Back to Journals » Journal of Pain Research » Volume 18
The Evaluation of Reference Values of Plasma and Effect-Site Concentrations of Propofol and Remifentanil During Extubation in Patients Who Had Hysteroscopy Procedures
Authors Wei Y, Wang J, Xu Z, Ma R
Received 8 July 2024
Accepted for publication 14 February 2025
Published 12 March 2025 Volume 2025:18 Pages 1211—1219
DOI https://doi.org/10.2147/JPR.S486147
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Karina Gritsenko
Yu Wei,1– 3,* Jianwei Wang,1– 3,* Zifeng Xu,1– 3 Rui Ma1– 3
1Department of Anesthesiology, the International Peace Maternity and Child Health Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, People’s Republic of China; 2Shanghai Key Laboratory of Embryo Original Diseases, Shanghai, Peoples Republic of China; 3Shanghai Municipal Key Clinical Specialty, Shanghai, Peoples Republic of China
*These authors contributed equally to this work
Correspondence: Rui Ma; Zifeng Xu, Department of Anesthesiology, the International Peace Maternity and Child Health Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai Key Laboratory of Embryo Original Diseases, Shanghai Municipal Key Clinical Specialty, Huashan Road 1961, Shanghai, 200030, People’s Republic of China, Tel +86-021-64070434, Email [email protected]; [email protected]
Aim: This study aimed to assess the correlation of plasma concentration (Cp) and effect-site concentration (Ce) of propofol and remifentanil with level of consciousness and evaluate their reference values during extubation in patients scheduled day-case operative hysteroscopy under propofol-remifentanil anesthesia.
Methods: Propofol (Marsh model) and remifentanil (Minto model) were simultaneously administered using a target-controlled infusion (TCI) pump for the induction and maintenance of anesthesia. The Cp and Ce of propofol (PCp and PCe) and remifentanil (RCp and RCe) before anesthesia induction, at the end of surgery, and at the time of extubation were respectively recorded. Predictive performance was assessed using the jackknife method.
Results: At the time of extubation, PCp was 1.17 ± 0.168 (95% CI: 1.14– 1.20 μg/mL), PCe was 1.7 ± 0.212 (95% CI: 1.65– 1.74 μg/mL), RCp was 0.769 ± 0.12 (95% CI: 0.75– 0.79μg/mL), and RCe was 0.972 ± 0.179 (95% CI: 0.94 − 1.01 μg/mL). The Pk values of PCp, PCe, RCp and RCe were 0.999, 0.993, 1.00 and 0.995, separately. Postoperative decreases in PCp (r = 0.089, p < 0.001), PCe (r = 0.087, p= 0.001), RCp (r = 0.072, p < 0.000) and RCe (r = 0.077, p < 0.001) were significantly correlated with the recovery time.
Conclusion: PCp, PCe, RCp and RCe, together with OAA/S Scale and the recovery of spontaneous respiration might be potential reference indicators for extubation in day-surgery hysteroscopy following general anesthesia using TCI.
Keywords: day surgery, effect-site concentration, plasma concentration, prediction probability, target-controlled infusion
Introduction
Operative hysteroscopy is a widely-accepted short and less traumatic practice that cause few complications and can be used to treat various intrauterine diseases quickly and effectively.1 Procedural sedation and analgesia are used to alleviate pain, stress, anxiety, and discomfort during invasive diagnostic and therapeutic procedures.2 Frequent monitoring of the level of consciousness during procedural sedation and analgesia can improve patient safety and sedation efficacy, and decrease the risk of adverse events, such as hypoxemia, inadequate ventilation or circulation.3,4 Processed electroencephalogram (EEG) - based anesthetic depth monitoring devices has been extensively applied to monitor the level of consciousness in anesthesia practice as an adjunct to clinical observation. One such frequently used device is the bispectral index (BIS),5,6 which provides numerical values indicative of different levels of depth of anesthesia. Hysteroscopy surgery requires successful induction of anesthesia, maintenance of adequate analgesia and sedation during the operation, rapid postoperative wake up and safe extubation to shorten the length of hospital stay and minimize relevant adverse events. Though EEG-based depth of anesthesia monitor is feasible for hysteroscopy surgeries, it might increase surgery time and cost. Therefore, it is necessary to seek a more convenient way to judge the timing for removing the laryngeal mask.
Accumulating studies using pharmacokinetic-pharmacodynamic models demonstrate that BIS values are inversely related to the plasma concentration (Cp) and effect-site concentration of propofol.7–9 Propofol is usually co-administered with remifentanil, which exhibits a synergistic anesthetic effect.10 Therefore, we hypothesize that Cp and the effect-site concentration (Ce) of propofol and remifentanil may be correlated with anaesthetic depth. To test this hypothesis, in this study, we investigated the association of Cp and Ce of propofol and remifentanil with anesthetic depth and extubation time in patients undergoing day-surgery operative hysteroscopy under general anesthesia using target-controlled infusion (TCI) of propofol and remifentanil.
Methods
Patients
This study has been registered on Chinese Clinical Trial Registry with accession number of chiCTR2000034837. The study protocol was approved by the Ethics Committee of International Peace Maternal and Child Health Hospital, School of Medicine, Shanghai Jiao Tong University (approval number: GKLW2019-49). The study protocol was in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
The inclusion criteria were as follows: American Society of Anesthesiologists (ASA) physical status I or II;11 age 20–60 years; scheduled day-surgery operative hysteroscopy, limited to those requiring uterine cavity examination for the diagnosis of unexplained uterine bleeding, causes of habitual miscarriage and assessment of the uterine condition in infertile patients, as well as those for simple intervention measures, such as removal of endometrial polyps, removal of intrauterine devices, decomposition of intrauterine adhesions; no history of mental or neurological disorders; no severe hypertension, no cardiac or endocrine diseases; and normal liver and kidney function. The exclusion criteria were as follows: known allergy to the drugs used in this study; body mass index < 17 kg/m2 or > 30 kg/m2; patients undergoing uterine cavity electrocision and uterine fibroids electrocision surgeries; chronic tertiary hypertension; severe arrhythmia; chronic bronchitis, asthma or other respiratory diseases; increased intraocular, intrathoracic, or intracranial pressure, and hearing impairment; operation time > 30 min; and administration of inhalational anesthetic agents and muscle relaxants because of surgery. From July 23, 2020 to September 30, 2020, 149 patients scheduled for day-surgery operative hysteroscopy were enrolled. After excluding unqualified patients, a total of 106 patients were initially included. During surgery, another 6 patients were excluded because of surgery changed (n =3), operation time > 30 min (n = 2) and administration of muscle relaxants (n =1). Finally, 100 patients in the day surgery ward of our hospital met the inclusion and exclusion criteria and were enrolled in the study (Figure 1).
 |
Figure 1 The flowchart of patients’ enrollment. |
Anesthetic Procedure
All patients received preoperative examinations the day before surgery. Routine visits to the anesthesia clinic were conducted to rule out contraindications to day surgery anesthesia. The patients fasted for solids and liquids for 8 h preoperatively.
All patients underwent general anesthesia monitoring including mean blood pressure (MBP), respiration rate (RR), heart rate (HR), electrocardiogram, BIS and oxygen saturation (SpO2). Propofol (Guangdong Jiabo Pharmaceutical Co., Ltd, Qingyuan, Guangdong province, China; registration number, H20133248) and remifentanil (Yichang Humanwell, Pharmaceutical Co., LTD, Yichang, Hubei province, China; registration number, H20054172) were simultaneously administered using a TCI pump (MED CAPTAIN medical technologies, HP-30 pump, Shenzhen, China). The Observer’s Assessment of Alertness/Sedation (OAA/S) Scale12,13 and BIS were used to evaluate the depth of anesthesia.
The commenced Ce of propofol (PCe) was 6 μg/mL (Marsh model), while that of remifentanil (RCe) was commenced at 5 ng/mL (Minto model). Subsequently, the level of sedation was evaluated and recorded using the OAA/S scale and BIS every 20s until loss of consciousness (OAA/S scale ≤1, BIS reached to 40–60 and disappearance of the eyelash reflex). Laryngeal mask airway (LMA) was inserted in all patients. The parameters of mechanical ventilation were set as follows: tidal volume (VT), 8 mL-10mL/kg; RR, 12 beats/min; inhalation/expiration ratio, 1:2; end-tidal carbon dioxide (PetCO2), 30–40 mmHg.
The operations were performed or directly supervised by a highly skilled hysteroscopic specialist after placing the laryngeal mask airway (LMA), Hysteroscopic morcellation was performed using the TruClear™ 5C system (Medtronic, Minneapolis, MN, USA), with a 0° optic and a 5.7 mm sheath, and a 2.9 mm rotary morcellator. No additional local anesthetics were given before cervical dilation. The operation time was calculated from the entry of the hysteroscopic morcellation into the uterine cavity. When all uterine cavity operations were completed and the hysteroscopic morcellation no longer entered the uterine cavity at the end, the operation was considered completed, and the total operation time was recorded. The anesthesia infusion pump stopped infusing drugs at the end of the uterine cavity operation.
Intraoperatively, PCe and RCe were adjusted according to surgical irritation and hemodynamic changes. PCe and RCe were set at 2.5 μg/mL and 2.5 ng/mL, respectively, to maintain anesthesia (BIS between 40–60). The shallowness of the anesthesia depth was evaluated by body movements during surgery. In case of active body movements, PCe was increased by 0.5ug/L to maintain an adequate depth of anesthesia.
Postoperatively, once the infusions of propofol and remifentanil were discontinued, we primarily employed verbal stimuli to assess consciousness. Anesthesiologists spoke to patients in a normal tone, giving commands or asking questions to observe their responses. Additionally, light tactile stimulation was applied as a supplementary measure to assess responsiveness. Awakening began one a BIS value greater than 80 was recorded, along with an OAA/S scale score of 5. The LMA was removed when the patient’s spontaneous breathing rate exceeded 12 breaths/min, VT was greater than 6 mL/kg, and SpO2 was above 95%. The interval from the cessation of drug infusion to the removal of the LMA was noted as the recovery time, and the BIS value at the time of initiating awakening was meticulously recorded to ensure a detailed and accurate evaluation of recovery dynamics.
MBP, HR, PCp, PCe, RCp and RCe of the patients were recorded before anesthesia induction (T0), at the end of surgery (T1), and at the time of extubation (T2). The total propofol or remifentanil dose (TP or TR) during surgery was also recorded. The duration from dis-continuation of propofol and remifentanil to remove LMA (both OAA/S scale and respiratory parameters were achieved) was defined as recovery time. Changes in PCp, PCe, RCp, and RCe between T1 and T2 were calculated and analyzed.
Management for Adverse Events
In cases of HR < 50 beats/min, a bonus of atropine (0.5mg) was administered intravenously.14 When blood pressure decreased by > 30% or was < 80/50mmHg, a bonus of 5–10 mg ephedrine was administered intravenously15 and TCIs of propofol and remifentanil were sped up. In the case of PetCO2 > 50mmHg or < 20mmHg, VT was adjusted, and the surgery was suspended until PetCO2 normalized.
Statistical Analysis
Continuous data were expressed as mean ± SD, and statistical analysis was performed using SPSS 22.0. Nonparametric Spearman correlation and linear regression analyses were used to analyze the correlations of total propofol dose, total remifentanil dose, operation time, and postoperative changes of PCp, PCe, RCp and RCe with recovery time. To assess the predictive value of these parameters for the level of consciousness during the awakening period, prediction probability (Pk) values were calculated by the jackknife method proposed by MILLER et al in R software (version 4.0.0).16 The Pk values ranged from 0 to 1. When Pk =1, this suggests that the parameter could 100% correctly predict the depth of anesthesia. When Pk < 0.5, this suggests the predictive accuracy was poor. Sample size was calculated based on jackknife method using the lowest acceptable Pk value of 0.7 as outcome.17 Standard error was set as 0.4, significance level was set as 0.05, test power was set as 0.9, and at least 18 patients were required.
Results
Day-surgery hysteroscopy was successfully performed in a total of 100 patients. Intra-operatively, the SpO2 was maintained at 98%-100%. The enrolled patients were aged between 23 years old and 59 years old, with an average age of (41.13 ± 8.99) years old. The average operation time was (18.12 ± 5.72) min and the recovery time was (5.43 ± 3.27) min (Table 1).
 |
Table 1 Characteristics of Patients |
MBP, HR, PCp, PCe, RCp and RCe of patients at T0, T1 and T2 time points are shown in Table 2. At the extubation time (T2), PCp was 1.17 ± 0.168 [95% confidence interval (CI): 1.14–1.20 μg/mL], PCe was 1.7 ± 0.212 (95% CI: 1.65–1.74 μg/mL), RCp was 0.769 ± 0.12 (95% CI: 0.75–0.79 μg/mL), and RCe was 0.972 ± 0.179 (95% CI: 0.94 −1.01 μg/mL). The Pk values of PCp, PCe, RCp and RCe were 0.999, 0.993, 1, and 1, respectively, which were higher than the Pk values of MBP and HR (0.654 and 0.714, respectively).
 |
Table 2 MBP, HR, Cp and Ce of Propofol and Remifentanil at Different Time Points |
Correlations of total propofol dose, total remifentanil dose, operation time, and postoperative decline in PCp, PCe, RCp, and RCe with recovery time were analyzed. As depicted in Table 3, postoperative declines in PCp (r = 0.089, p < 0.001), PCe (r = 0.087, p = 0.001), RCp (r = 0.072, p < 0.001) and RCe (r = 0.077, p < 0.001) were significantly correlated with recovery time. However, TP, TR, and operation time were not significantly correlated with recovery time (p > 0.05).
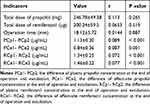 |
Table 3 Correlation Analysis With Recovery Time |
Two adverse events were reported during the procedure: one case of choking and one case of sinus bradycardia (Table 4).
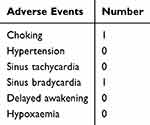 |
Table 4 Summary of Adverse Events |
Discussion
Given the recent increase in shorter procedures requiring general anesthesia, and the high demand of reducing medical costs in clinical settings, it is valuable to explore more useful reference indicators to facilitate good recovery. In this study, we investigated the correlation of PCp, PCe, RCp and RCe with recovery time and evaluated their reference values during extubation in patients undergoing day-surgery operative hysteroscopy following general anesthesia using TCI. Our findings indicated that under the Marsh model of propofol (initial concentration of 6ng/mL) and Minto model of remifentanil (initial concentration of 5ng/mL), the PCp, PCe, RCp and RCe were 1.17 ± 0.168 (95% CI: 1.14–1.20 μg/mL), 1.7 ± 0.212 (95% CI: 1.65–1.74 μg/mL), 0.769 ± 0.12 (95% CI: 0.75–0.79μg/mL), and 0.972 ± 0.179 (95% CI: 0.94 −1.01 μg/mL) at the extubation time. Postoperative declines in PCp (r = 0.089, p < 0.001), PCe (r = 0.087, p = 0.001), RCp (r = 0.072, p < 0.001) and RCe (r = 0.077, p < 0.001) were significantly correlated with recovery time. The Pk values of PCp, PCe, RCp and RCe were 0.999, 0.993, 1, and 1, respectively. PCp, PCe, RCp and RCe might be potential reference indicators for predicting the time of extubation, together with OAA/S Scale and the recovery of spontaneous respiration.
Discontinuing TCI of propofol and remifentanil in time according to Cp and Ce of propofol and remifentanil would shorten the recovery time and accelerate the turnover rate of surgery, thus reducing the requirements for anesthesia equipment and cutting anesthetic costs. Various processed EEG-based depth of anesthesia monitors have been extensively used to measure the depth of anesthesia intraoperatively and guide the extubation time postoperatively, such as the BIS,18 narcotrend index, patients state index,19 approximate entropy and sample entropy.20 Although these monitoring indexes are suitable for intraoperative monitoring, they are limited in monitoring the level of consciousness during the postoperative recovery period and may cause errors without co-administration of muscle relaxants.21 Besides, the EEG-based anesthetic care will increase about 20% cost of anesthesia and prolong the surgery time of 10%-20%. Therefore, it is valuable to explore more useful reference indicators to facilitate good recovery to save medical resources and maintain safety at the same time. Our result proposed using PCp, PCe, RCp and RCe, together with OAA/S Scale and the recovery of spontaneous respiration, as reference indicators for extubation in patients undergoing hysteroscopic surgery under general anesthesia using TCIs of propofol and remifentanil. To the best of our knowledge, this is the first study concerning the value of Cp and Ce of propofol and remifentanil in measuring the depth of anesthesia and guiding the time of extubation. However, far more research should be conducted before using these indicators in clinic for safety issues.
Propofol is a commonly used short-acting sedative agent characterized by rapid onset and offset for the induction and maintenance of anesthesia.22,23 Co-administration of remifentanil and propofol can achieve effective and safe anesthesia and has been widely used for general anesthesia.24–26 TCI has become a mature technology for the administration of propofol and opioids for general anesthesia in clinical practice.27,28 Our study used intravenous TCI of propofol and remifentanil to induce and maintain anesthesia in patients undergoing hysteroscopic surgery without administration of muscle relaxants. The predictive value of Cp and Ce of propofol and remifentanil for anesthetic depth was evaluated by calculating Pk values.17 In the present study, Pk values of PCp, PCe, RCp, and RCe were equal to or close to 1, suggesting a good predictive capability of PCp, PCe, RCp, and RCe for patients’ depth of anesthesia. This result indicates that TCI of propofol and remifentanil without administration of muscle relaxants might be sufficient for induction and maintenance of anesthesia in patients undergoing daytime surgery, such as operative hysteroscopy. Moreover, our study found that postoperative decreases in PCp, PCe, RCp and RCe were significantly related to recovery time. Our study suggests that, together with OAA/S Scale and the recovery of spontaneous respiration, it might be a safe way to remove LMA from patients or wake up patients when PCp is within the range of 1.14 −1.20 μg/mL, PCe is within the range of 1.65–1.74 μg/mL, RCp is within the range of 0.75–0.79 μg/mL, and RCe is within the range of 0.94–1.01 μg/mL. To the best of our knowledge, we are the first to propose the possibility of PCp, PCe, RCp and RCe to be used as potential reference indicators. Nevertheless, our study has some limitations. First, infusion of propofol and remifentanil was started and stopped simultaneously during the surgery, and then the concentrations of these two drugs were monitored. The drug concentration in this paper was the result of the interaction of the two drugs, and therefore, the Cp and Ce suggested was not suitable for the recovery prediction of a single drug. We found that the recovery of patients was satisfied when removed the LMA at the suggested Cp and Ce of the two drugs. Future prospective studies are required to validate the predictive capability of Cp and Ce values for the level of consciousness during the recovery period. Dedicated efforts to develop novel pharmacokinetic-pharmacodynamic models of drugs to predict depth of anesthesia and improve the TCI pump can lead to the determination of more accurate concentrations of propofol and remifentanil to guide postoperative extubation in patients undergoing day-surgery.29 Second, the study was a preliminary study conducted in a small population of non-elderly, non- obesity, and non-frail women. TCI anesthesia of propofol and remifentanil are suitable for most day hysteroscopic surgeries. Third, we only accessed the Marsh model and Minto model for TCI in this study. These models mainly adjust the drug concentration based on body weight and fail to fully consider the influence of factors such as age, gender, genes, and physiological state on drug metabolism. These factors can all lead to significant differences in an individual’s response to drugs. The effect-site concentration at recovery of consciousness is not only affected by the concentration of the effect-site when consciousness is lost, but also related to other factors. Studies have shown that the effect-site concentration at the time of recovery is negatively correlated with age.30,31 Therefore, the effect-site concentration at recovery of consciousness in the elderly is lower than that in the young. In Marsh model, age and body weight of patients are used as basic information to enter the system, but when adjusting plasma target concentration, only body weight is used as a variable and age is ignored. Schnider’s model takes age, height, and net weight as variables. Compared with Marsh model, the propofol dose calculated by Schnider model is smaller and the infusion time is longer when setting the same plasma target concentration32 and more suitable for elderly, frail or obese patients. Further research is still needed to investigate the other situations, such as in the elderly, obesity, and men. Additionally, this study does not propose specific cut-off values when using PCp, PCe, RCp, and RCe as extubation criteria.
In conclusion, the Cp and Ce of propofol and remifentanil partly reflected the recovery condition and they might be potential reference indicators, along with OAA/Scale and the recovery of spontaneous respiration, to guide the timing of extubation in patients undergoing operative hysteroscopy under general anesthesia via TCIs of propofol and remifentanil. At such might be suitable for predicting recovery time in non-elderly and non-frail women for the day surgery with fast turnover and high requirement of sobriety.
However, this study was limited to the prediction reference value of propofol and remifentanil concentrations for extubation. In future studies, we will directly measure and monitor drug concentrations through blood sample analysis to evaluate the pharmacokinetic and pharmacodynamic parameters more precisely. Besides, more advanced pharmacokinetic models, such as the Schnider model with increased sample diversity, including patients of different ages, weights, and health conditions will be considered. We believe that although this study has limitations, the obtained data still provide valuable insights into the application of TCI of propofol-remifentanil in daytime surgeries.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval
This study has been registered on Chinese Clinical Trial Registry with accession number of chiCTR2000034837. The study protocol was approved by the Ethics Committee of International Peace Maternal and Child Health Hospital, School of Medicine, Shanghai Jiao Tong University (approval number: GKLW2019-49). The study protocol was in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants.
Funding
There is no funding that supported this work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cholkeri-Singh A, Sasaki KJ. Hysteroscopy safety. Curr Opin Obstet Gynecol. 2016;28(4):250–254. doi:10.1097/gco.0000000000000289
2. Hinkelbein J, Lamperti M, Akeson J, et al. European society of anaesthesiology and European board of anaesthesiology guidelines for procedural sedation and analgesia in adults. Eur J Anaesthesiol. 2018;35(1):6–24. doi:10.1097/eja.0000000000000683
3. Conway A, Sutherland J. Depth of anaesthesia monitoring during procedural sedation and analgesia: a systematic review and meta-analysis. Int J Nurs Studies. 2016;63:201–212. doi:10.1016/j.ijnurstu.2016.05.004
4. Conway A, Sutherland J. Depth of anaesthesia monitoring during procedural sedation and analgesia: a systematic review protocol. Syst Rev. 2015;4:70. doi:10.1186/s13643-015-0061-z
5. Oliveira CR, Bernardo WM, Nunes VM. Benefit of general anesthesia monitored by bispectral index compared with monitoring guided only by clinical parameters. Systematic review and meta-analysis. Braz J Anesthesiol. 2017;67(1):72–84. doi:10.1016/j.bjane.2015.09.001
6. Rüsch D, Arndt C, Eberhart L, Tappert S, Nageldick D, Wulf H. Bispectral index to guide induction of anesthesia: a randomized controlled study. BMC Anesthesiol. 2018;18(1):66. doi:10.1186/s12871-018-0522-8
7. Araújo AM, Machado H, de Pinho PG, Soares-da-Silva P, Falcão A. Population pharmacokinetic-pharmacodynamic modeling for propofol anesthesia guided by the bispectral index (BIS). J Clin Pharmacol. 2020;60(5):617–628. doi:10.1002/jcph.1560
8. Puri GD, Mathew PJ, Sethu Madhavan J, Hegde HV, Fiehn A. Bi-spectral index, entropy and predicted plasma propofol concentrations with target controlled infusions in Indian patients. J Clin Monitoring Computing. 2011;25(5):309–314. doi:10.1007/s10877-011-9309-x
9. Blussé van Oud-Alblas HJ, Brill MJE, Peeters MYM, Tibboel D, Danhof M, Knibbe CAJ. Population pharmacokinetic-pharmacodynamic model of propofol in adolescents undergoing scoliosis surgery with intraoperative wake-up test: a study using Bispectral index and composite auditory evoked potentials as pharmacodynamic endpoints. BMC Anesthesiol. 2019;19(1):15. doi:10.1186/s12871-019-0684-z
10. Kim WH, Ahn HJ, Kim JA. Interactions of propofol and remifentanil on bispectral index under 66% N(2)O: analysis by dose-effect curve, isobologram, and combination index. Korean J Anesthesiol. 2010;59(6):371–376. doi:10.4097/kjae.2010.59.6.371
11. Mudumbai SC, Pershing S, Bowe T, et al. Development and validation of a predictive model for American society of anesthesiologists physical status. BMC Health Serv Res. 2019;19(1):859. doi:10.1186/s12913-019-4640-x
12. Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the observer’s assessment of alertness/sedation scale: Study with intravenous midazolam. J Clin Psychopharmacol. 1990;10(4):244–251.
13. Jun MR, Yoo JH, Park SY, et al. Assessment of phase-lag entropy, a new measure of electroencephalographic signals, for propofol-induced sedation. Korean J Anesthesiol. 2019;72(4):351–356. doi:10.4097/kja.d.19.00019
14. Li Y, Gao J, Jiang L, Sun C, Hong H, Yu D. Severe hypertensive response to atropine therapy for bradycardia associated with dexmedetomidine: case report and literature review. Clin Pharmacol. 2024;16:27–31. doi:10.2147/CPAA.S436188
15. Vercauteren MP, Coppejans HC, Hoffmann VH, Mertens E, Adriaensen HA. Prevention of hypotension by a single 5-mg dose of ephedrine during small-dose spinal anesthesia in prehydrated cesarean delivery patients. Anesthesia Analg. 2000;90(2):324–327. doi:10.1213/00000539-200002000-00016
16. Miller GR. The jackknife-a review. Biometrika. 1974;61(1):1–15.
17. Smith WD, Dutton RC, Smith NT. Measuring the performance of anesthetic depth indicators. Anesthesiology. 1996;84(1):38–51. doi:10.1097/00000542-199601000-00005
18. Lewis SR, Pritchard MW, Fawcett LJ, Punjasawadwong Y. Bispectral index for improving intraoperative awareness and early postoperative recovery in adults. Cochrane Database Syst Rev. 2019;9(9):Cd003843. doi:10.1002/14651858.CD003843.pub4
19. Punjasawadwong Y, Chau-In W, Laopaiboon M, Punjasawadwong S, Pin-On P. Processed electroencephalogram and evoked potential techniques for amelioration of postoperative delirium and cognitive dysfunction following non-cardiac and non-neurosurgical procedures in adults. Cochrane Database Syst Rev. 2018;5(5):Cd011283. doi:10.1002/14651858.CD011283.pub2
20. Chen W, Jiang F, Chen X, et al. Photoplethysmography-derived approximate entropy and sample entropy as measures of analgesia depth during propofol–remifentanil anesthesia. J Clin Monitoring Computing. 2020;35(2):297–305. doi:10.1007/s10877-020-00470-6
21. Fahy BG, Chau DF. The technology of processed electroencephalogram monitoring devices for assessment of depth of anesthesia. Anesthesia Analg. 2018;126(1):111–117. doi:10.1213/ane.0000000000002331
22. Chidambaran V, Costandi A, D’Mello A. Propofol: a review of its role in pediatric anesthesia and sedation. CNS Drugs. 2015;29(7):543–563. doi:10.1007/s40263-015-0259-6
23. Eleveld DJ, Colin P, Absalom AR, Struys M. Pharmacokinetic-pharmacodynamic model for propofol for broad application in anaesthesia and sedation. Br J Anaesth. 2018;120(5):942–959. doi:10.1016/j.bja.2018.01.018
24. Besch G, Chopard-Guillemin A, Monnet E, et al. Propofol-remifentanil anesthesia for upper airway endoscopy in spontaneous breathing patients: the ENDOTANIL randomized trial. Minerva anestesiologica. 2016;82(11):1138–1148.
25. Ren LQ, Sun XX, Guan Y. Effects of sevoflurane or propofol combined with remifentanil anesthesia on clinical efficacy and stress response in pregnant women with pregnancy-induced hypertension. Eur Rev Med Pharmacol Sci. 2018;22(6):1825–1829. doi:10.26355/eurrev_201803_14602
26. d’Hooghe JN, Eberl S, Annema JT, Bonta PI. Propofol and remifentanil sedation for bronchial thermoplasty: a prospective cohort trial. Resp Int Rev Thoracic Dis. 2017;93(1):58–64. doi:10.1159/000452478
27. Absalom AR, Glen JI, Zwart GJ, Schnider TW, Struys MM. Target-controlled infusion: a mature technology. Anesthesia Analg. 2016;122(1):70–78. doi:10.1213/ane.0000000000001009
28. Mu J, Jiang T, Xu XB, Yuen VM, Irwin MG. Comparison of target-controlled infusion and manual infusion for propofol anaesthesia in children. Br J Anaesth. 2018;120(5):1049–1055. doi:10.1016/j.bja.2017.11.102
29. Gonzalez-Cava JM, Reboso JA, Calvo-Rolle JL, Mendez-Perez JA. Adaptive drug interaction model to predict depth of anesthesia in the operating room. Biomed Signal Process Control. 2020;59:101931. doi:10.1016/j.bspc.2020.101931
30. Koo BN, Lee JR, Noh GJ, Lee JH, Kang YR, Han DW. A pharmacodynamic analysis of factors affecting recovery from anesthesia with propofol-remifentanil target controlled infusion. Acta Pharmacol Sin. 2012;33(8):1080–1084. doi:10.1038/aps.2012.85
31. Nunes CS, Ferreira DA, Antunes L, Amorim P. Clinical variables related to propofol effect-site concentrations at recovery of consciousness after neurosurgical procedures. J Neurosurg Anesthesiol. 2005;17(2):110–114. doi:10.1097/01.ana.0000163198.02742.9d
32. Absalom AR, Mani V, De Smet T, Struys MM. Pharmacokinetic models for propofol--defining and illuminating the devil in the detail. Br J Anaesth. 2009;103(1):26–37. doi:10.1093/bja/aep143
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

