Back to Journals » Journal of Multidisciplinary Healthcare » Volume 17
The Impact of Perceived Community Services for the Elderly on Self-Rated Health: An Analysis Utilizing a Mediated Latent Growth Model
Authors Jiang M , Yao Y, Xia X , Kong Y, Zhang N
Received 1 May 2024
Accepted for publication 29 August 2024
Published 7 September 2024 Volume 2024:17 Pages 4383—4396
DOI https://doi.org/10.2147/JMDH.S476502
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 7
Editor who approved publication: Dr Scott Fraser
Maomin Jiang,1,* Yisong Yao,2,* Xiaoqian Xia,3,* Yang Kong,4 Nan Zhang5
1School of Public Affairs, Xiamen University, Xiamen, Fujiang, People’s Republic of China; 2School of The Fourth Clinical Medical College, Qingdao University, Yantai, Shangdong, People’s Republic of China; 3Department of Public Health, Environments & Society, London School of Hygiene & Tropical Medicine, London, UK; 4School of Health Management, Binzhou Medical University, Yantai, Shangdong, People’s Republic of China; 5Physical Education Department, Shandong Technology and Business University, Yantai, Shangdong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Nan Zhang, Email [email protected]
Background: This study aims to investigate the relationship between older adults’ perceived community services for the elderly (PCSE), life satisfaction (LS), and self-rated health (SRH).
Methods: Data from four rounds of the Chinese Longitudinal Healthy Longevity Survey (CLHLS) from 2008 to 2018 were used. A total of 2454 older adults were obtained. Unconditional Least Squares (ULS) was used to measure PCSE, LS, and SRH growth trajectories without covariates. Finally, a mediating latent growth model was constructed using Mplus 8.3 to examine the mediating role of LS in the relationship between PCSE and SRH after adjusting for some demographic characteristics.
Results: The results from the ULS method indicate that the intercepts and slopes for PCSE and LS are significantly negatively correlated (β1 = − 0.629, β2 = − 0.579, p < 0.001). Additionally, there is a significant positive correlation between the intercept and slope of health levels (β = 0.774, p < 0.001). Using a parallel growth model, significant regression coefficients were found between the intercept of PCSE and the intercepts of SRH and LS (β1 = − 0.335, β2 = 0.378, p < 0.01). Similarly, the regression coefficients between the slope of PCSE and the slopes of SRH and LS were also significant (β1 = − 0.532, β2 = 0.344, p < 0.01). Furthermore, the regression coefficient between the intercept of LS and the intercept of SRH was significant (β = 0.415, p < 0.001). The regression coefficient between the slope of LS and the slope of SRH was also found to be significant (β = 0.729, p < 0.001).
Conclusion: It is essential to ensure adequate supply and accessibility of community services for older adults. LS especially is, and should be a promising target for assessing the quality of life and utilization of PCSE supply.
Keywords: perceived community services for elderly, life satisfaction, Self-rated health, Latent growth model, older adults
Introduction
Population aging has emerged as an irreversible and critical demographic trend globally in the short term. According to the research report by the World Health Organization in 2019, the global population of individuals aged over 60 reached a staggering 1 billion, with projections suggesting this number will exceed 1.4 billion by the end of 2030.1 Moreover, the seventh national census of China in 2020 revealed that the population aged 60 and above surpassed 260 million, accounting for 18.7% of the total population.2 Projections indicate that by 2050, the population of older adults in China will exceed 450 million.3 The escalating degree of population aging presents significant challenges to the aspiration of healthy aging. Studies have indicated that a staggering 78% of older adults in China suffer from at least one chronic non-communicable disease, highlighting the prevalence of sub-healthy and unhealthy status among them.4 Such chronic health issues not only inflict physical pain but also engender negative emotions and psychological distress.5,6 Hence, it becomes imperative to explore potential influencing factors and pathways to the health of older adults.
In the backdrop of deepening societal aging, the significance of community services for the elderly (CSE) in promoting healthy aging is garnering increasing scholarly attention. The evolving structure of the family and the impact of social trends are contributing to a decline in the role of the family in providing for older adults. Community services provided are increasingly recognized as indispensable pillars supporting their access to essential social provisions. In China, CSE encompasses services tailored to the unique needs of older individuals, including life care (eg, meal delivery, housekeeping), medical assistance (eg, in-home medical care services, therapy care services), mental health promotion, and social support services (eg, entertainment, emergency call services).7 Numerous studies have underscored the relationship between robust CSE and the physical and mental well-being.8 Robust CSE for older adults facilitates management of health issues and preserve their independence, thereby enhancing health outcomes and mitigating the risk of accidents, injuries, and health complications. Karlsson (2013) observed that inadequate CSE levels correlate with heightened vulnerability to dependency on assistive tools, visual impairment, and incontinence.9 In contrast, drawing from social support theory, ample CSE provision amplifies the social support networks and engagement opportunities, addressing their emotional needs, improving their mental well-being and influencing their overall health.10–12 It is noteworthy that certain scholars also have highlighted the potential adverse effects of aberrant social support and interaction within communities on the overall social participation levels of older adults. For instance, disparities in CSE quality may engender feelings of inequality among them, precipitating negative emotions such as frustration.13
Perceived community services for the elderly (PCSE) encompasses older adults’ perceptions of the sensibility and availability of CSE supply, playing a crucial role in enhancing the efficiency of CSE provision. Previous research has indicated a negative correlation between the perceived level of PCSE and the health status of older adults.14 Every individual behavior or tendency stems from an internal driving force.15 According to Maslow’s hierarchy of needs theory, when an individual’s physiological needs are unmet, there is a natural inclination to seek stimulation to restore balance.16 Therefore, as the health of older adults declines, they tend to allocate more time and effort to perceive the availability of healthcare institutions in their vicinity, which often correlates with higher levels of PCSE supply. Ones with better health status typically rely less on medical and healthcare services and elderly care facilities. For instance, studies have shown that the physical health of older adults significantly influences their perception of life care and medical services within CSE.17–19 Similarly, individuals with poor mental health are more likely to exhibit self-awareness and mental health issues, resulting in heightened perceptions of life care services.20 However, the specific pathways through which PCSE affects the health outcomes of older adults warrant further exploration.
Life satisfaction (LS) stands as a crucial indicator for assessing the quality of life among older adults and serves as a fundamental manifestation of the effective utilization of CSE supply.21,22 According to the social production function theory, robust PCSE provision serving as a significant component of social welfare can enhance the LS of older adults.23 The provision of PCSE has been shown to substantially elevate the LS of older individuals whose care needs are unmet by familial support, while also alleviating anxieties regarding future care needs among those still capable of self-care, thereby bolstering their LS.24 Moreover, ample evidence suggests that LS plays a pivotal role in promoting both the physical and mental health of older adults.25 In fact, when considering pathways through which LS might influence health outcome, there are at least three to consider: enhancing psychological and social resources; indirect effects through health behaviors and direct effects through biological ways.26 However, while the majority of studies support the notion that LS enhances mental well-being, a few have suggested otherwise.27 Therefore, further investigation is warranted to ascertain whether PCSE can influence the SRH of older adults by impacting LS.
Drawing upon the imperative of fostering healthy aging and recognizing the nuanced interplay between PCSE, LS, and self-rated health (SRH), we initiated a study to elucidate their relationship for the first time. The principal objective of our investigation is to conduct a developmental trend analysis of PCSE, LS, and SRH among older adults spanning from 2008 to 2018, while simultaneously examining the mediating role of LS in the pathway through which PCSE influences the health status of the elderly population in China. By doing so, our study aims to shed light on effective strategies for enhancing the overall well-being of older adults residing in communities and to provide insights for the judicious allocation of resources to meet the healthcare needs of this demographic.
Materials and Methods
Participants
The data utilized in this study were sourced from the Chinese Longitudinal Healthy Longevity Survey (CLHLS) database, a collaborative effort between the Healthy Aging and Development Research Center of Peking University and the National Development Research Institute. This project applied a multistage, stratified cluster sampling design, remaining methods used in this project can be consulted in previous studies.28 Spanning 23 provincial-level administrative regions in China, the survey project commenced its initial round in 1998 and has since conducted eight follow-up rounds, with data available up to 2018. The dataset utilized in this study comprises responses from the fifth (2008), sixth (2011), seventh (2014), and eighth (2018) rounds of the survey, focusing on surviving individuals aged 65 and above. Following a meticulous process of matching samples based on unique identifiers, we eliminated aberrant data points and instances with substantial missing information, resulting in a final sample size of 2454 participants. The data matching and inclusion process is shown in Figure 1.
 |
Figure 1 Sample inclusion process. |
Measures
Self-Rated Health (SRH)
The health level of older adults is measured by their Self-rated Health (SRH). SRH is measured by asking older adults, “How do you feel about your health”, the answers are divided into five levels (very bad = 1, bad = 2, fair = 3, good = 4, very good = 5). The total score of SRH ranges from 1 to 5, with higher scores indicating higher SRH. In the years 2008, 2011, 2014, and 2018, the overall Cronbach’s alpha was 0.785.
Life Satisfaction (LS)
Life Satisfaction (LS) is measured by asking older adults, “How do you think your life is now”, and the answers are divided into five levels (very bad = 1, bad = 2, fair = 3, good = 4, very good =5). The total score of LS ranges from 1 to 5, and the higher the score, the more satisfied older adults are with their lives. In the years 2008, 2011, 2014, and 2018, the overall Cronbach’s alpha was 0.819.
Perceived Community Services for Elderly (PCSE)
The measurement of PCSE includes eight items, including “daily care”, “seeing a doctor, delivering medicine”, “spiritual comfort, chatting to relieve boredom”, “daily shopping”, “organizing social and recreational activities”, “providing legal aid”, “Provide health knowledge”, “handle family and neighborhood disputes”, each item provides two options (“no = 0, yes = 1”). The total score of PCSE ranges from 0 to 8 points, and the higher the score, the more PCSE older adults have. In this study, the Cronbach alpha coefficients of the PCSE scale in 2008, 2011, 2014, and 2018 were 0.889, 0.888, 0.895, and 0.929, respectively, and the convergent validity was 0.502, 0.500, 0.524, and 0.628, indicating that the PCSE scale has a good Reliability and validity (Table 1).
 |
Table 1 Reliability and Validity of the PCSE Scale in 2008, 2011, 2014, 2018 |
Data Analysis
First, the statistical analysis using SPSS 27 includes: describing the demographic information with frequency and proportion; describing the variables of PCSE, LS, and SRH in the four years of 2008, 2011, 2014, and 2018 with the mean and standard deviation and use Pearson correlation analysis to assess the relationship between them pairwise. Then, use Mplus8.3 to build an intermediary latent growth model (LGM), use Unconditional Least Squares to measure the growth trajectory of PCSE, LS, and SRH without covariates,29 and examine the 2008–2018 The mediating role of LS in the relationship between PCSE and SRH of the subjects. Goodness-of-fit χ2, CFI, TLI, and RMSEA were used to examine the fit of this LGM with 95% CI, the p-value of close fit (Pclose), and SRMR. RMSEA<0.08, SRMR<0.08, CFI>0.90, and TLI>0.90 represent acceptable model-fitting results.30
Results
Descriptive Statistics
Table 2 shows the primary demographic information of the respondents in 2008. The results show that the 65–75-year-old group accounts for 58.11% of the total population; the rural population accounts for the majority, 1655 people (67.44%); the proportion of men and women are relatively equal; In terms of education years, the majority (46.74%) of older adults had no education, and only 119 (4.86%) had more than ten years of education.
 |
Table 2 Demographic Information of the Research Sample |
Correlation Analysis
Table 3 lists the average, standard deviation, and correlation between the PCSE, LS, and RSH variables in 2008, 2011, 2014, and 2018. All have weak correlations between PCSE (r: 0.07–0.26), LS (r: 0.15–0.29), and SRH (r: 0.19–0.31) in the four years. From 2008 to 2018, the PCSE level of the study population increased from 0.55±1.27 to 1.75±2.11, the LS level decreased from 3.93±0.807 to 3.63±0.79, and the SRH level decreased from 3.57±0.92 to 3.43±0.93.
 |
Table 3 Results of the Pearson Correlation Analysis |
The Impact Path of PCSE Supply on the SRH Development Trajectory of Older Adults
The results of the LGM indicated a good fit for the model. The fitting index of PCSE in 2008: χ2/df =3.836, CFI=0.968, TLI=0.915, RMSEA =0.073, SRMR =0.061; the fitting index of PCSE supply in 2011: χ2/df =2.881, CFI=0.953, TLI=0.904, RMSEA =0.071, SRMR =0.059; the fitting index of PCSE supply in 2014: χ2/df =2.201, CFI=0.980, TLI=0.946, RMSEA =0.059, SRMR =0.048; the fitting index of PCSE supply in 2018: χ2/df =2.730, CFI=0.979, TLI=0.960, RMSEA =0.065, SRMR =0.042. The fitting index of overall PCSE from 2008 to 2018: χ2/df = 5.103, CFI=0.942, TLI=0.937, RMSEA=0.042, SRMR=0.047); the fitting index of overall life satisfaction from 2008 to 2018: χ2/df =3.711, CFI=0.903, TLI=0.905, RMSEA=0.069, SRMR= 0.061; 2008~2018 overall SRH fitting index: χ2/df =1.336, CFI=0.988, TLI=0.986, RMSEA =0.051, SRMR =0.047. 2008~2018 overall model fitting index: χ2/df =4.476, CFI=0.915, TLI=0.907, RMSEA=0.036, SRMR=0.039 (Table 4).
 |
Table 4 Model Fit Index |
Table 5 shows the parameter estimates of PCSE, LS, and SRH in LGM. Strong evidence for a difference in PCSE levels (1.331±0.085) among older adults in 2008 (Ψ1=0.412, p <0.001) and a difference in growth rate (0.652±0.012) over the following ten years (Ψ2=0.310, p <0.001). Strong evidence for a difference in LS levels (3.780±0.011) among older adults in 2008 (Ψ1=0.189, p <0.001) and a difference in growth rate (−0.549±0.013) in the following ten years (Ψ2=0.025, p <0.001) There is strong evidence that there is a difference in the SRH level (3.468±0.012) in older adults in 2008 (Ψ1=0.198, p <0.001) and the growth rate (−0.365±0.008) in the subsequent ten years (Ψ2=0.017, p < 0.01).
 |
Table 5 Parameter Estimation for LGMs in PCSE, LS and SRH |
Figure 2 shows the path of the impact of PCSE on the trajectory of SRH in older adults. First, the intercept and slope of PCSE were negatively correlated (β= −0.629, p <0.001), indicating that the higher the PCSE level of older adults at baseline, the less their subsequent increase; the intercept and slope of LS were negative Correlation (β= −0.579, p <0.001), indicating that older adults with higher LS levels at baseline had a slower decline in LS. The intercept of SRH was positively correlated with the slope (β= 0.774, p < 0.001), indicating that older adults with higher SRH levels at baseline experienced faster SRH decline. Second, the intercept of PCSE was negatively correlated with the intercept of SRH (β= −0.335, p <0.001), indicating that the higher the PCSE level of older adults at baseline, the lower their SRH level. The slope of PCSE supply was negatively correlated with the slope of SRH (β= −0.532, p <0.01), indicating that the faster the growth rate of PCSE supply in older adults, the faster their SRH decreased. At the same time, the PCSE supply intercept was positively correlated with the LS intercept (β= 0.378, p <0.01), indicating that the higher the PCSE level of older adults at baseline, the higher their LS level. The PCSE supply slope was positively correlated with the LS slope of older adults (β= 0.344, p <0.01), indicating that the faster the PCSE growth rate of older adults, the slower the LS level decreased. The LS intercept was positively correlated with the SRH intercept of older adults (β= 0.415, p <0.001), indicating that the higher the LS level of older adults at baseline, the higher the SRH level. The regression coefficient of the LS slope on the SRH slope of older adults was significant (β= 0.729, p <0.001), indicating that the faster the LS decreased in older adults, the faster the SRH decreased.
 |
Figure 2 Final LGM mediation model. *p <0.05, ** p <0.01, *** p <0.001. |
Mediation Analysis
Table 6 presents the direct and indirect effects of PCSE on SRH in older adults. Among them, the PCSE intercept can directly affect the SRH intercept. The direct effect is −3.385 (95% CI: from −4.969 to −2.170), and it can also indirectly affect the SRH intercept of older adults by affecting the LS intercept, and the total indirect effect is 5.036 (95% CI: from 3.658 to 6.868), the total effect is 1.651 (95% CI: from 0.636 to 2.577). The slope of PCSE supply can directly affect the slope of SRH, with a direct effect of −3.854 (95% CI: from −6.798 to −1.491), and it can also indirectly affect the slope of SRH in older adults by affecting the slope of LS, with a total indirect effect of 5.188 (95% CI: from 2.787 to 8.367), but the total effect was not significant.
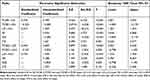 |
Table 6 Direct and Indirect Effects of PCSE on SRH |
Discussion
Development of SRH in Older Adults
From 2008 to 2018, the SRH of older adults in China exhibited a slight downward trajectory. Nevertheless, the overall level consistently remained higher than the general populace, a trend potentially attributed to the substantial proportion (58.11%) of relatively young individuals aged 65–75 years within the study cohort at baseline. Jiang (2020) noted that SRH in China tends to decline with advancing age.31 However, this decline is somewhat mitigated among older adults, possibly owing to the influence of preferential policies implemented by the Chinese government. Our study revealed that older adults with initially higher SRH experienced a more pronounced decline over the subsequent decade, suggesting that policies for older adults in China, including CSE, may exert a greater impact on postponing mortality rates among healthier older adults compared to those with lower SRH, for whom the effect of SRH decline was comparatively weaker. In light of these findings, it becomes imperative to bolster the proactive development of CSE and enhance its outreach efforts. Specifically, targeting older adults with limited awareness of CSE, such as the younger ones, necessitates intensified publicity campaigns to raise awareness about community-provided services tailored to their needs, thereby encouraging their proactive engagement with and utilization of such services. Concurrently, efforts to promote healthy lifestyles and disease prevention should be intensified to bolster SRH among this demographic. The study reveals that higher initial levels of self-rated health correlate with faster declines in health as age progresses. This may be due to reaching a health threshold as individuals age, beyond which health sharply deteriorates. Additionally, higher initial health levels might set higher psychological expectations, which, when unmet due to gradual health declines, could lead to greater psychological distress. Peer comparisons might also impact individuals’ perception of their health, especially when they see their peers maintaining stable health conditions. Therefore, even for those initially in good health, attention to psychological support and timely health interventions is crucial to mitigate the effects of rapid health declines.
The Impact of Demographic Characteristics on SRH and LS in Older Adults
This study employed latent growth curve modeling to explore the impact of demographic characteristics on the initial levels and change rates of LS and SRH among older adults. The findings indicate significant influences of age, residency, gender, and educational level on both LS and SRH. Firstly, our analysis shows that age significantly affects the initial level of LS, with younger seniors experiencing higher levels of life satisfaction. This may be due to relatively younger seniors having better health and higher participation in social activities, both of which have been shown to correlate positively with life satisfaction. Additionally, the change rate of SRH is faster among younger seniors, which may reflect more rapid changes in health status in the initial stages of aging. This finding suggests that health intervention and support strategies for the elderly need to consider age as a factor to be more targeted in supporting senior health management. Residential setting also significantly impacts the life satisfaction of older adults. Our results suggest that seniors living in urban areas not only have higher initial levels of life satisfaction but also experience slower rates of change in satisfaction. Urban residents might benefit from better medical services, more cultural and social activities, and more efficient daily living support systems, contributing to higher life satisfaction. This disparity highlights the inequality in resource distribution and accessibility between urban and rural areas, pointing out potential strategies for improving the quality of life for rural seniors. Regarding gender, our data indicate that men have higher initial SRH compared to women, consistent with many studies that find men rate their health better in the early stages of old age. This may be related to differences in physiology, psychology, and social roles between men and women. However, this gender difference also calls for further exploration of how social-cultural factors and health behaviors create health disparities between genders and how public health policies can reduce these disparities. The impact of educational level is more complex. Our findings indicate that higher educational levels correlate with higher initial levels of life satisfaction among seniors, possibly because individuals with higher education have better economic conditions and social status, as well as higher problem-solving abilities and coping strategies. However, the same group rates their initial SRH lower, which might relate to higher health expectations among the highly educated, leading them to judge their health more stringently. Additionally, individuals with higher education may face more health challenges upon entering old age due to career pressures and a faster pace of life.
The Development of PCSE Supply for Older Adults
The results of this study indicate that perceived community services (PCSE) have shown an increasing trend over time, particularly in the areas of daily care, medical treatment and medication delivery, and emotional comfort. This finding suggests that as the elderly age, their needs for these services gradually increase. This trend may be related to the gradual decline in physical and mental health among the elderly, necessitating more community support and medical assistance to maintain their quality of life. These results emphasize the importance of improving and expanding community services targeted at the elderly, especially in providing support for daily living and mental health services. To address the challenges of an aging society, community leaders and policymakers need to further enhance the accessibility and quality of these services to meet the growing needs of the elderly. Our study unveiled significant disparities in the supply of PCSE among older adults. Firstly, these variations may stem from discrepancies in the accessibility of older adults services across different communities. Previous research utilizing CLHLS data from 2008 to 2014 revealed that older adults in China perceived unmet needs for community services, with such perceptions correlating with a decline in their LS.32 Secondly, these differences may also be attributed to varying rates of demand, awareness, and utilization of CSE among older adults. Those with higher levels of need and awareness tend to exhibit greater proactivity in understanding and utilizing these services, consequently perceiving their existence more readily than their counterparts with lower levels of need.33 Furthermore, our study uncovered that older adults with lower baseline PCSE supply experienced a more pronounced increase in subsequent supply rates. This phenomenon may be attributable to older individuals with lesser initial demands for CSE exhibiting a heightened increase in service demand compared to those with greater needs, thus resulting in a perceived higher growth rate in service supply. Collectively, these findings underscore the paramount importance of ensuring an adequate supply of CSE from a demand-oriented perspective. To achieve this, it is imperative to assess the specific service needs of older adults within the community and identify any disparities between their requirements and the available services. This can be accomplished through a variety of methods, including surveys, focus groups, and consultations with older adults and their families. For communities falling short in meeting the needs of older adults, efforts should be directed towards enhancing the accessibility of services, including increased investment in funds, human resources, and infrastructure. Additionally, diversifying services to cater to the varied needs of older individuals is crucial. In the development of CSE, emphasis should be placed on fostering collaboration among government agencies, non-profit organizations, healthcare providers, and community groups. By forging partnerships and sharing resources, these stakeholders can enhance coordination and effectiveness in delivering comprehensive services to older adults.
The Impact of PCSE Supply on the Development of SRH in Older Adults
This study uncovered a noteworthy association between PCSE supply and the SRH of older adults. Specifically, older adults with higher baseline PCSE supply exhibited lower SRH, while those experiencing a faster increase in PCSE supply demonstrated a corresponding acceleration in SRH decline. This suggests that individuals with lower SRH or a more rapid decline may be inclined to pay greater attention to and utilize CSE, consequently driving up the supply level of PCSE. Given the documented positive impact of CSE on the physical and mental well-being of older adults, it is imperative to enhance the quality and public support of these services to improve the SRH of older adults. Firstly, investing in training and professional development opportunities for service providers catering to older individuals can significantly contribute to this endeavor. For instance, offering on-The-job training for social care workers can enhance interprofessional collaboration in caring for older people.34 Secondly, implementing a robust performance evaluation system framework is essential to regularly assess the effectiveness and impact of CSE. This enables timely adjustments to services based on feedback from older adults, thereby enhancing service quality and relevance.35 Moreover, emphasizing the significance of community services for older adults through diverse channels, including public events, media campaigns, and community initiatives, can foster public support and understanding. This heightened awareness can garner increased attention and resources for services, further bolstering their effectiveness and reach.
Mediating Role of LS in the Impact of PCSE Supply and SRH Development
The findings of this study underscore the positive impact of PCSE supply on enhancing LS, which in turn correlates positively with SRH and can mitigate the decline in SRH, serving as a mediator in this relationship. Consistent with prior research utilizing CLHLS data from 2018, which demonstrated that CSE can enhance the LS of older adults,24 our study aligns with findings by other scholars indicating a positive correlation between SRH, the receipt of community services, and LS among older adults.36,37 By bolstering LS among older adults through increased provision of CSE, individuals are likely to experience reduced stress levels and cultivate positive psychological states, fostering robust social support networks that positively impact their mental health.38 Furthermore, individuals content with their lives tend to engage in healthier behaviors, such as maintaining a positive mood, adhering to a balanced diet, pursuing lifelong learning, and undertaking preventive measures such as regular check-ups, all of which contribute to maintaining good physical health and reducing disease risk.39 In summary, enhancing the quantity and quality of services for older adults within the community is imperative to ensure they receive the necessary support and care for healthy aging, thereby preserving a good quality of life. Such efforts play a pivotal role in improving LS and SRH among older adults.
Limitations
Several limitations in this study deserve acknowledgment. Firstly, as data were collected directly from study participants, the measurement of health level and life satisfaction relied solely on subjective self-assessment, the presence of self-report or recall bias cannot be ruled out. Secondly, in writing the limitations section of this study, it is essential to acknowledge issues related to data missingness. Although the overall proportion of missing data is low, limiting its impact on the accuracy of the study results, the non-random nature of the missing data (MNAR: Missing Not At Random) may have profound implications for the interpretation and generalization of the study. The observed data missingness primarily resulted from participants withdrawing from the study or passing away. This pattern of missingness is likely directly associated with the participants’ health status and their access to and perceptions of community services. Given that these data were not missing at random, employing conventional multiple imputation methods to address this missingness could introduce bias, contravening the assumption of randomness required for multiple imputation. Application of such methods could lead to misleading interpretations of the results, which we strive to avoid. Despite the challenges in maintaining long-term participation of older adults in cohort studies, which has led to some data missingness, we have cautiously handled the missing data to minimize its impact on the accuracy of the study results. In future research, developing and adopting methods better suited for handling non-random missing data will be crucial for enhancing the quality and reliability of the findings. Moreover, this study did not explore the specific relationship and pathways between PCSE and LS and SRH among older adults by service type. Besides, Future research endeavors could delve into examining variations in the impact of different CSEs, shedding light on nuanced differences in their effects. Furthermore, the findings of this study are based on an established observational cohort study from China. It is possible that there may be additional, unidentified confounding factors, particularly those related to cultural and racial differences.
Conclusions
The results of this study reveal that higher perceptions of community services tailored for the elderly (PCSE) are directly and indirectly associated with improved self-rated health (SRH) among older adults, mediated through enhancements in life satisfaction (LS). This highlights the critical role that PCSE plays in fostering not only physical health but also psychological well-being among the elderly. Our findings advocate for sustained and comprehensive efforts to enhance both the quantity and quality of services available to older adults. It is imperative that these services not only meet the basic needs of the older adults but also enrich their life satisfaction, thereby indirectly contributing to better health outcomes. The interconnections between PCSE, LS, and SRH suggest that a holistic approach, which integrates the delivery of high-quality community services with initiatives aimed at boosting life satisfaction, could be particularly effective in promoting healthier aging. Moreover, the study emphasizes the necessity of community-based strategies that are responsive to the needs and preferences of older adults, encouraging their active participation in service planning and implementation. Such inclusive practices ensure that the services provided are not only accessible but also aligned with the actual needs of the elderly, thus maximizing their impact on both health and overall quality of life. In conclusion, the enhancement of PCSE is not just a matter of increasing service availability; it is about quality, suitability, and accessibility. It calls for a strategic focus on policies that recognize and support the complex interplay between an elderly individual’s satisfaction with life and their health. By doing so, we can foster an environment where older adults not only live longer but also enjoy a higher quality of life, making aging a more positive and fulfilling experience.
Data Sharing Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found here: http://opendata.pku.edu.cn/dataverse/CHADS<.
Ethics Approval and Consent to Participate
The studies involving human participants were reviewed and approved by the Ethical Review Committee of Peking University (IRB00001052-13074). Informed consent has been obtained from the participants, their parents and legally authorized representatives in this study. Our study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Binzhou Medical University (NO.2022-280).
Acknowledgments
The authors thank all the participants, assistants, and researchers for contributing to this study. Special thanks to Peking University, China Center for Disease Control and Prevention, China Center for Population and Development Research, and China Center for Aging Research (Chinese Longitudinal Healthy Longevity Survey, [CLHLS] team for providing the data).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by National Natural Science Foundation of China (No.72274023), Ministry of Education Humanities and Social Sciences Foundation of China (No.22YJA890037), Social Science Planning Fund of Shandong Province, China (No.22CGLJ01), Natural Science Foundation of Shandong Province, China (No. ZR2022MG037).
Disclosure
The authors declare no competing interests related to the study.
References
1. World Health Organization (2022). Aging: overview. Available online at: https://www.who.int/health-topics/ageing#tab=tab_1. (
2. Tan Y, Liu X, Sun H, et al. Population ageing, labour market rigidity and corporate innovation: evidence from China. Res Pol. 2022;51(2):104428. doi:10.1016/j.respol.2021.104428
3. Jiang M, Xiao M, Zhang J, et al. Middle-aged and older people’s preference for medical-elderly care integrated institutions in China: a discrete choice experiment study. BMC Nurs. 2024;23(1):1696. doi:10.1186/s12912-023-01696-w
4. Fang EF, Xie C, Schenkel JA, et al. A research agenda for ageing in China in the 21st Century (2nd edition): focusing on basic and translational research, long-term care, policy and Social Networks. Ageing Res Rev. 2020;64:101174. doi:10.1016/j.arr.2020.101174
5. Tang S, Liu M, Yang T, et al. Association between falls in elderly and the number of chronic diseases and health-related behaviors based on CHARLS 2018: health Status as a mediating variable. BMC Geriatr. 2022;22(1):3055. doi:10.1186/s12877-022-03055-x
6. Lan M, Yang L, Zhang H, et al. A structural equation model of the relationship between symptom burden, psychological resilience, coping styles, social support, and psychological distress in elderly patients with acute exacerbation chronic obstructive pulmonary disease in China. Asian Nurs Res. 2024;6(3):1016.
7. Jiang H, Liu Z. Community home elderly care services, multidimensional health and social participation of chronically ill elderly—empirical analysis based on propensity score matching and multiple mediation analysis. Front Public Health. 2023;11:21909.
8. Rahman MM, Byles JE. Older women’s patterns of home and Community Care Use and transition to residential aged care: an Australian cohort study. Maturitas. 2020;131:28–33. doi:10.1016/j.maturitas.2019.10.004
9. Karlsson S, Edberg AK, Jakobsson U, et al. Care satisfaction among older people receiving public care and service at home or in special accommodation. J Clin Nurs. 2013;22(3–4):318–330. doi:10.1111/jocn.12115
10. Deng S, Zhang C, Guo X, et al. Gaps in the utilization of community health services for the elderly population in rural areas of Mainland China: a systematic review based on cross-sectional investigations. Health Serv Insight. 2022;15:34352. doi:10.1177/11786329221134352
11. Wei K, Liu Y, Yang J, et al. Living arrangement modifies the associations of loneliness with Adverse Health Outcomes in older adults: evidence from the CLHLS. BMC Geriatr. 2022;22(1):27425. doi:10.1186/s12877-021-02742-5
12. Ma W, Shen Z. Impact of community care services on the health of older adults: evidence from China. Front Public Health. 2023;2023:60151.
13. Yang L, Wang L, Di X, et al. Utilisation of Community Care Services and self-rated health among elderly population in China: a survey-based analysis with propensity score matching method. BMC Public Health. 2021;21(1):11989. doi:10.1186/s12889-021-11989-x
14. Zeng Y, Wang LX, Fang Y. Rural-urban disparities in unmet long-term care need and community care services expectation among elderly in China. Innovn Aging. 2019;3(1):38569. doi:10.1093/geroni/igz038.569
15. Durgun H, Turan N, Kaya H. Relationship between fall behavior and quality of life of elderly individuals. Psychol Health Med. 2021;27(6):1366–1372. doi:10.1080/13548506.2021.1883686
16. Montag C, Sindermann C, Lester D, et al. Linking individual differences in satisfaction with each of Maslow’s needs to the Big Five personality traits and Panksepp’s primary emotional systems. Heliyon. 2020;6(7):e04325. doi:10.1016/j.heliyon.2020.e04325
17. Mangat M, Kaminski M. Home-based primary care: a solution for our frail elderly patients. Populat Health Manage. 2021;24(6):648–650. doi:10.1089/pop.2021.0101
18. Qin S, Cheng Y, Zhang H, Ding Y. Home/community-based medical and elderly care services utilization in China: a cross-sectional study from the middle-aged and elderly population. Healthcare. 2023;11(17):2431. doi:10.3390/healthcare11172431
19. Zhang L, Xu X. Construction of smart older adults care service model driven by Primary Health Care. Front Public Health. 2023;11:1157758. doi:10.3389/fpubh.2023.1157758
20. Wang Q, Fan K, Li P. Effect of the use of home and community care services on the multidimensional health of older adults. Int J Environ Res Public Health. 2022;19(22):15402. doi:10.3390/ijerph192215402
21. Costarelli V, Michou M. Perceived stress negatively affects diet quality and life satisfaction during the covid-19 lockdown period, in Greece. Nutr Food Sci. 2023;53(4):769–780. doi:10.1108/NFS-12-2022-0403
22. Zhang L, Hou Y, Wang H, et al. Self-rated health and life satisfaction among elderly migrants in China: a moderated mediation model of resilience and upward intergenerational support. Int J Environ Res Public Health. 2022;19(24):17009. doi:10.3390/ijerph192417009
23. Nieboer A, Lindenberg S, Boomsma A, et al. Dimensions of well-being and their measurement: the SPF-il scale. Soc Indic Res. 2005;73(3):313–353. doi:10.1007/s11205-004-0988-2
24. Zhang Z, Mao Y, Shui Y, et al. Do community home-based elderly care services improve life satisfaction of Chinese older adults? an empirical analysis based on the 2018 CLHLS dataset. Int J Environ Res Public Health. 2022;19(23):15462. doi:10.3390/ijerph192315462
25. Xu H. Physical and mental health of Chinese grandparents caring for grandchildren and great-grandparents. Soc Sci Med. 2019;229:106–116. doi:10.1016/j.socscimed.2018.05.047
26. Kim ES, Delaney SW, Tay L, et al. Life Satisfaction and Subsequent Physical. Behav Psychosocial Health Older Adults Milbank Q. 2021;99(1):209–239.
27. Aldridge Z, Thorne N, Bouman WP, et al. A longitudinal study exploring the role of mental health symptoms and social support regarding life satisfaction 18 months after initiation of gender-affirming hormone treatment. Healthcare. 2023;11(3):379. doi:10.3390/healthcare11030379
28. Ji JS, Zhu A, Lv Y, et al. Interaction between residential greenness and air pollution mortality: analysis of the Chinese Longitudinal Healthy Longevity Survey. Lancet Planet Health. 2020;4(3):1–10. doi:10.1016/S2542-5196(20)30027-9
29. Bollen KA, Curran P, et al. Latent Curve Models: A Structural Equation Approach. Wiley-Interscience; 2006.
30. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi:10.1080/10705519909540118
31. Jiang J, Zhang X. Social Transition and health inequality in China: an age-period-cohort analysis. Public Health. 2020;180:185–195. doi:10.1016/j.puhe.2019.08.025
32. Lu P, Shelley M, Kong D. Unmet community service needs and life satisfaction among Chinese older adults: a longitudinal study. Social Work Pub Health. 2021;36(6):665–676. doi:10.1080/19371918.2021.1948942
33. Ye L, Luo J, Shia B-C, et al. Multidimensional Health Groups and healthcare utilization among elderly Chinese: based on the 2014 CLHLS dataset. Int J Environ Res Public Health. 2019;16(20):3884. doi:10.3390/ijerph16203884
34. Nakamura K, Siongco KL, Moncatar TR, et al. In-service training programme for Health and Social Care Workers in the Philippines to strengthen interprofessional collaboration in caring for older adults: a mixed-methods study. Health Res Policy Syst. 2022;20(S1):09142. doi:10.1186/s12961-022-00914-2
35. Shao Q, Yuan J, Lin J, et al. A SBM-DEA based performance evaluation and optimization for social organizations participating in community and home-based elderly care services. PLoS One. 2021;16(3):48474. doi:10.1371/journal.pone.0248474
36. Song H, Li Z. Community-based service, psychological resilience and life satisfaction among Chinese older adults: a longitudinal study. Geriatr Nurs. 2023;54:148–154. doi:10.1016/j.gerinurse.2023.09.004
37. Liu Y, Liu J, Zhou S, et al. Life satisfaction and its influencing factors of middle-aged and elderly stroke patients in China: a National Cross-sectional survey. BMJ Open. 2022;12(8):59663.
38. Nakamura JS, Delaney SW, Diener E, et al. Are all domains of life satisfaction equal? differential associations with health and well-being in older adults. Qual Life Res. 2021;31(4):1043–1056. doi:10.1007/s11136-021-02977-0
39. Zadworna-Cieślak M. Spirituality, satisfaction with life and health-related behavior of older residents of long-term care institutions—a pilot study. Explore. 2020;16(2):123–129. doi:10.1016/j.explore.2019.07.016
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

