Back to Journals » Infection and Drug Resistance » Volume 18
The First Case of Antimicrobial-Resistant Salmonella Stanley ST29 Diagnosed Secondary to Acute Cholecystitis
Authors Wang W , Liu S, Zhang M, Chen Y, Liang Y, You S, Lv P, Xu X, Zhang F
Received 5 December 2024
Accepted for publication 24 April 2025
Published 5 May 2025 Volume 2025:18 Pages 2283—2290
DOI https://doi.org/10.2147/IDR.S507875
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Oliver Planz
Wenqing Wang,1,2,* Shufen Liu,3,* Minlan Zhang,3 Yan Chen,4 Yanru Liang,1,2 Shuqi You,1,2 Peijun Lv,4 Xuebin Xu,5 Fenghua Zhang3
1Department of Microbiology, Shanghai Pudong New Area Center for Disease Control and Prevention (Shanghai Pudong New Area Health Supervision Institute), Shanghai, People’s Republic of China; 2Fudan University Pudong Institute of Preventive Medicine, Shanghai, People’s Republic of China; 3Department of Laboratory Medicine, Zhoupu Hospital Affiliated to Shanghai University of Medicine and Health, Shanghai, People’s Republic of China; 4Department of Microbiology, Panzhihua City Center for Disease Control and Prevention, Panzhihua, People’s Republic of China; 5Division of Pathogen Testing and Analysis, Shanghai Center for Disease Control and Prevention, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fenghua Zhang, Email [email protected]
Objective: To analyze the phenotypic and genomic characteristics of a non-typhoidal Salmonella bile isolate from a patient with chronic diarrhoea secondary to acute cholecystitis.
Methods: The patient presented with chronic diarrhoea lasting for two weeks, which was secondary to acute cholecystitis. The non-typhoidal Salmonella bile isolate was identified using biochemical tests, mass spectrometry, serum agglutination tests, and antimicrobial susceptibility testing. Subsequently, whole-genome sequencing (WGS) was performed to predict and annotate the serotype, multilocus sequence typing (MLST), antimicrobial resistance genes (AMR), mobile genetic elements (MGEs), and virulence genes of the isolate.
Results: The isolate was identified as Salmonella spp. by biochemical tests and mass spectrometry. The serotype of the isolate identified by serum agglutination tests was consistent with WGS prediction and was identified as Salmonella Stanley (1,4,5,12: d:1,2, ST29). It was resistant to six antimicrobial agents, including ampicillin, ciprofloxacin, cefotaxime, azithromycin, trimethoprim/sulfamethoxazole, and chloramphenicol. Five major classes of antimicrobial agents, comprising a total of 14 resistance genes were screened, including β-lactam resistance genes: blaTEM-1B, blaOXA-1, and blaDHA-1; quinolone resistance gene: qnrB4 and aac(6′)-Ib-cr; macrolide resistance genes: mph(A), mph(E), and msr(E), and folate pathway inhibitor resistance genes: sul1, sul2, and dfrA14; chloramphenicol resistance genes: floR, catA2 and catB3. T57S mutation in the parC gene was detected in the quinolone resistance-determining region (QRDR). Three plasmid replicons (IncHI2/IncHI2A, IncR, IncN) and three insertion MGEs were predicted. Forty-two virulence genes were predicted, of which 25 were secretion and transporter genes, and ten were fimbrial adherence genes. Only one invasive protein-regulated gene(inv) was found in Salmonella Pathogenicity Islands 1(SPI-1), and no Typhoid toxin genes were predicted.
Conclusion: The case of Salmonella Stanley ST29 isolated from a patient with diarrhoea lasting 55 days secondary to cholecystitis aligns with the characteristics of high drug resistance and relatively low virulence. This highlights the need for increased vigilance in clinical practice regarding invasive cases and the significant disease burden associated with the intestinal migration of antimicrobial-resistant Salmonella isolates.
Keywords: Salmonella Stanley, acute cholecystitis, antimicrobial-resistant, whole-genome sequencing, invasive
Introduction
Salmonella is a significant foodborne pathogen that is widely distributed worldwide. According to the White-Kauffmann-Le Minor scheme, over 2,600 serovars of Salmonella have been identified.1 Based on their ability to cause specific diseases in humans, Salmonella strains are categorized into two groups: Typhoidal Salmonella and Non-typhoidal Salmonella (NTS).2 Over the past few decades, NTS infections have emerged as a growing public health concern, with a notable increase in incidence rates.3 While NTS typically caused diarrhea in humans, it also led to invasive infections such as bacteremia, urinary tract infections, and meningitis, particularly in vulnerable populations like the elderly and infants.4–6
Acute cholecystitis is an acute inflammatory condition of the gallbladder, characterized by severe abdominal pain, fever, and nausea.7 It is most commonly caused by gallstone obstruction of the cystic duct, resulting in bile stagnation and subsequent bacterial infection.8 Gallbladder disease affected approximately 20 million individuals in the United States, with 20% of patients with gallstones developed gallstone-related complications at an annual incidence rate of 1% to 4%.9 Calculous acute cholecystitis is the first clinical presentation in 10% to 15% of all patients with gallstones.9
The pathogenesis of acute cholecystitis involves a complex interplay between bacterial infection, inflammation, and host immune response.7 The etiology of acute cholecystitis is multifactorial. Previous studies have reported that approximately 20% of acute cholecystitis cases were due to intestinal bacterial infections, with the most common pathogens being Escherichia coli, Klebsiella spp., and Enterococcus spp.7,10 Nevertheless, several recent studies have underscored the emerging role of NTS as a pathogen in acute cholecystitis, particularly among immunocompromised individuals or those with pre-existing biliary tract diseases.11–13 For instance, notable cases included emphysematous cholecystitis caused by Salmonella Derby in the United States, Salmonella Enteritidis cholecystitis in Japan, and Group D NTS cholecystitis in China. Salmonella, with its unique virulence factors and ability to invade host tissues, may contribute to the severity and progression of acute cholecystitis. Despite these reports, the clinical impact of NTS-associated acute cholecystitis and characteristics of the isolates remained poorly documented and understood.
Here, we report the first case of antimicrobial-resistant Salmonella Stanley ST29 diagnosed in a patient with acute cholecystitis in Shanghai, China. We also provide detailed phenotypic and genomic analyses of the isolate, offering valuable scientific evidence for the prevention and control of NTS-related acute cholecystitis infections and for assessing the associated disease burden.
Materials and Methods
Case Presentation
On October 12, 2023, a 59-year-old male patient was admitted to Zhoupu Hospital, presenting with a 15-day history of diarrhea (occurring three times per day), loose stools, and abdominal distension. However, he did not experience vomiting or fever. The patient had a medical history of diabetes. Laboratory tests revealed elevated white blood cell (WBC) count at 18.08×109/L, with neutrophils comprising 87.40% of the total. Additionally, C-reactive protein (CRP) levels were at 103 mg/L, and serum amyloid A (SAA) was above the measurable limit at >320 mg/L. Despite the clinical indications, the patient refused to undergo pathogen isolation testing. As a result, empirical treatment with cefazoxime sodium (administered at 2.25 g per dose, twice daily) was initiated as a symptomatic intervention.
On November 21, the patient was admitted to the emergency room with unprovoked right upper abdominal pain, accompanied by radiating pain to the right shoulder and chest tightness. Upon admission, the patient’s temperature was 36.8°C, and the heart rate was 75 beats per minute. Laboratory tests revealed WBC: 11.90×109/L, with neutrophils comprising 75.00% of the total. CRP and urinary amylase levels were within normal limits. Imaging studies, including ultrasound, X-ray computed tomography (CT), and magnetic resonance imaging (MRI), diagnosed acute cholecystitis and the presence of stones in the neck of the gallbladder (Figure 1A). The following day, the patient underwent laparoscopic cholecystectomy, during which bile was collected for pathogen detection. On November 24, the laboratory reported the isolation of Salmonella spp. from the bile sample, which was subsequently sent to the public health laboratory for further identification (Figure 1B).
 |
Figure 1 Imaging of the patient with the arrow pointing to the location of the gallbladder (A), and the morphology of Salmonella after incubation at 37°C for 24 hours (B). |
Confirmation and Phenotypic Identification
The Salmonella isolate (GenBank ID: SAMN42186027) was confirmed by both VITEK 2 Compact (BioMérieux, France) and MALDI-TOF-MS (Bruker, Germany) in accordance with the protocols outlined in the Standard for Infectious Diarrhea (WS271-2007), Appendix B.1. Serum agglutination tests were conducted using Salmonella diagnostic serum and H antigen-inducing medium (SSI, Denmark) and were determined by referring to the White-Kauffmann-Le Minor scheme (9th edition). The antimicrobial susceptibility testing of the isolate was conducted using the minimum inhibitory concentrations (MICs) according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI) (M100-Ed34, 2024). Escherichia coli (ATCC25922) and Klebsiella pneumoniae (ATCC700603) were used as reference strains for quality control. Ten antimicrobial agents used in our study were as follows: ampicillin; ciprofloxacin; cefotaxime; azithromycin; imipenem; meropenem; ertapenem; trimethoprim/sulfamethoxazole; chloramphenicol and tetracycline.
Whole-Genome Sequencing (WGS) and Genomic Analysis
DNA libraries were constructed using KAPA SYBR® FAST qPCR kits (Kapa Biosystems, USA) and sequenced using the Illumina HiSeq PE150 sequencing platform (Illumina, USA). Paired-end reads (150 bp) were generated, and the sequencing depth was ≥100x. The raw data were assembled and evaluated using CLC Genomics Workbench 24.0.1 software (Qiagen, Germany). Salmonella serotype prediction was performed using SISTR and SeqSero2. Multilocus sequence typing (MLST) was confirmed using PubMLST database (https://pubmlst.org/databases/). Antimicrobial resistance (AMR) genes, mobile genetic elements (MGEs) and virulence genes were screened using ResFinder 4.3.3 (http://genomicepidemiology.org/services/) and VFDB database (http://www.mgc.ac.cn/VFs/), respectively.
Results
Serotyping and Antimicrobial Susceptibility Testing
The serotype of the isolate was identified as Salmonella Stanley (1,4,5,12: d:1,2), which was consistent with the serotype predictions by SISTR and SeqSero2 based on WGS. The isolate exhibited resistance to six antimicrobial agents, including ampicillin, ciprofloxacin, cefotaxime, azithromycin, trimethoprim/sulfamethoxazole, and chloramphenicol. However, it remained susceptible to imipenem, meropenem, ertapenem, and tetracycline (Table 1).
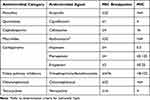 |
Table 1 Antimicrobial Susceptibility of Salmonella Stanley ST29 (μg/mL) |
MLST, AMR Genes, MGEs and Virulence Genes
The MLST of the isolate was identified as ST29. Five major classes of antimicrobial agents, comprising a total of 14 resistance genes were screened, including β-lactam resistance genes: blaTEM-1B, blaOXA-1, and blaDHA-1; quinolone resistance gene: qnrB4 and aac(6′)-Ib-cr; macrolide resistance genes: mph(A), mph(E), and msr(E), and folate pathway inhibitor resistance genes: sul1, sul2, and dfrA14; chloramphenicol resistance genes: floR, catA2 and catB3. Additionally, T57S mutation in the parC gene was detected in the quinolone resistance-determining region (QRDR). The isolate carried three plasmid replicons: IncHI2/IncHI2A, IncR, and IncN, as well as three insertional MGEs: ISSpu10, IS6100, and ISVsa3. The AMR genes mph(E) and msr(E) were located in ISSpu10, mph(A) in IS6100, and floR in ISVsa3. A total of 42 virulence genes were predicted, including 25 secretion and transporter genes, ten fimbrial adherence determinants, four nonfimbrial adherence determinants, three other virulence genes, as well. The Salmonella Pathogenicity Islands 1 (SPI-1) only contained inv gene, no highly pathogenic enterotoxin gene, such as Typhoid toxin (cdt or plt) gene, was found (Table 2).
 |
Table 2 Genomic Analysis of Salmonella Stanley ST29 |
Discussion
The World Health Organization (WHO) has estimated that the annual global incidence of Salmonella infections was approximately 550 million cases.14 While the number of cases and deaths caused by typhoid and paratyphoid (14.3 million) exceeded that of NTS (53.5 thousand),15 the overall disease burden of the latter remained higher due to its significant contribution to infectious diarrhea. Acute cholecystitis is a relatively common condition with a high disease burden, particularly among middle-aged and elderly populations worldwide. It was reported that more than 200,000 people in the United States were diagnosed with acute cholecystitis each year, with direct costs exceeding $1.6 billion annually.7 Accurate diagnosis of the etiology of acute cholecystitis and understanding the evolutionary characteristics of its pathogenic microorganisms are of great significance for the development of disease intervention policies.
The patient in this case had a history of diabetes and had been suffering from diarrhea for two weeks before the initial consultation. It was speculated that the patient had been infected Salmonella Stanley via fecal-oral route, which led to the diarrhea. Due to the lack of further epidemiological investigation, the source of Salmonella infection in the patient had not been determined. However, pathogen isolation testing was not performed simultaneously when the patient sought medical attention. The empirical treatment for three weeks failed to eliminate the antimicrobial-resistant pathogen, which persisted in the gut. A similar case was reported in Guangxi province, China.16 Subsequently, the pathogen migrated retrogradely from the gut, triggering an episode of acute cholecystitis. As one of the etiological factors for acute cholecystitis and other extra-intestinal infections, the persistence of antimicrobial-resistant Salmonella in the gut of high-risk populations should be a new focus in clinical practice.17 Accurate diagnosis of the etiology of diarrhea is an effective measure to prevent potential secondary cholecystitis. Strengthening the pathogen isolation and diagnostic capabilities of clinical laboratories is crucial for identifying and interrupting the translocation of antimicrobial-resistant, persistent pathogens within the gut that may lead to invasive diseases.
The commonly used antimicrobial agents for NTS are ciprofloxacin and third-generation cephalosporins. In recent years, multidrug-resistant NTS has been increasingly reported in clinical, environmental, and food samples.18–20 The resistance rates to ampicillin, tetracycline, and sulfamethoxazole exceed 40%, while the resistance rates to ciprofloxacin, cefotaxime, and azithromycin were below 10%.21 The recent research indicated that Salmonella Stanley ST29 isolated from pig farms harbored the super-resistant gene blaNDM-5 via the IncHI2/ST3 plasmid in Guangdong Province, China.22 In 2024, the WHO updated the Bacterial Priority Pathogens List, categorizing fluoroquinolone-resistant NTS as a high-priority pathogen.23 This classification reflected the increasing global concern regarding antimicrobial resistance. In this context, the antimicrobial-resistant Salmonella Stanley, implicated in secondary invasive cholecystitis cases, represented a convergence of both a pandemic priority pathogen and a high-priority pathogen for resistance control. This dual status significantly increased the complexity of clinical treatment and also imposed a greater disease burden on patients. Despite multidrug-resistant Salmonella being susceptible to carbapenems,24 physicians rarely used these antibiotics for treating diarrheal Salmonella infections. Therefore, culture-based antimicrobial strategies are essential to reduce empiric antibiotic use and spread of these pathogens in human populations.25
The resistance mechanism of the antimicrobial-resistant Salmonella Stanley ST29 in this case was related to resistance genes carried by plasmids and MGEs. Specifically, plasmid replicons, such as IncHI2/IncHI2A, IncR, and IncN, were capable of harboring a diverse array of resistance genes, including blaTEM, blaOXA-1, blaDHA-1, mph, msr, sul, dfrA14, and qnrB4. These plasmids have been demonstrated to be highly effective in facilitating the horizontal transfer of resistance genes among different serotypes of Enterobacteriaceae and Salmonella (such as S.Stanley, S.London, S.Typhimurium, and S.Bovismorbificans).26 For instance, the “superbug” Klebsiella pneumoniae K82 was found to possess a conjugative resistance plasmid, pK82-mcr-1 (IncFIA/IncHI2/IncHI2A/IncN/IncR), which conferred resistance to 12 antibacterial agents, including colistin.27 The plasmid characteristics and the types of resistance genes carried by this strain were highly similar to those identified in the isolates of this study. This suggests that the antimicrobial-resistant Salmonella Stanley ST29 may have acquired its super antimicrobial-resistant phenotype through horizontal gene transfer. Furthermore, studies have shown that the Inc series of plasmids carrying multidrug resistance genes, which evolving into stable clonal structures across different species within the Enterobacteriaceae family, including Klebsiella pneumoniae, Escherichia coli, and Salmonella.28 This highlights the significant role of plasmid-mediated horizontal transfer in the dissemination of multidrug resistance among clinically relevant pathogens.
Previous study has confirmed the relationship between gallbladder cancer and Salmonella infections.29 Specifically, it was demonstrated that Salmonella Typhi released the virulence factor Avr through the Type III Secretion System (TTSS). This process activated the Wnt-β-catenin signaling pathway, Janus kinase (JAK), and signal transducer and activator of transcription (STAT) pathway, ultimately leading to genomic instability in gallbladder cells. This study provided direct evidence that Salmonella Typhi played a role in the development of gallbladder cancer.29 In this case, Salmonella Stanley ST29 was found to carry the Avr virulence gene, indicating its potential carcinogenic risk. Therefore, enhancing the surveillance of Salmonella virulence genes associated with carcinogenicity in patients with acute cholecystitis is of great significance for the early prevention of gallbladder cancer. In this case, Salmonella Stanley ST29 was found to lack the Typhoid toxin gene. Previous study has shown that Salmonella adapted to the host ecological niche and enhanced its invasiveness through genomic degradation, which included gene deletion and pseudogene formation.30 In this case, it is hypothesized that Salmonella Stanley ST29 degraded highly pathogenic genes to adapt to the ecological pressure of the intestinal microbiota and the host immune response. This adaptation allowed the bacteria to persist in the intestinal tract, consistent with the patient’s clinical presentation of mild and chronic diarrhoea.
Conclusion
To our best knowledge, this study is the first case of antimicrobial-resistant Salmonella Stanley ST29 diagnosed secondary to acute cholecystitis in Shanghai, China, providing prospective insights and biological evidence for disease progression in potentially high-risk populations. It is recommended to conduct pathogen isolation and antimicrobial susceptibility testing to avoid the persistence of pathogens due to ineffective empiric antibiotic use, which may lead to secondary invasive infections. When diagnosing the causes of acute cholecystitis, clinicians should not neglect rare or uncommon etiologies. Additionally, multisource surveillance system of NTS and researches on the characteristics of strains are necessary to alert the spread of antimicrobial-resistant Salmonella worldwide. Precision clinical diagnosis and treatment, as well as precision public health measures, can effectively interrupt and warn against the human-to-human transmission of antimicrobial-resistant Salmonella cases.31
Data Sharing Statement
The data used to support the findings of this study are included within the article.
Ethics Approval and Consent to Participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study and the publication of case details were approved by the Ethics Committee of Zhoupu Hospital Affiliated to Shanghai University of Medicine and Health (No.2024-C-154-E01). Written informed consent was obtained from the patient.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The project was supported by Important Weak Disciplines of Shanghai Pudong New Area Health Commission (No. PWZbr2022-03) and Key Disciplines of Shanghai Municipal Health Commission (No. GWVI-11.1-02).
Disclosure
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
1. Issenhuth-Jeanjean S, Roggentin P, Mikoleit M, et al. Supplement 2008–2010 (no. 48) to the White–Kauffmann–Le Minor scheme. Res Microbiol. 2014;165(7):526–530. doi:10.1016/j.resmic.2014.07.004
2. Knodler LA, Elfenbein JR. Salmonella enterica. Trends Microbiol. 2019;27(11):964–965. doi:10.1016/j.tim.2019.05.002
3. Mallapaty S. The pathogens that could spark the next pandemic. Nature. 2024;632(8025):488. doi:10.1038/d41586-024-02513-3
4. Fierer J. Invasive Non-typhoidal Salmonella (iNTS) Infections. Clin Infect Dis. 2022;75(4):732–738. doi:10.1093/cid/ciac035
5. Zhan Z, Xu X, Gu Z, et al. Molecular epidemiology and antimicrobial resistance of invasive non-typhoidal Salmonella in China, 2007-2016. Infect Drug Resist. 2019;12:2885–2897. doi:10.2147/IDR.S210961.
6. Al Haddabi A, Al-Ajmi E, Al-Amrani F, et al. Nontyphoidal Salmonella Meningitis in a 5-Month-old Boy. Pediatr Infect Dis J. 2024;43(10):e379–e380. doi:10.1097/INF.0000000000004417
7. Jared RG, Charles A. Acute Cholecystitis: a Review. JAMA. 2022;327(10):965–975. doi:10.1001/jama.2022.2350
8. Liu T, Li M, Tang L, et al. Epidemiological, clinical and microbiological characteristics of patients with biliary tract diseases with positive bile culture in a tertiary hospital. BMC Infect Dis. 2024;24(1). doi:10.1186/s12879-024-09799-8
9. Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep. 2005;7(2):132–140. doi:10.1007/s11894-005-0051-8
10. Ramírez-Arbeláez JA, Arroyave-Zuluaga RL, Barrera-Lozano LM, et al. Relationship between Intraoperative Bile Culture Outcomes and Subsequent Postoperative Infectious Complications: a Retrospective Cohort Study. Biomed Res Int. 2024;2024:1–9. doi:10.1155/2024/3930130
11. Moanna A, Bajaj R, Del Rio C. Emphysematous cholecystitis due to Salmonella derby. Lancet Infect Dis. 2006;6(2):118–120. doi:10.1016/S1473-3099(06)70385-1
12. Yamashita Y, Kimura T, Tanaka N, et al. Salmonella Enteritidis cholecystitis with chronic granulomatous disease. IDCases. 2018;12:49–52. doi:10.1016/j.idcr.2018.03.012
13. Koh KJ, Lin LH. One-year-old Boy with Gallbladder Stone: a Case Report and Literature Review. J Med Ultrasound. 2020;28(4):260–263. doi:10.4103/JMU.JMU_28_20
14. WHO. Salmonella (non-typhoidal) [EB/OL]. 2024. https://www.who.int/zh/news-room/fact-sheets/detail/salmonella-(non-typhoidal).
15. Stanaway JD, Reiner RC, Blacker BF, GBD Typhoid and Paratyphoid Collaborators. The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect Dis. 2019;19(4):369–381. doi:10.1016/S1473-3099(18)30685-6
16. Zhong Y, Ruan J, Qin X, et al. Identification and clearance of high‑level drug‑resistant Salmonella Kentucky ST198.2-1 from an occupational health examinee. Chin J Lab Med. 2024;47(9):123–127. doi:10.3760/cma.j.cn114452-20231220-00368
17. Zhu M, Liu Y, Xu Y, et al. Systemic sclerosis with co‑infection by Salmonella Michigan ST2065: a case report. Chin J Lab Med. 2024;47(9):105–108. doi:10.3760/cma.j.cn114452-20240125-00052
18. Wang Y, Liu Y, Lyu N, et al. The temporal dynamics of antimicrobial-resistant Salmonella enterica and predominant serovars in China. Natl Sci Rev. 2023;10(3):nwac269. doi:10.1093/nsr/nwac269
19. She Y, Jiang Y, Luo M, et al. The Emergence of Chromosomally Located bla(CTX-M-14b) and qnrS1 in Salmonella enterica serotype Kentucky ST198 in China. Int J Antimicrob Agents. 2023;62(3):106896. doi:10.1016/j.ijantimicag.2023.106896
20. Liao Y, Wei H, Kuo H, et al. Chromosome-Borne CTX-M-65 Extended-Spectrum β-Lactamase–Producing Salmonella enterica Serovar Infantis, Taiwan. Emerg Infect Dis. 2023;29(8):1634–1637. doi:10.3201/eid2908.230472
21. Liao Y, Lauderdale T, Chang J, et al. Epidemiological trends in serotypes distribution and antimicrobial resistance in Salmonella from humans in Taiwan, 2004–2022. IJID Reg. 2024;11:100372. doi:10.1016/j.ijregi.2024.100372
22. Deng L, Lv LC, Tu J, et al. Clonal spread of blaNDM-1-carrying Salmonella enterica serovar Typhimurium clone ST34 and wide spread of IncHI2/ST3-blaNDM-5 plasmid in China. J Antimicrob Chemother. 2024;29:dkae178. doi:10.1093/jac/dkae178
23. WHO. WHO Bacterial Priority Pathogens List, 2024. Available from: https://www.who.int/publications/i/item/9789240093461.
24. Qureshi S, Naveed AB, Yousafzai MT, et al. Response of extensively drug resistant Salmonella Typhi to treatment with meropenem and azithromycin, in Pakistan. PLoS Negl Trop Dis. 2020;14(10):e8682. doi:10.1371/journal.pntd.0008682
25. Xiang Y, Zhu K, Min K, et al. Characterization of a Salmonella enterica serovar Typhimurium lineage with rough colony morphology and multidrug resistance. Nat Commun. 2024;15(1):6123. doi:10.1038/s41467-024-50331-y
26. Wang H, Cheng H, Huang B, et al. Characterization of resistance genes and plasmids from sick children caused by Salmonella enterica resistance to azithromycin in Shenzhen, China. Front Cell Infect Microbiol. 2023;13:1116172. doi:10.3389/fcimb.2023.1116172
27. Zhao Y, Qian C, Ye J, et al. Convergence of plasmid-mediated Colistin and Tigecycline resistance in Klebsiella pneumoniae. Front Microbiol. 2023;14:1221428. doi:10.3389/fmicb.2023.1221428
28. Pauly N, Hammerl JA, Grobbel M, et al. Identification of a blaVIM-1-carrying IncA/C2 multi resistance plasmid in an Escherichia coli isolate recovered from the German food chain. Microorganisms. 2021;9(1):29. doi:10.3390/microorganisms9010029
29. El TG, Garrett WS. Bacteria in cancer initiation, promotion and progression. Nat Rev Cancer. 2023;23(9):600–618. doi:10.1038/s41568-023-00594-2
30. Zhou X, Kang X, Chen J, et al. Genome degradation promotes Salmonella pathoadaptation by remodeling fimbriae-mediated proinflammatory response. Natl Sci Rev. 2023;10(10):nwad228. doi:10.1093/nsr/nwad228
31. Roberts MC, Holt KE, Fiol GD, et al. Precision public health in the era of genomics and big data. Nat Med. 2024;30(7):1865–1873. doi:10.1038/s41591-024-03098-0
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

