Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 20
The Cost-Effectiveness of a Personalised Early Warning Decision Support System (The COPDPredict™ System) to Predict and Prevent Acute Exacerbations of Chronic Obstructive Pulmonary Disease
Authors Hall JA , Turner AM , Gkini E , Mehta R, Spiteri M , Patel N, Jowett S
Received 10 September 2024
Accepted for publication 7 March 2025
Published 25 May 2025 Volume 2025:20 Pages 1693—1710
DOI https://doi.org/10.2147/COPD.S486309
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jill Ohar
James A Hall,1 Alice M Turner,2 Eleni Gkini,3 Rajnikant Mehta,4 Monica Spiteri,5 Neil Patel,5 Sue Jowett1
1Health Economics Unit, Department of Applied Health Sciences, University of Birmingham, Birmingham, UK; 2Department of Applied Health Sciences, University of Birmingham, Birmingham, UK; 3Birmingham Clinical Trials Unit, Department of Applied Health Sciences, University of Birmingham, Birmingham, UK; 4Centre for Evaluation and Methods, Wolfson Institute of Population Health, Queen Mary University of London, London, UK; 5NEPESMO Ltd, London, UK
Correspondence: Sue Jowett, Email [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) is a respiratory disease associated with significant morbidity, mortality, and healthcare burden. Many COPD patients are frequent exacerbators, which has a significant impact on patient prognosis. Prompt exacerbation management using a digital tool, COPDPredict™ may support COPD patients in identifying exacerbations earlier to reduce hospital admissions.
Methods: Trial-based cost-utility and cost-effectiveness analyses from the UK National Health Service perspective compared the cost-effectiveness of COPDPredict™ with usual care for a COPD GOLD stage B and D cohort. A model-based analysis was also performed by extrapolating data from the trial to obtain the-cost-utility over a 5-year time horizon. The de-novo model was constructed using GOLD stages A–D as the health states.
Results: The imputed trial-based analysis showed that at a willingness to pay £ 20,000 per quality-adjusted life-year (QALY), COPDPredict™ was 65% likely cost-effective in COPD B and D patients over 6-months with an incremental cost-effectiveness ratio (ICER) of £ 11,669/QALY (incremental cost +£ 238.16 (106.42), Incremental QALY +0.02 (0.012)). The results were robust to complete case analyses over 6- and 12-months. A similar ICER (£ 11,862/QALY) was obtained when performing model-based analysis over 5-years. Cost-effectiveness was sensitive to long-term effectiveness, cost parameters and alternative model structure, with expected value of information analyses suggesting a significant benefit from future research targeting the long-term effectiveness of the intervention.
Conclusion: COPDPredict™ is potentially cost-effective for COPD B and D patients. However, the small samples sizes upon which the results were obtained warrant further investigation.
Keywords: chronic obstructive pulmonary disease, respiratory medicine, self-management, digital health, cost-effectiveness analysis, decision modelling
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive lung disease affecting tens of millions of adults globally.1 The disease is accompanied by recurring acute exacerbations (AECOPD), that lead to clinical deterioration, and when severe, cause around 130,000 hospital admissions annually in the UK.2 The UK has one of the highest mortality rates from lung disease in Europe,3 with nearly 40% of patients dying or being readmitted to hospital within 90 days of an exacerbation of COPD.4 A 2022 study estimated that the healthcare costs of COPD in England was around £2bn and estimated to continue to increase5 to £2.32bn by 2030.6
National Institute for Health and Care Excellence (NICE) treatment guidance for COPD7 includes a supported tailored self-management plan (SSMP) for patients to identify and treat AECOPD, typically by taking rescue medications (antibiotics and steroids). Various treatments are recommended by NICE to reduce exacerbations and improve care; pharmacological treatments such as azithromycin, inhaled bronchodilators, and inhaled corticosteroids; and non-pharmacological treatments such as oxygen therapy, long-term non-invasive ventilation, or pulmonary rehabilitation.7
AECOPD often involves shifts in key biological markers, such as blood C-reactive protein (CRP), physiological indicators (eg lung function), and worsening symptoms. Integrating these data into patient assessments can enhance the accuracy of diagnosing, determining causes, or assessing severity. While some studies have utilised CRP measurement for treatment decisions, none have incorporated multiple measures or personalised guidance.8
Modern digital technologies enable regular monitoring of physiology, pathology, and symptoms for personalised early AECOPD warnings. This empowers patients, with or without healthcare support, to potentially avoid hospitalisation. Spirometry measurements, connected to symptom reporting via a Bluetooth-enabled app, can be performed at home, and point-of-care CRP tests can offer real-time biomarker data. Based on these principles, the COPDPredict™ system, an approved medical device, has shown in preliminary data it may reduce admissions in COPD patients. The Predict & Prevent Phase III two-arm, multi-centre, open-label, parallel-group, individually randomised clinical trial of the device was undertaken to determine whether the system could be adopted in UK practice.8
Recent clinical evidence suggested that the COPDPredict™ system is associated with lower hospital admissions and improved quality of life.9 Adoption decisions regarding new healthcare interventions in England and Wales require recommendations from NICE guidance based on clinical and cost-effectiveness evidence, with economic evaluations from an NHS/Personal Social Services (PSS) perspective using cost-utility analysis (cost-per-quality-adjusted-life-year (QALY)).10 The NHS/PSS perspective is preferred for economic evaluations in the UK, as interventions are funded directly by the NHS, which, in turn, is centrally funded by general taxation and national insurance via the Department of Health and Social Care. Economic evaluation evaluates cost-effectiveness by calculating the estimated incremental costs and effects arising from the introduction of a new technology compared with current care. Accordingly, using data from the Predict and Prevent trial, we present an economic evaluation of both cost-per-QALY gained and cost-per-disease-specific measure using cost-per-additional exacerbation prevented. Where the costs and effects arising from the introduction of a new technology are expected to last beyond the time horizon of the trial, it is recommended that decision modelling be undertaken to estimate the long-term cost-effectiveness of the intervention. With this in mind, we also present the modelled cost-effectiveness of the COPDPredict™ system over 5 years from the NHS/PSS perspective.
Methods
Overview
Full details of the Predict and Prevent trial methods are presented in the trial protocol8 and clinical effectiveness paper.9 In brief, a Phase III, multi-centre, individually randomised trial with 12-month follow-up investigated the efficacy of a personalised early warning decision support system (COPDPredict™) in predicting and preventing acute COPD exacerbations. The eligibility criteria were a clinical diagnosis of COPD confirmed through post-bronchodilator spirometry, and a history of one or more AECOPD episodes within any 12-month period in the past 2 years, or one or more hospital admissions for AECOPD within the preceding 2 years. Participants were excluded if they had a life expectancy under 12 months or had comorbidities that precluded patients from using the intervention. Due to recruitment difficulties, the final sample size was 90 patients, with 45 patients in each arm, and a follow-up period of 6–12 months. Therefore, patients with shorter follow-up periods were also included in the analysis to increase sample size.
Accordingly, the base case within-trial economic evaluation was performed over 6-months follow-up using imputation according to the intention-to-treat principle for participants providing economic data at least one follow-up point. All costs are reported in 2021 British pounds (£). The analysis was undertaken from the UK NHS/PSS perspective as per NICE guidance for economic evaluations.10 The cost-utility analysis calculated the cost-per-additional QALY gained, as well as a cost-effectiveness analysis of cost-per-hospitalisation prevented. STATA 17 (StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC). and Excel (Microsoft Corporation. 2022. Microsoft® Excel® (Version 2202 Build 16.0.14931.20806) 64-bit) was used for analysis.
Trial-Based Economic Evaluation
Health Care Resource Use and Costs
Resource use data were collected via questionnaires at 3-, 6-, 9-, and 12-months post-randomisation, respectively. The questionnaires documented details on AECOPD-related hospitalisations, respiratory clinic visits, A&E attendance, investigations, primary care visits, and medication use. Resource use was costed using standard unit costs (see Appendix 1), including NHS reference costs,11 NHS electronic drug tariff12 for medications, and Unit Costs for Health and Social Care.13
A detailed cost analysis involving communication with intervention developers, study members, and independent stakeholders determined NHS costs for the COPDPredict™ intervention (Table 1). It was assumed that most patients (70%) would receive the App within a hospital setting with the annual licence paid by the health system. The intervention would require clinical support for ongoing monitoring of the clinical dashboard (with a training cost in the first year). CRP testing and home spirometry would be ongoing, with initial costs of purchasing testing equipment in the first year.
 |
Table 1 Annual Costs Associated with COPDPredict™ |
 |
Table 2 Unadjusted Imputed Health Outcomes Over 6 months for Patients at Baseline, 3 and 6 Months. Costs at 6 Months. Values are Mean (SE) Scores Unless Stated |
Patient Costs and Work-Related Absence
Data on direct patient medical costs related to purchasing medical devices or paying for private healthcare were obtained from the questionnaires. Productivity costs were calculated using the human capital approach by multiplying self-reported absence by the respondent’s wage based on UK occupational classification coding and annual earnings for each job type, and assuming that the value of lost work is equivalent to compensation.14 Due to the small number of responses and the risk of spurious correlation these outcomes were not included in the cost-effectiveness analysis. Patient direct private healthcare costs are shown in Table 2, and outcomes related to work-related absence are reported in Appendix 2.
Outcomes
The EQ-5D-5L instrument generates a utility score based on health-related quality-of-life preferences. EQ-5D-5L scores were obtained using questionnaires at baseline and 3-, 6-, 9- and 12-months post-randomisation. EQ-5D-5L responses were converted into multi-attribute utility scores using an approved “cross-walk” to the 3 L instrument for the UK.15 QALYs were calculated using the area under the curve method, assuming linear interpolation between time periods. Deceased patients were excluded from the analysis as neither comparator was expected to impact mortality, and their inclusion may bias estimates due to small sample sizes as an early death would result in a QALY very close to zero. For the cost-effectiveness analysis, self-reported hospitalisations for either infective or non-infective COPD exacerbations were used as the outcome measure.
Statistical Analyses
Imputed mean healthcare costs and health-related quality of life (measured by EQ-5D-5L and QALYs) were presented for each intervention during 6-month follow-up. In the base-case cost-utility and cost-effectiveness analyses, missing cost and outcome data were analysed using intention-to-treat principles. Chained multiple imputation was utilised, using the arithmetic mean of 50 estimates for each missing value, and considering predictors of missingness, such as previous or subsequent observations of the same variable, age, gender, site, and COPD stage. Hospital admission for exacerbation was part of the imputation model for costs. Disaggregation of all mean costs related to the intervention and usual care, healthcare, patient-incurred costs, and time-off work were presented for the base case. Due to substantial missing data, a 12-month imputed analysis was presented as a speculative sensitivity analysis. Complete case analyses were shown for the 6-month and 12-month periods, using data from patients who completed all healthcare and EQ-5D questionnaires for those time points. The costs and QALYs were not discounted.
Incremental cost-effectiveness ratios (ICERs) were computed by dividing the adjusted difference in mean costs by the adjusted difference in mean QALYs for the cost-utility analysis and the adjusted difference in hospitalisations for the cost-effectiveness analysis, using non-parametric bootstrapping with 5,000 replications. Adjustment was made through seemingly unrelated regression of incremental costs and effects, incorporating baseline variables (age, gender, site, and COPD stage) along with the baseline EQ-5D for QALYs. The probability of cost-effectiveness was evaluated using the NICE threshold, reflecting the UK health system’s willingness to pay for an additional QALY, a threshold which lies between £20,000 ($25,000 or €23,400) and £30,000 ($37,300 or €35,100) per additional QALY.
Base case results were graphically depicted in cost-effectiveness planes and acceptability curves (CEACs), displaying the distribution of incremental costs and QALYs, and estimating cost-effectiveness across various willingness-to-pay (WTP) thresholds for an additional QALY. Deterministic sensitivity analysis assessed robustness by undertaking a complete case analysis as well as 12-month imputed and complete case analyses.
Model-Based Analysis
Overview
A cost-utility analysis extrapolating beyond the trial was performed by comparing COPDPredict™ with usual care for management of patients with COPD stage D. A Markov cohort model with a 1-month time cycle was constructed to estimate QALYs and costs from the NHS/PSS perspective. A 5-year time horizon was chosen, reflecting the duration experts felt the technology would benefit patients. Discounting was applied at 3.5% for both the costs and outcomes.
Model Population
As nearly all participants in the trial had COPD stage D (more COPD symptoms as well as ≥ 2 AECOPD or ≥ 1 hospitalised exacerbation) (87.8% stage D and 12.2% stage B), only this patient group had reliable parameter estimates; therefore, the base-case model was run exclusively for patients in COPD GOLD stage D.
Model Structure and Transition Probabilities
In the first year, the costs and QALYs for both comparators were derived from adjusted bootstrapped analyses of the trial data (Appendix 3 and Table S4). From year 1 onwards, patients began in health states that reflected the GOLD stage achieved in the trial at 12-months (see Table 3). COPDPredict™ had fewer patients in Stage D compared with usual care, resulting in a beneficial effect throughout the model.
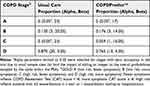 |
Table 3 Proportions in Each Health State at 12 months with PSA Beta Distribution Parameters |
From the second year onwards patients moved through the model as shown in Figure 1. A previous COPD model developed by the author team16 was updated to reflect recent COPD classifications.17 Patients transitioned between GOLD stages reflecting prognosis within the BLISS cohort study18 (described in Appendix 4), where patients were categorised into GOLD stages A-D at 12-month and 24-month follow-up.
When the patient had a severe hospitalised exacerbation, they occupied 3 post-discharge tunnel states for 3-months reflecting their reduced quality of life. As GOLD stage is partly based upon admission history patients in COPD A and B logically moved to C and D after an admission. A transition matrix reflecting movements between each of the stages over the second year of the study, is shown in Table S6 and Appendix 3.
Modelled Treatment Effect
There were four independent treatment effects relating to COPDPredict™ in the model. The first effect was shown in Table 3, eg, the benefit from improved starting states. Secondly, a lower rate of severe exacerbations was detected in the trial on COPDPredict™ meaning fewer patients will transition from Stages A and C to Stages B and D on the intervention. The usual care transition matrix shown in Table S6 was adjusted to reflect expert advice that the anticipated likely future benefit of COPDPredict™ upon exacerbations would continue but decline by 50% each year until the end of Year 5 (shown in Table 4). New transition probabilities for COPDPredict™ patients were calculated and are shown for year 2–5 in Table 4.
 |
Table 4 Monthly Transition Probabilities and Exacerbation Rates for COPDPredict™ Model Arm, yr 2–5 with PSA Distribution Parameters |
Third, for patients in states B and D, defined by a hospitalised exacerbation, fewer exacerbations would occur on the intervention. Mean exacerbations per stage were taken from BLISS18 (Table 4) and multiplied by the relative risks to obtain the exacerbation rate on the intervention.
Finally, those who had a hospitalised exacerbation had 1.278 (0.914) fewer bed days per exacerbation when receiving COPDPredict™.
Utility Values
During the first year of the model, utility values directly reflected those from trial data (Table S4). From 12 months onwards, utility values for each COPD stage for both comparators reflected mean utility values for patients at 12-month follow-up in the BLISS cohort (shown in Table 5). Disutility for hospitalised exacerbations were also obtained from the BLISS data.18
 |
Table 5 Year 2–5 Utility Values and Costs for GOLD Stages and Hospitalised Exacerbations with PSA Distribution Parameters |
Costs
During the first year of the model, the modelled data directly reflected the imputed costs obtained from the trial (Table 2).
Costs Years 2–5
For the modelled analysis, those on the COPDPredict™ intervention incurred costs associated with the intervention (Table 1), in addition to the mean costs associated with membership of each COPD stage. Stage membership costs were estimated independent of hospitalised exacerbation costs but included non-hospitalised exacerbation costs (Table 5). Costs were taken from the trial data because of the more comprehensive level of cost included compared with the BLISS cohort data.18 GLM Regression techniques were used to estimate costs associated with stages A and C by controlling for costs associated with exacerbations and subtracting them from states B and D. Hospitalised exacerbations were estimated using the prices shown in Appendix 1, with COPDPredict™ hospitalised exacerbation costs reduced to reflect fewer bed days.
Key Model Assumptions
Sensitivity Analysis
Deterministic analysis explored the impact of uncertainty in key model parameters, as well as methodological and structural decisions, on model outputs. These include the following alternative scenarios;
- Intervention costs
- Reduction in bed days
- Utility gains on the intervention
- Overall severe exacerbation rates
- Effect of intervention on severe exacerbations
- Starting states
Recognising the proposed updates to the GOLD categorisation of COPD severity, we included a sensitivity analysis reflecting the new GOLD classifications where A and B groups are unchanged but C and D are merged into a single group termed “E” which is >2 moderate exacerbations or >1 hospitalised exacerbation (detailed methods in Appendix 5).
For Probabilistic sensitivity analysis (PSA), distributions were constructed for each model parameter, and PSA was performed using 10,000 replications with sampling from the distributions. Distributions are stated in the model parameter tables, but generally beta distributions were used for probabilities and utility values, normal and gamma distributions for costs, and log-normal distributions for relative risks.
Cost-effectiveness planes were plotted to show the distribution of incremental costs and QALYs, and CEACs were constructed to reflect the intervention cost-effectiveness probability at different WTP per QALY thresholds. The Expected Value of perfect information (EVPI) analysis was undertaken to explore the value of further research, and the Expected Value of Perfect Parameter Information (EVPPI) to identify where that research should be targeted.
Results
Trial Based Analysis
Base Case Analysis Imputed Over 6-Months
There were considerable improvements in EQ-5D over the first six months on the intervention (Table 2). Accordingly, on average, COPDPredict™ was associated with 0.036 more QALYs over 6-months. However, COPDPredict™ was also associated with higher NHS costs, particularly related to the cost of the intervention and home visits, while the costs associated with hospitalisations were lower.
An economic analysis was not performed from a societal perspective because few patients were employed (n=15 at 6-months), skewing related to outliers (one patient had 61 days of work absence on usual care), and missingness (>50% at 12-months). Nonetheless it is worth noting that private healthcare and patient-incurred costs were £22.65 lower for COPDPredict™. Appendix 2 presents selected work-related outcomes.
Cost Utility Analysis
When adjusting for baseline randomisation variables and applying non-parametric bootstrapping of costs and QALYs, COPDPredict™ was associated with £238.16 additional NHS costs with a QALY gain of 0.020 (Table 6).
 |
Table 6 Imputed Descriptive and Bootstrapped Adjusted Incremental Health Outcomes and Costs Over 6 Months. Values are Mean (SE) Scores Unless Stated Otherwise |
The intervention was 65% likely to be cost-effective with an ICER of £11,669/QALY.
Figure 2 shows the distribution of bootstrapped costs and effects, with most samples showing an incremental gain in QALY, suggesting that the intervention is very likely to be effective.
 |
Figure 2 Adjusted bootstrapped imputed cost utility plane comparing COPDPredict™ with usual care at 6-months. |
When plotted on the cost-effectiveness acceptability curve, the intervention rises to 74% likelihood of cost-effectiveness at the upper bound of the NICE willingness-to-pay threshold of £30,000/QALY (Figure 3).
 |
Figure 3 Adjusted bootstrapped imputed cost effectiveness acceptability curve comparing COPDPredict™ with usual care at 6-months. |
Cost Effectiveness Analysis
The cost-effectiveness analysis in Table 7 shows that COPDPredict™ was associated with a reduction in hospitalisations of 0.018 over 6-months, with bootstrapped adjusted analysis showing a mean reduction of 0.016 in hospitalisations.
 |
Table 7 Imputed Incremental Hospitalisations and Costs Over 6 Months. Results are Adjusted for Baseline Randomisation Variables |
The ICER estimates a cost of £12,394 to avert a hospitalisation with a 57% probability of a reduction in hospitalisations over 6-months.
Sensitivity Analysis
Cost-utility results were robust to methodological approach, as Table 8 shows, the complete case results yield similar results at 6-months, albeit slightly higher probability of cost-effectiveness at 68% rising to 78% at £30,000/QALY.
 |
Table 8 Regression Adjusted and Bootstrapped Incremental Health Outcomes and Costs Over 6- and 12-Months. Complete Case Analyses. Values are Mean (SE) Scores Unless Stated Otherwise |
A complete case analysis over 12-months was more speculative, as only 43 patients returned all relevant data points. COPDPredict™ was still associated with a considerable QALY gain at a modest additional NHS cost when bootstrapping and adjustment are considered.
When imputing all surviving patients over 12-months Table 9 shows that the incremental costs of COPDPredict™ may be higher (+£526.38) than the complete case analysis suggests, with an accompanying smaller QALY gain (+0.019), resulting in an ICER above £20,000/QALY and a likely cost-effectiveness probability of 43%, increasing to 52% at £30,000/QALY.
 |
Table 9 Regression Adjusted and Bootstrapped Imputed Incremental Health Outcomes and Costs Over 12 Months. Values are Mean (SE) Scores Unless Stated Otherwise. N=78 |
Model-Based Analysis
Base Case
The base case model results are shown in Table 10.
 |
Table 10 Base Case Model Estimated Incremental Health Outcomes and Costs Over 5 years |
The intervention is likely to be cost-effective, with an ICER of £11,862/QALY. The PSA results in Figure 4 show that it is highly likely that the intervention provides incremental QALY gains, albeit at additional costs.
 |
Figure 4 Base case model cost utility plane comparing COPDPredict™ with usual care over 5 years. |
The CEAC in Figure 5 shows a 68% probability of cost-effectiveness at £20,000 per QALY, which increases to 76% at £30,000 willingness to pay.
 |
Figure 5 Base case modelled cost effectiveness acceptability curve comparing COPDPredict™ with usual care over 5 years. |
Deterministic and Scenario Analysis
The sensitivity analysis showed that the results were very sensitive to the costs and outcomes of the intervention (Appendix 6 and Table S14). If intervention costs were greater than those in the trial, then the intervention would be less cost-effective, and vice versa. If the reduction in bed days was not sustained beyond the first year, cost-effectiveness probability would decrease to 62%.
The base-case model did not include an intervention utility benefit, independent of reducing exacerbations. Cost-effectiveness would be much higher (rising to 92%), with an annual 0.04 improvement of EQ-5D score independent of the exacerbation effect.
As few patients experienced hospitalised exacerbations (<20%, even in COPD stage D), the model is robust to differing assumptions regarding interventions that reduce hospitalised exacerbations. However, the baseline severe exacerbation rates in the trial (and the BLISS cohort13) were much lower than those estimated by a recent analysis of COPD patients using CPRD and HES data with 44,000 patients.19 Accordingly, a sensitivity analysis was performed using higher estimates, with a significant improvement in the likelihood of the cost-effectiveness of COPDPredict™. Starting states are far more influential on cost-effectiveness if they are assumed to be equal at 12-months; then, cost-effectiveness falls to an ICER above the £20,000 NICE threshold.
When using a model structure with the GOLD ACE health states (Appendix 5 and Table S13) the ICER for the intervention falls just above the threshold (£21,689/QALY) with the PSA showing 48% probability of cost-effectiveness at the £20,000 NICE threshold, rising to 61% probability at £30,000/QALY (Figure S2).
Expected Value of Perfect Information
Unsurprisingly, given the small sample sizes and uncertainty, there is expected to be considerable value in further information; at a willingness to pay of £20,000/QALY, the EVPI is £556 per patient (Figure 6).
 |
Figure 6 Expected value of perfect information curve. |
Appendix 7 and Table S15 describe the methods used to obtain the estimated population expected to benefit from the intervention, 626,129, which is used to multiply per-patient costs. Table S16 in Appendix 6 shows that there is significant value in future research when the population size is considered, future research should target stage transitions and mortality rates, particularly for COPDPredict™.
Discussion
Main Findings and Interpretation
The results of both trial- and model-based economic analyses provide evidence that the COPDPredict™ system is cost-effective for COPD stage D patients in the UK. The strong likelihood of cost-effectiveness is driven primarily by an improvement in EQ-5D scores seen in the trial, as well as a reduction in hospitalised exacerbations which influences the long-term trajectory of patients in the model-based analysis.
Model-based results suggest that the intervention is likely to continue to be cost-effective when used over the longer-term. The trial-based and model-based analyses produced similar ICERs despite the additional period to benefit within the model. This is because the relative risk reduction in exacerbations is assumed to decline in magnitude over five years in the model, and the full cost of the licence fee for the intervention is also incurred over five years. Note, long-term cost-effectiveness modelling is predicated upon some continued reduction in exacerbations and bed days experienced from the intervention, improved COPD Gold state, and lower costs, which are currently based on small sample sizes in the trial and are therefore uncertain.
Sensitivity analysis can help understand the impact of these assumptions upon intervention cost-effectiveness. Whilst the model is somewhat robust to alternative assumptions regarding the period of benefit and even choice of model structure, the results are highly sensitive to small changes in costs. For example, if costs were reduced, perhaps by tailoring home-visit routines more efficiently to target patients most in need, the cost-effectiveness of the intervention would improve considerably. Equally, it is important to continue to look for ways to minimise costs to ensure that increases in costs do not render the intervention too expensive.
The base-case model is conservative in some respects and possibly underestimates the benefit of the intervention upon quality of life, which the trial-based analyses suggest could go beyond merely reducing exacerbations. If even minor improvements in quality of life were sustained during the model, this would lead to improved cost-effectiveness of the intervention. Moreover, the trial suggested low rates of hospitalised exacerbations across this population; however, if hospitalised exacerbation rates were higher, the cost-effectiveness of the intervention would improve significantly. This is a logical implication, as a relative risk reduction has a greater effect on the higher the base number it impacts. Therefore, another logical implication is that the intervention may be more effective in more frequently exacerbating patients.
Within the trial-based analysis, the imputed 12-month results suggest that there may be some uncertainty in the likely cost-effectiveness of the intervention, although it should be noted that imputing over 50% of the observations for the intervention should be considered highly speculative.
Whilst a novel methodology applying the new proposed GOLD ACE health states was presented, caution is proposed over the use of such classifications in long-term modelling of COPD patients. In economic modelling any attempt to merge health states can potentially reduce granularity and therefore the sensitivity of models to potential improvements in longer-term health prognosis. In this case GOLD C is superior to GOLD B and D (higher quality of life and lower costs), and therefore merging C and D into GOLD E dilutes the modelled benefit of COPDPredict™ over time. In this model this occurs in two separate ways; firstly, in the ABCD model 6% of patients initially move into GOLD C on COPDPredict™ and 0% on usual care, a benefit which is negated in the ACE model. Secondly, throughout the ABCD model COPDPredict™ has the effect of increasing GOLD B membership at the expense of GOLD D, As GOLD E has both a higher utility value and lower cost than GOLD D, this benefit is diluted for both costs and quality of life. We recommend health economists give consideration to the likely impact of the modelled intervention upon condition-specific disease processes before selecting an appropriate structure.
Implications for Clinical Practice
The results of these analyses could carry significant implications for clinical practice. Clinicians should recognise the potential that integration of app-based self-management tools into routine care could provide for the enhancement of patient outcomes by empowering patients with real-time support as well as education. Additionally, clinicians should note the potential benefits associated with reduced hospital admissions, such as freeing beds for the treatment of other patients. Successfully integrating COPDPredict™ does necessitate training for both healthcare professionals and patients to ensure effective utilisation and maximise the potential benefits of app-based self-management programs within the clinical setting. This necessitates consultant oversight of the dashboard (or training others to a sufficient level to do so) as well as the dashboard requiring a 7-day service for prompt response to alerts.
Strengths and Limitations
The strengths of our trial-based analysis lie in the presentation of both trial- and model-based analyses of the intervention, providing a broader understanding of the potential benefits and costs of the intervention as well as the degree of uncertainty and points of sensitivity.
The model itself represents a novel methodology in that it applies recent GOLD classifications to produce an original model which reflects recent understanding of the disease with progression through a model reflecting exacerbation frequency, which is critically important for this population. Analysing the Birmingham COPD cohort study allowed the generation of estimates on transitions between stages of ABCD for over 1000 patients, which were provided as transition probabilities and could be used to model future COPD ABCD models instead of the older models based on COPD 1–4. We also present the same innovation for newly proposed COPD ACE health states.
The model relies on assumptions regarding long-term treatment impacts derived from small sample sizes. However, decision-modelling methods have been used to estimate the impact of, and quantify the value of a reduction in, uncertainty. Broad deterministic sensitivity analyses were performed to account for the uncertainty in structural and methodological decisions. Probabilistic sensitivity estimates the probability of cost-effectiveness, given the joint uncertainty in the input parameters, and accounts for the small sample sizes used in the model. Expected Value of Information was used to quantify the benefit of a reduction in uncertainty and guide further research.
Clearly, small sample sizes impact the degree of confidence in the results obtained from both trial-based and model-based analyses. Further caution is warranted, given the results of the imputed analysis over 12-months suggest the ICER is close to the £30,000 WTP threshold for QALY. The intention-to-treat analyses also contain a high degree of imputation, reflective of the small sample sizes returning complete data in the trial (n=67 for 6-months and n=43 for 12-months) dictating that the results should be treated with caution.
The generalisability of the results should be considered within the context of the trial population (see Appendix 8); almost exclusively COPD D patients, and only patients with COPD D entered the model cohort. In other words, similar results may not be obtained for the other groups.
Future Research
Although early evidence is promising, more evidence on the long-term impact of COPDPredict™ based on a large cohort of patients is required to inform economic analyses. The Expected Value of Perfect Parameter information shows that there is significant value in further research regarding long-term transitions when using the intervention, as well as evidence from larger sample sizes regarding mortality. Meanwhile, deterministic sensitivity analyses demonstrate the need to obtain more information regarding the assumptions within the model, eg long-term reduction in bed days, maintenance of improved starting states, and long-term costs. The model-based analysis only runs for 5-years given the period the intervention is likely to impact cost-effectiveness, and any further benefit is not modelled here.
Currently, most of the patients in the trial had COPD D; hence, little is known about the effectiveness of the trial in other COPD severity grades. Future trials should look to improve the knowledge about the behaviour of the intervention in this patient group, which would also facilitate modelling of this group.
Conclusion
COPDPredict™ appears to be cost-effective for patients with COPD over the short- and long-term, up to a 5-year time horizon. Cost-effectiveness is potentially greater in more frequent hospitalised exacerbators. Uncertainty remains around the cost-effectiveness of the intervention, given the small sample sizes and the use of assumptions; further work is required.
Data Sharing Statement
All data relevant to the modelling study are included in the article or uploaded as supplementary information. We do not intend to share primary individual participant data for the trial-based analysis.
Ethics Statement
Ethical approval for the study was granted by the Stanmore Research Ethics Committee, London. Rec ref number: 19/LO/1939. Informed consent was obtained from all study participants. Guidelines outlined in the Declaration of Helsinki were followed.
The name of the approving Research Ethics Committee (REC) does not match with any of the author affiliations as in the UK any ethics committee across the country can approve a study, irrespective of where the applicants are based. The approval then stands for every site in the UK that might want to recruit, which is efficient for multisite studies like this one.
Predict and Prevent Trial Registration
Full title “The use of a personalised early warning decision support system with novel saliva bio-profiling to predict and prevent acute exacerbations of Chronic Obstructive Pulmonary Disease - ‘Predict & Prevent AECOPD’” Clinicialtrials.gov Identifier NCT04136418.
Acknowledgments
We would like to acknowledge the staff at all sites recruiting to the study, specifically University Hospitals Birmingham, University Hospitals Coventry and Warwickshire, University Hospitals Derby, Royal Alexandra Hospital, and Barts Health NHS Foundation Trust.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Institute for Health Research (NIHR) under its Invention for Innovation (i4i) Programme (Grant Reference Number NIHR200002). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health. The National Institute of Health Research (who funded the study) had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or decision to submit the results for publication.
Disclosure
Mrs Eleni Gkini reports grants from NIHR200002, during the conduct of the study.AT received grants or honoraria from multiple companies involved in COPD, specifically, AstraZeneca, GSK, Chiesi, CSL Behring, Boehringer, Grifols, Vertex, and Takeda.
MS was a Professor of Respiratory Medicine at the University Hospitals of North Midlands NHS Trust at the time of the above study and is a co-founder and director of NEPeSMO Limited and named inventor of COPDPredict-related granted patents. NP is a co-founder and director of NEPeSMO Limited. The authors report no other conflicts of interest in this work.
References
1. Safiri S, Carson-Chahhoud K, Noori M. et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990-2019: results from the Global Burden of Disease Study 2019. BMJ. 2022;378:e069679. doi:10.1136/bmj-2021-069679
2. National Institute for Health and Care Excellence (NICE) 2023. Quality standards and indicators briefing paper, Chronic Obstructive Pulmonary Disease update. Available from: https://www.nice.org.uk/guidance/qs10/documents/briefing-paper#:~:text=One%20in%20eight%20130%2C000%20emergency,be%20readmitted%20within%20three%20months.
3. British Lung Foundation. The Battle For. Breath – The Impact of Lung Disease in the UK. British Lung Foundation. 2016.
4. Echevarria C, Steer J, Heslop-Marshall K, et al. The PEARL score predicts 90-day readmission or death after hospitalisation for acute exacerbation of COPD. Thorax. 2017;72(8):686–693. doi:10.1136/thoraxjnl-2016-209298
5. NHS England (2022) Respiratory High Impact Interventions. Available from: https://www.england.nhs.uk/wp-content/uploads/2022/12/B1590-respiratory-high-impact-interventions.pdf.
6. McLean S, Hoogendoorn M, Hoogenveen RT. Projecting the COPD population and costs in England and Scotland: 2011 to 2030. Sci Rep. 2016;6(1):31893. doi:10.1038/srep31893
7. National Institute for Health and Care Excellence (NICE) 2023. Chronic Obstructive Pulmonary Disease Management Available from: https://www.nice.org.uk/cks-uk-only.
8. Kaur D, Mehta RL, Jarrett H, et al. Phase III, two arm, multi-centre, open label, parallel-group randomised designed clinical investigation of the use of a personalised early warning decision support system to predict and prevent acute exacerbations of chronic obstructive pulmonary disease: ‘Predict & Prevent AECOPD’ – study protocol. BMJ Open. 2023;13:e061050.
9. Gkini E, Rajnikant LM, Tearne S, et al. (2024) Use of a personalised early warning decision support system for acute exacerbations of chronic obstructive pulmonary disease: results of the ‘Predict & Prevent’ phase III trial, 18 July 2024, PREPRINT (Version 1). Research Square. doi:10.21203/rs.3.rs-4616866/v1.
10. National Institute for Health and Care Excellence (NICE) 2012. Cost effectiveness guidelines manual. Available from: https://www.nice.org.uk/process/pmg6/chapter/assessing-cost-effectiveness.
11. Department of Health and Social Care (2023) NHS 2021–22 reference costs [online]. Available from: https://www.england.nhs.uk/publication/2021-22-national-cost-collection-data-publication/.
12. Department of Health and Social Care (DoHSC, 2023a) NHS 2021–22 Electronic Drug Tariff. Available from: https://www.drugtariff.nhsbsa.nhs.uk/#/00849298-DD/DC00849294/Home.
13. Personal Social Services Research Unit (PSSRU) (2022). Unit costs of health and social care 2021, 2022. Available from: https://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-of-health-and-social-care-2021/.
14. Sculpher M. The role of productivity costs. In: Drummond MF, Maguire A, editors. Economic Evaluation in Health Care: Merging Theory and Practice. New York: Oxford University Press; 2001:94–112.
15. van Hout B, Janssen MF, Feng YS, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–715. doi:10.1016/j.jval.2012.02.008
16. Hall J, Turner AM, Dretzke J, Moore D, Jowett S. Cost-effectiveness of domiciliary non-invasive ventilation in patients with chronic obstructive pulmonary disease. Thorax. 2021;77(10):976–986. doi:10.1136/thoraxjnl-2021-217463
17. Global Initiative for Chronic Obstructive Lung Disease (GOLD) (2017). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2017 report. Available from https://www.wms-GOLD-2017-FINAL.pdf.
18. Adab P, Fitzmaurice DA, Dickens AP, et al. Cohort Profile: The Birmingham Chronic Obstructive Pulmonary Disease (COPD) Cohort Study. Int J Epidemiol. 2017;46(1):23. doi:10.1093/ije/dyv350
19. Merinopoulou L, Raluy-Callado M, Ramagopalan S, MacLachlan S, Mona Khalid J. COPD exacerbations by disease severity in England. Int J Chron Obstruct Pulmon Dis. 2016;11:697–709.
20. National Institute for Health and Care Excellence. (2018). Chronic obstructive pulmonary disease in over 16s: diagnosis and management. Nice guideline [NG115]. Available from https://www.nice.org.uk/guidance/ng115.
21. National Institute for Health and Care Research. Schedule of Events Cost Attribution Template (SoECAT). Available from: https://www.nihr.ac.uk/documents/online-soecat-guidance/30396#glossary-of-terms.
22. Rayner L, Sherlock J, Creagh-Brown B, et al. The prevalence of COPD in England: an ontological approach to case detection in primary care. Respir Med. 2017;132:217–225. doi:10.1016/j.rmed.2017.10.024
 © 2025 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a
Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
© 2025 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a
Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the
original author and source are credited.
Recommended articles
Development and Validation of a Multivariable Exercise Adherence Prediction Model for Patients with COPD: A Prospective Cohort Study

Ricke E, Bakker EW
International Journal of Chronic Obstructive Pulmonary Disease 2023, 18:385-398
Published Date: 22 March 2023
Factors Associated with Non-Adherence to Self-Management Among Patients with Chronic Obstructive Pulmonary Disease: A Survey Using the Delphi Technique and Analytic Hierarchy Process
Choi JY, Ryu EJ
International Journal of Chronic Obstructive Pulmonary Disease 2024, 19:1247-1259
Published Date: 4 June 2024



