Back to Journals » Journal of Pain Research » Volume 18
The Association of Occipital Spur with Craniocervical Posture and Craniofacial Morphology
Authors Cheng Q , Xiao C , Lau Rui Han S, Hu S, Wu X, Dong Y, Xiong X , Fang S
Received 7 September 2024
Accepted for publication 20 December 2024
Published 10 January 2025 Volume 2025:18 Pages 179—187
DOI https://doi.org/10.2147/JPR.S488467
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Alaa Abd-Elsayed
Qiaoyu Cheng,1 Chuqiao Xiao,1 Sophie Lau Rui Han,1 Shoushan Hu,1 Xiayanran Wu,1 Yanhua Dong,1 Xin Xiong,1 Shanbao Fang2
1State Key Laboratory of Oral Diseases & National Center for Stomatology & National Clinical Research Center for Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan, 610041, People’s Republic of China; 2Department of Orthodontics, College & Hospital of Stomatology, Guangxi Medical University, Nanning, Guangxi, 530021, People’s Republic of China
Correspondence: Xin Xiong, State Key Laboratory of Oral Diseases & National Center for Stomatology & National Clinical Research Center for Oral Diseases, West China Hospital of Stomatology, Sichuan University, Chengdu, Sichuan, 610041, People’s Republic of China, Email [email protected] Shanbao Fang, Department of Orthodontics, College & Hospital of Stomatology, Guangxi Medical University, Nanning, Guangxi, 530021, People’s Republic of China, Email [email protected]
Purpose: This cross-sectional study aimed to evaluate the relationship between occipital spur (OS) with both craniocervical posture and craniofacial morphology.
Methods: The study involved 240 lateral cephalograms from subjects with and without OS. The craniocervical posture and facial morphology of every individual were assessed through Uceph software analysis of their cephalograms, considering 32 variables. The Independent T-test and the Mann–Whitney U-test were used to evaluate the relationships between the measures and OS. Differences in craniocervical posture and craniofacial morphology between the two groups were investigated by logistic regression.
Results: Subjects with OS exhibited more severe forward head posture (FHP) (larger C0-C1, Ba-C3ia, C2ap-C4ip, craniocervical angle, CVT-OPT, and NSL-C2’) and larger facial configuration (greater mandibular body length, posterior cranial base length, and posterior facial height) than the subjects without OS. Larger C2ap-C4ip (OR 1.53; 95% CI 1.282~1.82), Craniocervical angle (OR 1.70; 95% CI 1.457~1.977) and NSL-C2’ (OR 1.18; 95% CI 1.097~1.264), were associated with greater likelihood of having OS.
Conclusion: The subjects with OS were more prone to forward head posture than the control group. For subjects observed with OS on cephalograms, attention should be given to their possible abnormal cervical and head postures.
Keywords: occipital spur, craniocervical posture, craniofacial morphology, cephalometric analysis, forward head posture
Introduction
Enthesophytes are osseous spurs that develop where tendons, ligaments, fascia, or joint capsules insert into bones.1,2 An occipital spur(OS) is an abnormal bone growth on the external occipital protrusion (EOP).3 Anatomically, it is where the nuchal ligament and the trapezius muscle insert.4 Occipital spurs are also known as occipital buns, occipital knobs, occipital horns, onion hooks, and chignons.5 Spur areas are classified into three types: type 1 (flat), type 2 (crest), and type 3 (spine) (Figure 1).6,7 The application of radiological techniques allows them to be detected more frequently. The study conducted by Shahar et al found that forty-one percent of young adults had an enlarged external occipital protuberance (EEOP).8 Bony spurs are typically asymptomatic, but they may develop symptoms and cause discomfort over time.5,7,9
Biomechanical, inflammatory, immune and genetic factors may contribute to bone spur formation.10,11 Shahar et al suggested that mechanical influences could be essential in developing large enthesophytes.11 Musculoskeletal disorders may be linked to poor posture and biomechanical stress.8 A recent study has shown that aberrant loading of the EOP enthesis and sustained poor posture may be associated with the development of an EEOP.10 Some researchers have suggested that OS may be associated with pain at the base of the skull and headaches, potentially extending to the shoulders and neck.6,12 Considering the correlation between the craniocervical and craniomandibular systems, it is crucial to determine whether anatomical variations in one system can cause changes in the other. For example, symptoms and signs of temporomandibular disorders might be associated with craniofacial dimensions and head posture.13 Studies about the relationship between OS and craniocervical posture and craniofacial morphology were limited.
The purpose of this cross-sectional study was to investigate the relationship between OS with both craniocervical posture and craniofacial morphology, which might help explain OS etiology. The null hypothesis was that there was no relationship between OS and craniocervical posture and craniofacial morphology, whereas the experimental hypothesis was that there was a relationship between them.
Materials and Methods
Study Design
The cross-sectional study was conducted in the Department of Orthodontics, West China Hospital of Stomatology, Sichuan University, China. A sample size of 210 subjects was calculated using G*Power version 3.1.9.7 (Franz Faul, Universität Kiel, Germany; 1-β = 0.95, α = 0.05, effect size: d = 0.5). The sample consisted of 240 lateral cephalograms. The study protocol was approved by the Institutional Review Board of West China Hospital of Stomatology (No. WCHSIRB-D-2022-153) and complied with the Declaration of Helsinki. The verbal informed consent approved by the West China Hospital of Stomatology that the images might be used for scientific research was obtained from each patient before the lateral cephalogram examination.
We consecutively included 120 subjects with OS from January 2021 to October 2021 and matched the control group accordingly. This research excluded participants who had undergone orthognathic or other craniofacial surgeries or received orthodontic treatment. Individuals with systemic diseases impacting the craniofacial region or possessing craniofacial tumors and other anomalies were likewise not included. In addition, the study did not involve pregnant women or individuals under the age of 18. Lateral cephalometric radiographs taken in a natural head position (NHP) and teleradiographic examinations that highlight at least four cervical vertebrae are required for inclusion in this research. An OS could be determined when the spur length is greater than 5 mm (Figure 1). We divided subjects into two groups in this study: participants with OS (n=120) and those without OS (n=120).
Cephalometric Analysis
The lateral cephalograms were obtained following a standardized technique; the patients were instructed to stand in an NHP with maximum intercuspation, and not to swallow during the procedure. The radiographs were analyzed on Uceph software (version 4.3.3, Chengdu, China) to obtain the measurements. Cephalograms were traced by two experienced orthodontists blinded to the diagnosis of the patients. The reliability of the cephalometric method was tested by measuring 20 cephalometric radiographs randomly selected from each group twice within a 4-week interval. As the correlation coefficients between measurement errors exceeded 0.8, a high level of reliability was demonstrated.
A total of 25 landmarks were recorded on each radiograph, and 32 variables were calculated based on these landmarks: 15 variables for craniocervical posture and 17 variables for craniofacial morphology (Supplementary Table 1). The anatomical landmarks used for the analysis were shown in Figure 2. Measurements for craniocervical posture and craniofacial morphology were illustrated in Figures 3 and 4.
Statistical Analysis
All data were analyzed with the Statistical Package for the Social Sciences for Windows version 20.0 software. Quantitative variables were expressed as mean ± standard deviation (mean ± SD), while qualitative variables were expressed as n (%). Shapiro–Wilks test was used to test for normal distribution of each parameter. Whenever the data showed a normal distribution, the Independent samples t-test was used, and whenever not, the Mann–Whitney U-test was used. The Pearson correlation coefficient was used to test the collinearity between the variables. Then the differences in craniocervical posture and craniofacial morphology between the two groups were investigated by logistic regression. Statistical significance was set at P < 0.05.
Results
A total of 240 patients were included in this study, including 120 subjects with OS and 120 subjects without OS. Their age range was 18.10 to 47.67 years (mean age, 27.86±7.25). In terms of demographic characteristics, no significant difference in gender distribution or age distribution was noted between the two groups(P>0.05) (Table 1).
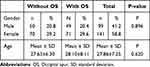 |
Table 1 Demographic Characteristics of Subjects with and without OS |
Six craniocervical measurements were statistically significant between the two groups. The C0-C1, Ba-C3ia, C2ap-C4ip, craniocervical angle, CVT-OPT, and NSL-C2’ of the subjects with OS were significantly greater than those without OS (Table 2). The standard distance between C0-C1 is 4–9 mm. Distances less than 4 mm may indicate a posterior rotation of the skull, whereas distances over 9 mm may indicate an anterior rotation.14 Higher values of Ba-C3ia indicate a more severe forward head posture.15 C2ap-C4ip represents the cervical spine’s length. The normal craniocervical angle is 96° to 106°. Values exceeding 106° suggest head flexion, and values below 96° suggest head extension.16 Increasing values of NSL/C2’ indicate an increase in cervical forward flexion in the second cervical segment and a more severe degree of forward head posture (FHP).17 The term “extension of the head” denotes a raised position of the head with respect to the cervical column, whereas the term “flexion of the head” indicates a forward bent posture. It appeared that subjects with OS exhibited a more severe FHP than those without OS.
 |
Table 2 Mean and Standard Deviation of the Different Measures of Cervical Posture in Subjects with and without OS |
Regarding craniofacial measurements, the OS group demonstrated significantly greater mandibular body length, posterior cranial base length, and posterior facial height compared with the control group (Table 3).
 |
Table 3 Mean and Standard Deviation of the Different Measures of Facial Morphology in Subjects with and without OS |
A positive correlation coefficient of 0.861 was observed between Ba-C3ia and C2ap-C4ip, and a positive correlation coefficient of 0.821 was observed between posterior facial height and Posterior cranial base length (P < 0.05) (Supplement Table 2). A high correlation coefficient between two variables (eg, > 0.8) indicates collinearity. Ba-C3ia and posterior facial height were excluded due to collinearity, and then a logistic regression was conducted. Results indicated that larger C2ap-C4ip (OR 1.53; 95% CI 1.282~1.82), Craniocervical angle (OR 1.70; 95% CI 1.457~1.977), and NSL-C2’ (OR 1.18; 95% CI 1.097~1.264), were associated with a greater likelihood of having OS (Table 4).
 |
Table 4 Results of Logistic Regression |
Discussion
The main objective of the study was to identify variations in craniocervical position and craniofacial morphology among individuals with OS and those without it. Statistical analysis confirms our hypothesis, showing significant differences in craniocervical posture and craniofacial morphology between the two groups. The C0-C1, Ba-C3ia, C2ap-C4ip, craniocervical angle, CVT-OPT, and NSL-C2’ of subjects with OS were significantly greater than those of the subjects without OS, which indicates that those with OS have a significant tendency to FHP. Considering the statistical differences in mandibular body length, posterior cranial base length, and posterior facial height, it is also possible to conclude that craniofacial morphology is associated with the development of OS.
An aberrant posture such as FHP may be responsible for the development of OS due to the insertion of key tendons and ligaments on the OS. As FHP increases, the mechanical load on the OS might increase due to the direct tension exerted at the attachment point by the upper trapezius fibers and ligamentum nuchae.18 In our study, the subjects with OS exhibited a mean value of 11.06±2.75mm of the C0-C1, suggesting a potential inclination towards anterior skull rotation. Increased Ba-C3ia, craniocervical angle, and NSL/C2’ values suggest a more pronounced FHP. The value of the craniocervical angle in the OS group exceeding 106° indicates head flexion. As implied from the binary logistic regression analysis outcome, greater C2ap-C4ip, Craniocervical angle, and NSL-C2’ tend to relate to the occurrence of OS, suggesting that subjects with OS were more likely to have a more pronounced FHP. Shahar et al found that mechanical forces played a significant role in bone spur formation, regardless of inflammatory or genetic factors.11 The study found that all participants who showed distinct FHP also had a history of aberrant posture and postural habits.11 The odds ratios of a cross-sectional study indicate that every 10 mm increase in FHP increases the likelihood of having EEOP by 1.03 times.10,19 In conclusion, it is likely that FHP plays a significant role in OS development. A high prevalence of EEOP among young people is speculatively attributed to poor posture influenced by the extensive use of handheld devices.10 However, Porrino et al found no significant association between iPhone accessibility and an exophytic external occipital protuberance.20 Differences in results may be due to variations in the grouping methods of the study samples.
It has been observed that subjects with OS tend to have a larger facial configuration than subjects without OS. The results of this investigation agree with the finding of a previous study that showed greater linear craniofacial measurements in subjects with enlarged occipital spur (EOS) than in those with OS.21 A possible association between OS and the development of the craniomaxillofacial system during puberty has been proposed.21 It is interesting to note that Çağlayan’s study found that OS is more common in mesocephalic and dolichocephalic skulls.22 FHP and craniofacial morphology might be involved in the development of OS, and further investigation is necessary.
Our results provide an innovative perspective on the link between OS and craniocervical posture from a clinical perspective. The OS has been associated with pain at the base of the skull, which may extend to the shoulder, limiting the movement of the shoulder and neck.6 Additionally, the tubercle may cause occipital headaches. This condition has been observed to be more common in tree climbers and basketball/volleyball players, who frequently perform vertical biomechanical movements of the neck.23 The results of this study suggested that FHP may be associated with OS, suggesting that people should avoid poor posture in their daily lives. By identifying the presence of OS on the lateral cephalograms, the orthodontist can inquire about the patient’s pain complaint, provide early diagnosis and referral, and advise the patient to correct their FHP.
There are several limitations in our study. The direct causal relationships between OS and craniocervical posture or between OS and craniofacial morphology were not clear due to the lack of longitudinal studies. Furthermore, these results were derived from lateral cephalograms of subjects in static positions and, therefore, did not accurately reflect the kinematics of the craniocervical region. Besides, the results might be limited to the test population and may not be generalizable to other age groups. Further studies with longitudinal data are needed to clarify the relationships of craniocervical posture and craniofacial morphology with OS. For patients with OS, this would be useful in the prevention and treatment planning process of OS development.
Conclusion
Statistically significant differences were observed regarding head and cervical posture and craniofacial morphology in the sample studied. Individuals with OS displayed a more severe FHP than those without OS. Identifying OS on lateral cephalograms might allow the orthodontist to ask the patient about cervical pain, provide early diagnosis and referral, and advise the patient in correcting FHP. Longitudinal assessments are necessary to confirm this conclusion.
Ethics Approval Information
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (Institution Review Board of the West China Hospital of Stomatology, Sichuan University, China) (No. WCHSIRB-D-2022-153).
Funding
The research was supported by National Clinical Key Specialty Construction Project (No. CZ000037), Guangxi Clinical Research Center for Craniofacial Deformity and Joint Project on Regional High-Incidence Diseases Research of Guangxi Natural Science Foundation under Grant No. 2023GXNSFAA026475, the National Natural Science Foundation of China (82301129) and Clinical Research Project of West China Hospital of Stomatology, Sichuan University (LCYJ-2023-YY-2).
Disclosure
The authors have no conflicts of interest relevant to this article.
References
1. Hermann S, Eshed I, Sáenz I, Doepner N, Ziegeler K, Hermann KGA. Osteo-proliferative lesions of the phalanges on radiography: associations with sex, age, and osteoarthritis. Diagnostics. 2022;12(3):618. doi:10.3390/diagnostics12030618
2. Di Matteo A, Cipolletta E, Destro Castaniti GM, et al. Reliability assessment of the definition of ultrasound enthesitis in SpA: results of a large, multicentre, international, web-based study. Rheumatology. 2022;61(12):4863–4874. doi:10.1093/rheumatology/keac162
3. Sattur M, Korson C, Henderson FJ, Kalhorn S. Presentation and management of traumatic occipital spur fracture. Am J Emerg Med. 2019;37(5):1005.e1–1005.e2. doi:10.1016/j.ajem.2019.01.043
4. Kadri PA, Al-Mefty O. Anatomy of the nuchal ligament and its surgical applications. Neurosurgery. 2007;61(5 Suppl 2):301–304. doi:10.1227/01.neu.0000303985.65117.ea
5. Varghese E, Samson RS, Kumbargere SN, Pothen M. Occipital spur: understanding a normal yet symptomatic variant from orthodontic diagnostic lateral cephalogram. BMJ Case Rep 2017. 2017;bcr2017220506. doi:10.1136/bcr-2017-220506
6. Srivastava M, Asghar A, Srivastava NN, Gupta N, Jain A, Verma J. An anatomic morphological study of occipital spurs in human skulls. J Craniofac Surg. 2018;29(1):217–219. doi:10.1097/SCS.0000000000004205
7. Singal A, Chaudhary P, Singh P. External occipital protuberance classification with special reference to spine type and its clinical implications. Surg Radiol Anat. 2023;45(5):555–561. doi:10.1007/s00276-023-03133-8
8. Shahar D, Sayers MGL. A morphological adaptation? The prevalence of enlarged external occipital protuberance in young adults. J Anat. 2016;229(2):286–291. doi:10.1111/joa.12466
9. Marshall RC, Abela C, Eccles S. Painful exostosis of the external occipital protuberance. J Plast Reconstr Aesthet Surg. 2015;68(11):e174–e176. doi:10.1016/j.bjps.2015.06.013
10. Shahar D, Sayers MGL. Author Correction: prominent exostosis projecting from the occipital squama more substantial and prevalent in young adult than older age groups. Sci Rep. 2019;9(1):13707. doi:10.1038/s41598-019-49153-6
11. Shahar D, Evans J, Sayers MGL. Large enthesophytes in teenage skulls: mechanical, inflammatory and genetic considerations. Clin Biomech. 2018;53:60–64. doi:10.1016/j.clinbiomech.2018.02.004
12. Gómez Zubiaur A, Alfageme F, López-Negrete E, Roustan G. Type 3 external occipital protuberance (Spine Type): ultrasonographic diagnosis of an uncommon cause of subcutaneous scalp pseudotumor in adolescents. Actas Dermosifiliogr. 2019;110(9):774–775. doi:10.1016/j.ad.2018.04.015
13. Sonnesen L, Bakke M, Solow B. Temporomandibular disorders in relation to craniofacial dimensions, head posture and bite force in children selected for orthodontic treatment. Eur J Orthod. 2001;23(2):179–192. doi:10.1093/ejo/23.2.179
14. Ekici Ö, Camcı H. Relationship of temporomandibular joint disorders with cervical posture and hyoid bone position. Cranio. 2024;42(2):132–141. doi:10.1080/08869634.2021.1926745
15. Kang JH. Effects on migraine, neck pain, and head and neck posture, of temporomandibular disorder treatment: study of a retrospective cohort. Arch Oral Biol. 2020;114:104718. doi:10.1016/j.archoralbio.2020.104718
16. Matheus RA, Ramos-Perez FM, Menezes AV, et al. The relationship between temporomandibular dysfunction and head and cervical posture. J Appl Oral Sci. 2009;17(3):204–208. doi:10.1590/S1678-77572009000300014
17. Xiao CQ, Wan YD, Li YQ, et al. Do temporomandibular disorder patients with joint pain exhibit forward head posture? A cephalometric study. Pain Res Manag. 2023;2023:7363412. doi:10.1155/2023/7363412
18. Mercer SR, Bogduk N. Clinical anatomy of ligamentum nuchae. Clin Anat. 2003;16(6):484–493. doi:10.1002/ca.10121
19. Shahar D, Sayers MGL. Prominent exostosis projecting from the occipital squama more substantial and prevalent in young adult than older age groups. Sci Rep. 2018;8(1):3354. doi:10.1038/s41598-018-21625-1
20. Porrino J, Sunku P, Wang A, Haims A, Richardson ML. Exophytic external occipital protuberance prevalence pre- and post-iPhone introduction: a retrospective cohort. Yale J Biol Med. 2021;94(1):65–71. doi:10.1002/art.38729
21. Cheng Q, Xiong X, Li Y, et al. Enlarged occipital spur and craniofacial morphology: a cephalometric analysis. Oral Radiol. 2023;39(4):743–749. doi:10.1007/s11282-023-00694-7
22. Çağlayan F, Güller H, Öncü E, Kuzey N, Dalcı H. The frequency of occipital spurs in relation to the cephalic index: an anatomorphometric cone beam CT study. Niger J Clin Pract. 2024;27(5):647–653. doi:10.4103/njcp.njcp_45_24
23. Singh R. Bony tubercle at external occipital protuberance and prominent ridges. J Craniofac Surg. 2012;23(6):1873–1874. doi:10.1097/SCS.0b013e31826c7d48
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





