Back to Journals » Risk Management and Healthcare Policy » Volume 18
The Impact of Autonomy Reform on the Efficiency of Public Hospitals in China: A DEA-ITSA Combination Analysis
Authors An N , Zou Q, Li JB , Luo K , Sun G , Ni X, Xia O
Received 15 January 2025
Accepted for publication 30 March 2025
Published 16 April 2025 Volume 2025:18 Pages 1333—1346
DOI https://doi.org/10.2147/RMHP.S514512
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gulsum Kubra Kaya
Ningbo An,1,2 Quan Zou,3 Ji-Bin Li,4 Kaiyuan Luo,5 Gang Sun,6 Xing Ni,7 Oudong Xia1,8,9
1School of Public Health, Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 2Dermatology Hospital of Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 3Shenzhen Nanshan Center for Chronic Disease Control, Shenzhen, Guangdong, People’s Republic of China; 4Department of clinical research, Sun Yat-sen University Cancer Center, Guangzhou, Guangdong, People’s Republic of China; 5The Third Affiliated Hospital, Guangzhou Medical University, Guangzhou, Guangdong, People’s Republic of China; 6Department of Health Management, School of Health Management, Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 7School of Public Administration and Policy, Renmin University of China, Beijing, People’s Republic of China; 8Zhujiang Hospital, Southern Medical University, Guangzhou, Guangdong, People’s Republic of China; 9Shantou University Medical College, Shantou, Guangdong, People’s Republic of China
Correspondence: Xing Ni, Email [email protected] Oudong Xia, Email [email protected]
Purpose: Since 2014, China has been rolling out a new autonomy reform for public hospitals, aiming to enhance their efficiency and better utilize the health budgets. The purpose of this research is to assess the reform’s success and explore its effects on hospital outcome efficiency, laying a foundation based on empirical evidence for future policy decisions.
Methods: The data envelopment analysis(DEA) and interrupted time-series analysis (ITSA) approaches were combined to analyze the reform impacts on the 16 samples of Shenzhen municipal public hospitals in China, using data extracted from the Shenzhen Health Statistics Yearbook from 2002 to 2023.
Results: The results revealed that from 2002 to 2023, 15 out of 16 sample hospitals achieved total factor productivity improvement in Shenzhen city of China, with the average growth rate of Malmquist total factor productivity index(MI) was 3.05% and the highest growth rate was 6.93%, yet only one hospital showing a growth rate of − 0.02%. The results of ITSA show a significant intervention in 2014. After the policy intervention, the fixed reference Malmquist total factor productivity index(FRMI) for the general and the specialty hospital group increased at rates of 0.04680(P< 0.000) and 0.1746(p< 0.000) per year by the Newey-West model, similarly, the rates of 0.04689(P< 0.000) and 0.1762(p< 0.000) per year by the Prais-Winsten model.
Conclusion: The reform has positively impacted public hospitals’ total factor productivity(TFP). The TFP of the general hospitals was increasing before the policy intervention of autonomy hospitals, but the time of its implementation was associated with a more significant rise. Meanwhile, the TFP of specialty hospitals decreased before the intervention; however, its trend shifted to growth after the intervention. This research further emphasizes the applicability of the DEA-ITSA combination method as an effective tool for health policies evaluation using public data within China’s healthcare framework.
Keywords: public hospital reform, decentralization, autonomy, data envelopment analysis, interrupted time-series analysis, China
Introduction
China has dedicated itself to promoting the reform of public hospital autonomy to solve the problems of shortage of healthcare resources and inefficiency of medical services since 1978.1 The reform adopted a gradualist reform model, introducing market mechanisms in public hospitals, such as property rights reform, outsourcing services, and establishing public-private partnerships.2–4 In the past three decades, the governance of public hospitals in China could be characterized as a distorted semi-autonomous model.5 Beginning in 2009, China initiated a series of new health reforms, often with enhanced autonomy of hospitals, to draw public focus towards financial productivity, healthcare quality, and fostering social unity.6 In this context, the pilot reform of public hospitals was officially launched in 2010, and the “Guidance on Comprehensive Reform Urban Public Hospitals with Pilot Program” was issued by the central government.7 Between 2010 and 2016, 200 cities in China implemented reforms in public hospitals, exploring new policies, including contemporary hospital management systems, corporate governance, and public hospital financing models. These pilot cities were authorized by the central government to experiment with different policy combinations to achieve the goals of the reform.8 Shenzhen, a major city in the Guangdong province of China with a large population and a strong economy, was selected as one of the first pilot cities and has introduced a series of reform policies. The Shenzhen Municipal Government has gradually introduced a series of policies aimed at the autonomy of public hospitals, including the reform of the corporate governance structure of public hospitals, the “quota system” human resource management model, and the diagnosis-intervention packet (DIP) payment model, and so on.9
A significant number of nations remain dedicated to realizing a crucial aspect of their healthcare systems: efficiency.10,11 Based on this, some international scholars have also conducted extensive research on the impact of autonomy reform on the efficiency of public hospitals. The reform of public hospital autonomy has different implications for medical service efficiency among different countries or regions. Some developing countries have reported improvements in resource utilization efficiency, such as a reduction in average length of stay days and better inventory management control, following the implementation of autonomy reforms.12 Two studies from Kenya and Colombia found improvements in technical efficiency13 and total factor productivity of hospitals undergoing autonomy reform.14 Regarding bed occupancy rates, a study in Kenya suggested an increase in the rates due to autonomy reform, while Turkey and Vietnam had no significant impact. In contrast,15–17 two studies in Indonesia concluded that reforming hospital autonomy did not notably impact efficiency,12,18 and a research paper from Poland indicates that fiscal decentralization may decrease hospital efficiency, although these results lacked statistical significance.19 It is apparent that it remains controversial whether the autonomy reform of public hospitals has a significant impact on the efficiency of public hospitals.
Data envelopment analysis(DEA) is particularly suitable for analyzing the efficiency of organizations with multiple inputs and outputs, especially for evaluating the efficiency of health organizations.20 A systematic review summarized 317 studies on the evaluation of health system efficiency. Among these, DEA is used in 82% of frontier efficiency analyses.21–23 In another systematic review, this proportion was even higher, reaching 90%.24 Based on the above research, we are confident that DEA is a universal method for studying the efficiency of health systems. DEA’s advantage is found in spotting inefficient and optimal units, but its weak ability to reveal reasons for the inefficiencies in processes hinders the further promotion and extension of this method.25,26
This study will attempt to use a combined approach of interrupted time-series analysis (ITSA, offers a quasi-experimental research design) and DEA to compensate for the insufficiency of causal inference capabilities of DEA.27,28 Taking Shenzhen City, a pilot city for public hospital reform in China, as the research subject, this study has two objectives: firstly, to assess the impact of the autonomy reform of public hospitals on their efficiency; secondly, this research further emphasizes the applicability of the DEA-ITSA combination method as an effective tool for health policies evaluation using public data within China’s healthcare framework.
Samples and Methods
Research Design
This study was divided into three steps. First, we initially selected input and output variables based on the literature study and two-stage clustering method. In the second step, we used the appropriate DEA model to input the selected variables. We obtained the Malmquist Total Factor Productivity Index(MI) and Fixed Reference Malmquist Total Factor Productivity Index(FRMI), as well as the decomposition EC and TC of each sample hospital during different periods. Third, we utilized ITSA to analyze these indices to evaluate the efficiency changes by time series and the impact of policies on them.
Data
The data are primarily collected from Shenzhen Health Statistics Yearbook from 2002 to 2023, with the data in 2023 being in an electronic spreadsheet obtained by emailing the Shenzhen Municipal Health Commission. Overall, the study’s sample consists of public hospitals in Shenzhen, totaling 16 medical institutions, including nine general hospitals and seven specialty hospitals. This study excluded the Shenzhen Occupational Disease Prevention and Treatment Hospital, a prevention institution that does not match the characteristics of other sample hospitals; it also excludes district-level public hospitals to meet the homogeneity requirement of the DEA. The data from the electronic documents was directly imported into WPS 12.0, while the yearbook data was manually entered using a double-checking method to ensure data entry quality.
Methods
Variable Selection
Based on literature research,29–36 we initially selected the input and output variables for hospitals. Then, according to the descriptive statistical results, we removed variables with high zero-value rates, as excessive zero values lead to unstable model outputs.37 Next, we used clustering methods to preliminarily classify the sample hospitals, as the DEA model requires homogeneity among the samples. Simultaneously, we utilized the importance index of predictor variables in the two-stage clustering method to eliminate variables with low informational content. This study did not use correlation coefficients to select variables to avoid omitting variables purely on the grounds of correlation.38 Descriptive statistics and cluster analysis were performed using SPSS 26.
DEA and Model Selection
DEA, a non-parametric linear programming technique, evaluates production units’ relative efficiency by determining the ratio of a unit’s output weighted sum to the total weighted of its input.39 Efficiency indicates how well an organization has used its resources to produce the best outcome over a period. There are two main components of efficiency: allocative and technical efficiency.40 Technical efficiency refers to achieving the maximum possible output with the least available sets of inputs;24 allocative efficiency refers to the ability of an organization to utilize different input resources in optional proportion to produce a mix of different outputs.41–43
Considering Shenzhen has a population of over 20 million, we hope medical institutions can provide more healthcare services to meet the growing demand for medical treatment. Therefore, this study adopts the output-oriented model.44 The production technology of the healthcare system exhibits variable returns to scale, so this paper selects the Variable Returns to Scale(VRS) model.27,37 The standard radial model can only achieve a maximum efficiency value of 1. Andersen and Petersen proposed a method to further differentiate the efficiency levels of effective Decision Making Units(DMUs), which later became known as the super-efficiency model.45 This study requires continuous annual efficiency values for regression analysis as observation variables; thus, this model is used to further distinguish the most efficient hospitals. Technological progress must be considered when analyzing the technical efficiency of cross-period DMUs, so the Malmquist total factor productivity index DEA model is chosen.
The policy impact emerged in 2014 as the fixed frontier in the fixed-reference-Malmquist model for every DMU.46 The average value of FRMI from 16 sample hospitals between 2002 and 2023 will be used as the dependent variable in the ITSA.
Mix-sample analyzing leads to efficiency overestimation or underestimation. Thus, it is necessary to measure the efficiency separately for each type of hospital. We applied the Meta-Frontier-DEA model by Rao et al28,47 and used the Technology Gap Ratio (TGR) to measure efficiency differences across hospital types. If the TGR is more than 1, it indicates an apparent difference between different groups, making it necessary to divide all samples into various groups. The above DEA model analysis was completed using MaxDEA 8.22.
ITSA
When evaluating the effects of alterations in public policies, like introducing new legislations or taxes, scholars frequently encounter just one effective example. It’s usual in such scenarios for only aggregate data, such as unemployment rates and efficiency.48 ITSA differs from typical intervention study formats as it focuses solely on a single sample instead of contrasting it with a control group.49 Imagine acquiring several data points on a specific outcome variable both before and after the intervention.48 Under such circumstances, an ITSA adopts a quasi-experimental research style, holding promise for considerable internal reliability.49
This study uses ITSA to assess changes in the total factor productivity index of sample hospitals. Typically used in natural experiments, this approach assesses observed changing trends in variables before and after a known intervention. It’s effective in evaluating non-control group interventions and circumvents issues like bias in selecting unrecorded factors due to differences between groups.49 However, continuous observations of at least 20 points are required.50 The single-group ITSA regression model assumes the following form:51,52
The model illustrates β0 as the initial observed variable’s intercept; β1 as the gradient of variable pre-intervention; β2 as the immediate alteration in the observed variable’s value post-intervention; β3 as the variance in observational slopes before and after intervention; Yt as the cumulative outcome variable at every evenly spaced time point t; Tt as the interval from the study’s commencement; Xt as a placeholder (indicator) for the intervention (with 0 pre-intervention, or 1 otherwise); XtTt the interaction term, and εt as the residual at time t.48 The above ITSA was completed using STATA 16.
Results
Variable Selection
Selection of variables was guided by prior empirical research and literature. Input variables usually include labor, capital, and investment. Among the 256 samples, due to the adjustment of statistical indicators by the Shenzhen Municipal Health Commission, nine indicators are no longer included in the yearbook. We have removed these indicators:1) recovery rate, 2) mortality rate, 3) bed workdays, 4) bed utilization rate, 5) bed turnover rate, 6) bank loans, 8) total actual bed days occupancy, and 9) discharged patients bed days.
Frequency statistics show that some labor variables, such as radiologists, clinical technologists, support staff, and as well as capital, such as the annual actual total investment, total construction investment, and total equipment purchase amount, exhibit over 20% zero values, then removed them. Finally, we used the two-step cluster method to select the indicators on the importance of predictor variables above 0.853 and excluded several indicators, such as the management staff and pharmacists. Ultimately, this study used the total number of employee staff, the total number of medical and technical, and the number of registered doctors and nurses to represent human resources, while the number of beds served as a capital input variable.
Output variables usually include the number of outpatient visits, inpatients, medical services, income, quality, etc. After removing non-continuous indicators and those with more than 20% zero values, we used a two-step cluster classification method to predict variable importance below 0.8, eliminating indicators such as average medical expenses per patient visit, etc. Ultimately, in this study, the number of patient visits, outpatient visits, and discharges were used to represent medical service factors, while outpatient and inpatient medical revenue were used to describe revenue factors as output variables. Descriptive statistics of the input-output variables are shown in Table 1.
 |
Table 1 Descriptive Statistics |
Test and Analysis of the TGR
Considering the DEA requirements for the homogeneity of DMUs, we conducted TGR tests on different types of sample hospitals. First, we conducted a non-parametric test on two groups of hospital data, and the statistical results indicated that neither conformed to a normal distribution.
The Mann–Whitney U-test suitably revealed statistically significant differences between the two groups of TGR, as shown in Table 2. Next, comparing the mean TGR values of the two groups, the results indicated differences in the mean TGR values and the meta-technology frontier. Compared to the meta-frontier, the general group was higher, while the specialty group was lower, as shown in Table 2. Clearly, it is necessary to measure their MI separately, ensuring that their technical efficiency values are closer to reality. This result also corroborates the findings of the previous cluster analysis.
 |
Table 2 Comparison of Technical Efficiency Gap Between General and Specialized Public Hospitals in Shenzhen From 2002 to 2023 |
Results of DEA
This study applied the Super Efficiency and MetaFrontier-Fixed Reference Malmquist model with output-oriented parameters and the VRS model. The year (2014) is confirmed as the fixed frontier period to measure each DMU’s Malmquist total factor productivity index (MI and FRMI). The cumulative MI was used to analyze whether each sample hospital improved the total factor productivity from 2002 to 2023. The accumulative MI from 2002 to 2023 is used to evaluate the samples and determine whether these hospitals achieved TFP progress. The FRMI is used as the outcome variable for the ITSA to analyze the impact of policy intervention.
From 2002 to 2023, 15 out of 16 sample hospitals achieved total factor productivity improvement, with only one hospital showing a growth rate of −0.02%. The highest growth rate was 6.93%, and the average growth rate was 3.05%, as shown in Table 3. Using the FRMI, we observed the time-series trend of efficiency change for two groups of hospitals during different periods (Figure 1). Both the general and the specialty groups showed an upward trend after 2014. Before 2014, the specialized group showed a downward trend, while the general group showed an upward trend. The trend change for the specialty group before and after the intervention is easily observable (Figure 1b); unfortunately, the general group cannot be accurately determined (Figure 1a), requiring further analysis.
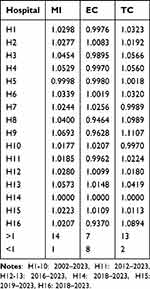 |
Table 3 Malmquist Index of 16 hospitals in SHENZHEN Between 2002 and 2023 |
 |
Figure 1 Single-group ITSA with Newey–West standard errors and one lag. (a) General-hospitals Group, (b) Specialized-hospitals Group. |
Results of ITSA
This study uses ITS to assess the impact of the autonomy policy on improving Shenzhen public hospitals’ total factor productivity progress, using a single-group design. More specifically, we evaluate whether the introduction of the autonomy policy in public hospitals has led to changes in the level and trend of FRMI in these hospitals.
Next, we specify a single-group ITSA, using the mean FRMI of two group sample hospitals in each period as the observed variable and 2014 as the start of the intervention. We request the post-intervention trend estimates and plot the results. The model is estimated using Newey (zero lag) and the Prais model.
The ITSA Results of the General Hospital Group
As shown in the Table 4 model (1), the initial level of FRMI was estimated at 0.919, and FRMI appeared to increase every year before 2014 by 0.00668 (P=0.189, CI= [−0.003, 0.016]), but this increase was not statistically significant. In the first year of policy intervention (2014), FRMI appeared to be a substantial increase of 0.182 (P<0.000, CI= [0.110, 0.255]), followed by a significant increase in annual trend (relative to the pre-intervention trend) of 0.0401 (P<0.000, CI= [0.025, 0.054]). We also see, from the lincom estimate produced by specifying post trend, that after the introduction of the autonomy policy, the FRMI increased annually at the rate of 0.0468 per year (P<0.000, 95% CI= [0.037, 0.056]), as shown in Table 4, Model ID (1). Figure 1a provides a visual display of these results.
 |
Table 4 ITSA Results for General-Hospitals Group Only |
Then, actest was used to ensure that a fitting model could accurately explain the autocorrelation structure. As shown in the Output table, autocorrelation is not present from lag 1 to 9. Thus, the initial model specifying lag (0) should correctly account for this autocorrelation.
We use another Prais model to cross-validate the results with the Newey model. The former is designed to adapt to the AR (1) model and add robust standard errors, while the latter is based on an OLS model.
The two models cannot be directly compared with the output parameters since the estimates produced using Prais are transformed. However, these results confirm a significant increase in the annual trend of FIMI of 0.0399 (relative to the trend before policy intervention, P < 0.000, CI = [0.022, 0.058]). The Prais model provides the Durbin-Watson d statistic to indicate the model’s correction for first-order autocorrelation. d can take on values between 0 and 4; under the null hypothesis, d equals 2. A value of d less than 2 indicates positive autocorrelation (p > 0), while a value of d greater than 2 indicates negative autocorrelation (p < 0). After transformation, the d value decreased from 2.221 to 2.004, as shown in Table 4, Model ID (4).
The ITSA Results of the Specialty Hospital Group
We repeated the above steps for the specialty hospitals group and obtained the estimated results, as shown in Table 5 Model ID (7), (10) and Figure 1b.
 |
Table 5 ITSA Results for Specialized-Hospitals Group Only |
Results of the Robust Test
We conducted the ITSA robust test using two approaches: setting different intervention starting times and altering different model estimation methods. Using the Newey model to output results, we observed that the general group’s results showed a significant increase in the annual trend of FRMI changes (relative to the pre-intervention trend of 0.0511 (P <0.000) and 0.0553 (P <0.000), and the specialty group’s result showed the change of 0.224 (P <0.000) and 0.235 (P <0.000) per year at the intervention start years in 2015 and 2016. We also obtained significant results regarding the observed variables’ changes in intervention effects using another Prais model. The results are shown in Tables 4 and 5.
However, the AIC and BIC values of the Newey model outputs for the three different intervention points from 2014 to 2016 gradually increased, and the adjusted R2 value of the Prais model outputs gradually decreased, indicating a decline in model fit. Fortunately, the Newey and Prais models yielded significant analytical results, giving us confidence that the intervention effectively influences the observed variables.
Discussions
Autonomy and the Efficiency of Public Hospitals
Challenges in public hospital systems common to public services include technical and distributional inefficiency; diminished productivity; lack of patient responsiveness; waste generation; among others. Lately, the concepts of autonomization and corporatization, akin to recent public sector organizational advancements, have been increasingly considered to enhance hospital performance.10 Autonomy reform of public hospitals leads to intensified market competition, which can improve healthcare efficiency and quality.54,55 The concept of hospital autonomy involves the transfer of administrative authority to the hospital management groups.56 The core idea is to grant hospitals greater autonomy to enhance operational efficiency.57
Hospitals play an important role in boosting healthcare expenses and form the primary segment of healthcare spending in numerous nations,58 hence the focus of various reforms aiming to curb costs and enhance the value of healthcare expenditures.59 Hospital autonomy reform initiatives began in developed nations including France, the Netherlands, Italy, New Zealand, the United Kingdom, and the United States, and from 1980 onwards, extended to developing countries like Ghana, India, Indonesia, Uganda, Zambia, and Kenya.20 A holistic review summarized six major themes, based on 27 articles, about the effects of autonomy reform on hospitals:5,60 healthcare quality, hospital management indicators, type and number of services, social functions, financial management, and individuals, both of staffs and patients.56 Adopting the Preker Harding model, one Chinese research indicates that hospital autonomy reform has impacted hospital costs and public welfare, medical service quality and efficiency, and accountability.57 From the literature review, we can observe that the impact of hospital autonomy reforms on healthcare services varies across different countries.
Positive Impact on the TFP of Public Hospitals
Descriptive analysis shows that 15 of 16 sample hospitals from 2002 to 2023 achieved progress in total factor productivity. Based on MI growth, we can use FRMI as the outcome variable for the ITSA method; otherwise, the analysis results would be inaccurate.37
The results of this study indicate that between 2002 and 2023, the efficiency levels of municipal public hospitals in Shenzhen varied depending on the type of hospital. Through the mean FRMI scatter plot, general hospitals displayed a gradual upward trend with a more significant increase after 2014; however, the slope change is difficult to distinguish. Meanwhile, specialty hospitals followed a V-shaped trend, as shown in Table 1 and Figure 1.
Consistent with the descriptive analysis results, the ITSA method showed a significant intervention in 2014. After the policy intervention, the FRMI for the general and the specialty hospital groups increased at rates of 0.04680 (P<0.000) and 0.1746 (P<0.000) per year. Our findings can support the conclusion that the autonomy reform of public hospitals is proceeding as planned and significantly affects the efficiency of Shenzhen municipal public hospitals, which may be optimistic.
We observed that the FRMI did not show statistically significant changes over time in the general hospital group’s ITSA results before the policy intervention. Therefore, we attempt to adjust the intervention period to 2015 and 2016, and then obtain the statistically significant estimated parameters both in the Newey and the Prais models.
However, the AIC and BIC of the Newey model outputs for the three different intervention points from 2014 to 2016 gradually increased, and the R² of the Prais model outputs gradually decreased, indicating a decline in the model’s fit (Table 4 Model 2,3,5,6,8,9,11,12).
According to the results of ITSA in the specialized hospital group, except for the first year of intervention in 2014, the level changes of the outcome variable were not statistically significant. The intervention did not immediately change the level of the variable but significantly increased its annual growth rate. These results indicated that policy interventions have a positive long-term impact on the observed variable (Table 5).
The robust test results are acceptable. Nevertheless, we also found that the AIC and BIC for the Newey model in the general hospital group gradually increased at the three different intervention points, indicating a decline in model fit. Additionally, the R² for the Prais model in 2014, 2015, and 2016 showed a downward trend in both groups, further suggesting a decline in model fit. The trend may be related to the reduced number of observations as the intervention period is backward, meaning fewer observations lead to worse model fitting.50
This study demonstrates that the nationwide public hospital reform initiated in 2014 may have positively impacted the improvement of public hospitals’ efficiency. The ITSA results show that the FRMI of general hospitals increased from 0.00668(P>0.05) to 0.0401(P<0.000) annually; the FRMI of specialty hospitals shifted from a yearly decrease of −0.065 (P=0.017) to an increase of 0.240 (P<0.000). Through decomposition analysis of EC and TC, the efficiency improvements mainly stemmed from technological advances (81.25% of sample hospitals had a cumulative TC greater than one from 2002 to 2023), while the contribution of technical efficiency was limited (43.75% of sample hospitals had a cumulative EC greater than one from 2002 to 2023). Additionally, we found that 31.25% of sample hospitals saw contributions from technical efficiency and technological advances to overall efficiency improvements, achieving optimal efficiency. See K.’s research, which indicates that the TFP of public hospitals in Shenzhen from 2005 to 2013 was declining,61 consistent with the conclusion for specialty hospitals in this study but not general hospitals. See’s research may have led to an underestimation of the efficiency of general hospitals. This result also confirms the necessity of using the Meta-DEA model.
Our research indicates that the reform has a more significant impact on specialized hospitals. This result is consistent with the studies of Feng Ying,6 Liu Song,62 Chen Xinlan,63 and Xia Qing64 but inconsistent with the findings of Wu Jian65 and Wu Guangyi.66 By decomposing the MI, we observed that only one specialized hospital achieved simultaneous progress in EC and TC, while the majority of specialized hospitals experienced a decline in EC. There are several reasons why the TFP of specialized hospitals is slightly lower than the Meta-frontier, possibly due to their smaller scale and relatively insufficient investment in human resources compared to general hospitals; specialized hospitals, due to their limited service population, are restricted in expanding their medical service volume. However, in cities, smaller hospital areas imply better transportation convenience, and by focusing on a specific field of expertise, they are more likely to maximize the advantages of medical technology and attract more patients.66 Producing greater output with fewer inputs may be an essential reason for the more significant efficiency changes they experience after policy impacts.
Promotion of Local Hospital Management by Autonomy Reform
This study asserts that the autonomy reform has a positive impact on the efficiency of public hospitals, which may be the result of the combined effect of four policy tools in the following aspects.
First, the reform of autonomy expanded the management authority of hospitals. This allowed hospitals to make timely decisions in internal management matters without needing government approval or using a filing process. The decision-making procedures were shortened, saving time.67
Secondly, the new human resources management model adopts a system where a relatively fixed total number of staff is determined based on the number of hospital beds and the hospital’s grade but allows hospitals to adjust the actual total staff number freely according to operational needs.67 Hospitals are organizations that are intensive in technical personnel, and the provision of medical services relies on a large number of experienced medical staff. Determining a fixed total number of staff based on bed numbers often leads to a dilemma where there is both redundancy in personnel and ineffective motivation. The optimal strategy for hospitals is to dynamically adjust the ratio between labor costs and effective incentives while ensuring the service workload and quality, maintaining a balance in human resource management efficiency.
Third, the hospital funding reform mainly implemented the DIP payment system, which is similar to the internationally popular diagnosis-related groups (DRGs).68 Due to its simplicity in operation and relatively low difficulty in implementation, this method can be adapted to regions across the country with different economic levels. A study from a city in China shows that the DIP payment model has achieved positive results in reducing patients’ economic burden and improving care quality.69
Fourth, a comprehensive performance evaluation and patient satisfaction survey were implemented. Since 2013, sample cities have conducted comprehensive hospital performance evaluations for all municipal public hospitals in the region, linking the results to the appointment of hospital directors.9 Since 2013, annual and quarterly random patient satisfaction surveys have been conducted for all public hospitals in the region, and the results have been made publicly available on a quarterly and annual basis.9 The comprehensive performance evaluation and patient satisfaction surveys are important policy tools for accountability, effectively promoting the progress of hospital management.
Further Policy Analysis
Firstly, reforming the corporate governance structure of public hospitals enhances hospital autonomy and improves the efficiency of hospital decision-making by defining the scope of hospital operation authority. Secondly, the quota system human resource management model has been adopted, which determines government subsidy standards based on the workload for medical services rather than a fixed staffing quota amount. A post-management model featuring de-administration and de-institutionalization is implemented in newly established hospitals. These measures have enhanced the autonomy of hospitals in human resource management and reduced human capital expenditure. Thirdly, a financing model for public hospitals is primarily based on government procurement of services. Medical insurance institutions purchase medical services from public hospitals through a payment method via a DIP. The medical pricing structure has been adjusted, eliminating the markup on public hospital drug sales while increasing the prices of technical medical services. The fourth is to enhance the informatization capabilities of hospitals, build a regional public hospital information data platform centered around electronic medical records, and promote the refinement, intelligence of hospital management, and the convenience of patient medical services. Lastly, performance assessment and patient satisfaction evaluation should be implemented in public hospitals, and the assessment results should be linked to government investment in these hospitals.70
Additionally, Shenzhen City has adopted the “separation of ownership and operation” model since 2013 to collaborate with internationally and domestically renowned medical institutions such as The University of Hong Kong, Southern Medical University, Chinese Academy of Medical Sciences, and Sun Yat-sen University to co-construct public hospitals.67 The introduction of these hospitals has, on one hand, promoted the enhancement of medical technology and improvement of hospital management, and on the other hand, stimulated medical market competition, encouraging public hospitals to strive to improve their service technology and service levels to attract more patients.70,71
Compared to the Other Pilots
Compared with the medical reforms in other pilots of China, the autonomous reform of public hospitals in Shenzhen seems to be more successful. Xia Qing64 and Wu Jingjing72 reported that the public hospital reform evaluation results in the pilot city of Jiangsu Province showed a decline in TFP. Bai Jie’s study showed that the TFP of public hospitals in Zhuhai City also declined.73 Zheng’s74 research also found that two-thirds of the hospitals in Chongqing still have space for efficiency improvement. Cao Xinxin63 studied the efficiency evaluation of public hospitals in Tianjin, and the results showed that TFP progress was mainly due to TE progress. At the same time, some studies have yielded positive results. The research samples from Shanghai and Weifang City showed that the reform is conducive to the progress of TFP in public hospitals. Different research findings illustrate that a poor policy mix or insufficient complementary policy measures in medical reform may lead to unsuccessful outcomes.
What issues arise from solely pursuing efficiency improvements? Tsuei75 and Zhang X76 suggest that although efficiency has improved, hospital costs have not been effectively controlled, and overall, the reform has not achieved its expected goals. The fundamental reason is the unaltered motivation system for providers in service delivery.76
Conclusion
This study used the Meta-Frontier-Malmquist and super-efficiency model to assess Shenzhen municipal public hospitals’ total factor productivity index between 2002 and 2023. Then, we evaluated the effect of autonomy reform on hospital efficiency by using descriptive analysis and the ITSA method with a single group. Studies have confirmed that the autonomy reform has positively impacted the total factor productivity(TFP) of public hospitals. Therefore, we have demonstrated that the policies introduced by the Shenzhen municipal government to promote the autonomy of public hospitals have effectively improved their efficiency. This study suggests that conducting policy pilots simultaneously across multiple cities can help the central government quickly identify effective policy measures and find the optimal policy combination, thereby improving policy quality. This model is also a policy-making method frequently used by China’s politicians. This research further emphasizes the applicability of the DEA-ITSA combination method as an effective tool for health policy evaluation using public data within China’s healthcare framework.
Data Sharing Statement
This study analyzed publicly available datasets. The data can be found here: Shenzhen Health Statistical Yearbooks published from 2002 to 2022, and the 2023 data is in an electronic spreadsheet obtained by emailing the Shenzhen Municipal Health Commission.
The initial work of the study is part of the main article; additional questions can be addressed to the corresponding author or first author.
Ethics Approval and Consent to Participate
The Medical Ethics Committee of Dermatology Hospital of Southern Medical University confirmed: Ningbo An’ s paper” The impact of autonomy reform on the efficiency of public hospitals in China: a DEA-ITSA combination analysis” does not involve the category of medical ethics, so there is no need for medical ethics review.
Acknowledgments
The authors gratefully acknowledge the Shenzhen Municipal Health Commission, which provided the data for this study, Guoying Dong from the Second People’s Hospital of Shenzhen, who provided policy consultation. Xiaobo Xie provided data collection consulting; professional Zhirong Zeng from Guangdong Medical University provided the research design consultation; and professional Jiajian Zhou from Dermatology Hospital of Southern Medical University provided the writing consultation.
Every assertion in this document solely belongs to the writers and may not represent the positions of the associated groups, the publisher, editors, or critics. The product under review in this paper or the manufacturer’s claims are not assured or supported by the publisher.
Funding
This research was funded by the 2019 General Project Foundation of Humanities and Social Sciences Research of the Ministry of Education of the People’s Republic of China: Research on the Evaluation of the Decentralization Reform Effect of Public Hospitals Based on DEA: A Case Study of Shenzhen city, grant number 19YJC630001.
Disclosure
The authors declare that their study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Zan X. The Echo of History: china’s State-owned Hospital Reform(1978-1992). Res Chin Econ Hist. 2020;2020(02):175–190.
2. Qian Ran HE, Song DENG D, Yu Jiao LI. The Evaluation on China’s Reform of Public Hospitals Based on Public Policy Theory. Soc Secur Stud. 2014;(01):3–13. doi:10.3760/cma.j.issn.0254-6450.2015.09.023
3. Zhang YJ. The Pilot Mechanism of Policy in the Gradually Advancing Reform. Reform. 2017;2017(09):38–46.
4. Huang Y, Qian M. How gradualist are Chinese reforms? Evidence from rural income determinants. Eur J Finance. 2018;24(1):19–35. doi:10.1080/1351847X.2017.1290669
5. Allen P, Cao Q, Wang H. Public hospital autonomy in China in an international context. Int J Health Plann Manage. 2014;29(2):141–159. doi:10.1002/hpm.2200
6. Feng Y, Wang M, Wang L, Han AQ, Tang Y. Analysis on the efficiency of health resource allocation in 17 types of medical institutions in Beijing. Chin Health Econ. 2024;43(10):67–72.
7. China G 2012. Guidance on comprehensive reform urban public hospitals with pilot program. 2015. Available from: https://www.gov.cn/zhengce/content/2015-05/17/content_9776.htm.
8. Hao H, Bei WS. The number of pilot cities for public hospital reform has increased to 200. 2016. Available from: https://www.gov.cn/xinwen/2016-04/26/content_5068239.htm.
9. Lifen F, Quan Z, Jibin L, et al. Knowledge graph-based bibliometric visualization analysis of the research on reform policy of de-administration in public hospitals. Chin J Med Manag Sci. 2022;12(04):82–87.
10. Preker AS, Harding A, editors. Innovations in Health Service Delivery: The Corporatization of Public Hospitals. World Bank; 2003.
11. Papanicolas I. Health System Performance Assessment: A Framework for Policy Analysis.
12. Maharani A, Tampubolon G. The double-edged sword of corporatisation in the hospital sector: evidence from Indonesia. Health Econ Policy Law. 2017;12(1):61–80. doi:10.1017/S174413311600027X
13. Collins D, Njeru G, Meme J, Newbrander W. Hospital autonomy: the experience of Kenyatta National Hospital. Int J Health Plann Manage. 1999;14(2):129–153. doi:10.1002/(SICI)1099-1751(199904/06)14:2<129::AID-HPM541>3.0.CO;2-R
14. McPake B, Yepes F, Lake S, Sanchez L. Is the Colombian health system reform improving the performance of public hospitals in Bogota? Health POLICY Plan. 2003;18(2):182–194. doi:10.1093/heapol/czg023
15. Sarp N, Esatoğlu AE, Akbulut Y. An example of health sector reforms in turkey: hospital decentralization (health enterprises). J Ank Med Sch. 1–10. doi:10.1501/Jms_0000000004
16. Wagstaff A, Bales S. The Impacts of Public Hospital Autonomization: Evidence From a Quasi-Natural Experiment. The World Bank; 2012; doi:10.1596/1813-9450-6137
17. London JD. The promises and perils of hospital autonomy reform by decree in Viet Nam. Soc Sci Med. 2013;96:232–240. doi:10.1016/j.socscimed.2013.07.009
18. Govindaraj R, Chawla M. Recent Experiences With Hospital Autonomy in Developing Countries – What Can We Learn? Harvard School of Public Health; 1996.
19. Kosycarz E, Dedys M, Ekes M, Lawa D WW. The effects of provider contract types and fiscal decentralization on the efficiency of the Polish hospital sector: a data envelopment analysis across 16 health regions. Health POLICY. 2023;129. doi:10.1016/j.healthpol.2023.104714
20. Mbau R, Musiega A, Nyawira L, et al. Analysing the efficiency of health systems: a systematic review of the literature. Appl Health Econ Health Policy. 2023;21(2):205–224. doi:10.1007/s40258-022-00785-2
21. Hollingsworth B. Non-parametric and parametric applications measuring efficiency in health care. Health Care Manag Sci. 2003;6(4):203–218. doi:10.1023/A:1026255523228
22. Hollingsworth B, Dawson PJ, Maniadakis N. Efficiency measurement of health care: a review of non-parametric methods and applications. Health Care Manag Sci. 1999;2(3):161–172. doi:10.1023/a:1019087828488
23. Hollingsworth B. The measurement of efficiency and productivity of health care delivery. Health Econ. 2008;17(10):1107–1128. doi:10.1002/hec.1391
24. Babalola TK, Moodley I. Technical efficiency and productivity of public district hospitals in KwaZulu-Natal province, South Africa. J Public Health Res. 2020;9(1):1741. doi:10.4081/jphr.2020.1741
25. Kohl S, Schoenfelder J, Fügener A, Brunner JO. The use of data envelopment analysis (DEA) in healthcare with a focus on hospitals. Health Care Manag Sci. 2019;22(2):245–286. doi:10.1007/s10729-018-9436-8
26. Charnes A, Cooper WW, Rhodes E. Measuring the efficiency of decision making units. Eur J Oper Res. 1978;2(6):429–444. doi:10.1016/0377-2217(78)90138-8
27. Banker RD, Charnes A, Cooper WW. Some models for estimating technical and scale inefficiencies in data envelopment analysis. Manage Sci. 1984;30(9):1078–1092. doi:10.1287/mnsc.30.9.1078
28. Battese GE, Rao DSP, O’Donnell CJ. A metafrontier production function for estimation of technical efficiencies and technology gaps for firms operating under different technologies. J Product Anal. 2004;21(1):91–103. doi:10.1023/B:PROD.0000012454.06094.29
29. Yin G, Ning J, Peng Y, Yue J, Tao H. Configurational paths to higher efficiency in county hospital: evidence from qualitative comparative analysis. Front PUBLIC Health. 2022;10. doi:10.3389/fpubh.2022.918571
30. Ilgun G, Sonmez S, Konca M, Yetim B. Measuring the efficiency of Turkish maternal and child health hospitals: a two-stage data envelopment analysis. Eval Program Plann. 2022;91. doi:10.1016/j.evalprogplan.2021.102023
31. Piubello Orsini L, Leardini C, Vernizzi S, Campedelli B. Inefficiency of public hospitals: a multistage data envelopment analysis in an Italian region. BMC Health Serv Res. 2021;21(1):1281. doi:10.1186/s12913-021-07276-5
32. Peng Z, Zhu L, Wan G, Coyte PC. Can integrated care improve the efficiency of hospitals? Research based on 200 hospitals in China. COST Eff Resour Alloc. 2021;19(1). doi:10.1186/s12962-021-00314-3
33. Yin G, Chen C, Zhuo L, He Q, Tao H. Efficiency comparison of public hospitals under different administrative affiliations in China: a Pilot city case. HEALTHCARE. 2021;9(4). doi:10.3390/healthcare9040437
34. Mitropoulos P, Mitropoulos I, Karanikas H, Polyzos N. The impact of economic crisis on the Greek hospitals’ productivity. Int J Health Plann Manage. 2018;33(1):171–184. doi:10.1002/hpm.2410
35. Flokou A, Aletras V, Niakas D. Decomposition of potential efficiency gains from hospital mergers in Greece. Health CARE Manag Sci. 2017;20(4):467–484. doi:10.1007/s10729-016-9365-3
36. Otay I, Oztaysi B, Onar SC, Kahraman C. Multi-expert performance evaluation of healthcare institutions using an integrated intuitionistic fuzzy AHP&DEA methodology. Knowl-BASED Syst. 2017;133:90–106. doi:10.1016/j.knosys.2017.06.028
37. Cheng G. Data Envelopment Analysis:Method and Maxdea Software.
38. Chilingerian JA, Sherman HD. Health-Care Applications: from Hospitals to Physicians, from Productive Efficiency to Quality Frontiers. In: Cooper WW, Seiford LM, Zhu J editors. Handbook on Data Envelopment Analysis. Vol 164. International Series in Operations Research & Management Science. Springer US; 2011:445–493. doi:10.1007/978-1-4419-6151-8_16.
39. Foroughi Z, Ebrahimi P, Aryankhesal A, Maleki M, Yazdani S. Hospitals during economic crisis: a systematic review based on resilience system capacities framework. Bmc Health Serv Res. 2022;22(1):977. doi:10.1186/s12913-022-08316-4
40. Czypionka T, Kraus M, Mayer S, Röhrling G. Efficiency, ownership, and financing of hospitals: the case of Austria. Health Care Manag Sci. 2014;17(4):331–347. doi:10.1007/s10729-013-9256-9
41. Akazili J, Adjuik M, Chatio S, et al. What are the Technical and Allocative Efficiencies of Public Health Centres in Ghana? Ghana Med J. 2008;42(4):149–155.
42. Kirigia JM, Emrouznejad A, Sambo LG. Measurement of technical efficiency of public hospitals in Kenya: using data envelopment analysis. J Med Syst. 2002;26(1):39–45. doi:10.1023/A:1013090804067
43. Moshiri H, Aljunid SM, min RMA. HOSPITAL Efficiency: CONCEPT, MEASUREMENT TECHNIQUES and REVIEW of HOSPITAL EFFICIENCY STUDIES. 2011. https://api.semanticscholar.org/CorpusID:4282935.
44. Gang C, Hua QIAN Z. Health system efficiency assessment: conceptual framework and methods using data envelopment analysis. Chin J Health Policy. 2012;5(03):52–60.
45. Andersen P, Petersen NC. A procedure for ranking efficient units in data envelopment analysis. Manage Sci. 1993;39(10):1261–1264. doi:10.1287/mnsc.39.10.1261
46. Berg SA, Førsund FR, Jansen ES, Berg SA, Forsund FR. Malmquist indices of productivity growth during the deregulation of Norwegian banking, 1980-89. Scand J Econ. 1992;
47. Rao PDS. Metafrontier Functions for the Study of Interregional Productivity Differences. Australasian Meeting of the Econometric Society. 2003.
48. Linden A, Adams JL. Applying a propensity score-based weighting model to interrupted time series data: improving causal inference in programme evaluation. J Eval Clin Pract. 2011;17:1231–1238. doi:10.1111/j.1365-2753.2010.01504.x
49. Bernal JL, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47(6):2082–2093. doi:10.1093/ije/dyy135
50. Shao H, Qi Wang Q, Yue Hua H, Liu W, Shicheng Y, Yao H. Interrupted time-series analysis and its application in public health. Chin J Epidemiol. 2015;36(9):1015–1017. doi:10.3760/cma.j.issn.0254-6450.2015.09.023
51. Huitema BE, McKean, Mckean JW, Joseph W. Design specification issues in time-series intervention models. Educ Psychol Meas. 2000;60:38–58. doi:10.1177/00131640021970358
52. Simonton DK. Cross-sectional time-series experiments: some suggested statistical analyses. Psychol Bull. 1977;84(489–502). doi:10.1037/0033-2909.84.3.489
53. Pingyan C, Shengli A. IBM SPSS Applications.
54. Chuang D, Peng Zhu H. The evolutionary logic of urban health care systems in China. Soc Sci China. 2016; 248:206.
55. Ding Z. Review of research on public service delivery in Western Countries. China Public Adm Rev. 2016;2016(1):111–131.
56. Ravaghi H, Foroughi Z, Nemati A, Bélorgeot VD. A holistic view on implementing hospital autonomy reforms in developing countries: a systematic review. Health Policy Plan. 2018;33(10):1118–1127. doi:10.1093/heapol/czy095
57. Deng QW, Wei Y, Chen YY. The characteristics and inspiration of foreign public hospital autonomy practice:based on preker-harding model. Chin Hosp Manag. 2023;43(06):93–96.
58. Barber SL, Borowitz M, Bekedam H, Ma J. The hospital of the future in China: china’s reform of public hospitals and trends from industrialized countries. Health Policy Plan. 2014;29(3):367–378. doi:10.1093/heapol/czt023
59. Docteur E, Oxley H. Health-care systems: lessons from the reform experience. 2003;9. doi:10.1787/865047648066
60. Ahmad S, Saeed A. Evaluating the nature and extent of autonomy in public teaching hospitals: a case study of Jinnah Hospital Lahore. Public Policy Adm Res. 2013;3(2):9–18.
61. See KF, Ng YC. Do hospital reform and ownership matter to Shenzhen hospitals in China? A productivity analysis. Econ Anal POLICY. 2021;72:145–155. doi:10.1016/j.eap.2021.06.008
62. Song L, Hui Z, Lin C, Qiu Z. Operation efficiency of public hospitals and private hospitals based on DEA-malmquist index, Guangdong. Mod Prev Med. 2019;46(21):3920–3924.
63. XinXin C, YiYou Z, Ying L. Dynamic evaluation on the efficiency of public hospitals in Tianjin:based on DEA-Malmquist index model. Mod Prev Med. 2020;47(19):3536–3540.
64. Qing X, Ji-xia XIONG. Operation performance evaluation of public hospitals in a typical pilot city of medical reform based on DEA-Malmquist index. Mod Prev Med. 2021;48(13):2396–2400.
65. Jian W, Zi Han MU, Xiao Li FU, et al. Operation efficiency and improvement strategy of provincial hospitals:a case study of Henan. Mod Prev Med. 2021;48(19):3560–3564.
66. Wu GY, Jin yan Tang, Xiao hua Ying. efficiency and influencing factors of municipal hospitals in shanghai from 2013 to 2019. Chin Health Resour. 2023;26(03):274–280+297. doi:10.13688/j.cnki.chr.2023.230132
67. Ningbo A, Miaowen Y, Shangqi L, et al. SWOT analysis of development strategy for major public hospitals in the Government-University Cooperation mode. Chin Hosp. 2020;24(08):41–43. doi:10.19660/j.issn.1671-0592.2020.08.12
68. Zhang Y, yi XS, Tan G-M. Tan G ming. Unraveling the effects of DIP payment reform on inpatient healthcare: insights into impacts and challenges. BMC Health Serv Res. 2024;24(1):887. doi:10.1186/s12913-024-11363-8
69. Lin K, Li Y, Yao Y, Xiong Y, Xiang L. The impact of an innovative payment method on medical expenditure, efficiency, and quality for inpatients with different types of medical insurance: evidence from a pilot city, China. Int J Equity Health. 2024;23(1):115. doi:10.1186/s12939-024-02196-2
70. Wang D, Lin H, Wang S. Exploration on the Construction of Modern Public Hospital Management System in Shenzhen.
71. Ningbo A. Connotation of organizational mission of university-affiliated hospitals. Chin J Med Manag Sci. 2022;12(03):30–36.
72. Jing Jing W, Xian Chen Z, Nan Zhang X, Gao S. Evaluating the effect of comprehensive reform on public hospitals in Jiangsu province based on intermittent time series analysis. Chin Health Serv Manag. 2018;35(03):163–166+201.
73. Bai J, Qian Fang P, Juan X, Hua Mei W. Analysis on the management efficiency of the pilot reform of Zhuhai public hospital. Chin Hosp. 2020;24(02):40–42.
74. Zheng W, Sun H, Zhang P, Zhou G, Jin Q, Lu X. A four-stage DEA-based efficiency evaluation of public hospitals in China after the implementation of new medical reforms. PLoS One. 2018;13(10):e0203780. doi:10.1371/journal.pone.0203780
75. Tsuei SH, Yip W. How hospital autonomy affects provider payment reform effectiveness. Int J Health Plann Manage. 2024;39:1350–1369. doi:10.1002/hpm.3806
76. Zhang X, Lai H, Zhang L, He J, Fu B, Jin C. The impacts and unintended consequences of the nationwide pricing reform for drugs and medical services in the urban public hospitals in China. BMC Health Serv Res. 2020;20(1):1058. doi:10.1186/s12913-020-05849-4
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


