Back to Journals » Journal of Experimental Pharmacology » Volume 17
The Effects of the Ethanol Extract of Allium Ascalonicum L. in High-Fat-High-Fructose-Induced Insulin Resistance Swiss-Webster Male Mice
Authors Elkanawati RY, Sumiwi SA, Levita J
Received 13 January 2025
Accepted for publication 9 April 2025
Published 16 May 2025 Volume 2025:17 Pages 207—221
DOI https://doi.org/10.2147/JEP.S513301
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Abdelwahab Omri
Rani Yulifah Elkanawati,1,* Sri Adi Sumiwi,2,* Jutti Levita2,*
1Faculty of Pharmacy, Universitas Padjadjaran, Sumedang, West Java, Indonesia; 2Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Sumedang, West Java, Indonesia
*These authors contributed equally to this work
Correspondence: Jutti Levita, Department of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Jl. Raya Bandung-Sumedang km 21, Sumedang, West Java, 45363, Indonesia, Email [email protected]
Background: Insulin resistance (IR) is a condition where the body cannot respond properly to insulin, leading to elevated blood glucose and the development of type 2 diabetes mellitus (T2DM). The first-line anti-T2DM drug is metformin, however, it has shown adverse effects, challenging the search for alternative natural drugs. Plant flavonoids stimulate cellular glucose uptake, decrease hyperglycemia, and regulate key signaling pathways in glucose metabolism. Brebes shallots (Allium ascalonicum L.) are known to contain flavonoids and thus may have the potential to inhibit IR.
Purpose: To evaluate the effects of the ethanol extract of Brebes shallots in improving IR conditions.
Methods: Brebes shallots were collected from West Java, Indonesia. 500 g of the shallots were oven-dried and extracted using 70% ethanol for 3× 24 h, the solvent was evaporated to a thick consistency, and the extract was abbreviated as EAA. The effects of EAA were studied in high-fat-high-fructose (HFHF)-induced Swiss-Webster male mice by performing the insulin tolerance test (ITT) and oral glucose tolerance test (OGTT), and the liver and pancreas index. The nutritional composition and quercetin levels in the extract were also determined.
Results: The extraction process yielded a 28.1% EAA. EAA reduces % weight gain, blood glucose levels in OGTT, and liver and pancreas index. EAA significantly improved insulin tolerance in the HFHF-induced mice (p < 0.05). Proximate analysis resulted in 3.92% ash, 0.12% fat, 13.45% protein, and 60.69% carbohydrate, while quercetin was at 0.0065%.
Conclusion: Allium ascalonicum L. extract may improve IR conditions as confirmed by its ability to increase the ITT value and reduce blood glucose levels. However, further studies are needed to confirm its role in alleviating metabolic disorders.
Keywords: Allium sp, diabetes mellitus, flavonoids, hypoglycemia, insulin resistance, quercetin
Introduction
Insulin resistance (IR), characterized by the unresponsiveness of cells to insulin, has commenced to become the focus of metabolic disorder studies.1,2 It greatly impacts global public health, in particular, due to unhealthy and sedentary lifestyles.2,3 IR is the major factor in the development of type 2 diabetes mellitus (T2DM), which is alarmingly increased worldwide. It was estimated in 2021 that 537 million people have diabetes, and this number is projected to reach 643 million by 2030, and 783 million by 2045. Of those, Indonesia was ranked 5th, after China, India, Pakistan, and the USA as the 1st, respectively.4 DM is signed by elevated blood glucose levels, known as hyperglycemia,5 arising when the body fails to produce or effectively use insulin.6 Insulin, secreted by pancreatic Langerhans beta-cells, works by controlling blood glucose levels, facilitating cell respiration in the mitochondria, and metabolizing protein and fat.1,7 A cross-sectional study involving 402 patients with T2DM in Nantong, China, described that a sedentary lifestyle may independently account for the increase in body fat percentage and the decrease in appendicular skeletal muscle mass.8 Another study of changes in adipocyte size distribution in response to 8 weeks of overfeeding in 22 males suggested that during substantial weight gain, an increase in small adipocytes may link to impaired metabolic health outcomes.9 Therefore, the risk factors of T2DM may include high-carbohydrate and high-fat intake, lack of physical activity, high blood pressure (≥ 140/90 mmHg), low high-density lipoprotein (< 35 mg/dL) and/or triglyceride (> 250 mg/dL), and obesity.8–10 An increased production of free fatty acids (FFAs), reactive oxygen species (ROS), and proinflammatory cytokines may contribute a role in the pathogenesis of IR. FFAs and dietary lipids in excessive levels could enter the cells of non-adipose organs, such as the liver, muscle, and pancreas, and are deposited as ectopic fat, thus leading to lipotoxicity.11
Metformin, the first-line pharmacotherapy for managing T2DM, increases insulin sensitivity, decreases IR, and suppresses hepatic gluconeogenesis,12 by enhancing adenosine monophosphate-activated protein kinase activity in the liver.13 Other oral antidiabetic drugs, such as sulfonylureas, bind and inhibit the ATP-sensitive potassium channel, which eventually changes the resting membrane potential of the cell, causes an influx of calcium, stimulates the release of insulin from pancreatic β-cells, and reduces blood glucose levels.13 Sulfonylureas are given as the first-line medication of choice for patients who are intolerant to metformin. Unfortunately, the risk of the failure of sulfonylurea as a monotherapy agent is higher than that of metformin.14 Sulfonylureas interact with salicylates, sulfonamides, and warfarin, and the major adverse events are a greater risk of hypoglycemia and weight gain. The American College of Physicians (ACP) suggests that for patients with T2DM, a combination of either a sulfonylurea, a thiazolidinedione, an SGLT-2 (sodium-glucose cotransporter-2) inhibitor, or a DPP-IV (dipeptidyl peptidase-IV) inhibitor to metformin, is required to control blood glucose levels. Moreover, it was described that metformin therapy was linked with lesser cardiovascular mortality than sulfonylureas, and the evidence of metformin therapy to reduce HbA1c levels was reported better than that of DPP-IV inhibitors.15 However, metformin, the biguanide drug, was reported in several cases to affect sleep quality and cause lactate acidosis, thus, patients taking metformin should be assessed for their kidney performance, blood pH, and blood metformin level.14 Thiazolidinediones exert their hypoglycemic effects by activating the peroxisome proliferator-activated receptor gamma (PPARγ), decreasing the IR damage, and increasing the response of pancreatic β-cells towards blood glucose levels. It was reported that thiazolidines may elevate the risk of cardiovascular disease, weight gain, water retention, and edema.15,16 Rosiglitazone, a thiazolidinedione, was withdrawn due to its disadvantageous effects on the bones and the heart.17 Therefore, maintaining a normal range of blood glucose levels remains challenging, and numerous remedies, such as plant products for adjuvant therapy have been found interesting.
A study confirmed that turmeric supplementation at a dose of 2 g/day for 4 weeks as an adjuvant to 60 male T2DM patients on metformin, had significantly reduced their fasting glucose, HbA1c, lipid peroxidation, and malondialdehyde levels.18 Moreover, a systematic review and meta-analysis study on the effect of Chinese herbal formulas combined with metformin on T2DM patients reported better efficacies than metformin monotherapy in regulating the gut microbiota, decreasing HbA1c, fasting plasma glucose, 2-hour postprandial blood glucose, fasting insulin, and homeostasis model assessment of insulin resistance (HOMA-IR).19 Herbal adjuvant therapy for T2DM patients combined with mild cognitive impairment was effective and did not significantly increase the adverse effects.20 The consumption of herbal teas as adjuvant therapy on T2DM patients was reported to improve insulin resistance, protect islet β-cells, inhibit glucose absorption, and suppress gluconeogenesis.21 A double-blind, randomized, placebo-controlled trial evaluating the effects of Ginkgo biloba extract (120 mg/day) as an adjuvant to metformin in 62 patients with uncontrolled T2DM revealed that the extract significantly reduced blood HbA1c (p < 0.001), glucose (p < 0.001) and insulin (p = 0.006) levels, BMI (p < 0.001), waist circumference (p < 0.001), and visceral adiposity index (p = 0.007), and did not damage the liver, kidney, or hematopoietic functions.22 A quasi-experimental study in T2DM patients supplemented with 500 mg of Gymnema sylvestre herb daily for 3 months showed reduced polyphagia, fatigue, blood glucose, HbA1c, and lipid profiles.23
Fruits and herbs have been reported to have multiple health benefits, particularly flavonoids, which are widely studied for their antidiabetic activities.24 The hypoglycemic activity of flavonoids contributes to regulating carbohydrate digestion, insulin signaling, insulin secretion, glucose uptake, and adipose deposition.25
Brebes shallots (Allium ascalonicum L., Amaryllidaceae family) were reported to contain flavonoids, saponins, tannins, terpenoids, and volatile oils.26 The main subclasses of flavonoids present in Allium sp. are flavonols, such as quercetin, kaempferol, isorhamnetin, fisetin, myricetin, and morin, whose content ranges from 0.0007 to 0.1917% w/w of fresh weight.27 Total flavonoids in the ethanol extract and ethyl acetate fraction of A. ascalonicum L. were 13.493 ± 0.018 mg of quercetin equivalence (QE)/g or 1.3493% w/w and 96.776 ± 0.015 mg QE/g or 0.96776% w/w, respectively.28 Quercetin was reported to be present in A. ascalonicum L. peels with a main α-glucosidase inhibitory activity, with an IC50 value of 0.012 ± 0.002 mg/mL for the ethyl acetate extract and 0.047 ± 0.04 mg/mL for the methanol extract. This inhibition slows glucose absorption, thus reducing blood glucose levels.29 Other studies have delineated the antiobesity and IR-suppressing activity of red onion extracts on a high-fat diet (HFD)-induced obesity C57BL/6J mice.30,31 Moreover, the kaempferol glycoside-enriched butyl alcohol fraction of Allium tuberosum has decreased blood glucose levels by improving serum lipid profile and antioxidant parameters in alloxan-induced diabetic rats.32
Considering everything, this study aimed to evaluate the effect of ethanol extract of A. ascalonicum L. in improving IR conditions in high-fat-high-fructose (HFHFD)-induced Swiss-Webster male mice.
Methods
Plant Materials and Preparation of the Ethanol Extract of Allium Ascalonicum (EAA)
Fresh Brebes shallot bulbs in their maturation stage (Figure 1) were collected from Brebes, Central Java, Indonesia (6°53′42,1″S 108°51′48,5″E), and were authenticated by Arifin Surya Dwipa Irsyam (https://www.scopus.com/authid/detail.uri?authorId=57211286941; https://herbarium.sith.itb.ac.id/profil-kurator/), a certified botanist at the School of Life Sciences and Technology, Bandung Institute of Technology (Bandung, West Java, Indonesia), (https://herbarium.sith.itb.ac.id/koleksi/). The material was confirmed to be Allium ascalonicum L. of the family Amaryllidaceae (document number 534/IT1.C11.2/TA.00/2024) with characteristics that matched those described in the reference.33
 |
Figure 1 Fresh Brebes shallot bulbs in their maturation stage, collected from Brebes, Central Java, Indonesia. |
EAA was prepared by following previously described methods with modifications.26,28,34 In brief, 5 kg of fresh A. ascalonicum bulbs were examined and their dry layers were manually removed. The bulbs were washed under running water to remove dirt and other contaminants, thin-sliced using an electric food processor (https://www.idealife-online.com/), dried in a vacuum oven at 40 °C (SHEL LAB), ground into a coarse powder, and sieved using a Mesh-60 sieve to ensure particle uniformity, resulting in a weight of 520 g. Approximately 500 g of the coarse powder was cold extracted using 70% ethanol, a universal solvent, at a ratio of 1:10 (w/v) for 3×24 h. The liquid extracts were collected and filtered, and the solvent was evaporated in a vacuum rotary evaporator (Büchi) at 50 °C, 40 rotations per minute until a viscous extract of EAA was yielded (21.8% w/w).
Analysis of the Nutritional Composition and Quercetin Levels in the Extract
The nutritional composition of EAA was determined by following the Official Methods of Analysis 2023 (https://www.aoac.org/official-methods-of-analysis/).35 The quercetin levels in EAA were analyzed by thin layer chromatography (TLC)-densitometry following a method previously described by Doshi and Une et al in 2016.36 Approximately 5 g of EAA was placed in an evaporating dish and dissolved in 50 mL of ethanol, and similarly 10 mg of quercetin standard in 10 mL of ethanol. Both standard solution and samples were filtered using Whatman filter paper no. 41 before spotting onto a TLC plate (Silica gel 60 F254, 10 cm), with varying concentrations of quercetin standard (250, 500, 750, 1000, and 1250 µg/mL). The plate was inserted into a chamber saturated with a mixture of toluene: ethyl acetate: and formic acid (5:4:0.5) as the mobile phase, eluted, dried, observed under UV light at 254 nm, and analyzed using TLC-Densitometry at 320 nm. The data for each peak, including area and Rf values, were recorded, and the concentration of quercetin was quantified using a linearity standard addition curve.
Animals and Ethical Approval
In this study, we used 24 adult male Swiss-Webster mice (20–30 g), obtained from the Experimental Animal Laboratory, Bandung Institute of Technology, West Java, Indonesia. The mice were randomly assigned to six groups (n = 4 per cage, as derived from the Federer formula for sample size in animal experimental design: (T-1) (N-1) > 15, where T represents the number of groups and N is the number of samples per group), in a room set at temperatures of 25 ± 2 °C, under a 12 h light, 12 h dark cycle, and 55% relative humidity. The cages were cleaned and the husks were replaced every three days. The mice were given standard feed (70 g/cage), containing water 12%, protein 20%, fat 4%, fiber 4%, calcium at 12%, phosphor 0.7%, and free access to fresh water, during 7 days of acclimatization. The health condition and behavior of the mice were observed during the adaptation and in vivo study. The animal handling procedure is approved by the Research Ethics Committee, Universitas Padjadjaran, Indonesia (https://kep.unpad.ac.id/; approval documents number 799/UN6.KEP/EC/2024), which strictly follows The Guide for the Care and Use of Laboratory Animals (NRC 2011; eighth edition) (https://grants.nih.gov/grants/olaw/guide-for-the-care-and-use-of-laboratory-animals.pdf).37
In this animal study, we employed 3 control groups, (1) the normal control which did not receive inducement or the treatment being studied (drug or extracts), (2) the negative control which was diabetic-induced but did not receive the treatment being studied, and (3) the positive control which was diabetic-induced and received standard drug treatment. The normal control is crucial for establishing a baseline, illustrating normal conditions without induction and treatment, and ensuring that observed changes are due to the treatment and not to other factors. The negative control group assesses the success of induction and the disease’s development without treatment. The positive control group validates the method used, demonstrating the expected effect. If the results in the positive control group align with the expected, it signifies the procedure was executed correctly and the test results are considered valid.
Effects of EAA on Blood Glucose Levels by Oral Glucose Tolerance Test
The effects of EAA on glucose tolerance were studied in vivo in mice at the Pharmacology Laboratory of the Faculty of Pharmacy, Universitas Padjadjaran, Indonesia. After the acclimatization period, the mice were fasted for 14 h and randomly grouped as follows: (1) the normal group (treated with sodium carboxy methyl cellulose 0.5% suspension); (2) the negative control or glucose-induced group (induced with 3 g of glucose in sodium carboxy methyl cellulose 0.5% suspension); (3) the positive control or drug control group (treated with acarbose 25 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension and induced with 3 g of glucose); (4) the test-1 group (treated with EAA 100 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension and induced with 3 g of glucose); (5) test-2 group (treated with EAA 200 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension and induced with 3 g of glucose); (6) test-3 group (treated with EAA 400 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension and induced with 3 g of glucose). Acarbose (25 mg/kg body weight) and EAA (100 mg/kg body weight, 200 mg/kg body weight, and 400 mg/kg body weight) were given to the mice 30 min before the mice were induced with glucose. The acarbose/EAA treatment and glucose inducement were carried out by oral route using a rodent 18-gauge rounded tip. The blood was collected from their tail vein and measured for their blood glucose levels at 30-, 60-, 90-, and 120-min after glucose inducement.38
In this study fasting was carried out for 14 h to avoid the effects of food on the digestive tract, proving that changes in glucose levels were caused by EAA or acarbose. This was necessary to obtain baseline glucose levels as a comparison before administering glucose and treatment (EAA or acarbose). Mice still had access to drinking water (food was removed at 6:00 pm to start testing the next morning at 8:00 am).
Effects of EAA on Weight Gain (%), Insulin Tolerance, and Organ Index
The insulin tolerance test was performed after the glucose tolerance test. The mice were divided into 6 groups as follows: (1) the normal group (treated with sodium carboxy methyl cellulose 0.5% suspension); (2) the negative control or high fat-high fructose-induced group (induced with Lipofundin emulsion dose of 20 mL/kg body weight and fructose 2.52 g/kg body weight in sodium carboxy methyl cellulose 0.5% suspension); (3) the positive control or drug control group (induced with Lipofundin emulsion dose of 20 mL/kg body weight and fructose 2.52 g/kg body weight and treated with metformin 100 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension); (4) the test-1 group (induced with Lipofundin emulsion dose of 20 mL/kg body weight and fructose 2.52 g/kg body weight and treated with EAA 100 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension); (5) test-2 group (induced with Lipofundin emulsion dose of 20 mL/kg body weight and fructose 2.52 g/kg body weight and treated with EAA 200 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension); (6) test-3 group (induced with Lipofundin emulsion dose of 20 mL/kg body weight and fructose 2.52 g/kg body weight and treated with EAA 400 mg/kg body weight in sodium carboxy methyl cellulose 0.5% suspension). The insulin inducement and EAA treatment were carried out daily for 21 days. The body weight was observed on day 1 and day 21 to observe the weight gain (%). On day 1, day 7, day 14, and day 21, the mice were insulin-induced intraperitoneally at a dose of 0.0125 U/kg body weight, and post-insulin injection, the blood was centrifuged for 10 min to separate the serum and the glucose levels were measured.39,40
Subsequently, the mice were sacrificed using a combination of ketamine at a dose of 125 mg/kg body weight and xylazine 10 mg/kg body weight via intraperitoneal injection. The euthanasia procedure was carried out by trained personnel. Death was confirmed by determining cardiac and respiratory arrest.41–43 The liver and pancreas of the mice were separated, washed, and weighed, and the organ index was calculated.
Statistical Analysis
IBM SPSS for Windows was employed to analyze the data. Shapiro–Wilk test was used to analyze data distribution, for normal distribution (p < 0.05), the analysis was continued for significant differences between groups using one-way analysis of variance (ANOVA), followed by the post-hoc Tukey’s test. For abnormal distribution, the analysis was continued by the Kruskal–Wallis test. All data are presented as the mean ± SD; p < 0.05 indicates a significant result.
Results
The Nutritional Composition and Quercetin Levels in EAA
The extraction process of Brebes shallots using ethanol yielded a 28.1% EAA. Determination of nutritional composition revealed that EAA contained 21.82% water, 3.92% ash, 0.12% fat, 13.45% protein, and 60.69% carbohydrate.
The thin-layer chromatography bands of EAA are depicted in Figure 2 and the thin-layer chromatography-densitometry chromatograms in Figure 3. Quercetin was measured at 320 nm and eluted at Rf 0.59, and its levels were calculated using the linear regression equation of the standard addition curve (Figure 4) y = 93.12 x – 1196.4; R = 0.9715) resulting in 65 µg/mg (0.0065%).
 |
Figure 4 Quercetin standard addition curve of the thin-layer chromatography-densitometry of EAA. The linear regression equation of the standard addition curve is y = 93.12 x – 1196.4; R = 0.9715. |
Effects of EAA on Blood Glucose Levels by Oral Glucose Tolerance Test
The effects of EAA on glucose tolerance are tabulated in Table 1. At T0 (the time point when all animals were treated with sodium carboxymethyl cellulose, acarbose, or EAA, without glucose inducement), the blood glucose levels ranged between 72.75 ± 10.21 mg/dL (mice in the positive control or acarbose-treated group) to 116.00 ± 28.79 mg/dL (mice in the test-3 group). At T30 all mice underwent an increase in their blood glucose levels, except those in the normal group. Ranging from the lowest at 207.75 ± 64.46 mg/dL (mice in the positive control or acarbose-treated group) to the highest at 287.50 ± 109.60 mg/dL (mice in the negative control or untreated group). At the end of the glucose tolerance study (T120), the blood glucose levels of the mice in the positive control or acarbose-treated group were 98.75 ± 13.23 mg/dL (a decrease of 52.47% compared to T30), while those in the EAA groups were 109.75 ± 9.32 mg/dL (a decrease of 58.31% compared to T30), 114.25 ± 17.02 mg/dL (a decrease of 51.28% compared to T30), and 112.25 ± 11.27 mg/dL (a decrease of 46.93% compared to T30), in respect to the increasing doses of EAA.
 |
Table 1 The Effect of EAA on the Blood Glucose Levels in Oral Glucose Tolerance Tests of the Mice |
Effects of EAA on Weight Gain (%), Insulin Tolerance, and Organ Index
At the end of the study (D21), mice in all groups demonstrated an increase in body weight (Table 2), however, treatment with metformin 100 mg/kg body weight and all doses of EAA resulted in a lower % weight gain compared to the mice in the high fat-high fructose-induced group (Figure 5 and Table 2).
 |
Table 2 The Effect of EAA on the Body Weight and % Weight Gain of the Mice |
 |
Figure 5 Effects of EAA on the % weight gain of the HFHF-induced mice. The asterisk (*) shows a significant difference compared to the negative control or untreated group, with p < 0.05. |
The 21-day inducement with high fat-high fructose feed triggered the occurrence of IR, as proven by the insulin tolerance test (ITT) depicted in Figure 6 and Table 3. All mice in EAA and metformin groups improved IR as proven by higher ITT values (ITT = 2.54 ± 0.52 for EAA 100 mg/kg BW; ITT = 2.60 ± 0.48 for EAA 200 mg/kg BW; ITT = 2.98 ± 0.47 for EAA 400 mg/kg BW; and ITT = 3.43 ± 0.71 for metformin) compared with the high fat-high fructose-induced group without treatment (ITT = 0.15 ± 0.13). Interestingly, mice treated with an EAA dose of 400 mg/kg BW exhibited the highest ITT value of 2.98 ± 0.47.
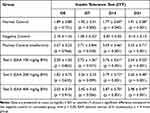 |
Table 3 The Effect of EAA on the Insulin Tolerance of the Mice |
 |
Figure 6 Effects of EAA on insulin tolerance of the HFHF-induced mice. The asterisk (*) shows a significant difference compared to the negative control or untreated group, with p < 0.05. |
The effects of EAA on the liver and pancreas indices are presented in Figure 7, which shows that the metformin treatment (p = 0.001) and all doses of EAA (p = 0.006 for the EAA dose of 100 mg/kg BW, p = 0.005 for the EAA dose of 200 mg/kg BW, and p = 0.001 for the EAA dose of 400 mg/kg BW) significantly lowered the liver index of the high fat-high fructose-induced mice compared to the negative control or untreated group (Figure 7a). However, only the highest dose of EAA (p = 0.024) and metformin (p = 0.05) significantly lowered the pancreas index of the mice (Figure 7b).
Further, we analyzed the correlation between parameters, and the results are tabulated in Table 4, indicating a positive correlation between ITT and % decrease in blood glucose, with a significant difference, and a negative correlation between ITT and body weight, liver index, and pancreas index.
 |
Table 4 Correlation Between ITT and % Decrease in Blood Glucose, Body Weight, and Organ Index |
Discussion
Allium ascalonicum L. (Amaryllidaceae) has shown a lot of potential to be utilized as a medicinal plant. The main findings of our study are that (1) the extraction process of 500 g Brebes shallots yielded 28.1% w/w of the ethanol extract of A. ascalonicum (EAA) with the nutritional composition including 3.92% ash, 0.12% fat, 13.45% protein, and 60.69% carbohydrate, and quercetin at 0.0065% w/w levels; (2) EAA lowered % weight gain, liver and pancreas index, and blood glucose levels, in high fat-high fructose-induced mice; (3) EAA significantly improved insulin tolerance (p < 0.05) in high fat-high fructose-induced mice. However, the limitations of this study are the use of only male mice and how EAA affects the proteins involved in the pathogenesis of IR.
In comparison to our nutritional analysis results, a previous study has reported that the extraction of shallots (A. ascalonicum L.) purchased from the local market in Chiang Mai, Thailand in 2021, yielded 9.11 ± 0.23% w/w of the extract. The extract contained polysaccharide at 0.09% w/w glucose, total protein at 0.101% w/w, and quercetin at 0.0029% w/w,44 lower than those contained in the Brebes shallots. Another study reported that the water extract of freshly harvested shallots, purchased from Shasha Market, Akure, Ondo State, Nigeria, contained 94.60 ± 0.20% water, 5.00 ± 1.00% ash, 5.17 ± 0.15% fat, 9.07 ± 0.2% protein, and 71.76 ± 2.48% carbohydrate. The total flavonoids calculated as rutin equivalence was 2.41 ± 0.04 mg/g or 0.241% w/w.45 Allium bulbs collected in Tarnogród, Poland, were reported to contain 11.75 ± 2.06% protein, 2.21 ± 0.12% ash, and 3.81 ± 0.30% fiber. It was described that different cultivated methods might affect the parameters of nutrition.46 Moreover, shallot accessions (Allium × cornutum, Allium × proliferum, and Allium cepa Aggregatum) from the ex-situ collection of the Institute of Agriculture and Tourism, Poreč, Croatia, collected in 2018 and 2019, were reported to contain abundant in phenolic compounds, especially quercetin and isorhamnetin glycosides.47 The ethanol extract of Korean onion (Allium cepa L.) peels, purchased from a local market in Daejeon, Korea, was reported to contain quercetin at 6.04 g/100 g (or 6.04% w/w) dried weight of peels. The extract exhibited a strong α-glucosidase inhibitory activity in diabetic-induced Sprague-Dawley rats.48
Flavonoids such as quercetin, kaempferol, and rutin could lower postprandial blood glucose response in HFFD-induced diabetic rats, and the effects are ascribed to the inhibition of carbohydrate digestive enzymes including α-amylase, α-glucosidase, and sucrase. Quercetin or kaempferol at a dose of 2.6 mmol/kg was reported to significantly lower fasting blood glucose, while quercetin or rutin at a dose of 2.6 mmol/kg markedly reduced the HOMA-IR index in HFFD rats, thus improving IR.49 Moreover, low-dose quercetin (50 µg/day) effectively overcomes HFD-induced IR by enhancing muscle mitochondrial function and PGC1α expression, which contributes to improved insulin sensitivity after 8 weeks of administration.50 Red onions purchased from a local grocer in West Lafayette, USA, containing low-dose of quercetin, were reported to increase insulin sensitivity, as evidenced by a decrease in blood glucose levels approaching the level in the group fed a low-fat diet (LF), both in the insulin tolerance test (ITT) and glucose tolerance test (GTT).30
In our study, the 21-day feed with lipofundin emulsion in combination with high fructose could increase body weight and induce the occurrence of insulin resistance in mice, as proven by the insulin tolerance test (ITT), tabulated in Table 3. Similarly, a previous study reported that a high-fat-high fructose diet affected the body weight of male Institute of Cancer Research (ICR) mice. At the end of the study, the high fat-high fructose (HFFD)-fed ICR mice exhibited significantly impaired glucose tolerance and insulin tolerance.51
Interestingly, studies in humans revealed that 4 weeks of feeding a high-fructose meal in healthy participants could significantly elevate the triglycerides, lactate, glucose, and leptin, with no changes in body weight, insulin sensitivity, and lipid.52 A former investigation reported the effects of meals containing fructose and delineated that this fruit sugar contributes a predisposing cause in the development of IR in correlation with the occurrence of high triglyceride levels in the blood.53
Our study confirmed that the ethanol extract of A. ascalonicum significantly improved IR in HFHFD-induced diabetic mice. Corresponding to our results, a previous study described that red onion extracts have shown antiobesity and IR-suppressing activity in high-fat diet-induced obesity C57BL/6J mice.30,31 The water extract of shallot bulbs, purchased at a local market in Mashhad, Iran, when administered for eight weeks, significantly improved intraperitoneal glucose tolerance and diminished the fasting IR index of male albino Wistar rats.54 The ethanol extract of onion (Allium cepa L.) peel, provided by the Center for Changnyeong Onion Bioindustry (Changwon, Korea), was reported to improve glucose response and IR-associated with T2DM, by alleviating metabolic dysregulation of free fatty acids, suppressing oxidative stress, up-regulating glucose uptake, and down-regulating hepatic inflammatory gene expression in male Sprague-Dawley rats.55 The ethanol extract of onion peel and onion bulb, purchased from a local market in Phulkara, India, was reported to lower blood glucose levels in alloxan-induced diabetic male Sprague-Dawley rats.56
Further, higher consumption of Allium vegetables, particularly garlic (Allium sativum) and onions (Allium cepa), was considered a nutritional strategy to improve glucose/insulin homeostasis. These activities were thought to be attributed to their rich content of flavonols and organosulfur compounds. The prospective cohort study was conducted on 1141 adult men and women in Tehran, Iran, from 2006 to 2011.57 Another study reported the effects of 150 mL of low-fat yogurt (1.5% fat) and 150 mL of low-fat yogurt (1.5% fat) plus shallot intake for 10 weeks on lipid profiles in 48 T2DM female participants. The study revealed that triglycerides and total cholesterol levels in participants who were given yogurt plus shallot were significantly reduced than those who consumed only yogurt (p = 0.003 and p = 0.04, respectively). This activity was thought to be contributed by the activity of the organosulfur compounds in the shallots that inhibit lipid synthesis through the oxidation of lipid-synthesizing enzymes.58 Organosulfur compounds such as S-methyl cysteine sulfoxide and allyl propyl disulfide have shown hypoglycemic activity.59,60 S-methyl cysteine sulfoxide works by lowering blood glucose levels by stimulating insulin secretion and increasing the activity of antioxidant enzymes such as superoxide dismutase which functions to reduce oxidative stress. Meanwhile, allyl propyl disulfide increases insulin sensitivity and glucose uptake in peripheral tissues.61 In addition, a systematic review by Moldovan et al thoroughly studied 116 articles and concluded that shallots, particularly A. ascalonicum and A. cepa var. aggregatum may have benefits as adjuvant therapy in cardiovascular diseases, diabetes, cancer prevention, and other non-communicable diseases associated with inflammatory and oxidative pathways.62
Conclusion
The present study evaluated the ethanol extract of shallot bulbs collected from a rural area in Brebes, Central Java, Indonesia, namely Allium ascalonicum L. of the family Amaryllidaceae. Our study revealed that the ethanol extract of A. ascalonicum L. (EAA) contained 3.92% ash, 0.12% fat, 13.45% protein, and 60.69% carbohydrate, and a small quantity of quercetin at a level of 0.0065%. We announce that this is the first report on the activity of Brebes shallots extract in decreasing blood glucose levels in oral glucose tolerance tests, lowering weight gain, decreasing liver and pancreas index, and significantly inhibiting IR in high fat-high fructose-induced mice. Quercetin despite its low levels in the extract may contribute to the activity, however, other metabolites in the shallot bulbs, such as kaempferol and organosulfur compounds, potentiate this activity. These findings provide evidence that EAA can be further explored for its mechanism to how it suppresses IR conditions. Future research should be directed to explore the mechanism by which the extract modulates certain signaling pathways in the pathogenesis of IR, such as diacylglycerol (DAG)/protein kinase C (PKC) pathway, peroxisome proliferator-activated receptor γ (PPARγ)/sterol regulatory element-binding protein 1c (SREBP-1c), its effects on GLUT4R expression, the long-term effects of EAA in animal models, the effects of EAA towards the pro-inflammatory and anti-inflammatory cytokines, the potential herbal-drug interactions with oral antidiabetic drugs, and finally the effect of EAA in humans. It should be noted that the goal of these studies is to better understand the therapeutic potential of EAA in managing IR and improving the efficacy of diabetes treatment.
Acknowledgments
The authors thank the Rector of Universitas Padjadjaran via the Directorate of Research and Community Engagement of Universitas Padjadjaran for funding the research via the Universitas Padjadjaran Academic-Leadership Grant year 2024 of Prof. Sri Adi Sumiwi and facilitating the APC. This study is the research thesis of the first author in the Master Program in Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran.
Disclosure
The authors declared no potential conflicts of interest to the research, authorship, or publication of this article.
References
1. Wilcox G. Insulin and insulin resistance. Clin Biochem Rev. 2005;26(2):19–39.
2. Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes. 2014;7:587–591. doi:10.2147/dmso.s67400
3. Martins FO, Conde SV. Impact of diet composition on insulin resistance. Nutrients. 2022;14(18):3716. doi:10.3390/nu14183716
4. Magliano DJ, Boyko EJ. IDF Diabetes Atlas 10th edition scientific committee. In: IDF DIABETES ATLAS.
5. WHO. Health Topics: diabetes. 2023. Available from: https://www.who.int/health-topics/diabetes.
6. Mukhtar Y, Galalain A, Yunusa U. A modern overview on diabetes mellitus: a chronic endocrine disorder. Eur J Biol. 2020;5(2):1–14. doi:10.47672/ejb.409
7. Khin PP, Lee JH, Jun H-S. Pancreatic beta-cell dysfunction in type 2 diabetes. Eur J Inflamm. 2023;21. doi:10.1177/1721727X231154152.
8. Li DD, Yang Y, Gao ZY, et al. Sedentary lifestyle and body composition in type 2 diabetes. Diabetol Metab Syndr. 2022;14(1):8. doi:10.1186/s13098-021-00778-6
9. White U, Beyl RA, Ravussin E. A higher proportion of small adipocytes is associated with increased visceral and ectopic lipid accumulation during weight gain in response to overfeeding in men. Int J Obes. 2022;46(8):1560–1563. doi:10.1038/s41366-022-01150-y
10. Elkanawati RY, Sumiwi SA, Levita J. Impact of lipids on insulin resistance: insights from human and animal studies. Drug Des Devel Ther. 2024;18:3337–3360. doi:10.2147/dddt.s468147
11. Ahmed B, Sultana R, Greene MW. Adipose Tissue and Insulin Resistance in Obese. Biomed Pharmacother. 2021;137:111315. doi:10.1016/j.biopha.2021.111315
12. Gonzalez-Lopez C, Wojeck BS. Role of metformin in the management of type 2 diabetes: recent advances. Pol Arch Intern Med. 2023;133(6):16511. doi:10.20452/pamw.16511
13. Ganesan K, Rana MBM, Sultan S Oral Hypoglycemic Medications. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482386/.
14. Susilawati E, Levita J, Susilawati Y, Sumiwi SA. Review of the case reports on metformin, sulfonylurea, and thiazolidinedione therapies in type 2 diabetes mellitus patients. Med Sci. 2023;11(3):50. doi:10.3390/medsci11030050
15. Qaseem A, Barry MJ, Humphrey LL, et al. Oral Pharmacologic Treatment of Type 2 Diabetes Mellitus: a Clinical Practice Guideline Update From the American College of Physicians. Ann Intern Med. 2017;166(4):279–290. doi:10.7326/m16-1860
16. Lee J, Noh S, Lim S, Kim B. Plant extracts for Type 2 Diabetes: from traditional medicine to modern drug discovery. Antioxidants. 2021;10(1):81. doi:10.3390/antiox10010081
17. Chatterjee S, Davies MJ, Tarigopula G. Pharmacological control of blood sugar. Anaesth Intensive Care Med. 2017;18(10):532–534. doi:10.1016/j.mpaic.2017.06.017
18. Maithili Karpaga Selvi N, Sridhar MG, Swaminathan RP, Sripradha R. Efficacy of turmeric as adjuvant therapy in type 2 diabetic patients. Indian J Clin Biochem. 2015;30(2):180–186. doi:10.1007/s12291-014-0436-2
19. Xu Y, Zheng S, Jiang S, Chen J, Zhu X, Zhang Y. The effect of Chinese herbal formulas combined with metformin on modulating the gut microbiota in the amelioration of type 2 diabetes mellitus: a systematic review and meta-analysis. Front Endocrinol. 2022;13:927959. doi:10.3389/fendo.2022.927959
20. Liu C, Guo X. Adjuvant Chinese medicine for the treatment of type 2 diabetes mellitus combined with mild cognitive impairment: a systematic review and meta-analysis of a randomised controlled trial. Pharmaceuticals. 2022;15(11):1424. doi:10.3390/ph15111424
21. Zhang X, Zhang L, Zhang B, et al. Herbal tea, a novel adjuvant therapy for treating type 2 diabetes mellitus: a review. Front Pharmacol. 2022;13:982387. doi:10.3389/fphar.2022.982387
22. Aziz TA, Hussain SA, Mahwi TO, Ahmed ZA, Rahman HS, Rasedee A. The efficacy and safety of Ginkgo biloba extract as an adjuvant in type 2 diabetes mellitus patients ineffectively managed with metformin: a double-blind, randomized, placebo-controlled trial. Drug Des Devel Ther. 2018;12:735–742. doi:10.2147/dddt.s157113
23. Kumar SN, Mani UV, Mani I. An open-label study on the supplementation of Gymnema sylvestre in Type 2 Diabetics. J Diet Suppl. 2010;7(3):273–282. doi:10.3109/19390211.2010.505901
24. Al-Ishaq RK, Abotaleb M, Kubatka P, Kajo K, Büsselberg D. Flavonoids and their anti-diabetic effects: cellular mechanisms and effects to improve blood sugar levels. Biomolecules. 2019;9(9):430. doi:10.3390/biom9090430
25. Vinayagam R, Xu B. Antidiabetic properties of dietary flavonoids: a cellular mechanism review. Nutr Metab. 2015;12:60. doi:10.1186/s12986-015-0057-7
26. Nurcahyo H, Sumiwi SA, Halimah E, Wilar G. Secondary metabolites determination from Brebes shallot’s ethanol extract and its ethyl acetate fraction “Allium ascalonicum L. J Adv Pharm Educ Res. 2022;12(1):70–73. doi:10.51847/NFNMFJB9AC
27. Kothari D, Lee WD, Kim SK. Allium flavonols: health benefits, molecular targets, and bioavailability. Antioxidants. 2020;9(9):888. doi:10.3390/antiox9090888
28. Nurcahyo H, Sumiwi SA, Halimah E, Wilar G. Total flavonoid of dry extract and fraction of selected shallot (Allium ascalonicum L.) using ultraviolet-visible spectrophotometry and HPLC. Food Res. 2023;7(2):137–142. doi:10.26656/fr.2017.7(2).765
29. Kongstad KT, Özdemir C, Barzak A, Wubshet SG, Staerk D. Combined use of high-resolution α-glucosidase inhibition profiling and high-performance liquid chromatography-high-resolution mass spectrometry-solid-phase extraction-nuclear magnetic resonance spectroscopy for investigation of antidiabetic principles in crude plant extracts. J Agric Food Chem. 2015;63(8):2257–2263. doi:10.1021/jf506297k
30. Henagan TM, Cefalu WT, Ribnicky DM, et al. In vivo effects of dietary quercetin and quercetin-rich red onion extract on skeletal muscle mitochondria, metabolism, and insulin sensitivity. Genes Nutr. 2015;10(1):451. doi:10.1007/s12263-014-0451-1
31. Forney LA, Lenard NR, Stewart LK, Henagan TM. Dietary quercetin attenuates adipose tissue expansion and inflammation and alters adipocyte morphology in a tissue-specific manner. Int J Mol Sci. 2018;19(3):895. doi:10.3390/ijms19030895
32. Tang X, Olatunji OJ, Zhou Y, Hou X. Allium tuberosum: antidiabetic and hepatoprotective activities. Food Res Int. 2017;102:681–689. doi:10.1016/j.foodres.2017.08.034
33. Khassanov F, Yusupov Z. A Taxonomical Revision of Genus Allium L. (Amaryllidaceae) in the Flora of Middle Asia. Biodiversity Conserv Sustain. 2022;403–433. doi:10.1007/978-3-030-73943-0_22
34. Moldovan C, Nicolescu A, Frumuzachi O, et al. Ultrasound-assisted sustainable extraction of bioactive phytochemicals in shallot (Allium ascalonicum L.) peel: a DoE and metabolomics combined approach. Sustain Chem Pharm. 2024;41:101729. doi:10.1016/j.scp.2024.101729
35. AOAC. Official Methods of Analysis. 2023. Available from: https://www.aoac.org/official-methods-of-analysis/.
36. Doshi GM, Une HD. Quantification of quercetin and rutin from Benincasa hispida seeds and Carissa congesta roots by high-performance thin layer chromatography and high-performance liquid chromatography. Pharmacogn Res. 2016;8(1):37–42. doi:10.4103/0974-8490.171098
37. National Research Council of the National Academies Guide for the Care and Use of Laboratory Animals. Washington DC, USA: The National Academies Press; 2011. Available from: https://grants.nih.gov/grants/olaw/guide-for-the-care-and-use-of-laboratory-animals.pdf.
38. Susilawati E, Levita J, Susilawati Y, Sumiwi SA. Erythrina subumbrans (Hassk) Merr. (Fabaceae) inhibits insulin resistance in the adipose tissue of high fructose-induced Wistar rats. Drug Des Devel Ther. 2024;18:3825–3839. doi:10.2147/DDDT.S472660
39. Wei J, Hao Q, Chen C, et al. Epigenetic repression of miR-17 contributed to di(2-ethylhexyl) phthalate-triggered insulin resistance by targeting Keap1-Nrf2/miR-200a axis in skeletal muscle. Theranostics. 2020;10(20):9230–9248. doi:10.7150/thno.45253
40. Freeman AM, Acevedo LA, Pennings N. Insulin Resistance. In: StatPearls. StatPearls Publishing; 2023. Available from. http://www.ncbi.nlm.nih.gov/books/NBK507839/.
41. Schoell AR, Heyde BR, Weir DE, Chiang PC, Hu Y, Tung DK. Euthanasia method for mice in rapid time-course pulmonary pharmacokinetic studies. J Am Assoc Lab Anim Sci. 2009;48(5):506–511.
42. Giroux MC, Hélie P, Burns P, Vachon P. Anesthetic and pathological changes following high doses of ketamine and xylazine in Sprague Dawley rats. Exp Anim. 2015;64(3):253–260. doi:10.1538/expanim.14-0088
43. Hohlbaum K, Bert B, Dietze S, Palme R, Fink H, Thöne-Reineke C. Impact of repeated anesthesia with ketamine and xylazine on the well-being of C57BL/6JRj mice. PLoS One. 2018;13(9):e0203559. doi:10.1371/journal.pone.0203559
44. Ruksiriwanich W, Khantham C, Muangsanguan A, et al. Phytochemical constitution, anti-inflammation, anti-androgen, and hair growth-promoting potential of shallot (Allium ascalonicum L.) extract. Plants. 2022;11(11):1499. doi:10.3390/plants11111499
45. Adeyemo AE, Omoba OS, Olagunju AI, Josiah SS. Assessment of nutritional values, phytochemical content, and antioxidant properties of Shallot (Allium ascalonicum L.) leaf and bulb. Measurement: Food. 2023;10:100091. doi:10.1016/j.meafoo.2023.100091
46. Czech A, Szmigielski M, Sembratowicz I. Nutritional value and antioxidant capacity of organic and conventional vegetables of the genus Allium. Sci Rep. 2022;12(1):18713. doi:10.1038/s41598-022-23497-y
47. Major N, Perković J, Palčić I, et al. The Phytochemical and Nutritional Composition of Shallot Species (Allium × cornutum, Allium × proliferum and A. cepa Aggregatum) Is Genetically and Environmentally Dependent. Antioxidants. 2022;11(8):1547. doi:10.3390/antiox11081547
48. Kim SH, Jo SH, Kwon YI, Hwang JK. Effects of onion (Allium cepa L.) extract administration on intestinal α-glucosidases activities and spikes in postprandial blood glucose levels in SD rats model. Int J Mol Sci. 2011;12(6):3757–3769. doi:10.3390/ijms12063757
49. Li BW, Zhao L, Wang Y, et al. Effects of quercetin, kaempferol, and rutin on high-fructose and high-fat diet-induced metabolic syndrome in rats. Food Sci. 2019;40:223–233.
50. Henagan TM, Lenard NR, Gettys TW, Stewart LK. Dietary quercetin supplementation in mice increases skeletal muscle PGC1α expression, improves mitochondrial function and attenuates insulin resistance in a time-specific manner. PLoS One. 2014;9(2):e89365. doi:10.1371/journal.pone.0089365
51. Zhuhua Z, Zhiquan W, Zhen Y, et al. A novel mice model of metabolic syndrome: the high-fat-high-fructose diet-fed ICR mice. Exp Anim. 2015;64(4):435–442. doi:10.1538/expanim.14-0086
52. Lê KA, Faeh D, Stettler R, et al. A 4-wk high-fructose diet alters lipid metabolism without affecting insulin sensitivity or ectopic lipids in healthy humans. Am J Clin Nutr. 2006;84(6):1374–1379. doi:10.1093/ajcn/84.6.1374
53. Dornas WC, de Lima WG, Pedrosa ML, Silva ME. Health implications of high-fructose intake and current research. Adv Nutr. 2015;6(6):729–737. doi:10.3945/an.114.008144
54. Jalal R, Bagheri SM, Moghimi A, Rasuli MB. Hypoglycemic effect of aqueous shallot and garlic extracts in rats with fructose-induced insulin resistance. J Clin Biochem Nutr. 2007;41(3):218–223. doi:10.3164/jcbn.2007031
55. Jung JY, Lim Y, Moon MS, et al. Onion peel extracts ameliorate hyperglycemia and insulin resistance in high fat diet/streptozotocin-induced diabetic rats. Nutr Metab. 2011;8(1):18. doi:10.1186/1743-7075-8-18
56. Masood S, Rehman AU, Bashir S, et al. Investigation of the anti-hyperglycemic and antioxidant effects of wheat bread supplemented with onion peel extract and onion powder in diabetic rats. J Diabetes Metab Disord. 2021;20(1):485–495. doi:10.1007/s40200-021-00770-x
57. Mirmiran P, Bahadoran Z, Tohidi M, Azizi F. Higher consumption of Allium vegetables may modulate insulin homeostasis: a longitudinal follow-up study. J Herbs Med. 2019;17-18:100260. doi:10.1016/j.hermed.2019.100260
58. Mehrabani S, Abbasi B, Darvishi L, et al. Effects of yogurt and yogurt plus shallot consumption on lipid profiles in type 2 diabetic women. Int J Prev Med. 2017;8(1):54. doi:10.4103/2008-7802.211605
59. Chakraborty AJ, Uddin TM, Matin Zidan BMR, et al. Allium cepa: a treasure of bioactive phytochemicals with prospective health benefits. Evid Based Complement Alternat Med. 2022;18:4586318. doi:10.1155/2022/4586318
60. Kianian F, Marefati N, Boskabady M, Ghasemi SZ, Boskabady MH. Pharmacological properties of Allium cepa, preclinical and clinical evidences; a review. Iran J Pharm Res. 2021;20(2):107–134. doi:10.22037/ijpr.2020.112781.13946
61. Sabiu S, Madende M, Ajao AA-N, Aladodo RA, Nurain IO, Ahmad JB. The genus Allium (Amaryllidaceae: alloideae): features, phytoconstituents, and mechanisms of antidiabetic potential of Allium cepa and allium sativum. Bioactive Food Dietary Interventions Diabet. 2019;137–154. doi:10.1016/b978-0-12-813822-9.00009-6
62. Moldovan C, Frumuzachi O, Babotă M, et al. Therapeutic uses and pharmacological properties of shallot (Allium ascalonicum): a systematic review. Front Nutr. 2022;9:903686. doi:10.3389/fnut.2022.903686
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Decreased Serum Osteocalcin is an Independent Risk Factor for Metabolic Dysfunction-Associated Fatty Liver Disease in Type 2 Diabetes
Wang YJ, Jin CH, Ke JF, Wang JW, Ma YL, Lu JX, Li MF, Li LX
Diabetes, Metabolic Syndrome and Obesity 2022, 15:3717-3728
Published Date: 29 November 2022
Association Between Plasma Asprosin Levels and Gestational Diabetes Mellitus
Boz İB, Aytürk Salt S, Salt Ö, Sayın NC, Dibirdik İ
Diabetes, Metabolic Syndrome and Obesity 2023, 16:2515-2521
Published Date: 23 August 2023
Phytochemical Analysis, Computational Study, and in vitro Assay of Etlingera elatior Inflorescence Extract Towards Inducible Nitric Oxide Synthase
Prayoga DK, Pitaloka DAE, Aulifa DL, Budiman A, Levita J, Jiranusornkul S, Nguyen BP
Journal of Experimental Pharmacology 2025, 17:123-141
Published Date: 8 March 2025




