Back to Journals » Risk Management and Healthcare Policy » Volume 17
The Impact of Medical Risk Perception on Patient Satisfaction: The Moderating Role of Shared Decision-Making
Authors Zhou K , Chen L , Li M
Received 13 August 2024
Accepted for publication 22 November 2024
Published 4 December 2024 Volume 2024:17 Pages 2981—2995
DOI https://doi.org/10.2147/RMHP.S482908
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Kyriakos Souliotis
Kairu Zhou,1,* Li Chen,2,* Min Li3
1School of Public Administration, South China University of Technology, Guangzhou, 510640, People’s Republic of China; 2Department of Clinical Research, Guangdong Second Provincial General Hospital, Guangzhou, 510317, People’s Republic of China; 3School of Business Administration, South China University of Technology, Guangzhou, 510641, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Min Li, School of Business Administration, South China University of Technology, Guangzhou, 510641, People’s Republic of China, Email [email protected]
Purpose: The perception of medical risks is ubiquitous, influencing patients’ healthcare experiences, yet the “black box” of this influencing process is seldom explored. This study explores the relationship between medical risk perception, trust, and patient satisfaction while taking shared decision-making as a moderator.
Methods: A stratified random sample of 450 inpatients from a tertiary public hospital in Guangzhou was selected for investigation, from June 2023 to September 2023. A moderated mediation model was tested using the PROCESS program, wherein medical risk perception was linked to patient satisfaction through trust, with shared decision-making acting as the moderating variable.
Results: Medical risk perception had a significant negative predictive effect on patient satisfaction (β = − 0.383, p < 0.001), and after introducing the mediating variable, the negative predictive effect of medical risk perception on patient satisfaction remained significant (β = − 0.237, p < 0.001). Trust partially mediated the relationship between medical risk perception and patient satisfaction, with the mediating effect accounting for 37.86% of the total effect. The interaction term between medical risk perception and shared decision-making (β = 0.211, p < 0.001) significantly predicted trust.
Conclusion: This study confirmed the mediating and moderating effects of trust and shared decision-making on the relationship between medical risk perception and patient satisfaction. The theoretical model constructed based on the theory of information asymmetry provides strategies and methods for healthcare managers to improve the quality of healthcare services and alleviate tensions in doctor-patient relationship.
Keywords: medical risk perception, doctor-patient relationship, shared decision-making, trust, patient satisfaction
Introduction
Medical risks are pervasive and encompass multiple dimensions, including the complexity of diseases, the limitations of treatment methods, complications during the treatment process, and issues related to diagnostic accuracy.1 Due to the differences in healthcare systems and patient treatment habits across countries, medical outcomes and risks exhibit variability.2,3 In this context, the Chinese healthcare system faces unique challenges. According to a survey conducted by the Chinese Hospital Association, an average of 27 incidents of violence against healthcare workers occur annually in each medical institution nationwide. A report analyzing 46 typical doctor-patient conflict cases that occurred in 2016 found that the number of individuals involved in these disputes exceeded 330.4 The scarcity of medical resources and the frequent occurrence of severe medical incidents under China’s distinctive healthcare framework exacerbate tensions in doctor-patient relationship.
The underlying cause of these tensions stems primarily from patient dissatisfaction with medical services, which is influenced by the medical risk perception.5 Medical risk perception refers to an individual’s subjective assessment of the potential risks and uncertainties associated with the medical process, encompassing various dimensions such as physical health risks, economic risks, and socio-psychological risks. Different individuals’ perceptions of risk lead to varying attitudes and behaviors, which in turn result in distinct risk outcomes.6 When patients perceive that medical risks may threaten their health, this perception is likely to trigger conflicts with healthcare providers, leading to feelings of anxiety and fear, ultimately affecting patient satisfaction and their overall healthcare experience.
The establishment of trust between patients and physicians is a process grounded in risk and self-awareness. The management of patients’ medical risk perception serves as the intrinsic basis for alleviating the fragility of trust in the doctor-patient relationship.7 Research has indicated that, in the face of medical risk, patients’ trust in healthcare providers is positively correlated with their satisfaction.8 The complexity and uncertainty inherent in the medical process often evoke subjective fear in patients,9 a fear that not only affects their trust in healthcare professionals but also further impacts their overall healthcare experience.
Within the framework of information asymmetry theory, conflicts between patients and physicians often stem from a lack of trust in doctors. To effectively alleviate patients’ anxiety in the specific context of the Chinese healthcare environment, the introduction of a shared decision-making mechanism has emerged as an important strategy. As a psychological regulation tool, shared decision-making integrates patients’ value preferences, influences emotional and behavioral choices through enhanced self-awareness, and employs strategies to achieve desired outcomes.10 During hospitalization, patients rely on their intrinsic psychological mechanisms to regulate emotions and promote health behaviors. In the process of shared decision-making, when individuals perceive medical risks, this decision-making model can enhance patients’ motivation for treatment, prompting them to evaluate how their behaviors impact risk events and subsequently adjust their self-perception, thereby encouraging adaptive behaviors to maintain their health.
Currently, there is relatively limited research exploring the relationship between medical risk perception and patient satisfaction. This study focuses on the dimension of physical health risk perception to clarify the mechanisms underlying this relationship. Based on information asymmetry theory, we have constructed a moderated mediation model to examine the mediating role of trust and the moderating role of shared decision-making in this relationship. Specifically, our research investigates the predictive mechanisms of medical risk perception in patient satisfaction, focusing on the mediating role of trust and the moderating role of shared decision-making. The aim is to unveil the “black box” of how patients’ medical risk perception influences their satisfaction, thereby providing valuable insights for improving the quality of healthcare services and fostering harmonious doctor-patient relationship.
Research Hypotheses
Medical risk perception refers to an individual’s subjective judgment regarding the likelihood of developing a disease, encompassing the cognitive assessment of risks associated with medical interventions, such as potential loss of life, physical disability, and physiological impairment.11 To some extent, medical risk perception serves as an external manifestation of patients’ pursuit of certainty regarding their health conditions. This perception can elicit psychological stress and anxiety among patients. Research indicates that during the Covid-19 pandemic, risk perception was negatively correlated with mental health outcomes.12 Given the complexities of medical knowledge and its inherent uncertainties, patients often struggle to effectively differentiate and interpret various medical information during hospitalization.9 This uncertainty in healthcare can provoke feelings of worry and unease among patients, leading them to question the quality of hospital services and the professional competence of physicians, ultimately impacting their healthcare experience.13 Studies have found that a woman’s low satisfaction with breastfeeding in the first month postpartum is associated with a higher risk of discontinuing exclusive breastfeeding six months prior.5 Patient satisfaction is defined as the comparison between patients’ expectations of service and their perceived service experience, reflecting an overall evaluation of the healthcare services provided by hospitals.14 It embodies the individual’s assessment of their physiological functioning, psychological state, and overall healthcare experience. When confronted with serious illnesses or surgical procedures, patients may be concerned about treatment efficacy, surgical risks, and potential complications. Such worries and anxieties can lead to dissatisfaction and resistance towards the healthcare process, thereby affecting patient satisfaction. Based on the above analysis, this study proposes the following hypotheses:
H1: Medical risk perception has a significant negative impact on patient satisfaction.
Trust is a conviction and reliance that patients have regarding the professional competence, ethical standards, service attitude, and the reliability and effectiveness of treatment plans provided by physicians during the process of receiving medical services. This trust is founded on patients’ confidence in the personal qualities, professional skills, and the credibility of the healthcare institution, making it one of the core elements in the doctor-patient relationship.15 The construction of trust is a self-conscious process based on risk. Diotaiuti et al16 suggested that medical risk perception is a precursor variable of trust. When patients face medical decisions, they weigh the perceived risks and potential benefits. If the perceived risks are high, patients may experience anxiety and unease, making it difficult to trust healthcare providers. Perceived risks can also influence patients’ willingness to seek medical care and their level of cooperation.17 When patients are concerned about medical risks, they may delay seeking treatment, refuse certain therapies or tests, and even harbor doubts and resistance towards medical advice, all of which can decrease trust in healthcare providers. Therefore, the vigilance of patients’ medical risk perception affects the fragility of the doctor-patient trust.15
When patients trust healthcare providers, they are more likely to actively cooperate with treatment plans. This trust reduces patients’ doubts and resistance, making them more willing to accept medical recommendations such as surgeries or medication. The level of trust patients have in their doctors directly impacts their acceptance of treatment and treatment outcomes. Patients with high levels of trust are more likely to follow medical advice, leading to improved treatment outcomes and increased patient satisfaction.18 Based on trust, doctors are also more likely to pay attention to patients’ needs, providing more detailed and attentive care, further enhancing patient satisfaction.19 When patients perceive a high level of risk during the process of receiving medical services, they may begin to question their trust in the healthcare institution and the physicians involved. This erosion of trust can lead to a decreased acceptance of medical advice and treatment plans, ultimately impacting treatment outcomes and patient satisfaction. Therefore, this study proposes the following hypothesis:
H2: Trust plays a significant mediating role between medical risk perception and patient satisfaction.
Shared decision-making is a collaborative process that emphasizes the joint evaluation of various options by physicians and patients based on in-depth communication. This process involves assessing the advantages and disadvantages of each option while fully considering the patient’s individual perspectives, preferences, and the uniqueness of their specific circumstances, ultimately leading to the co-creation of a decision-making plan.20 Shared decision-making is crucial to the realization of every patient’s right to health.21 Patient-centered care, which involves patients in clinical decision-making, can improve the quality of medical services for patients.22 Shared decision-making, as a new model of diagnosis and treatment, is also an important tool for promoting patient autonomy.23 When patients are more involved in shared decision-making, they are more willing to communicate with doctors and self-regulate in the face of medical uncertainties, enabling them to face hospital environments and their own conditions more calmly, thus weakening the negative impact of medical risk perception on trust. On the contrary, when patients are less involved in shared decision-making, they communicate less with doctors and become more anxious when confronted with the complexity of medicine and the uncertainty of medical outcomes, thereby enhancing the negative impact of medical risk perception on trust. Therefore, this study proposes the following hypothesis:
H3: Shared decision-making moderates the relationship between medical risk perception and trust.
In this study, a moderated mediation model was further proposed, wherein the impact of medical risk perception on patient satisfaction through trust is influenced by shared decision-making. Owing to the disparate signals conveyed by shared decision-making and medical risk perception, when the level of involvement in shared decision-making is high, under the premise of sufficient doctor-patient communication, the impact of medical risk perception on trust during the medical treatment process is mitigated, indirectly affecting patient satisfaction. Conversely, when the level of involvement in shared decision-making is low, under the premise of insufficient doctor-patient communication, the impact of medical risk perception on trust is intensified, thereby affecting patients’ satisfaction with medical outcomes. Based on this, the following hypothesis is proposed by this study:
H4: Shared decision-making moderates the indirect impact of medical risk perception on patient satisfaction through trust, acting as a regulatory factor in this mediation process.
Methods
Study Population
This study invited inpatients randomly from a tertiary hospital in Guangzhou, China, for the distribution of paper-based questionnaires. To ensure the accuracy and reliability of sample acquisition, the participants inclusion criteria were: (1) Participants were hospitalized for not less than 3 days, (2) The condition of the participants was stable, (3) Participants gave verbal informed consent and were willing to co-operate with the investigation. We explain the specific content and significance of this investigation with relevant departments of the hospital to get a consent before initiating. Prior to questionnaire distribution, a pilot study involving 10 inpatients was conducted to modify any unclear or inappropriate items. Investigators were present to address inquiries of patients on-site and collected completed questionnaires immediately. The survey received approval from the Ethics Committee Review Board of Guangdong Second Provincial General Hospital. During the study, verbal consent was obtained from participants, and written consent was signed by them on the front page of the questionnaire. In this study, informed consent for all participants under the age of 18 was obtained from their parents.
The present study selects a comprehensive hospital for investigation. To adhere to the principles of stratified random sampling, the sample is stratified according to the types of diseases, with sampling proportions determined based on the overall characteristics of the population. Specifically, cardiovascular diseases account for 30%, respiratory diseases for 25%, digestive system diseases for 20%, oncological diseases for 15%, and neurological diseases for 10%. The sampling proportions for each stratum are established according to the characteristics of the respective diseases, ensuring the comprehensiveness and representativeness of the research. Questionnaires were distributed and collected from June 2023 to September 2023. A total of 450 questionnaires were distributed, with 32 invalids and 418 valids, resulting in an effective rate of 92.89%. As shown in Table 1, in terms of age distribution, there are slightly more males (219) than females (199), with males accounting for 52.39% and females for 47.61%. The age distribution of the sample is primarily concentrated in the 50–65 age range, which constitutes 33.73% of the overall sample, followed by the 34–39 age group at 28.95%. Regarding educational attainment, the majority of participants hold a bachelor’s degree or attended a higher vocational college, representing 36.60% and 30.38% of the sample, respectively. In terms of monthly income distribution, those earning over 8000 yuan comprise only 14.36% of the total sample.
 |
Table 1 Patients’ Demographics (N=418) |
Measures
By referencing existing literatures and considering the practical circumstances of the questionnaire survey, four core variables have been identified for this study. Internationally and domestically recognized and authoritative scales were employed. Through a translation-back-translation process, the Chinese versions of the scales were ensured to accurately convey the original concepts. The scales selected for this study all utilize the widely accepted Likert 5-point rating method for measurement, where 1 corresponds to “strongly disagree” and 5 corresponds to “strongly agree.”
Medical Risk Perception
We drew inspiration from Michalovic et al24, who developed a Risk Perception Assessment Scale for behavior plans. This study explores the cognitive processing models of individual risk information and their impact on the formulation and implementation of exercise action plans. Building upon the work of Woringer et al25 and Liu et al,26 the items related to medical risk perception include concerns such as “concerns about the treatment plan not achieving the desired effects, leading to a deterioration in my health”, “Worries that complications from the treatment may impact its effectiveness and prognosis”, “Concerns regarding insufficient or excessive treatment by the physician”.
Shared Decision-Making
This study utilized a scale developed by Kriston et al27 to measure shared decision-making. The variable was assessed using a single-dimensional scale with nine items. Items include statements like “My doctor helped me understand all the information”, “My doctor asked me which treatment option I prefer”, “My doctor and I thoroughly weighed the different treatment options”, “My doctor and I selected a treatment option together”, “My doctor and I reached an agreement on how to proceed”, “My doctor made clear that a decision needs to be made”. The scale has been demonstrated good reliability and validity.
Trust
The Wake Forest Scales Measuring Trust, developed by Hall et al,28 was employed in this study to measure trust. Widely used to assess patients’ trust levels in familiar healthcare providers, the items include statements such as “To ensure my health, my doctor will do their best and be responsible”, “In general, I trust my doctor”, “The level of my doctor’s competence does not meet my expectations of what a physician should achieve”, “My doctor is thorough and considerate”, “I believe that the treatment plan chosen by my doctor is the most suitable for me”, “I feel that my doctor does not listen attentively to the issues I present”, “I can confidently entrust my safety to my doctor”.
Patient Satisfaction
Drawing on Lifshitz et al’s29 development of a patient satisfaction scale and incorporating adaptations from Zhou et al30 to suit the Chinese context, the satisfaction scale was further refined based on European satisfaction scales. The items include statements such as “Overall satisfaction with the hospital”, “Satisfaction with the comparison between my medical expenses and the medical services I received” and “Satisfaction compared to the hospital that you consider satisfactory”.
Control Variables
In line with existing research, this study considered patient factors such as gender, age, education level and monthly income as control variables.
Statistical Analysis
This study conducted data entry, descriptive statistics, and correlational analyses using the SPSS 26.0 software, and further determined the degree of correlation between variables based on the Pearson correlation coefficient and its significance. Subsequently, confirmatory factor analysis was conducted using Amos software. Furthermore, the mediation effects, moderation effects, and moderated mediation effects of the model were verified using PROCESS version 2.16, with p < 0.05 considered statistically significant.
Results
Reliability and Validity Test
To ensure the reliability and validity of the design, the study pre-tested the questionnaire based on random principles before forming the official questionnaire and conducted reliability and validity tests on the pilot test results. In the reliability testing phase, the study selected the widely used Cronbach’s α coefficient method. The test results showed that the Cronbach’s α coefficients for the scales of medical risk perception, trust, shared decision-making, and patient satisfaction are 0.947, 0.939, 0.947, and 0.859, respectively, demonstrating a good level of reliability.
In the validity testing phase, the study examined the validity of the scale from two aspects: content validity and discriminant validity. For content validity, the study relied on mature scales that have been used and tested repeatedly in existing research. On this basis, three professors from related disciplines were invited to further revise the scales, ensuring excellent content validity. For discriminant validity, the study conducted a confirmatory factor analysis on the variables. The analysis report shows (see Table 2) that the Average Variance Extracted (AVE) values for medical risk perception, trust, shared decision-making, and patient satisfaction are 0.668, 0.612, 0.667, and 0.686, respectively, all exceeding 0.50, indicating that the convergent validity meets the research requirements. The Composite Reliability (CR) values were 0.948, 0.940, 0.947, and 0.866, respectively, with all CR values greater than 0.7, indicating good internal consistency. Furthermore, the model fit test indices were: χ2=1115.534, df=428, RMSEA=0.062, CFI=0.934, TLI=0.929, showing that all model indices fall within the recommended ranges, presenting excellent fitting standards. Therefore, the scale data of the study possessed ideal reliability and validity, fulfilling the research needs.
 |
Table 2 Confirmatory Factor Analysis |
Correlation Analysis
The results for the mean values, standard deviations, and Pearson correlation coefficients of the study variables were presented in Table 3. There was a negative correlation between the medical risk perception and patient satisfaction. Additionally, the medical risk perception was negatively correlated with trust, while trust was positively correlated with patient satisfaction. These findings provided preliminary validation of the data.
 |
Table 3 Descriptive Statistics and Correlation Analysis |
Mediating Analysis
To explore the underlying mechanism through which medical risk perception negatively impacts patient satisfaction, trust was introduced as a mediating variable in the study. The mediating effect was examined using Model 4 in the PROCESS program, and the bootstrap method provided by Hayes31 was employed to verify the mediating role of trust between medical risk perception and patient satisfaction. The number of bootstrap samples was set at 5000, with control variables including gender, age, education level, and monthly income. As shown in Table 4, medical risk perception negatively predicted patient satisfaction (β = −0.383, p < 0.001), thus confirming hypothesis H1. Medical risk perception negatively predicted trust (β = −0.281, p < 0.001), and trust positively predicted patient satisfaction (β = 0.517, p < 0.001).
 |
Table 4 Mediating Effect of Trust |
According to Table 5, trust serves as a mediator between medical risk perception and patient satisfaction, with the upper and lower limits of the Bootstrap 95% confidence interval not including zero. This indicates that medical risk perception has a direct effect on patient satisfaction and also exerts an indirect effect through the variable of trust. The direct effect (−0.237) and the mediating effect (−0.145) account for 62.14% and 37.86% of the total effect, respectively. Therefore, hypothesis H2 is validated.
 |
Table 5 The Mediating Role of Trust in the Relationship Between Medical Risk Perception and Patient Satisfaction |
Moderation Analyses
In addition, this study employed Model 7 from the PROCESS program to test for moderation effects, with the Bootstrap resampling set at 5000 iterations. Controlling for gender, age, education level, and monthly income, two regression equations were established. As shown in Table 6, the coefficient of the interaction term between medical risk perception and shared decision-making was positive and significant (β=0.211, p < 0.001), indicating that shared decision-making positively moderates the relationship between medical risk perception and trust, thus demonstrating the presence of a moderating mediating effect. H3 was confirmed.
 |
Table 6 Test Results of Moderated Mediation Effect |
To further elucidate the moderating effect of shared decision-making, the participants were divided into high and low groups based on one standard deviation above and below the mean of shared decision-making, and a simple slope test was conducted. As shown in Figure 1, comparison of the slopes of the regression lines for the high and low groups indicated that the individual samples in the low shared decision-making group are greater than those in the high shared decision-making group, suggesting that at high levels of shared decision-making, the negative impact of medical risk perception on trust is attenuated.
 |
Figure 1 Shared decision making (SDM) as a moderator of the relationship between medical risk perception (MRP) and trust. |
As illustrated in Figure 2, medical risk perception negatively predicts trust (β = −0.281, p < 0.001), and the interaction term between medical risk perception and shared decision-making significantly positively predicts trust in healthcare professionals (β = 0.211, p < 0.001), indicating that shared decision-making moderates the relationship between medical risk perception and trust. Furthermore, the trustof patients in healthcare professionals positively predicted patient satisfaction (β = 0.517, p < 0.001), while medical risk perception negatively predicted patient satisfaction (β = −0.237, p < 0.001).
 |
Figure 2 Moderated mediation model. Notes: All path coefficients are β. ***p<0.001. |
Moderated Mediation Analyses
Overall, the impact process of medical risk perception on patient satisfaction through the mediation of trust was moderated by shared decision-making. As shown in Table 7, When the level of patient involvement in shared decision-making was high, the indirect effect of medical risk perception on patient satisfaction through trust was weaker (β = −0.057, 95% CI = [−0.092, −0.017]), while at low levels of patient involvement in shared decision-making, the indirect effect of medical risk perception on patient satisfaction through trust was stronger (β = −0.232, 95% CI = [−0.354, −0.123]). Therefore, H4 was confirmed.
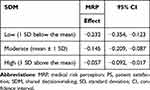 |
Table 7 Conditional Indirect Effects of Medical Risk Perception on Patient Satisfaction Through Trust at Values of Shared Decision-Making |
Discussion
Our study investigated the mediating role of trust and the moderating role of shared decision-making in the relationship between medical risk perception and patient satisfaction. The findings indicated that medical risk perception indirectly affects patient satisfaction through trust, and shared decision-making serves as a moderator, thus forming a moderated mediation model. The discoveries of this research offered new theoretical insights and support for the development of preventive and intervention measures aimed at enhancing the patient satisfaction.
Our study demonstrated that medical risk perception negatively impacts patient satisfaction, indicating that the higher the perceived medical risk patients experience during the medical treatment process, the lower the satisfaction they will achieve. This finding was consistent with the results of Rianthomy et al.32 Research from the perspective of occupational health has demonstrated that occupational health risks significantly negatively affect job satisfaction.33 Sacks et al34 found that older patients with more severe conditions tend to report lower satisfaction scores when receiving treatment in hospitals. Patients’ perceptions of medical risk during treatment can trigger anxiety and unease, leading them to doubt the skills of their physicians, ultimately resulting in decreased patient satisfaction. Arafa et al35 discovered a negative correlation between individual life satisfaction and the risk of atherosclerotic cardiovascular diseases. However, some studies suggest that individuals experiencing chronic stress may perceive their social environment as fraught with risks, which can motivate proactive responses to various threats.36 Slovic37 posited that risk is socially constructed and that individuals often rely on subjective cognition rather than medical authority and empirical knowledge to assess health risks. Additionally, this study found that male patients have a higher medical risk perception compared to female patients, which contradicts the findings of Koipuram et al.38 Considering risk perception as a source of stress, it can significantly influence individuals’ subjective experiences and overall physical and mental well-being.
Furthermore, we revealed that trust mediates the relationship between medical risk perception and patient satisfaction. On one hand, medical risk perception has a significant negative predictive effect on trust, indicating that the higher the perceived medical risk among inpatients, the lower their trust in healthcare professionals. This finding aligns with the results of Diotaiuti et al.16 Concurrently, Kim et al39 discovered a negative correlation between trust and risk perception, while also noting a positive correlation between trust and the willingness to engage in preventive behaviors. Stahl40 emphasized the importance of acting in the best interests of patients and fostering strong personal relationships between physicians and patients to gain trust and respect. Trust is dynamic, it encompasses expectations regarding the future development of the doctor-patient relationship.41 Trust is a form of risk delegation, and due to the initial lack of familiarity between patients and providers, it is often difficult for healthcare professionals to earn a high level of trust immediately. However, as the number of healthcare encounters increases, the relationship shifts from that of strangers to acquaintances, leading to an enhancement in trust levels. On the other hand, trust has a significant positive impact on patient satisfaction, which is consistent with the findings of Al-Hilou et al.42 The cognitive mechanisms of trust play a critical role in this process. The elaboration likelihood model proposed by Nordhielm43 further posits that emotional responses such as liking and satisfaction arise from cognitive processing. Based on the theory of information asymmetry, patients with limited medical knowledge will find their level of trust in physicians directly influences their willingness to adhere to medical advice and treatment plans. Patients with higher levels of trust are more likely to comply with medical recommendations, resulting in better treatment outcomes and higher satisfaction.44 Therefore, enhancing patient satisfaction can be achieved by addressing perceived medical risks, improving doctor-patient communication, alleviating patient anxiety, and fostering trust in healthcare providers.
More importantly, our study suggests that shared decision-making moderates the relationship between medical risk perception and trust. Shared decision-making is one of the key indicators of judging medical quality and is also considered the best approach to practicing patient-centered care.45 Specifically, when patients are more involved in shared decision-making, they have a better understanding of different treatment options, potential risks, and outcomes, which enables them to better comprehend the treatment plan, reducing misunderstandings and doubts, thereby weakening the negative impact of medical risk perception on trust.46 This study further suggests that enhancing the level of shared decision-making can lead to a more rational perception of medical risks, thereby improving trust between healthcare providers and patients, as well as increasing patient satisfaction. Shared decision-making is rooted in the theory of information asymmetry, emphasizing that individuals can enhance their medical understanding through active communication with physicians. This process not only effectively regulates patients’ motivations and influences their psychological and behavioral responses but also maximizes patients’ self-management capabilities, helping to maintain their health status at a relatively satisfactory level.47
Finally, the impact of medical risk perception on patient satisfaction through the mediating role of trust is moderated by shared decision-making. Shared decision-making is an effective way for patients and doctors to communicate in a timely manner, taking into account patients’ values and preferences.48 When patients are highly involved in shared decision-making, information is shared between doctors and patients, and patients have a clear understanding of their treatment options, resulting in a weaker indirect effect of medical risk perception on trust and patient satisfaction. Conversely, when patients have lower levels of involvement in shared decision-making, the indirect effect of medical risk perception on trust and patient satisfaction is stronger.
Based on the theory of asymmetric information, our study indicated the impact of medical risk perception on patient satisfaction and elucidates the mediating role of trust between medical risk perception and patient satisfaction. Objectively assessing patients’ levels of perceived medical risk perception can help healthcare professionals tailor clinical interventions and health guidance based on individual patient characteristics. In addition, our study examined the moderating effect of shared decision-making on medical risk perception and trust. Shared decision-making, by providing medical information for patients to participate in decision-making, aims to meet patients’ needs for medical information and involvement in decision-making. Ultimately, our study provides an effective model for improving patient satisfaction and offers a basis for healthcare decision-makers and managers to formulate strategies to reduce tension in doctor-patient relationship in Chinese hospitals.
Academic Contributions and Limitations
Our study made four academic contributions. Firstly, it deepened the understanding of the relationship between medical risk perception and patient satisfaction. The research revealed the negative impact of medical risk perception on patient satisfaction, further confirming that the risks perceived by patients during the medical service process directly affect their evaluation of service quality. This finding has important practical implications for healthcare service managers, suggesting that they should focus on reducing patients’ perceived medical risks to enhance patient satisfaction. Secondly, it clarified the mediating role of trust between medical risk perception and patient satisfaction, enriching the explanatory mechanism of the model that links medical risk perception to patient satisfaction and providing a new perspective for understanding patient satisfaction. Thirdly, the study innovatively explores the moderating role of shared decision-making between medical risk perception and trust, offering a new theoretical perspective on understanding doctor-patient relationship. Shared decision-making breaks the traditional pattern of asymmetric information and power imbalance between doctors and patients, establishing an equal cooperative relationship between them. This equal cooperation not only strengthens trust and understanding between doctors and patients but also helps reduce medical disputes, improve doctor-patient relationship, and provide a solid foundation for medical practice. Lastly, our study constructed a moderated mediation model, comprehensively examining the relationships between medical risk perception, trust, shared decision-making, and patient satisfaction, and empirically validates the model’s rationality. This model provided a strong theoretical framework for future research, aiding in further exploration of the factors influencing healthcare service quality and their mechanisms.
However, our research also had several limitations. Firstly, the study employed a questionnaire survey method, which is significantly influenced by the subjective perceptions of hospitalized patients and may be subject to measurement bias. Secondly, the research sample was drawn solely from Guangdong Province, which may constrain the generalizability of the results. Further research is necessary to ascertain whether our findings are applicable to other populations and to explore the underlying mechanisms.
Conclusion
Medical risk perception directly negatively influences patient satisfaction, with trust acting as a key mediating factor in this relationship. Shared decision-making plays a moderating role between medical risk perception and trust. The moderated mediation model reveals that the impact of medical risk perception on patient satisfaction through the mediating role of trust is contingent upon shared decision-making. The model constructed in this study provides profound theoretical insights into understanding patient satisfaction, helping them enhance patient satisfaction, build harmonious doctor-patient relationship, and improve healthcare outcomes through strengthening doctor-patient communication and encouraging shared decision-making.
Data Sharing Statement
All data generated or analysed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Ethical Approval and Informed Consent
All procedures performed in studies involving human participants were approved by the Ethics Committee Review Board of Guangdong Second Provincial General Hospital and complied with the 1964 Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study. All the data in study analyzed was anonymous.
Acknowledgments
We would like to thank the patients, doctors and administrative staff who took time and efforts to participate in this study.
Funding
This research project was supported by the Doctoral Workstation Project of Guangdong Second Provincial General Hospital (No. 2019BSGZ017).
Disclosure
The authors report no conflicts of interest in this study.
References
1. Liang H, Fung IC, Tse ZTH. et al. How did Ebola information spread on twitter: broadcasting or viral spreading? BMC Public Health. 2019;19(1):438. doi:10.1186/s12889-019-6747-8
2. Abdulle HM, Masika MM, Oyugi JO. COVID-19: knowledge, perception of risk, preparedness and vaccine acceptability among healthcare workers in Kenya. Pan Afr Med J. 2022;41:239. doi:10.11604/pamj.2022.41.239.33985
3. Sherif RD, Lisiecki J, Gilman RH. Perception of risk among aesthetic plastic surgeons. Aesthet Surg J. 2021;41(9):NP1218–NP1224. doi:10.1093/asj/sjab132
4. Sohu Public Platform. [homepage on the Internet]. 2016 Medical Data Annual Review: top Ten Incidents of Violence Against Healthcare Professionals; 2016. Available from: http://mt.sohu.com/20161212/n475590786.shtml.
5. Bizon A, Giugliani C, Giugliani ERJ. Women’s satisfaction with breastfeeding and risk of exclusive breastfeeding interruption. Nutrients. 2023;15(24):5062. doi:10.3390/nu15245062
6. Pennings JM, Grossman DB. Responding to crises and disasters: the role of risk attitudes and risk perceptions. Disasters. 2008;32(3):434–448. doi:10.1111/j.1467-7717.2008.01048.x
7. Wang Z, Wang Y, Hu P. Vulnerability of trust between doctors and patients: theoretical framework and antifragile development system. J Gansu Admin Inst. 2019;6:105–113. Chinese.
8. Wei D, Xu A, Wu X. The mediating effect of trust on the relationship between doctor-patient communication and patients’ risk perception during treatment. Psych J. 2020;9(3):383–391. doi:10.1002/pchj.327
9. Mei Y, Tan L, Yang W, et al. Risk perception and gratitude mediate the negative relationship between COVID-19 management satisfaction and public anxiety. Sci Rep. 2023;13(1):3335. doi:10.1038/s41598-023-29815-2
10. Hargraves IG, Fournier AK, Montori VM, Bierman AS. Generalized shared decision making approaches and patient problems Adapting AHRQ’s SHARE approach for purposeful SDM. Pat Educ Couns. 2020;103(10):2192–2199. doi:10.1016/j.pec.2020.06.022
11. Aycock DM, Clark PC, Araya S. Measurement and outcomes of the perceived risk of stroke: a review. West J Nurs Res. 2019;41(1):134–154. doi:10.1177/0193945917747856
12. Krok D, Zarzycka B. Risk Perception of COVID-19, meaning-based resources and psychological well-being amongst healthcare personnel: the mediating role of coping. J Clin Med. 2020;9(10):3225. doi:10.3390/jcm9103225
13. Rahman MK, Bhuiyan MA, Zailani S. Healthcare services: patient satisfaction and loyalty lessons from Islamic friendly hospitals. Patient Prefer Adherence. 2021;15:2633–2646. doi:10.2147/PPA.S333595
14. Zarei E, Daneshkohan A, Pouragha B, Marzban S, Arab M. An empirical study of the impact of service quality on patient satisfaction in private hospitals, Iran. Glob J Health Sci. 2014;7(1):1–9. doi:10.5539/gjhs.v7n1p1
15. Hawley K. Trust and distrust between patient and doctor. J Eval Clin Pract. 2015;21(5):798–801. doi:10.1111/jep.12374
16. Diotaiuti P, Valente G, Mancone S, et al. Perception of risk, self-efficacy and social trust during the diffusion of Covid-19 in Italy. Int J Environ Res Public Health. 2021;18(7):3427. doi:10.3390/ijerph18073427
17. Rains SA, Hingle MD, Surdeanu M, Bell D, Kobourov S. A test of the risk perception attitude framework as a message tailoring strategy to promote diabetes screening. Health Commun. 2019;34(6):672–679. doi:10.1080/10410236.2018.1431024
18. Andreano PR, Pardede RJISS. Service quality and patient trust on patient loyalty mediated by patient satisfaction on inpatients. Interdisciplinary Soc Stud. 2023;2(12):2684–2692. doi:10.55324/iss.v2i12.595
19. Tang L. The influences of patient’s trust in medical service and attitude towards health policy on patient’s overall satisfaction with medical service and sub satisfaction in China. BMC Public Health. 2011;11(1):472. doi:10.1186/1471-2458-11-472
20. Faiman B, Tariman JD. Shared decision making: improving patient outcomes by understanding the benefits of and barriers to effective communication. Clin J Oncol Nurs. 2019;23(5):540–542. doi:10.1188/19.CJON.540-542
21. Fiorillo A, Barlati S, Bellomo A, et al. The role of shared decision-making in improving adherence to pharmacological treatments in patients with schizophrenia: a clinical review. Ann Gen Psychiatry. 2020;19(1):43. doi:10.1186/s12991-020-00293-4
22. Berger ZD, Brito JP, Ospina NS, et al. Patient centred diagnosis: sharing diagnostic decisions with patients in clinical practice. BMJ. 2017;359:j4218. doi:10.1136/bmj.j4218
23. Klenzak S, Danelisen I, Brannan GD, Holland MA, van Tilburg MA. Management of gastroesophageal reflux disease: patient and physician communication challenges and shared decision making. World J Clin Cases. 2018;6(15):892–900. doi:10.12998/wjcc.v6.i15.892
24. Michalovic E, Hall S, Duncan LR, Bassett-Gunter R, Sweet SN. Understanding the effects of message framing on physical activity action planning: the role of risk perception and elaboration. Int J Behav Med. 2018;25(6):626–636. doi:10.1007/s12529-018-9746-8
25. Woringer M, Nielsen JJ, Zibarras L, et al. Development of a questionnaire to evaluate patients’ awareness of cardiovascular disease risk in England’s national health service health check preventive cardiovascular programme. BMJ Open. 2017;7(9):e014413. doi:10.1136/bmjopen-2016-014413
26. Liu Y, Wang R, Huang R, Cao Y, Wang J, Feng D. Influencing factors and their relationships of risk perception and decision-making behaviour of polypharmacy in patients with chronic diseases: a qualitative descriptive study. BMJ Open. 2021;11(4):e043557. doi:10.1136/bmjopen-2020-043557
27. Kriston L, Scholl I, Hölzel L, Simon D, Loh A, Härter M. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns. 2010;80(1):94–99. doi:10.1016/j.pec.2009.09.034
28. Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59(3):293–318. doi:10.1177/1077558702059003004
29. Lifshitz R, Nimrod G, Bachner YG. Measuring risk perception in later life: the perceived risk scale. J Am Psychiatr Nurses Assoc. 2016;22(6):469–474. doi:10.1177/1078390316659910
30. Zhou K, Li M. Study on the Influence of Guanxi hospitalization on patients’ healthcare-seeking behavior. Med Phil. 2023;44(4):45–50. Chinese.
31. Hayes AF. An index and test of linear moderated mediation. Multivariate Behav Res. 2015;50(1):1–22. doi:10.1080/00273171.2014.962683
32. Rianthomy AR, Prayoga TZ, Rahmiati F, Goenadhi F. Influence of risk perception and destination image mediated by satisfaction towards destination loyalty in tanjung lesung tourism. Intl J Appl Business Int Mgmt. 2023;8(2):279–293. doi:10.32535/ijabim.v8i2.2130
33. Shan B, Liu X, Gu A, Zhao R. The effect of occupational health risk perception on job satisfaction. Int J Environ Res Public Health. 2022;19(4):2111. doi:10.3390/ijerph19042111
34. Sacks GD, Lawson EH, Dawes AJ, et al. Relationship between hospital performance on a patient satisfaction survey and surgical quality. JAMA Surg. 2015;150(9):858–864. doi:10.1001/jamasurg.2015.1108
35. Arafa A, Kashima R, Kokubo Y. Life satisfaction and the risk of atherosclerotic cardiovascular disease in the general Japanese population: the Suita Study. Environ Health Prev Med. 2023;28:62. doi:10.1265/ehpm.23-00125
36. Samamdipour E, Seyedin H, Ravaghi H. Roles, responsibilities, and strategies for enhancing disaster risk perception: a quantitative study. J Educ Health Promot. 2019;8(1):9. doi:10.4103/jehp.jehp_185_18
37. Slovic P. Perception of risk. Science. 1987;236(4799):280–285. doi:10.1126/science.3563507
38. Koipuram A, Carroll S, Punthakee Z, Sherifali D. Diabetes knowledge, risk perception, and quality of life among South Asian caregivers in young adulthood. BMJ Open Diabetes Res Care. 2020;8(2):e001268. doi:10.1136/bmjdrc-2020-001268
39. Chan Won Kim HRS. Structural relationships among public’s risk characteristics, trust, risk perception and preventive behavioral intention - the case of MERS in Korea. Crisisonomy. 2017;13(6):85–95. doi:10.14251/crisisonomy.2017.13.6.85
40. Stahl B. Foundations of a trusting doctor-patient relationship. Quintessence Int. 2003;34(2):85–86.
41. Wu Q, Jin Z, Wang P. The relationship between the physician-patient relationship physician empathy, and patient trust. J Gen Intern Med. 2022;37(6):1388–1393. doi:10.1007/s11606-021-07008-9
42. Al-Hilou M, Suifan T. The mediating effect of patient trust on the relationship between service quality and patient satisfaction. Int J Health Care Qual Assur Epub, 2023 36 1/2 1–16 doi: 10.1108/IJHCQA-05-2023-0028.
43. Nordhielm CL. The influence of level of processing on advertising repetition effects. J Consum Res. 2002;29(3):371–382. doi:10.1086/344428
44. Zhou C, Chen J, Tan F, et al. Relationship between self-care compliance, trust, and satisfaction among hypertensive patients in China. Front Public Health. 2022;10:1085047. doi:10.3389/fpubh.2022.1085047
45. Dennison Himmelfarb CR, Beckie TM, Allen LA, et al. Shared decision-making and cardiovascular health: a scientific statement from the American heart association. Circulation. 2023;148(11):912–931. doi:10.1161/CIR.0000000000001162
46. Ali MA, Raza SA, Khamis B, Puah C-H, Amin H. How perceived risk, benefit and trust determine user Fintech adoption: a new dimension for Islamic finance. Foresight. 2021;23(4):403–420. doi:10.1108/FS-09-2020-0095
47. Morrison T, Foster E, Dougherty J, Barton J. Shared decision making in rheumatology: a scoping review. Semin Arthritis Rheum. 2022;56:152041. doi:10.1016/j.semarthrit.2022.152041
48. Forner D, Noel CW, Boland L, Pieterse AH, Borkhoff CM, Hong P. The multifocal approach to sharing in shared decision making: a critical appraisal of the MAPPIN’SDM. Med Decis Making. 2022;42(1):114–124. doi:10.1177/0272989X211010738
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Patient Preferences Influencing Treatment Decision-Making in Early-Stage Breast Cancer in Germany, Italy, and Japan

Flood E, McCutcheon S, Beusterien K, Mackie DS, Mokiou S, Guillaume X, Mulvihill E
Patient Preference and Adherence 2024, 18:1517-1530
Published Date: 25 July 2024

