Back to Journals » Drug Design, Development and Therapy » Volume 19
The Recovery of Ciprofol, Remimazolam and Remimazolam-Flumazenil for General Anesthesia Undergoing Fundus Surgery: A Single-Center, Prospective, Randomized, Controlled Clinical Study
Authors Zhang S, Liu Y, Liu Y, Xu T
Received 27 December 2024
Accepted for publication 16 April 2025
Published 5 May 2025 Volume 2025:19 Pages 3691—3700
DOI https://doi.org/10.2147/DDDT.S512431
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Tin Wui Wong
Shuang Zhang, Yunfei Liu, Yanyu Liu,* Ting Xu*
Department of Anesthesiology, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yanyu Liu, Department of Anesthesiology, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, People’s Republic of China, Tel +8617744339886, Email [email protected] Ting Xu, Department of Anesthesiology, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, People’s Republic of China, Tel +8617708130267, Email [email protected]
Purpose: Ciprofol (HSK3486 injectable emulsion) is a 2.6-disubstituted phenol derivative that acts similarly to propofol with a fast onset, quick, and stable recovery. Moreover, remimazolam is a new benzodiazepine with a faster onset and recovery than midazolam, and more stable hemodynamics than propofol. We found no relevant literature that directly compared these two drugs. The primary objective of this study was to compare the recovery of HSK3486 with that of remimazolam during successful general anesthesia.
Patients and Methods: This prospective, randomized, double-blind study included 93 patients who had undergone fundus surgery. The patients were divided into three groups: HSK3486 (H group), remimazolam-saline (RS group), and remimazolam-flumazenil (RF group). The primary outcome was the time from drug withdrawal to eye opening, and the secondary outcome was the time from drug withdrawal to laryngeal mask removal, the time for Aldrete modified score ≥ 9, intraoperative hemodynamic changes, post-operative adverse events (nausea, vomiting, pain, delirium, re-sedation), and the Quality of Recovery-15 score before surgery and at 1, 7, and 14 days post-operatively.
Results: The RF group showed the shortest eye-opening time: 3.8 (2.8) min vs 13.3 (5.2) min for the H group, P < 0.001; and 11.5 (5.5) min for the RS group, P < 0.001. And laryngeal mask removal time was 5.2 (3.1) min for the RF group vs 14.1 (5.2) min for the H group, P < 0.001; and 12.4 (5.5) min for the RS group, P < 0.001. There were no significant differences in other post-operative outcomes.
Conclusion: The incorporation of flumazenil with remimazolam for total intravenous anesthesia provided rapid and reliable recovery of consciousness, although there were no significant visible differences between HSK3486 and Remimazolam-saline.
Keywords: remimazolam, HSK3486, recovery, fungus surgery, total intravenous anesthesia
Introduction
Fundus surgery refers to advanced microsurgical interventions targeting posterior segment ocular structures, including the retina, vitreous, and macula. It is primarily employed to manage vision-threatening conditions such as retinal detachment, diabetic retinopathy, macular holes, and vitreous hemorrhage. Some surgeries require immediate awakening after the procedure to accommodate the prone position. And intraoperative surgical precision and proper control of intraocular pressure are crucial.1,2 Although local anesthesia combined with Monitored Anesthesia Care technology can be used for cooperative adults, complex net detachment and glass incision surgeries require general anesthesia to satisfy the need for complete immobilization during delicate internal eye surgery.3
Remimazolam is a new ultrashort-acting benzodiazepine hypnotic that shows the potential to replace midazolam and propofol, with a faster onset and recovery than midazolam and a more stable hemodynamic change than propofol.4–6 It undergoes an organ-independent metabolism and is hydrolyzed by tissue esterases into inactive metabolites.7 Importantly, the cardiovascular and respiratory systems were less affected by remimazolam administration. Injection of pain is rare. Recently, remimazolam has been widely used for sedation and general anesthesia.8,9
Ciprofol (HSK3486) is a promising alternative to propofol. The addition of a cyclopropyl ethyl group to the side chain of the core phenol structure exerts its effects by binding to the gamma-aminobutyric acid A (GABAA) receptor, leading to central nervous system inhibition and achieving sedative or anesthetic effects. Multiple preclinical and clinical studies indicated that HSK3486 would offer several advantages over propofol, exhibiting rapid onset of action, lower rates of injection site pain and providing stable recovery of consciousness.10,11 It is also associated with mild-to-moderate adverse events (AEs). Recent studies conducted in China have evaluated the safety and efficacy of HSK3486 for the induction and maintenance of general anesthesia during elective surgeries, including outpatient surgery, colonoscopy, and bronchoscopy procedures. The sedation success rates for HSK3486 were 97.7% and 100% in the pre-protocol set.12–14 Despite its broad application prospects, HSK3486 is still a relatively new entrant in the field of anesthetics and, as such, requires more details. To date, the clinical efficacy and safety of remimazolam and HSK3486, both new optimization of anesthetic drugs, have been studied and compared with propofol in patients. However, a head-to-head comparison of these two drugs in terms of recovery and maintenance of surgical anesthesia needs to be established.
Given the similar but different sedative features of remimazolam and HSK3486, we conducted this trial to evaluate patients undergoing fundus surgery that required laryngeal mask airway (LMA) insertion. We aimed to compare total intravenous anesthesia (TIVA) between remimazolam and HSK3486 in terms of anesthesia recovery and safety, post-induction hypotension, and post-operative complications.
Materials and Methods
Design and Patients
The study protocol was approved by the Ethics Committee of Sichuan Provincial People’s Hospital (2023–234-1) and registered with chictr. org. cn (ChiCTR2400079506). This single-center prospective randomized study was conducted in accordance with the Declaration of Helsinki from March to September 2024. All participants provided written informed consent prior to enrollment.
Patients scheduled to undergo elective fundus surgery were screened for eligibility if their surgery was anticipated to last ≥30 minutes and required LMA insertion. The inclusion criteria were adult patients aged between 18 and 65 years with an American Society of Anesthesiologists (ASA) physical status of I–II and a body mass index (BMI) between 18 and 25 kg/m2. Patients were excluded if they abused alcohol or drugs; had a history of allergies to medications used in the study protocol; or had clinically significant cardiovascular (myocardial infarction, severe arrhythmias, valvular heart disease requiring surgical intervention), respiratory (chronic obstructive pulmonary disease, active pulmonary hypertension), or liver disease (acute hepatitis, portal hypertension with variceal bleeding history) and so on. Patients who had underlying systemic diseases or poorly controlled psychiatric disorders that could interfere with the interpretation of the outcome assessments, or those who demonstrated an inability to understand the informed consent and study protocol were also excluded.
Intervention and Sedation/Anesthesia Protocol
Eligible participants were randomized into three groups: the HSK3486 group (H group), remimazolam-saline group (RS group), and remimazolam-flumazenil group (RF group) using a computer-generated coding system with blocked randomization in a 1:1:1 allocation ratio. Group assignment was performed in an opaque envelope by an investigator who was not involved. As anesthesiologist investigators who induced general anesthesia could not be blinded to the group assignment owing to different anesthetic management requirements among the three groups, all data collection and analysis were performed by a dedicated investigator who was blinded to the group assignment. All patients and outcome assessors in the post-anesthesia care unit (PACU) and ward were blinded to the group allocation.
Vital signs (noninvasive blood pressure, heart rate, pulse oxygen saturation, and noninvasive temperature) were monitored and recorded at set time points (T1, pre-induction; T2, loss of consciousness; T3, after laryngeal mask airway (LMA) insertion; T4, beginning of surgery; T5, end of surgery; T6, out of the operating room; T7, opening eyes; T8, reaching PACU; T9, LMA withdrawal; T10, leaving the PACU). In PACU, the time was recorded that it took to reach an Aldrete modified score of ≥9. Quality of Recovery-15 (QoR-15) was used to evaluate the quality of post-operative recovery before the surgery and on the second, seventh, and fourteenth days after surgery. Numerical rating scores (NRS) and adverse events were recorded.
All patients received oxygen via mask at a rate of 6 L/min. The patients in the HSK3486 group (H group) received HSK3486 injectable emulsion (Haisco Pharmaceutical Group, China) at a speed of 0.4 mg/kg within 30 seconds with remifentanil 2 μg/kg intravenously after disappearance of a corneal reflex. The anesthesiologist then inserted a laryngeal mask and implemented the mechanical ventilation. The recommended rate of HSK3486 administration was 0.1–0.3 mg/kg/h and 0.1–0.2 μg/kg/min remifentanil during maintenance. Subjects in the remimazolam-saline group (RS group) and remimazolam-flumazenil group (RF group) received total intravenous administration of remimazolam (Yichang Humanwell Pharmaceutical Co., Ltd., China) 0.2 mg/kg and remifentanil (2 μg/kg). Intravenous remimazolam 1–2 mg/kg/h and remifentanil 0.1–0.2 μg/kg/min were infused continuously for maintenance.
Intravenous anesthetic infusion was discontinued immediately after surgery. Flurbiprofen axetil (50 mg) and tropisetron (5 mg) were also administered. Flumazenil 0.5 mg was administered to the RF group and the same volume of normal saline was administered to the H and RS groups.
Also, rescue 0.1 mg/kg of cisatracurium was added if severe involuntary movements, laryngospasm, or peak airway pressure ≥30 mmHg appeared after LMA insertion. Therefore, these patients were excluded from this study. During surgery, adverse events (hypotension, bradycardia, tachycardia, apnea, respiratory depression, and myoclonus) were evaluated. If MAP was < 65 mmHg, ephedrine 6 mg was administered intravenously. If the heart rate was < 40 beats per minute, the operation was immediately stopped and atropine (0.2 mg or 0.004–0.01 mg/kg) was injected intravenously if bradycardia persisted ≥1 minutes after discontinuing surgical stimuli.
Statistical Analysis
To the best of our knowledge, no study has directly described the recovery of HSK3486 and remimazolam. It has been reported that the average recovery time after HSK3486 withdrawal is less than 10 minutes for maintaining anesthesia in general elective surgery within 2 hours. Upon reviewing the literature and our preliminary result, we presuppose the mean time to emergence from anesthesia was 10.5 (9.0) minutes in the remimazolam group vs 8.3 (5.1) minutes in the HSK3486 group. If α = 0.15 and β = 0.9, using the one-way Analysis of Variance formula, at least 19 patients calculated by Power Analysis and Sample Size (PASS) V15.0.5 software (NCSS, LLC, Kaysville) would be needed in each group. Considering a 30% dropout rate, the sample size was increased to 28 for each group, for a total sample size of 84.
The Statistical Package for Social Sciences (SPSS) software (version 25.0; Inc., Chicago, Illinois, USA) was used for statistical analysis. Data were tested for normal distribution using the Kolmogorov–Smirnov test. The Mann–Whitney–Wilcoxon test was used for data with non-normal distribution. For all analyses, P values were two-sided, and statistical significance was set at P < 0.05.
Normally distributed variables were expressed as mean ± standard deviation (SD) and were used one-way ANOVA to assess overall differences across all three groups. Conduct post hoc tests (Bonferroni-corrected t-tests) only if ANOVA reveals significant differences. The Mann–Whitney U-test was used for non-normally distributed data, which were presented as median and interquartile range (IQR), and 95% confidence intervals (CIs) for non-normally distributed variables were calculated using the Hodges-Lehmann estimator. Categorical variables were analyzed using the χ2 test and Fisher’s exact test and were expressed as frequencies and percentages. The Wilcoxon rank-sum test was used to compare the rank variables. Pairwise comparisons were conducted for continuous parameters at each time point using multivariate analysis of variance.
Outcomes
The primary outcome was the time from medication cessation to eye opening, laryngeal mask withdrawal, and the time until an Aldrete modified score ≥ 9. The following indicators were met when the laryngeal mask was removed: the patient could respond to verbal stimulation, the tidal volume reached 6–8 mL/kg; hemodynamic parameters were stable, and spontaneous ventilation resumed.
The secondary efficacy outcomes included vital sign fluctuations (MAP, HR, airway pressure peak), dosage of rescue ephedrine and atropine, and change in QoR-15 scores. Complications, such as injection pain, muscle rigidity, and hiccups, were noted.
Results
Patient Characteristics
From July 2023 to June 2024, 110 patients were screened for eligibility, 107 patients were randomized, and three patients refused to participate. Nine patients (four patients in the HSK3486 and RF groups; one patient in RS group) were excluded due to loss to follow-up. Five patients (two in the RF and HSK3486 groups and one in the RS group) who received rescue cisatracurium were excluded from the analysis. Thus, 93 patients were included in the analysis (Figure 1, CONSORT diagram). Dropout rates did not differ among the three groups.
 |
Figure 1 Consolidated standards of reporting trials.(CONSORT) diagram. |
Primary Outcomes
The time to eye opening was 11.5 (5.5) minutes in the remimazolam group vs 13.3 (5.2) minutes in the HSK3486 group, and 3.8 (2.8) minutes for the remimazolam-flumazenil group (Table 1, Figure 2A). The mean difference between the H and RS groups was −1.7 (95% CI: –4.6–0.9, P = 0.78) minutes, with a difference of −7.7 (95% CI: −10.0, −5.5, P ≤ 0.01) minutes between groups RS and RF. The difference between the H and RF groups was −9.5 (95% CI: −11.71, −7.308, P ≤ 0.01) minutes.
 |
Table 1 Summary of Primary and Secondary Efficacy Outcomes |
Secondary Outcomes
The two groups were comparable in terms of their baseline characteristics (Table 2). The time to removing the laryngeal mask for the H group was 14.1 (5.2) min vs 12.4 (5.5) min for the RS group, median difference: −1.7 (95% CI: −4.4, 0.9 min, P = 0.21). The time for the RF group was 5.2 (3.1) minutes. The median difference between groups H and RF was −8.8 (95% CI: −11.2, −6.7, P ≤ 0.01) (Table 2 and Figure 2B). The RF group had the shortest time to reach an Aldrete modified score ≥ 9: 11.9 (6.0) vs 21.0 (6.0) min, P ≦ 0.01 for RF vs H group, 11.9 (6.0) vs 21.7 (8.4) min, P ≦ 0.01 for RF vs RS group), one patient in the RS group did not reach the goal score till 30 minutes after surgery, becoming fully alert in the next 15 minutes. No significant difference was observed between the H and RS groups. This result is illustrated as a Kaplan-Meier survival curve (Figure 2C). Figure 2D shows that the time change in the BIS values between 40 and 60 for HSK3486 was significantly longer than that in the remimazolam-saline group. The total infused doses of the study medications are shown in Table 1 (HSK3486: 130.8 (86.7) mg; remimazolam: 113.5 (67.8) mg for the RS group and 91.9 (42.3) mg for the RF group. The total infused dose of remifentanil was similar between the groups: 864.2 (358.0) µg in the HSK3486 group, 1030.5 (518.5) µg in the RS group, and 867.6 (279.5) µg in the RF group (P = 0.264). The total duration of anesthesia was approximately 2 hours in all groups.
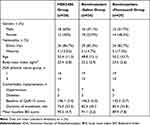 |
Table 2 Demographic and Surgical Characteristics |
The QoR-15 score before surgery did not show a significant difference among the groups at 1, 7, and 14 days after surgery (Table 2). The three groups also did not differ in terms of the rate of complications (nausea and vomiting). None of the patients reported any post-operative injection pain. There was no difference in the incidence of muscle rigidity or hiccups among the three groups.
It seems that the HSK3486 group had a higher incidence of post-induction hypotensive episodes and administration of ephedrine administration was higher in patients receiving HSK3486 than in those receiving remimazolam; however, the difference was not statistically significant (Table 2 and Figure 3A). No significant difference was observed in the incidence of critical bradycardia. Based on the reanalysis, the incidence rate of post-induction hypotensive events was 27 (42.8%) in patients receiving remimazolam and 16 (53.3%) in patients receiving HSK3486 (P = 0.5069) (Figure 3B).
Discussion
To the best of our knowledge, this is the first trial to directly compare the quality of recovery after TIVA with remimazolam or HSK3486 in patients undergoing fundus surgery. We found that remimazolam-based TIVA with planned incorporation of flumazenil led to significantly faster recovery of consciousness than HSK3486 or remimazolam with saline. Moreover, no significant differences were observed in the emergence of HSK3486 and remimazolam in saline.
There are several considerations regarding the efficacy of remimazolam compared with that of HSK3486 in this study. Anesthesiologists were experienced in the rational use of propofol; however, most of them had not used HSK3486 and had little or no experience with titration to maintain anesthesia. Pharmacokinetic and pharmacodynamic models for HSK3486 and remimazolam, as well as our organizational experience, were used to calculate the dosing scheme.15–18 An identical dosage or dosage range for remifentanil in all three groups was administered similarly because there were no available interaction models for remimazolam and remifentanil. Because the effect of remimazolam on commercially available processed EEG received inconsistent performance, with HSK3486 unstudied, we could not expect to achieve the same EEG result as the reference.19 Therefore, it is unknown whether the achieved emergence feature comparison is clinically significant. Residual neuromuscular blockade can cause discomfort in patients and may affect the primary outcome. Therefore, we attempted to eliminate the dosage of neuromuscular relaxation in the pilot trial, and followed this protocol in a formal experiment. Additionally, we did not attempt to use verbal arousal to accelerate the emergence process, which differs from a previous study.8 This may also explain why all patients recovered more slowly than those in the other studies. We hope that these contrasts with most other trials will make direct comparisons more robust.
Although some studies reported inconsistent longer times with tracheal extubation and orientation after remimazolam administration, similar results have been reproduced in flumazenil-accelerated recovery speeds.4,5,15,20,21 A recent report showed that the planned incorporation of flumazenil in remimazolam-based TIVA resulted in a significantly faster recovery than that of propofol in patients undergoing endoscopic variceal ligation under general anesthesia.22 In our study, the time to eye opening was significantly longer in patients who received remimazolam with saline than in those who received remimazolam with flumazenil, with a median time of 7.7 minutes. In addition, the time to withdrawal of LMAs of remimazolam-based TIVA with planned incorporation of flumazenil was 7.2 minutes faster than that of remimazolam with saline. No post-operative re-inhibition was observed in remimazolam-based TIVA with the planned incorporation of flumazenil.
Rare direct data proved that HSK3486 was associated with semblable quick recovery compared with propofol, and there is a scarcity of data for HSK3486 compared with remimazolam. The recovery time of HSK3486 6 mg/kg/h was 10.5 (5.9) minutes.12 In our study, we found that the RF group had the shortest mean eye-opening time, but resembled the emergence time between HSK3486 and remimazolam with saline. We presupposed that the recovery time of HSK3486 may be shorter than that of remimazolam with saline. And the time for withdrawing LMA demonstrated the same characteristics (5.3 minutes for group RF vs 14.2 minutes for group H and 12.4 minutes for group RS). Surprisingly, HSK3486 did not show an advantage in recovery time compared to remimazolam with saline in this study. However, we did not enroll in the analysis of propofol results; the median recovery time of propofol at our institution was less than 10 minutes (based on historical experimental data). Although the difference between the HSK3486 and Remimazolam-saline groups for the time to reach an Aldrete modified score ≥ 9 was insignificant, we found that the HSK3486 group showed slower eye opening and a longer time for LMAs to withdraw, but higher initial Aldrete scores, and one patient in the remimazolam group showed a marked delay in awakening. This inconsistent result should be taken into consideration because the Aldrete score was obtained every 5 minutes for half of 1 hour, but it also requires more detailed observation. However, the accuracy of the results remains unclear. However, this phenomenon requires further investigation.
The incidence of hypotensive events, defined as MAP ≤ 65 mmHg, did not differ significantly between the remimazolam and HSK3486 groups. Although no difference in vasopressor dosage was observed between the HSK3486 and remimazolam groups, the HSK3486 group exhibited a relatively higher rate of hypotension and ephedrine dosage. This finding is consistent with our prediction. Several conditions for trial design and experimental agents could explain this, including relatively robust adults, composed of patients with ASA I–II and low-risk surgeries. Further studies should be conducted to explore performance in high-risk patients. As remifentanil can also cause cardiovascular depression, we cannot ignore the effects of remifentanil. This further addresses the potential cardiovascular benefits of remimazolam in this setting. For intraoperative eye inversion, we did not receive any negative feedback from the surgeons. Although we noticed transiently elevated plateau pressure, particularly in remimazolam TIVA, these factors did not affect surgical procedures, which may be because there was only a weak correlation between eye inversion and airway muscle movement.
We employed the BIS index to monitor the depth of anesthesia but did not judge this, since controversial reports exist regarding the relevance of remimazolam and BIS.19,23 There are very few reports on the relationship between HSK3486 and BIS index. All anesthesia procedures were administered by an experienced professor who was blinded to the group allocation. The responsible anesthesiologist adjusted the infusion dose based on a synthetic analysis of his experience and body movements during the operation. No incidence of intraoperative awareness has been reported. We found that BIS values were higher in the remimazolam group (> 60) than in the HSK3486 group during surgery. Hence, when the BIS value was maintained at 40–60, some patients in the remimazolam group may have achieved undesired deeper sedation.
QoR-15 scores were recorded before and after surgery. No significant differences were found between the groups. Investigators reported the absence of clinically verified delirium as an adverse event; therefore, the incidence of delirium could not be confirmed until the first 14 post-operative days in patients receiving remimazolam or HSK3486. Furthermore, fundus surgery itself can also affect the daily activities of patients after surgery, resulting in relatively low scores (daily activity scores are partly affected by eye discomfort). In addition, the incidence of nausea and/or vomiting was similar among the three groups. We did not observe any problems regarding the safety of the study drugs.
Most of these drawbacks were addressed in our trial; however, this study has some limitations. First, the BIS has not been validated for quantifying the anesthetic effect of remimazolam or HSK3486, and we did not adjust the anesthetic doses under BIS guidance and maintained a BIS index < 60 in all patients. Second, this study was designed as a single-center clinical trial. Despite enrolling patients from ethnic minorities, the sample size was still limited, which might lack the generalizability of the results. Third, no propofol trials were performed concurrently because we were more interested in exploring the advantages of HSK3486 and remimazolam in future clinical application.
Conclusion
In conclusion, we have shown that remimazolam-based TIVA with planned incorporation of flumazenil is more effective in reducing the time required for emergence and optimizing the recovery quality from general anesthesia, compared to HSK3486 and remimazolam. In addition, the use of remimazolam also significantly reduced the incidence of postinduction hypotension in patients. Clinicians may wish to consider using remimazolam with flumazenil reversal for induction and maintenance of anesthesia when requiring rapid postoperative recovery and coordination of body positioning.
Data Sharing Statement
Deidentified participant data, including demographic information, clinical baseline characteristics, and outcome measurements (primary/secondary endpoints) and processed datasets used for statistical analyses will be shared.
To protect participant privacy while promoting transparency, the specific data will be made available upon formal and reasonable request. Researchers may contact the corresponding author via email at [email protected] or through our institutional data repository [Department of Anesthesiology, Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China]. We welcome inquiries and will gladly assist requestors in navigating access procedures.
The data will be released six months after publication of this article and remain accessible for five years. Recognizing the evolving nature of scientific inquiry, we remain open to discussing extended access timelines for justified academic purposes. All requests will be evaluated with strict adherence to institutional ethics policies and data protection regulations.
Available Study Documents are Full study protocol (original and amended versions); Informed consent form template (with confidential information redacted); Analytical code supporting the reported results.
Ethical Statement
Studies involving human participants were reviewed and approved by the Ethics Committee of Sichuan Provincial People’s Hospital (2023-234-1) and were registered with chictr.org.cn (ChiCTR2400079506).
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang Y, Ryu CL, Mokhtarzadeh A, Lee M, Harrison A, McClelland C. Optic nerve sheath fenestration for treatment of retrolaminar silicone oil migration. Ophthalmic Plast Reconstr Surg. 2019;35(2):e31–e34. doi:10.1097/IOP.0000000000001300
2. Wainwright AC. Positive pressure ventilation and the laryngeal mask airway in ophthalmic anaesthesia. Br J Anaesth. 1995;75(2):249–250. doi:10.1093/bja/75.2.249
3. Licina A, Sidhu S, Xie J, Wan C. Local versus general anaesthesia for adults undergoing pars plana vitrectomy surgery. Cochrane Database Syst Rev. 2016;9(9):CD009936. doi:10.1002/14651858.CD009936.pub2
4. Choi JY, Lee HS, Kim JY. Comparison of remimazolam-based and propofol-based total intravenous anesthesia on postoperative quality of recovery: a randomized non-inferiority trial. J Clin Anesth. 2022;82:110955. doi:10.1016/j.jclinane.2022.110955
5. Fechner J, El‐Boghdadly K, Spahn DR. Anaesthetic efficacy and postinduction hypotension with remimazolam compared with propofol: a multicentre randomised controlled trial. Anaesthesia. 2024;79(4):410–422. doi:10.1111/anae.16205
6. Dong SA, Guo Y, Liu SS. A randomized, controlled clinical trial comparing remimazolam to propofol when combined with alfentanil for sedation during ERCP procedures. J Clin Anesthesia. 2023;86:111077.
7. Chae D, Kim H-C, Song Y, Choi YS, Han DW. Pharmacodynamic analysis of intravenous bolus remimazolam for loss of consciousness in patients undergoing general anaesthesia: a randomised, prospective, double-blind study. Br J Anaesth. 2022;129(1):49–57. doi:10.1016/j.bja.2022.02.040
8. Oh EJ, Chung YJ, Lee J-H. Comparison of propofol vs. remimazolam on emergence profiles after general anesthesia: a randomized clinical trial. J Clin Anesth. 2023;90:111223. doi:10.1016/j.jclinane.2023.111223
9. Mao Y, Guo J, Yuan J, Zhao E, Yang J. Quality of recovery after general anesthesia with remimazolam in patients’ undergoing urologic surgery: a randomized controlled trial comparing remimazolam with propofol. Drug Des Devel Ther. 2022;16:1199–1209. doi:10.2147/DDDT.S359496
10. Gan TJ, Bertoch T, Habib AS. Comparison of the efficacy of HSK3486 and propofol for induction of general anesthesia in adults: a multicenter, randomized, double-blind, controlled, Phase 3 noninferiority trial. Anesthesiology. 2024;140(4):690–700. doi:10.1097/ALN.0000000000004886
11. Yang Y, Xia Z, Xu C, Zhai C, Yu X, Li S. Ciprofol attenuates the isoproterenol-induced oxidative damage, inflammatory response and cardiomyocyte apoptosis. Front Pharmacol. 2022;13:1037151. doi:10.3389/fphar.2022.1037151
12. Akhtar SMM, Fareed A, Ali M. Efficacy and safety of Ciprofol compared with Propofol during general anesthesia induction: a systematic review and meta-analysis of randomized controlled trials (RCT). J Clin Anesth. 2024;94:111425. doi:10.1016/j.jclinane.2024.111425
13. Chen B-Z, Yin X-Y, Jiang L-H, Liu J-H, Shi -Y-Y, Yuan B-Y. The efficacy and safety of ciprofol use for the induction of general anesthesia in patients undergoing gynecological surgery: a prospective randomized controlled study. BMC Anesthesiol. 2022;22(1):245. doi:10.1186/s12871-022-01782-7
14. Ding G, Wang L, Zhao W, Diao Y, Song D. Comparison of the efficacy and safety of ciprofol and propofol for ERCP anesthesia in older patients: a single-center randomized controlled clinical study. J Clin Anesth. 2024;99:111609. doi:10.1016/j.jclinane.2024.111609
15. Lee A, Shirley M. Remimazolam: a review in procedural sedation. Drugs. 2021;81(10):1193–1201. doi:10.1007/s40265-021-01544-8
16. Liu L, Wang K, Yang Y. Population pharmacokinetic/pharmacodynamic modeling and exposure-response analysis of ciprofol in the induction and maintenance of general anesthesia in patients undergoing elective surgery: a prospective dose optimization study. J Clin Anesth. 2024;92:111317. doi:10.1016/j.jclinane.2023.111317
17. Hu C, Ou X, Teng Y. Sedation effects produced by a ciprofol initial infusion or bolus dose followed by continuous maintenance infusion in healthy subjects: a Phase 1 trial. Adv Ther. 2021;38(11):5484–5500. doi:10.1007/s12325-021-01914-4
18. Yuan J, Liang Z, Geoffrey M. Exploring the median effective dose of ciprofol for anesthesia induction in elderly patients: impact of frailty on ED(50). Drug Des Devel Ther. 2024;18:1025–1034. doi:10.2147/DDDT.S453486
19. Schüttler J, Eisenried A, Lerch M, Fechner J, Jeleazcov C, Ihmsen H. Pharmacokinetics and pharmacodynamics of remimazolam (CNS 7056) after continuous infusion in healthy male volunteers: Part II. Pharmacodynamics Electroencephalogram Effects Anesthesiol. 2020;132(4):652–666.
20. Borkett KM, Riff DS, Schwartz HI. A Phase IIa, randomized, double-blind study of remimazolam (CNS 7056) versus midazolam for sedation in upper gastrointestinal endoscopy. Anesth Analg. 2015;120(4):771–780. doi:10.1213/ANE.0000000000000548
21. Zhu H, Su Z, Zhou H. Remimazolam dosing for gastroscopy: a randomized noninferiority trial. Anesthesiology. 2024;140(3):409–416. doi:10.1097/ALN.0000000000004851
22. Doi M, Morita K, Takeda J, Sakamoto A, Yamakage M, Suzuki T. Efficacy and safety of remimazolam versus propofol for general anesthesia: a multicenter, single-blind, randomized, parallel-group, phase IIb/III trial. J Anesth. 2020;34(4):543–553. doi:10.1007/s00540-020-02788-6
23. Kreuer S, Bruhn J, Larsen R, Bialas P, Wilhelm W. Comparability of Narcotrend index and bispectral index during propofol anaesthesia. Br J Anaesth. 2004;93(2):235–240. doi:10.1093/bja/aeh182
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



