Back to Journals » Journal of Pain Research » Volume 18
The Degeneration of Paraspinal Muscles and Its Correlation with the Postoperative Clinical Outcomes Following Minimally Invasive Transforaminal Lumbar Interbody Fusion (MIS-TLIF)
Authors Hu W, Zhang K, Shi X, Yang G, Li A, Gao Y
Received 12 November 2024
Accepted for publication 25 March 2025
Published 5 April 2025 Volume 2025:18 Pages 1827—1836
DOI https://doi.org/10.2147/JPR.S506153
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor King Hei Stanley Lam
Weiran Hu,1,2 Kai Zhang,1,2 Xinge Shi,1,2 Guang Yang,1,2 Ang Li,1,2 Yanzheng Gao1,2
1Department of Spinal Cord Surgery, Henan Provincial People’s Hospital, Zhengzhou, Henan, 45003, People’s Republic of China; 2Department of Spinal Cord Surgery, People’s Hospital of Zhengzhou University, Zhengzhou, Henan, 45003, People’s Republic of China
Correspondence: Yanzheng Gao, Email [email protected]
Objective: This study aims to analyze the degeneration of paraspinal muscles after minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) surgery and its correlation with clinical outcome.
Methods: Retrospective analysis was conducted on data from patients who underwent single-segment MIS-TLIF surgery in our hospital. MRI examinations were performed before the operation, at 6 months, and at 12 months after the operation to evaluate changes in volume and steatosis of the psoas major muscle and lumbar posterior muscles. VAS scores and ODI were filled out at 12 months after the operation, and correlations between psoas volume, posterior muscle volume, steatosis rate, and clinical outcome were analyzed.
Results: After surgery, both the psoas major muscle and dorsal muscles of fused segments showed atrophy. The steatosis in the fusion segment improved significantly at 12 months compared to 6 months after surgery (29.7± 8.2 vs 20.6± 6.1, P< 0.05), while there was no improvement in adjacent segment muscle steatosis during the follow-up period. VAS score was strongly negatively correlated with lumbar posterior muscle of fused segments (r=− 0.819, P < 0.001), strongly positively correlated with steatosis of fused segments (r=0.868, P < 0.001), and moderately negatively correlated with psoas major muscle of fused segments (r=− 0.435). ODI index was moderately negatively correlated with lumbar posterior muscles (r=− 0.-512, P=0-004) as well as psoas major muscles (r=− 0402, P< 005). ODI index also had a moderate negative correlation with adjacent dorsal muscles (r=− 0478, P=002).
Conclusion: Continuous atrophy was observed in both psoas major muscle and lumbar posterior muscles of fused segments as well as adjacent segments. However, by the end of the 12-month period after the operation, an improvement in fatty degeneration was noted specifically in the lumbar posterior muscles of the fused segment. The volume and steatosis rate of lumbar posterior muscles were found to have a significant correlation with clinical outcome.
Keywords: paraspinal muscles, clinical outcome, MIS-TLIF
Introduction
Minimally invasive Transforaminal Lumbar Interbody Fusion (MIS-TLIF) has gained widespread utilization in the treatment of lumbar degenerative diseases.1 MIS-TLIF offers muscle protection, reduces paravertebral muscle damage, and facilitates faster recovery compared to traditional surgery.2 However, it is necessary to evaluate through imaging whether paravertebral muscle degeneration still occurs after MIS-TLIF. Quantitative investigations into the changes occurring in paravertebral muscles following MIS-TLIF are currently lacking.
Paraspinal muscles encompass lumbar posterior muscle and psoas major muscles. These muscles play a crucial role in maintaining spinal stability and providing power for spinal movement.3 The lumbar posterior muscle (LM) contributes to spinal stability maintenance while the erector spinae muscle aids in preserving spinal balance.4 Paravertebral muscle degeneration can lead to lumbar pain and instability, resulting in unfavorable clinical outcomes with increased rates of surgical failure and revision.5 In a biomechanical test conducted by Kang et al,6 it was proposed that when there is a 20% atrophy of paraspinal muscles, the axial pressure borne by the spine increases by 0.5 MPa.
Many scholars have conducted research on the degeneration of paravertebral muscles in lumbar spine surgery. Fu et al7 found that statically significant post-operative MFI change was only noted in erector spinae muscle at caudal adjacent level and L2-S1 mean global level. Conventional open surgery produces a greater area of decompression on follow up MRI than minimally invasive surgery. Han et al8 found through a meta-analysis that for postoperative pain, multifidus could also be an effective predictor for persistent low back pain after surgery (SMD = 0.17, 95% CI 0.02–0.31, p = 0.03).
Previous studies on MIS-TLIF have primarily focused on comparing its clinical advantages and disadvantages with open surgery.7 The assessment of muscle injury has often been limited to intraoperative blood loss and postoperative quality of life scores, lacking direct evidence of postoperative paravertebral muscle changes. However, the degeneration of paravertebral muscles also impacts surgical efficacy, making it crucial to identify these muscular changes in order to enhance surgical techniques.9 Therefore, this study aims to quantitatively evaluate the components of degenerative paravertebral muscles from an imaging perspective and explore their correlation with clinical outcome.
Method
Inclusion and Exclusion Criteria
Inclusion criteria: 1) Single-segment MIS-TLIF procedure. 2) Patients with complete follow-up data and postoperative magnetic resonance imaging (MRI) examination. 3) Patients aged between 40 and 50 years old. 4) Patients with a preoperative body mass index (BMI) ranging from 18.5 to 23.9 kg/m2, which may prevent the interference caused by elevated levels of adipose tissue in the patient’s musculature. 5) Patients with complete follow-up data and a minimum of 12 months of follow-up.
Exclusion criteria: 1) Multi-segmental disc herniation or spinal stenosis. 2) Lumbar spondylolisthesis and kyphoscoliosis. 3) Spinal nerve diseases. 4) Historical background of lumbar plexus block. 5) Patients who experience poor wound healing after surgery.
Perioperative Treatment Methods
All patients received MIS-TLIF surgery via the expandable channel. Unilateral decompression was employed if the preoperative symptoms were unilateral. If the contralateral side also presented symptoms, the unilateral laminotomy for bilateral decompression(ULBD) was adopted. During the operation, bilateral pedicle screws were fixed through the channel. Postoperatively, patients wore braces for more than two months as directed by the doctor’s orders. Subsequently, they initiated the exercise of the lumbar and back muscles under the guidance of the outpatient department. All patients received homogeneous rehabilitation training guidance.
The General Information
This is a retrospective cohort study. According to the inclusion criteria, a total of 50 patients were enrolled, including 22 males and 28 females. The average age was 44.7±4.6 years (41–50 years). Body mass index 22.9±1.5 kg/m2 (19.6–23.8 kg/m2); The median preoperative visual analogue scale (VAS) score was 7.3 (6–9). The median preoperative Oswestry disability index (ODI) was 71.4 (62.0–84.0). There were 32 patients with lumbar disc herniation, 14 patients with lumbar spinal stenosis, and 4 patients with lumbar instability. The surgical fusion level included L4/5 in 32 cases and L5/S1 in 18 cases. At the end of the 12 month post-operation, the median VAS score decreased to 3.2 points (ranging from 1 to 4), while the median ODI improved to a value of 12 0.4 (ranging from 6 0.0 to 24 0.0).
This study has been approved by the Medical Ethics Committee of Henan Provincial People’s Hospital (2021–173). Written informed consent was obtained from the patient. All researchers adhered to the principles outlined in the Declaration of Helsinki, and written informed consent was obtained from every participant.
The Study Outcome Measures
Evaluation indexes of paravertebral muscle mass: The paraspinal muscles were categorized into the lumbar posterior muscle (LM) and Psoas major muscle (Psoas). Muscle quality was assessed based on the extent of muscular development and the severity of fatty infiltration. The relative volume of paravertebral muscle was utilized to indicate the degree of muscular development, while the steatosis rate represented the severity of fatty infiltration.10 These evaluation parameters included lumbar dorsal muscle relative volume (LM%), Psoas major muscle relative volume (Psoas%), and fatty degeneration rate (FD%). Due to the differences in height and weight among individuals, the cross-sectional area of their vertebral bodies also varies. The ratio of LM/VB and Psoas/VB provide a uniform baseline for comparison among different individuals.
Imaging measurements of the paraspinal muscles were conducted on MRI images: The MRI image data were saved in DICOM format. Following the method proposed by Hyun et al11 for evaluating muscle area on MRI images. The MRI cross-sectional image was segmented, and the relative muscle volume was quantified based on the area of each muscle image segmentation. Fast spin-echo T2 weighted imaging (FSE T2WI) was performed using PiView software to measure the cross-sectional area of lumbar dorsal muscle, vertebral body (VB), and psoas major muscle. The cross-sectional area was calculated by contouring around it with a cursor. (Figure 1)
Calculation of paravertebral muscle steatosis: LM% is determined by calculating the ratio of the cross-sectional area of the dorsal muscle to that of the vertebral body (LM/VB). Similarly, Psoas% is calculated as the ratio between its cross-sectional area and that of the vertebral body (Posas/VB). To assess fatty degeneration in lumbar dorsal muscles, we employed a method proposed by Jun et al.10 Image J software was utilized to calculate and analyze pixel gray levels in both paraspinal muscles and subcutaneous fat areas within images. FD% was measured by determining the number of pixels with fatty degeneration in relation to total pixels present in lumbar dorsal muscles.
The cross-sectional MRI images of the fusion level and the intervertebral disc level at the adjacent segment were selected preoperatively, as well as at 6 and 12 months postoperatively. Following image segmentation, measurements were obtained for the cross-sectional areas of LM, Psoas and vertebral bodies. Subsequently, calculations were performed to determine LM%, Psoas%, and FD% for both the fusion level and adjacent segments. The final value was derived by averaging these two measurements.
The Clinical Outcomes
The clinical outcomes was assessed using the Visual Analog Scale (VAS) score and Oswestry Disability Index (ODI) at 12 months post-surgery. All the scores are filled in by the patients in a quiet environment.
Visual Analogue Scale (VAS) was used to assess pain and its severity on a scale of 0–10. The tested subject, using a straight horizontal line with a length of 10 cm, indicates the level of pain felt. The researcher then marks the indicated point. Range of 0–3 signifies no pain or weak pain, 4–6 signifies severe pain, and 7–10 a very strong to the strongest pain imaginable.12
Oswestry Disability Index (ODI) is the method for assessing disability caused by back pain. It contains 10 questions regarding: the intensity of pain and its variability, self reliance, weight lifting, ability to travel, sexual intercourse, rising from a sitting position, sleeping, walking, standing and sitting. Questions are scored on a scale of 0 to 5. The maximum number of points is 50. The result is presented on a scale of 0–50 points or as a percentage from 0–100%. Using Fairbank’s interpretation of ODI results, on a scale of 0–100%, five disability groups are determined: minimal 0–20%, moderate 21–40%, severe 41–60%, very serious 61–80% and exaggerated symptoms 81–100%.13
The Analysis of Correlation
The correlation between paravertebral muscle degeneration and clinical outcome is composed of two parts: the correlation between VAS score and the degeneration of paraspinal muscles and the correlation between ODI index and the degeneration of paraspinal muscles. The association between LM%, Psoas%, FD% and VAS score, as well as ODI index at the end of follow-up, was examined.
Statistical Methods
The Shapiro–Wilk test was employed to assess the normal distribution of measurement data using IBM SPSS 23.0. Measurement data demonstrating a normal distribution and homogeneity of variance were presented as x±s. Repeated measures analysis of variance (ANOVA) was utilized for comparing LM%, Psoas%, FD% and VAS score, ODI index at different time points, while the LSD-t test was applied for multiple comparisons. Pearson correlation analysis was conducted to examine the relationship between LM%, Psoas%, FD% and VAS score, ODI index, with the strength of association evaluated using the correlation coefficient (r). The absolute value of r ranged from 0.8–1.0 denoting an extremely strong correlation, 0.6–0.8 indicating a strong correlation, and 0.4–0.6 representing a moderate level of correlation respectively; whereas an r value ranging from 0 to 0.2 suggested very weak or no correlation existed between variables under investigation.11 A significance level of P < 0 0.05 was considered statistically significant.
Results
The LM% and Psoas% in the fusion segment exhibited a significant decrease at 6 and 12 months post-operation compared to pre-operative levels (P < 0.05). However, there was no statistically significant difference between measurements taken at 6 and 12 months after surgery (P > 0.05). The FD% of the fusion segment significantly increased at both time points compared to pre-operative values (P < 0.05), with a higher increase observed at 6 months than 12 months (P < 0.05). These findings indicate muscle atrophy in the LM and Psoas within the fusion segment following surgery, which does not show significant recovery during the follow-up period. Additionally, steatosis improves by 12 months post-surgery when compared to 6 months. (Table 1 and Figure 2A)
The adjacent segments of LM% and Psoas% showed a significant decrease at 6 and 12 months post-operation (P < 0.05). However, there was no significant difference between the measurements taken at 6 months and those obtained at 12 months after surgery (P > 0.05). The FD% of adjacent segments significantly increased compared to pre-operative levels (P < 0.05). Nevertheless, there was no significant difference in FD% between 6 months and 12 months post-operation (P > 0.05). The LM and Psoas muscles of adjacent segments exhibited postoperative atrophy, while steatosis did not show improvement during the follow-up period. (Table 2 and Figure 2B)
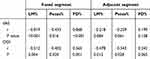
The VAS score exhibited a strong negative correlation with the LM% (r=−0.819, P < 0.001), FD% (r=0.868, P < 0.001), and a moderate negative correlation with the Psoas% (r=−0.435, P=0.016). The ODI showed a moderate negative correlation with the LM% (r=−0.512, P=0.004) and Psoas% (r=−0.402, P= 0.020), and a moderate positive correlation with the FD% (r=0.565, P=0.001). The most closely related to clinical outcome were LM% and FD% of the fusion segment, followed by Psoas% of the fusion segment.(Figure 3A and B)
There was no correlation between VAS score and LM%, Psoas% and FD% of adjacent segments (P > 0.05). ODI was negatively correlated with LM% (r=−0.478, P=0.012) and weakly correlated with Psoas% (r=−0.343, P=0.028). The most significant effect on clinical outcome was LM% of adjacent segments. (Table 3, Figure 3C and D)
Discussion
There are numerous factors that influence the efficacy of lumbar spine surgery.1 Previous studies have predominantly focused on surgical factors and postoperative fusion, with limited attention given to the impact of paravertebral muscles on postoperative outcomes. The primary objective of MIS-TLIF technology is to minimize muscle damage during lumbar fusion surgery. However, some patients still experience muscle atrophy following MIS-TLIF, which subsequently contributes to reduced satisfaction due to postoperative low back pain.14 Therefore, it is worth investigating whether there exists a correlation between residual symptoms after surgery and degeneration of the low back muscles.
Muscle injury and degeneration frequently result in persistent low back pain following surgery.15 Research has indicated that deep muscle tissue damage can lead to long-term postoperative pain, often accompanied by chronic inflammation.16 Quantitative assessment of muscle degeneration is valuable for objectively understanding intraoperative injuries and postoperative muscular changes. Cross-sectional MRI images effectively depict the contour of paravertebral muscles, while alterations in image signal intensity on T2-weighted images can indicate the extent of fat infiltration.17 Hyun et al11 proposed a method for measuring the area of the psoas major muscle, erector spinae muscle, and multifidus muscle on MRI images through image segmentation. The authors utilized the cross-sectional area of the vertebral body as a reference point and employed the ratio between muscle area and vertebral body area as a parameter to evaluate paraspinal muscles’ condition. Furthermore, this study draws inspiration from this method.
The LM% and Posas% of the fusion segment exhibited a decrease to 89.3% and 85.7%, respectively, at the 6-month postoperative mark. Similarly, the LM% and Posas% of adjacent segments experienced a decline to 85.5% and 91.2%, respectively, at the same time point after surgery. This study provides evidence demonstrating a reduction in paravertebral muscle volume following surgical intervention, with no observed trend towards improvement in muscle volume during the subsequent 12-month follow-up period. Figure 4 presents pre- and post-operative MRI images of the lumbar muscles.
Some studies suggest a proportional relationship between the volume of paravertebral muscles and the isometric contraction force of the lumbar spine.18 Simultaneously, a decrease in muscle volume directly leads to reduced support strength of the paravertebral muscles, resulting in increased pressure load on the spine. Salimi et al19 discovered through bioelectrical impedance experiments that dorsal muscle volume exhibited a positive correlation with bioelectrical impedance (r=0.752), indicating that decreased dorsal muscle volume would weaken trunk strength. According to the findings of this study, postoperative patients experienced continuous atrophy in their dorsal and psoas major muscles during the follow-up period, signifying a significant decline in lumbar support strength after surgery.
The findings of this study revealed a persistent rate of paravertebral muscle steatosis following fusion segment surgery. Although the steatosis rate at 12 months post-surgery demonstrated improvement compared to that at 6 months, it remained elevated relative to the preoperative level, indicating an inability for the muscle steatosis rate to fully revert back to its initial state. Furthermore, there was a significant increase in the steatosis rate of adjacent segments at both 6 and 12 months after surgery (P < 0.05), with no statistically significant difference observed between these two time points (P > 0.05). These results suggest that post-operative steatosis in adjacent segments continues to worsen and does not improve during the follow-up period.
The occurrence of muscle steatosis can be attributed to intraoperative injury.20 However, the presence of a stable repair environment does not ameliorate the steatosis in adjacent segments. Previous research has demonstrated that post lumbar spine surgery, axial stress is uniformly distributed to neighboring segments, resulting in a 25% increase in muscle stress within these segments after lumbar fusion.21 This redistribution of axial stress may induce alterations in muscle morphology within adjacent segments, potentially accounting for the persistently elevated rate of steatosis observed.
The variables most strongly associated with clinical outcome score were the LM% in the fusion segment (r=−0.819, P=0.000) and the FD% in that same segment (r=0.868, P=0.000). In adjacent segments, the variable most closely related to postoperative clinical outcome score was the LM% (r=−0.4784, P=0.008). Both the Posas% in both fusion and adjacent segments showed a negative correlation with clinical outcome.
The reduction in muscle volume will impact the normal physiological function of the lumbar spine, subsequently affecting the clinical outcomes.22 The LM plays a crucial role in maintaining sagittal balance and providing power for the lumbar spine’s normal physiological activities. Anatomical studies demonstrated that LM volume is directly proportional to lumbar spine mobility.23 The continuous decrease in dorsal muscle volume post-surgery indicates a persistent decline in lumbar spine mobility among patients. Seyedhoseinpoor et al,24 through finite element analysis modeling, discovered that reduced LM results in a 30% increase in energy consumption during lumbar spine motion. This implies that patients undergoing MIS-TLIF surgery require more energy for lumbar movement, which may contribute to the decline in clinical outcome.
Meanwhile, relevant literature has also compared the muscle damage caused by MIS-TLIF and OPEN-TLIF. Hu et al25 found that there were no significant differences in blood loss postoperative creatine kinase content between the two methods (p > 0.05). Baharat et al26 conducted that mean reduction in lean muscle mass of multifidus muscle was greater in OPEN-TLIF group as compared to MIS-TLIF. There was greater reduction in lean muscle mass in females and on side of cage insertion. Subsequently, we will also conduct a research on the imaging assessment of the differences between the two to better evaluate the long-term advantages and disadvantages of the two surgical methods.
This study still has limitations. Firstly, the inclusion of cases was restricted in number. Despite the fact that all MRI examinations in this study underwent artifact removal correction, the presence of implants may still impact the experimental outcomes. Secondly, there is a limitation on follow-up time and paraspinal muscle degeneration may vary over time. Additionally, to minimize confounding factors’ influence on the experimental results, this study imposed restrictions on BMI and age for included patients while excluding those with excessive body weight. Lastly, it should be noted that this study is a single-center retrospective study where surgeons’ experience and operating habits might have influenced the research findings.
Conclusion
The MIS-TLIF procedure resulted in a reduction in paraspinal muscle volume and the presence of fat deposits in the dorsal muscles. However, at the fusion level, there was an improvement in FD% after 12 months of follow-up, while no significant improvement was observed at the adjacent level during this period. Furthermore, clinical outcome was found to be closely associated with both LM% and FD% at the fusion level.
Data Sharing Statement
All of the data are described in the manuscript. Data available on request from the corresponding author.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Science and technology Research program of Henan Province (242102310107) and the Medical Science and technology research program of Henan Province (LHGJ20240006). Natural science foundation of Henan province (232300421284).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Choll WK. MIS TLIF, EndoTLIF, and the ability of navigation/robotics to enable spinal surgery in an ambulatory care setting. Global Spine J. 2022;12:34S–9S.
2. Sara L, Christoph W, R Nick H, et al. Defining the MIS-TLIF: a systematic review of techniques and technologies used by surgeons worldwide. Global Spine J. 2020;10:151S–67S.
3. Tom AR, Flavia MC, Tue SJ, et al. Are the size and composition of the paraspinal muscles associated with low back pain? A systematic review. Spine J. 2017;17(11):1729–1748.
4. Leonid K, Eli C, Ella B. The association between imaging parameters of the paraspinal muscles, spinal degeneration, and low back pain. Biomed Res Int. 2017;2017:2562957.
5. Andrew JH, Tyler JM. Anatomical study and proposed EMG technique for the cervical paraspinal muscles. PM R. 2023;16(2):165–173.
6. Sungwook K, Min Cheol C, Hwanjin K, et al. The effects of paraspinal muscle volume on physiological load on the lumbar vertebral column: a finite-element study. Spine. 2021;46(19):E1015–21.
7. Chen-Ju F, Wen-Chien C, Meng-Ling L, Chih-Hsiu C, Chi-Chien N. Comparison of paraspinal muscle degeneration and decompression effect between conventional open and minimal invasive approaches for posterior lumbar spine surgery. Sci Rep. 2020;10(1):14635.
8. Gengyu H, Haotian W, Jinyue D, et al. Does paraspinal muscle morphometry predict functional status and re-operation after lumbar spinal surgery? A systematic review and meta-analysis. Eur Radiol. 2023;33(8):5269–5281.
9. Hitesh NM, Utsab S. Comparison of clinical outcome and radiologic parameters in open TLIF versus MIS-TLIF in single- or double-level lumbar surgeries. Int J Spine Surg. 2021;15(5):962–970.
10. George D, Panayota M, Vaia L, Eirini M, Sotirios AR. Insulin effects in muscle and adipose tissue. Diabet Res Clin Pract. 2011;93:S52–9.
11. Hyun SJ, Bae CW, Lee SH, Rhim SC. Fatty degeneration of the paraspinal muscle in patients with degenerative lumbar kyphosis: a new evaluation method of quantitative digital analysis using MRI and CT scan. Clin Spine Surg. 2016;29(10):441–447. doi:10.1097/BSD.0b013e3182aa28b0
12. Mimmi Å, Zin Min TL, Fitsum Sebsibe T, Kristina B, Jenny B. Use of the visual analogue scale for health state valuation: a scoping review. Qual Life Res. 2023;32(10):2719–2729.
13. Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25(22):2940–2953.
14. Jun Hao T, Gabriel L, Ruimin N, Nishant K, Hee-Kit W, Gabriel L. Is MIS-TLIF superior to open TLIF in obese patients?: a systematic review and meta-analysis. Eur Spine J. 2018;27(8):1877–1886.
15. Patrick S, Christa B, Lothar AS. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763–1768.
16. Jia Bin L, Jun Long W, Rui Z, Chang Qing L, Chao Z, Yue Z. Does MIS-TLIF or TLIF result in better pedicle screw placement accuracy and clinical outcomes with navigation guidance? BMC Musculoskelet Disord. 2022;23(1):153.
17. Kevin CJ, Madhav RP, Alexander WP, et al. The effect of the severity of preoperative back pain on patient-reported outcomes, recovery ratios, and patient satisfaction following minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF). World Neurosurg. 2021;156:e254–65.
18. Yoshiaki H, Shingo M, Shinichi I, et al. Preoperative low back pain affects postoperative patient satisfaction following minimally invasive transforaminal lumbar interbody fusion surgery. Asian Spine J. 2023;17(4):750.
19. Huanan L, Jiaqi L, Yapeng S, et al. A comparative study of a new retractor-assisted WILTSE TLIF, MIS-TLIF, and traditional PLIF for treatment of single-level lumbar degenerative diseases. Orthop Surg. 2022;14(7):1317–1330.
20. Olga NL, Evgeny AC, Aleksandr VK. MIS-TLIF versus O-TLIF for single-level degenerative stenosis: study protocol for randomised controlled trial. BMJ Open. 2021;11(3):e041134.
21. Salimi H, Ohyama S, Terai H, et al. Trunk muscle mass measured by bioelectrical impedance analysis reflecting the cross-sectional area of the paravertebral muscles and back muscle strength: a cross-sectional analysis of a prospective cohort study of elderly population. J Clin Med. 2021;10(6):1187. doi:10.3390/jcm10061187
22. Jin-Sung K, Byungjoo J, Sang-Ho L. Instrumented minimally invasive spinal-transforaminal lumbar interbody fusion (MIS-TLIF): minimum 5-year follow-up with clinical and radiologic outcomes. Clin Spine Surg. 2012;31(6):E302–9.
23. Shengxiang A, Wenjie Z, Junlong W, et al. Comparison of Preliminary clinical outcomes between percutaneous endoscopic and minimally invasive transforaminal lumbar interbody fusion for lumbar degenerative diseases in a tertiary hospital: is percutaneous endoscopic procedure superior to MIS-TLIF? A prospective cohort study. Int J Surg. 2020;76:136–143.
24. Seyedhoseinpoor T, Taghipour M, Dadgoo M, et al. Relationship between the morphology and composition of the lumbar paraspinal and psoas muscles and lumbar intervertebral motion in chronic low-back pain: an exploratory study. Clin Anat. 2022;35(6):762–772. doi:10.1002/ca.23893
25. Weiran H, Guang Y, Hongqiang W, et al. Which is better in clinical and radiological outcomes for lumbar degenerative disease of two segments: MIS-TLIF or OPEN-TLIF? J Pers Med. 2022;12(12).
26. Bharat RD, Nandan M, Shivanand M, et al. Does Conventional Open TLIF cause more muscle injury when compared to minimally invasive TLIF?-A prospective single center analysis. Global Spine J. 2022;14(1). doi:10.1177/21925682221095467
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.