Back to Journals » Journal of Pain Research » Volume 18
The Impact of Interscalene Brachial Plexus Block with Different Concentrations of Ropivacaine on Diaphragmatic Paralysis: A Randomized Controlled Study
Authors Deng Y, Wang L, Zhang H , Xu Z, Jiang L, Zhou Y
Received 16 December 2024
Accepted for publication 12 March 2025
Published 17 March 2025 Volume 2025:18 Pages 1341—1349
DOI https://doi.org/10.2147/JPR.S505238
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Karina Gritsenko
Ying Deng,1,2,* Liwei Wang,1,2,* Hua Zhang,3 Zhichao Xu,4 Ling Jiang,5 Yang Zhou1,2,6
1Department of Anesthesiology, Peking University Third Hospital, Beijing, People’s Republic of China; 2Beijing Center of Quality Control and Improvement on Clinical Anesthesia, Beijing, People’s Republic of China; 3Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing, People’s Republic of China; 4Department of Anesthesiology, Xuancheng People’s Hospital, Xuancheng City, Anhui Province, People’s Republic of China; 5Ultrasound Diagnosis Department, Peking University Third Hospital, Beijing, People’s Republic of China; 6Anesthesia and Perioperative Medicine Branch of China International Exchange and Promotive Association for Medical and Health Care, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yang Zhou, Department of Anesthesiology, Peking University Third Hospital, No. 49, North Garden Street, Haidian District, Beijing, 100191, People’s Republic of China, Tel/Fax +8610-82267260, Email [email protected] Ling Jiang, Department of Anesthesiology, Peking University Third Hospital, No. 49, North Garden Street, Haidian District, Beijing, 100191, People’s Republic of China, Tel/Fax +8610-82267260, Email [email protected]
Background: This study aims to evaluate the degree of diaphragmatic paralysis by assessing diaphragmatic excursion and pulmonary function following an ultrasound-guided interscalene brachial plexus block with two different concentrations of ropivacaine (0.2% and 0.5%).
Methods: Forty patients undergoing shoulder arthroscopic surgery were randomly assigned to receive ultrasound-guided interscalene brachial plexus block with 20 mL of either 0.2% or 0.5% ropivacaine. Diaphragmatic excursion (DE) and diaphragm thickening fraction (TF) were measured using M-mode ultrasound before and 30 minutes after the block. Pulmonary function was assessed using a portable spirometer. Additional outcomes included pain scores and the occurrence of adverse effects.
Results: DE was significantly reduced 30 minutes after block in the 0.5% group compared to the 0.2% group (p< 0.01), as well as the TF (p< 0.01). Forced vital capacity (FVC) was also significantly reduced in the 0.5% group 30 minutes after block in the preparation room compared to the 0.2% group (p< 0.001). Both 0.2% and 0.5% ropivacaine had similar effects in improving postoperative pain. There were no serious block-related complications in either group.
Conclusion: 0.2% ropivacaine may impair pulmonary function less than 0.5% ropivacaine. The clinical significance of these differences requires further investigation.
Keywords: interscalene brachial plexus block, ropivacaine, diaphragmatic paralysis, diaphragmatic excursion, thickening diaphragm fraction
Introduction
Interscalene brachial plexus block (ISB) is a well-established anesthesia and analgesia technique widely used in upper limb surgeries. In recent years, the widespread use of ultrasound technology has enhanced ISB by allowing visualization of anatomical structures and dynamic monitoring of local anesthetic diffusion, shortening the anesthesia operation time, increasing the success rate of anesthesia, and reducing the incidence of complications.1,2 However, due to the close anatomical proximity, it is challenging to avoid blocking the phrenic nerve and causing diaphragmatic paralysis.3,4 Diaphragmatic dyskinesia can result in reduced ventilation, lower oxygen saturation (SpO2), and dyspnea,5–7 particularly in patients with pre-existing ventilatory dysfunction, such as obese patients.8 Previous studies have found that reducing the volume of local anesthetic can reduce the incidence of diaphragmatic paralysis.9–11 However, there is still a lack of research on the effects of local anesthesia at different concentrations on both analgesia and diaphragmatic paralysis.
Ultrasound is a non-invasive, cost-effective, and easily obtainable tool that can be used to evaluate diaphragmatic dysfunction (DD).12,13
In this study, we aimed to use the same volume but two different concentrations of ropivacaine for ultrasound-guided ISB. We then used the ultrasound to evaluate the diaphragmatic dysfunction following the nerve block. Additionally, we observed the analgesic effects and other characteristics of the brachial plexus block to provide more data for improving clinical safety.
Methods
Subjects
Our trial was prospectively registered in the Clinical Trial Registry of the People’s Republic of China (Registry No. NCT06640621). This study was approved by the Ethics Committee of Peking University Third Hospital. All participants were informed about the purpose of the trial, in accordance with the Declaration of Helsinki and written consent was obtained from all participants. According to previous studies,14,15 the incidence of complete phrenic nerve block after 0.5% ropivacaine 20 mL interscalene brachial plexus block was about 60%, and the incidence of complete phrenic nerve block after 0.2% ropivacaine 20 mL interscalene nerve block was about 20%. Set α = 0.05, β = 0.2, the calculation results were 20 cases in each group. From November 2022 to October 2023, forty patients scheduled for shoulder arthroscopic surgery under general anesthesia were included in the study. ISB was used for postoperative analgesia. The inclusion criteria were: American Society of Anesthesiologists Physical Status Classification I or II, age 18~65 years, and a body mass index (BMI) of 18~30 kg/m2. Exclusion criteria included allergy to local anesthetics, infection at the injection site, coagulation disorders, respiratory diseases, phrenic nerve injury, severe organ dysfunction, and refusal to provide consent.
Research Design
A computer-generated sequence of random numbers and a sealed-envelope technique were used to assign patients randomly to receive either 20 mL 0.2% ropivacaine (Group L) or 20 mL 0.5% ropivacaine (Group H). The patients, anesthesiologists, and outcome assessors were blinded to the patients’ group allocations.
Preparation Before Block
All patients underwent routine fasting and water restriction before surgery, with no preoperative medication administered. After establishing intravenous access, standard monitoring was initiated, including electrocardiogram, blood pressure, and pulse oxygen saturation.
Diaphragm Mobility Monitoring
Diaphragm excursion (DE) and thickening diaphragm fraction (TF) were measured both before and 30 minutes after the nerve block.16 To measure DE, patients were placed in a supine position, a convex transducer (3.5 ~ 5 MHz, Wisonic, China) was used to scan while the right diaphragm through the hepatic window and the left diaphragm through the splenic window, which located near the anterior-axillary line. The craniocaudal movement of the diaphragm was documented during deep inspiration using M-mode. Complete diaphragmatic paralysis was defined as a 75% ~ 100% reduction in DE, including the occurrence of paradoxical movement. Partial diaphragmatic paralysis was defined as a 25% ~ 75% reduction, while no diaphragmatic paralysis was indicated by a DE reduction of less than 25%.17 To measure TF, patients were placed in the same position with the head of the bed at 45°. The diaphragm zones of apposition were located along the mid-axillary line with a linear transducer (4 ~ 15 MHz, Wisonic, China).
All measurements were repeated twice in each patient and by the same blinded investigator to reduce intra-observer and inter-observer variability.
Additionally, a handheld spirometer (SP10BT; CONTAC) was used to measure pulmonary function tests, including forced vital capacity (FVC), with patients in an upright-seated position at baseline and 30 minutes after the nerve block, as well as 2-hours post-surgery. Spirometry was performed three times, with the best effort recorded.
Ultrasound-Guided ISB
All nerve blocks are performed by an experienced anesthesiologist in the preparation room before the surgery. After skin disinfection, 2% lidocaine was used for infiltration, followed by an in-plane ISB using a 22-gauge, 50-mm insulated short bevel needle (SonoPlex STIM, Pajunk Medical Systems, USA). The block needle was inserted in-plane from posterior to the probe, with the needle tip positioned between the anterior and middle scalene muscles. Local anesthetic was injected in divided doses after confirming negative aspiration for blood. An observer, blinded to the injection concentration, evaluated sensory and motor blocks every 5 minutes last for 30 minutes post-block.
Sensory assessment of cold sensation was conducted on the C4 (top of shoulder), C5 (lateral shoulder), C6 (thumb and index finger), C7 (middle finger), C8 (ring and little fingers), and T1 (medial forearm) dermatomes, with the opposite side as a control. Sensory testing was graded on a 3-point scale: 0 points for no block, 1 point for pain relief (touch sensation present, but cold absent), and 2 points for anesthesia (no sensation of touch or cold).
Motor block was evaluated in the C5 (shoulder abduction), C6 (elbow flexion), C7 (elbow extension), C8 (thumb opposition), and T1 (finger adduction) dermatomes with the opposite side as a control. The block was considered successful if the sensory score was 1 or higher; otherwise, it was classified as a failure. Motor blockade was evaluated by shoulder abduction and forearm flexion, using the modified Bromage scale as follows: 4-full power, 3-reduced power but able to lift the arm against resistance, 2-able to move the muscle group against gravity but unable to lift the arm against resistance, 1-perceptible muscle contraction, but unable to move on purpose, and 0-unable to move the relevant muscle group.
Perioperative Management
All patients received general anesthesia during the operation with sufentanil 0.3 µg/kg, propofol 1 ~ 1.5 mg/kg, and cisatracurium 0.2 mg/kg for induction and tracheal intubation. Anesthesia was maintained with remifentanil 0.01 ~ 0.03 µg/kg/min and sevoflurane 1.5 ~ 2% to maintain the blood pressure and heart rate within 20% of the patient’s basic value. The bispectral index value was maintained within 40 ~ 60. Flurbiprofen axetil 50mg and ondansetron 8mg were administered during skin incision closure.
Outcome Measurements
The primary outcome was the incidence of ipsilateral HDP. The secondary outcomes included pain scores at 2- and 24-hours post-surgery, assessed using the Numeric Rating Scale (NRS)-11 scale. Patients with an NRS-11 score greater than 4 received rescue analgesia of tramadol 100 mg. Patients’ total analgesia consumption in 24 hours was documented.
In addition, complications such as local anesthetic toxicity, Horner’s syndrome, hypoxemia, dyspnea, pneumothorax, and any adverse events like postoperative nausea and vomiting (PONV) and dyspnea were also recorded.
Statistical Analysis
SPSS (V.22.0; SPSS Inc., Chicago, ILL, USA) was used for statistical analysis. Continuous variables were analyzed using the Student’s t-test or the Mann–Whitney U-test based on the normality of data distribution. For normally distributed data, results are expressed as mean ± standard deviation ( ± s), and comparisons between groups were conducted using the independent samples t-test. For non-normally distributed data, results are represented as median (P25– P75), with comparisons between groups performed using the Wilcoxon rank-sum test. Categorical variables are represented as frequencies (percentages), and the Pearson χ2 test was used for comparison between groups. A p-value of <0.05 was considered statistically significant.
± s), and comparisons between groups were conducted using the independent samples t-test. For non-normally distributed data, results are represented as median (P25– P75), with comparisons between groups performed using the Wilcoxon rank-sum test. Categorical variables are represented as frequencies (percentages), and the Pearson χ2 test was used for comparison between groups. A p-value of <0.05 was considered statistically significant.
Results
Out of 45 patients assessed for eligibility, four patients did not meet the inclusion criteria, and one patient declined to participate. Forty patients participated in the study; the CONSORT flowchart is shown in Figure 1. The patients’ characteristics and surgical data are shown in Table 1. There was no significant difference in sex distribution between the groups according to Fisher’s exact test (p=0.626). All patients were between 18 and 65 years of age, with no significant difference between the groups (p=0.360). Additionally, BMI was comparable across both groups (p=0.189). Thus, the two groups were well-matched in terms of baseline characteristics, including sex distribution, age, and BMI. The results of sensory block and motor block in the two groups are shown in Table 2. NRS was used to assess the degree of postoperative pain at 2- and 24- hours after surgery, as shown in Table 3. Despite the different concentrations of ropivacaine used, there was no significant difference in NRS pain scores between the two groups at either time point. These findings suggested that both 0.2% and 0.5% ropivacaine provide similar effects in improving postoperative pain in patients.
 |
Table 1 Patient Characteristics |
 |
Table 2 Sensory and Motor Block Assessment After 30 min After Interscalene Block (n, %) |
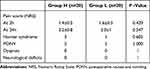 |
Table 3 Pain Scores and Adverse Effects |
 |
Figure 1 The CONSORT flowchart. |
The diaphragm DE refers to the displacement of the diaphragm during inhalation contraction, while the diaphragm TF is used to quantify its contractile ability. As shown in Table 4, in the 0.5% ropivacaine group, both DE and TF reduced significantly after the block (p<0.001), both during normal and deep respiration. In the 0.2% ropivacaine group, despite the lower concentration of ropivacaine, both DE and TF reduced significantly after the block (p<0.001), similar to those observed in the 0.5% group. Further comparison of the effects of different ropivacaine concentrations on diaphragmatic activity showed that both DE and TF under both normal and deep respiration was significantly reduced in the 0.5% group compared to the 0.2% group. Fisher’s exact test revealed a statistically significant difference in TF distribution between the two groups (p<0.001). These findings suggest that while both low and high concentrations of ropivacaine affect diaphragmatic activity, the impact is more pronounced with higher concentrations.
 |
Table 4 Diaphragmatic Paralysis and Pulmonary Function Test |
The diaphragm is the primary muscle responsible for respiratory activity. Therefore, we evaluated changes in pulmonary function while observing diaphragm activity. As shown in Table 4, the use of 0.5% ropivacaine significantly reduced pulmonary function than the 0.2% ropivacaine group at both 30 minutes post-block (p<0.001) and 2 hours postoperatively (p<0.001). In contrast, 0.2% ropivacaine did not affect pulmonary function, which means pulmonary function, particularly FVC, was better preserved in the low-concentration group compared to the high-concentration group.
Baseline DE was similar between the two groups (group L: 5.7 ±0.8 cm vs group H: 5.6±1.0 cm; p=0.771). In group L, one patient (5.0%) experienced complete HDP, while 19 patients (95.0%) had partial HDP. In group H, 14 patients (70.0%) experienced complete HDP, and six patients (30.0%) had partial HDP (Table 4). There were no significant differences in the pre-block FVC between the groups; however, reductions in FVC after the block were significant (Table 4).
Pre-operative TF was 55 ± 8% in Group L and 56±8% in Group H (p = 0.319). Post-operative TF was 9±4% in Group L compared to 27 ± 8% in Group H (p<0.01). The changes in TF before and after the block are shown in Figure 2. Consequently, post-block diaphragm function showed a more significant decrease in Group H compared to Group L.
 |
Figure 2 The changes in TF before and after the block. |
There were no significant differences in the adverse events. Additionally, no neurological deficits were identified during follow-up in either group (Table 3).
Discussion
This study demonstrates that reducing the concentration of 20 mL ropivacaine from 0.5% to 0.2% for ISB in arthroscopic shoulder surgery reduces the degree but not the incidence of HDP.
Ropivacaine is one of the most commonly used local anaesthetic drugs for ISB. The optimal volume and concentration of the anesthetic play a pivotal role in minimizing the adverse effects associated with peripheral nerve blocks. Michael J et al demonstrated that the concentration of ropivacaine for interscalene block primarily influences the extent of motor block.18 Our study yielded similar results, showing that both low- and high-concentration ropivacaine groups provided effective analgesia at 2- and 24- hours postoperatively. However, the incidence of complete diaphragmatic paralysis was significantly lower in the low-concentration group.
The phrenic nerve originates from the C3–C5 spinal nerves, courses along the surface of the anterior scalene muscle, and descends into the thorax to innervate the diaphragm. Previous studies have shown that the incidence of HDP after ISB with 20 mL of local anesthetic is as high as 92% to 100%.3,19,20 Our findings are consistent with these results, as the incidence of HDP was 100% in both the low- and high-concentration groups. However, the degree of paralysis varied: in the low-concentration group, most cases were partial, with only one case (1/20) of complete paralysis. In contrast, the high-concentration group had 14 cases (14/20) of complete paralysis. This may be due to the potential for sensory-motor separation with low-concentration ropivacaine, where the degree of motor blockade is reduced.21 Contrary to our findings, Zhai Wenwen et al reported no statistically significant difference in the probability of complete anesthesia between the high-concentration (0.5%) group and the low-concentration (0.25%) group after surgery.22 This discrepancy could be attributed to differences in the volume of local anesthetic administered, with 10 mL used in the high-concentration group and 20 mL in the low-concentration group.
Postoperative ipsilateral diaphragmatic paralysis remains a common occurrence following BPBA, while the incidence of PPC after surgery is rare and predominantly mild.10,23 Our research findings align with previous literature, confirming that while both patient groups exhibited varying degrees of diaphragmatic paralysis, none experienced complications such as respiratory distress or decreased oxygen saturation. This may be attributed to the compensatory enhancement of contralateral diaphragm function following paralysis of the affected side, leading to an overall increase in diaphragm functionality.16 However, in patients with compromised respiratory function, such as those affected by obstructive or restrictive ventilatory disorders, neuromuscular conditions, or morbid obesity, HDP may lead to significant adverse effects.8,24,25
Our study has important clinical implications, as optimizing the dosage of local anesthetics could significantly improve patient outcomes by decreasing the incidence of respiratory complications associated with complete diaphragm paralysis. This is especially relevant for individuals with pre-existing respiratory conditions.
The study has several limitations. First, patients with lung diseases or severe obesity were excluded from our research, highlighting the need for further investigation in these populations. Second, our findings are specific to arthroscopic shoulder surgery and may not be directly applicable to open shoulder surgery. Third, our evaluation was restricted to pain assessment within the initial 24 hours post-surgery, and we did not extend follow-up beyond this period. Finally, we were unable to assess the onset and duration of the brachial plexus blockade.
In conclusion, this study demonstrates that administering a lower concentration of ropivacaine (0.2%) during shoulder arthroscopy effectively manages postoperative pain while preserving diaphragm function, compared to using a higher concentration of ropivacaine (0.5%).
Data Sharing Statement
All the authors agreed to share the individual deidentified participant data and the data are available from the corresponding author Yang Zhou ([email protected]) upon reasonable request.
Funding
The authors acknowledge financial support from national key research and development program of China 2023YFC2410804 and the innovation and transformation fund of Peking University Third Hospital BYSYZHKC2023107.
Disclosure
The authors report no conflicts of interest in this work.
References
1. McNaught A, Shastri U, Carmichael N, et al. Ultrasound reduces the minimum effective local anaesthetic volume compared with peripheral nerve stimulation for interscalene block. Br J Anaesth. 2011;106(1):124–130. doi:10.1093/bja/aeq306
2. Neal JM. Ultrasound-guided regional anesthesia and patient safety: update of an evidence-based analysis. Reg Anesth Pain Med. 2016;41(2):195–204. doi:10.1097/AAP.0000000000000295
3. Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesthesia Analg. 1991;72(4):498–503. doi:10.1213/00000539-199104000-00014
4. Li XT, Tian T, Xue FS. Hemidiaphragmatic paresis associated with interscalene nerve block. Canad J Anaesthes J Canad d’Anesthesie. 2022;69(10):1311–1312. doi:10.1007/s12630-022-02289-y
5. Jules-Elysee K, Reid SC, Kahn RL, Edmonds CR, Urban MK. Prolonged diaphragm dysfunction after interscalene brachial plexus block and shoulder surgery: a prospective observational pilot study. Br J Anaesth. 2014;112(5):950–951. doi:10.1093/bja/aeu130
6. Bu J, Li N, Huang X, He S, Wen J, Wu X. Feasibility of fast-track surgery in elderly patients with gastric cancer. J Gastrointestinal Surg. 2015;19(8):1391–1398. doi:10.1007/s11605-015-2839-7
7. Fujimura N, Namba H, Tsunoda K, et al. Effect of hemidiaphragmatic paresis caused by interscalene brachial plexus block on breathing pattern, chest wall mechanics, and arterial blood gases. Anesthesia Analg. 1995;81(5):962–966. doi:10.1097/00000539-199511000-00012
8. Lang J, Cui X, Zhang J, Huang Y. Dyspnea induced by hemidiaphragmatic paralysis after ultrasound-guided supraclavicular brachial plexus block in a morbidly obese patient. Medicine. 2022;101(2):e28525. doi:10.1097/MD.0000000000028525
9. Riazi S, Carmichael N, Awad I, Holtby RM, McCartney CJ. Effect of local anaesthetic volume (20 vs 5 mL) on the efficacy and respiratory consequences of ultrasound-guided interscalene brachial plexus block. Br J Anaesth. 2008;101(4):549–556. doi:10.1093/bja/aen229
10. Lee JH, Cho SH, Kim SH, et al. Ropivacaine for ultrasound-guided interscalene block: 5 mL provides similar analgesia but less phrenic nerve paralysis than 10 mL. Canad J Anaesthes J Canad d’Anesthesie. 2011;58(11):1001–1006. doi:10.1007/s12630-011-9568-5
11. Kim H, Han JU, Lee W, et al. Effects of local anesthetic volume (Standard Versus Low) on incidence of hemidiaphragmatic paralysis and analgesic quality for ultrasound-guided superior trunk block after arthroscopic shoulder surgery. Anesthesia Analg. 2021;133(5):1303–1310. doi:10.1213/ANE.0000000000005654
12. Zambon M, Greco M, Bocchino S, Cabrini L, Beccaria PF, Zangrillo A. Assessment of diaphragmatic dysfunction in the critically ill patient with ultrasound: a systematic review. Intensive Care Med. 2017;43(1):29–38. doi:10.1007/s00134-016-4524-z
13. Laguado-Nieto MA, Roberto-Avilán SL, Naranjo-Junoy F, et al. Diaphragmatic dynamics and thickness parameters assessed by ultrasonography predict extubation success in critically ill patients. Clin Med Insights. 2023;17:11795484231165940. doi:10.1177/11795484231165940
14. Zhang H, Wu J, Miao Y, et al. Determination of the optimal volume of 0.5% ropivacaine in single-injection retroclavicular brachial plexus block for arthroscopic shoulder surgery: a Phase I/II trial. Anesthesiology. 2024;142(1):155–65.
15. Danelli G, Berti M, Casati A, et al. Ipsilateral shoulder pain after thoracotomy surgery: a prospective, randomized, double-blind, placebo-controlled evaluation of the efficacy of infiltrating the phrenic nerve with 0.2%wt/vol ropivacaine. European J Anaesthesiol. 2007;24(7):596–601. doi:10.1017/S0265021506002390
16. Rovira L, Kot P, Pozo S, Cano B, De Andrés J. Peri-operative hemi-diaphragmatic variations after brachial plexus block above the clavicle: a prospective observational study of the contralateral side. Ultrasound Med Biol. 2023;49(9):2113–2118. doi:10.1016/j.ultrasmedbio.2023.05.018
17. Cros Campoy J, Domingo Bosch O, Pomés J, Lee J, Fox B, Sala-Blanch X. Upper trunk block for shoulder analgesia with potential phrenic nerve sparing: a preliminary anatomical report. Reg Anesth Pain Med. 2019;44(9):872–874. doi:10.1136/rapm-2019-100404
18. Fredrickson MJ, Smith KR, Wong AC. Importance of volume and concentration for ropivacaine interscalene block in preventing recovery room pain and minimizing motor block after shoulder surgery. Anesthesiology. 2010;112(6):1374–1381. doi:10.1097/ALN.0b013e3181d6929d
19. Kim BG, Han JU, Song JH, Yang C, Lee BW, Baek JS. A comparison of ultrasound-guided interscalene and supraclavicular blocks for post-operative analgesia after shoulder surgery. Acta anaesthesiologica Scandinavica. 2017;61(4):427–435. doi:10.1111/aas.12864
20. Aliste J, Bravo D, Layera S, et al. Randomized comparison between interscalene and costoclavicular blocks for arthroscopic shoulder surgery. Reg Anesth Pain Med. 2019;44(4):472–477. doi:10.1136/rapm-2018-100055
21. Casati A, Santorsola R, Cerchierini E, Moizo E. Ropivacaine. Minerva anestesiologica. 2001;67(9 Suppl 1):15–19.
22. Zhai W, Wang X, Rong Y, Li M, Wang H. Effects of a fixed low-dose ropivacaine with different volume and concentrations on interscalene brachial plexus block: a randomized controlled trial. BMC Anesthesiol. 2016;16(1):80. doi:10.1186/s12871-016-0248-4
23. Rogerson D, Williams JP, Yates S, Rogers E. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: las Vegas - an observational study in 29 countries. European J Anaesthesiol. 2017;34(8):492–507. doi:10.1097/EJA.0000000000000646
24. Wang J, Hou X, Zhang X, et al. Comparison of pulmonary function during interscalene block vs. supraclavicular block: a single-center, double-blind, randomized trial. BMC Anesthesiol. 2023;23(1):12. doi:10.1186/s12871-022-01967-0
25. Desai M, Willson CM, Chitty L, Gang BW, Lydon K, Shah S. A case of hospitalization after pre-operative interscalene nerve block in an ambulatory surgery center. Cureus. 2024;16(5):e59717. doi:10.7759/cureus.59717
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

