstrated that a lower SI was associated with increased aortic valve thickness, fibrosis, and calcification. Thus, the sarcopenia index may serve as a valuable marker for predicting AVSc in patients with CAD.
The present study highlights that patients with lowest SI level had a higher prevalence of AVSc in patients with CAD. Additionally, patients with lowest SI level tended to be older, less proportion of male, and had a higher systolic blood pressure. The findings are consistent with previous research that has identified age and hypertension as common risk factors for both AVSc and sarcopenia,11,20 suggesting that AVSc and sarcopenia may exhibit overlapping pathways. This study shows a significant association between a 10-unit increment in the SI and a reduced incidence of AVSc, as shown by an adjusted odds ratio of 0.580 (P<0.001). Restricted cubic spline analysis with a multivariate logistic regression model revealed an inverse relationship between the SI and the incidence of AVSc, the observed nonlinear relationship need for further validation in larger, prospective cohorts to confirm. In this study, SI held a C-statistic of 0.708, given that the lack of gold standard biomarker, though it suggests moderate discriminative power, it is higher than the biomarker that had developed (eg t-PA 0.698).5 Incorporating SI into predictive models significantly enhances their accuracy in detecting AVSc among patients with CAD. This is evidenced by an increase in the C-statistic from 0.840 to 0.866 with NRI of 0.597 and an IDI of 0.064 (P<0.001). Additionally, SI proves to be a reliable predictor of sarcopenia, which in turn shows predictive capacity for AVSc. This study provides the inaugural evidence that a reduced SI correlates with the incidence of AVSc in individuals suffering from CAD, independent of demographic, clinical, and laboratory variables. The findings suggest that sarcopenia may play a crucial role in AVSc development, highlighting sarcopenia, a widespread skeletal muscle disorder, as a key factor. Skeletal muscle is integral to glucose metabolism and actin secretion,21 both of which decline with age, affecting muscle, bone, and fat tissue composition and reducing basal metabolic rate.22 The resultant muscle loss increases adiposity and insulin resistance, altering lipid metabolism and precipitating dyslipidemia.11 These metabolic disturbances are implicated in AVSc progression. Additionally, skeletal muscle functions as a secretory organ,23 releasing myokines such as irisin24 and follistatin-like protein 1 (FSTL1),25 both of which have been inversely associated with aortic valve calcification and stenosis. Previous research has also shed light on the common underlying mechanisms linking AVSc and sarcopenia, specifically chronic inflammation throughout the body and increased oxidative stress.26 Chronic systemic inflammation emerges as a pivotal link, where inflammatory cytokines such as TNF-α and IL-6 drive muscle catabolism in sarcopenia and promote valve calcification progression in AVSc, thereby connecting these conditions.27,28 In sarcopenia, persistent inflammatory responses lead to muscle protein degradation and impede regenerative processes, resulting in muscle wasting and weakness.29 Conversely, in AVSc, endothelial damage facilitates lipid infiltration and the recruitment of inflammatory cells, which contribute to the calcification of valve leaflets.30 Additionally, metabolic disturbances commonly observed in AVSc patients, including dyslipidemia and insulin resistance, increase oxidative stress and inflammatory responses, adversely affecting muscle health.20,31,32 Elevated serum calcium levels, as noted by Tao et al,33 further increase the risk of AVSc and disrupt muscle metabolism. The convergence of pathological factors in sarcopenia and AVSc indicates previously unrecognized clinical relationships between these conditions. However, the pathological and clinical relevance between declined SI and progression of SI still needs to be further investigated in a prospective, multi-center study.
Subgroup analysis further reveals that elevated SI levels are consistently associated with a lower risk of AVSc across diverse demographics, especially among elder adults, likewise, SI demonstrates stronger discriminative power for AVSc in elder age groups, with a C-statistic of 0.724 compared to 0.547 in younger cohorts, with high sensitivity. These findings underscore the potential of SI as a valuable detection indicator for enhancing AVSc risk prediction and stratification in varied CAD patient populations, with particular applicability to older adults, who represent the highest risk group for AVSc, sarcopenia, and CAD. Our study using an aged murine model confirmed these findings. Mice in the lower SI group showed significantly higher peak systolic aortic valve flow velocities, inversely correlated with SI (Spearman’s rho = −0.578, P = 0.006). Additionally, the aortic valve leaflets in the lower SI group mice exhibited notable increases in thickness, fibrosis, and calcification ratios. These observations highlight the negative effects of reduced SI on aortic valve structure and function.
Limitations
This is a single-center retrospective study, the causal relationship between SI and AVSc cannot be established, and ROC analysis still needs to be further validated in a large, multi-center, prospective study. Besides, the population of this study is predominantly Chinese, which limits the applicability of this study to other ethnic and geographic groups. The molecular links between sarcopenia and AVSc are poorly understood, necessitating advanced research to uncover therapeutic targets. The study’s reliance on the SI and its predominantly high-risk CAD patient population limit generalizability, highlighting the need for diverse cohorts and comprehensive sarcopenia assessments in future research.
Conclusion
This study elucidates the association between the SI and AVSc in patients with CAD. The findings reveal that lower SI levels are linked to a higher prevalence of AVSc. Furthermore, SI demonstrates moderate discriminatory capability for AVSc and enhances risk prediction when incorporated into clinical traditional models. Supporting these clinical observations, animal studies indicate that lower SI may correlate with increased aortic valve thickness, fibrosis, and calcification. Overall, the study highlights that sarcopenia index can be a valuable biomarker for predicting AVSc in CAD patients, which still need be further investigated by following up.
Funding
This work was supported by grants from the National Natural Science Foundation of China (82070401, 82100381), National Science and Technology Major Project 2023ZD0513700 and sponsored by the Shanghai Pujiang Program (22PJD044).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Madhavan MV, Gersh BJ, Alexander KP, Granger CB, Stone GW. Coronary artery disease in patients ≥80 years of age. J Am Coll Cardiol. 2018;71:2015–2040. doi:10.1016/j.jacc.2017.12.068
2. Coffey S, Cox B, Williams MJ. The prevalence, incidence, progression, and risks of aortic valve sclerosis: a systematic review and meta-analysis. J Am Coll Cardiol. 2014;63:2852–2861. doi:10.1016/j.jacc.2014.04.018
3. Otto CM, Newby DE, Hillis GS. Calcific aortic stenosis: a review. JAMA. 2024;332:2014–2026. doi:10.1001/jama.2024.16477
4. Freeman RV, Otto CM. Spectrum of calcific aortic valve disease: pathogenesis, disease progression, and treatment strategies. Circulation. 2005;111:3316–3326. doi:10.1161/circulationaha.104.486738
5. Chen Z, Shen Y, Xue Q, et al. Clinical relevance of plasma endogenous tissue-plasminogen activator and aortic valve sclerosis: performance as a diagnostic biomarker. Front Cardiovasc Med. 2020;7:584998. doi:10.3389/fcvm.2020.584998
6. Ooi H, Welch C. Obstacles to the Early Diagnosis and Management of Sarcopenia: current Perspectives. Clin Interv Aging. 2024;19:323–332. doi:10.2147/cia.S438144
7. Sasaki KI, Kakuma T, Sasaki M, et al. The prevalence of sarcopenia and subtypes in cardiovascular diseases, and a new diagnostic approach. J Cardiol. 2020;76:266–272. doi:10.1016/j.jjcc.2020.03.004
8. Kashani KB, Frazee EN, Kukrálová L, et al. Evaluating muscle mass by using markers of kidney function: development of the sarcopenia index. Crit Care Med. 2017;45:e23–e29. doi:10.1097/ccm.0000000000002013
9. Won MH, Yun KH, Kim H, Son YJ. Prognostic role of sarcopenia on major adverse cardiac events among patients who underwent successful percutaneous coronary intervention: a retrospective cohort study. Eur J Cardiovasc Nurs. 2024;23:287–295. doi:10.1093/eurjcn/zvad080
10. He N, Zhang Y, Zhang L, Zhang S, Ye H. Relationship between sarcopenia and cardiovascular diseases in the elderly: an overview. Front Cardiovasc Med. 2021;8:743710. doi:10.3389/fcvm.2021.743710
11. Damluji AA, Alfaraidhy M, AlHajri N, et al. Sarcopenia and Cardiovascular Diseases. Circulation. 2023;147:1534–1553. doi:10.1161/circulationaha.123.064071
12. Ngo DT, Sverdlov AL, Willoughby SR, et al. Determinants of occurrence of aortic sclerosis in an aging population. JACC Cardiovasc Imaging. 2009;2:919–927. doi:10.1016/j.jcmg.2009.03.016
13. Agmon Y, Khandheria BK, Meissner I, et al. Aortic valve sclerosis and aortic atherosclerosis: different manifestations of the same disease? Insights from a population-based study. J Am Coll Cardiol. 2001;38:827–834. doi:10.1016/s0735-1097(01)01422-x
14. Al-Taesh H, Çelekli A, Sucu M, Taysi S. Trace elements in patients with aortic valve sclerosis. Ther Adv Cardiovasc Dis. 2021;15:1753944720985985. doi:10.1177/1753944720985985
15. Williams B, Mancia G, Spiering W, et al. ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi:10.1093/eurheartj/ehy339
16. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323. doi:10.1093/eurheartj/ehz486
17. Bittl JA, Baber U, Bradley SM, Wijeysundera DN, Wijeysundera DN. Duration of dual antiplatelet therapy: a systematic review for the 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2016;134:e156–178. doi:10.1161/cir.0000000000000405
18. Herrmann HC, Pibarot P, Wu C, et al. Bioprosthetic aortic valve hemodynamics: definitions, outcomes, and evidence gaps: JACC state-of-the-art review. J Am Coll Cardiol. 2022;80:527–544. doi:10.1016/j.jacc.2022.06.001
19. Moncla LM, Briend M, Bossé Y, Mathieu P. Calcific aortic valve disease: mechanisms, prevention and treatment. Nat Rev Cardiol. 2023;20:546–559. doi:10.1038/s41569-023-00845-7
20. Gharacholou SM, Karon BL, Shub C, Pellikka PA. Aortic valve sclerosis and clinical outcomes: moving toward a definition. Am J Med. 2011;124:103–110. doi:10.1016/j.amjmed.2010.10.012
21. Kalyani RR, Corriere M, Ferrucci L. Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014;2:819–829. doi:10.1016/s2213-8587(14)70034-8
22. Baumgartner RN. Body composition in healthy aging. Ann N Y Acad Sci. 2000;904:437–448. doi:10.1111/j.1749-6632.2000.tb06498.x
23. Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat Rev Endocrinol. 2012;8:457–465. doi:10.1038/nrendo.2012.49
24. Wang SS, Li JM, Hu P, et al. Circulating Irisin level as a biomarker for pure aortic stenosis and aortic valve calcification. J Cardiovasc Transl Res. 2023;16:443–452. doi:10.1007/s12265-022-10327-9
25. Zhang Q, Ye J, Yang G, et al. Role of follistatin-like 1 levels and functions in calcific aortic stenosis. Front Cardiovasc Med. 2022;9:1050310. doi:10.3389/fcvm.2022.1050310
26. Kumar M, Pettinato A, Ladha F, et al. Sarcopenia and aortic valve disease. Heart. 2024;110:974–979. doi:10.1136/heartjnl-2024-324029
27. Bilski J, Pierzchalski P, Szczepanik M, Bonior J, Zoladz JA, Ribatti D. Multifactorial mechanism of sarcopenia and sarcopenic obesity. role of physical exercise, microbiota and myokines. Cells. 2022;11. doi:10.3390/cells11010160
28. Nishikawa H, Fukunishi S, Asai A, Yokohama K, Nishiguchi S, Higuchi K. Pathophysiology and mechanisms of primary sarcopenia (Review). Int J Mol Med. 2021;48. doi:10.3892/ijmm.2021.4989
29. Pan L, Xie W, Fu X, et al. Inflammation and sarcopenia: a focus on circulating inflammatory cytokines. Exp Gerontol. 2021;154:111544. doi:10.1016/j.exger.2021.111544
30. New SE, Aikawa E. Molecular imaging insights into early inflammatory stages of arterial and aortic valve calcification. Circ Res. 2011;108:1381–1391. doi:10.1161/circresaha.110.234146
31. Branch KR, O’Brien KD, Otto CM. Aortic valve sclerosis as a marker of active atherosclerosis. Curr Cardiol Rep. 2002;4:111–117. doi:10.1007/s11886-002-0022-8
32. Lerman DA, Prasad S, Alotti N. Calcific aortic valve disease: molecular mechanisms and therapeutic approaches. Eur Cardiol. 2015;10:108–112. doi:10.15420/ecr.2015.10.2.108
33. Tao J, Wang J, Peng H, et al. Association between serum phosphate, magnesium, calcium and aortic valve sclerosis: a propensity score-matched case-control study. Acta Cardiol. 2024;79:522–529. doi:10.1080/00015385.2024.2379682
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.