Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 17
The Relationship Between Computerized Face and Tongue Image Segmentation and Metabolic Parameters in Patients with Type 2 Diabetes Based on Machine Learning
Authors Wen S , Li Y, Xu C, Jin J, Xu Z, Yuan Y, Chen L, Ren Y, Gong M, Wang C, Dong M , Zhou Y, Yuan X, Li F, Zhou L
Received 17 August 2024
Accepted for publication 25 October 2024
Published 29 October 2024 Volume 2024:17 Pages 4049—4068
DOI https://doi.org/10.2147/DMSO.S491897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Song Wen,1,2 Yanyan Li,1 Chenglin Xu,1 Jianlan Jin,1 Zhimin Xu,1 Yue Yuan,1 Lijiao Chen,1 Yishu Ren,1 Min Gong,1 Congcong Wang,1 Meiyuan Dong,1 Yingfan Zhou,3 Xinlu Yuan,1 Fufeng Li,4 Ligang Zhou1,2,5
1Department of Endocrinology, Shanghai Pudong Hospital, Fudan University, Pudong Medical Center, Shanghai, 201399, People’s Republic of China; 2Fudan Zhangjiang Institute, Fudan University, Shanghai, 201203, People’s Republic of China; 3Medical School of Tianjin University, Tianjin, 300072, People’s Republic of China; 4Shanghai University of Traditional Chinese Medicine, Shanghai, 201203, People’s Republic of China; 5Shanghai Key Laboratory of Vascular Lesions Regulation and Remodeling, Shanghai Pudong Hospital, Fudan University Pudong Medical Center, Shanghai, People’s Republic of China
Correspondence: Ligang Zhou, Department of Endocrinology, Shanghai Pudong Hospital, Fudan University, Pudong Medical Center, Shanghai, 201399, People’s Republic of China, Tel +8613611927616, Email [email protected] Fufeng Li, Shanghai University of Traditional Chinese Medicine, Shanghai, 201203, People’s Republic of China, Email [email protected]
Objective: We aim to examine and reestablish the correlational and linear regression relationships, as well as the predictive value, between the significant facial and tongue features and the metabolic parameters in type 2 diabetes mellitus (T2DM).
Materials and Methods: From March to May 2024, we studied 269 patients with T2DM in the endocrinology department of Shanghai Pudong Hospital. The patients’ facial and tongue characteristics were sampling by a tongue imaging device equipped with artificial intelligence (AI) (XiMaLife, Sinology, China) of automated and advanced machine learning algorithms. Then, the imaging features were examined in relation to the blood examination.
Results: Multiple facial and tongue features, as well as dimensional facial and tongue color parameters, were significantly correlated with glycated hemoglobin A1c (HbA1c) (r < 0.3, p < 0.05), glycated albumin (GA) (− 0.20 < 0.30, p < 0.05), C-peptide (− 0.20.20, p < 0.05), plasma insulin (r < 0.30, p < 0.05), fasting plasma glucose (FPG) (r < 0.3, p < 0.05), significant hepatic and renal function indicators (− 0.30 < r < 0.20, p< 0.05), cardiac injury markers (− 0.30 < r < 0.30, p < 0.05), tumor markers (− 0.5 < r < 0.5, p < 0.05), thyroid function (− 0.15 < r < 0.55, p < 0.05), and blood cell count, including white blood cells (r < 0.2, p < 0.05), and hemoglobin (Hb) (− 0.30 < r < 0.3, 0.0001. The correlational results demonstrated that the tongue’s characteristics and signs may be linked with the dynamic of the metabolic status of T2DM. In order to examine the causal relationships, we performed linear regression analyses, which revealed that various facial and tongue imaging parameters partially determined the metabolic indicators. The predictive value of imaging features was evaluated by receiver operating characteristic curve (ROC) to assess metabolic status in T2DM.
Conclusion: This study demonstrated that metabolic status, renal and hepatic, cardiac, and thyroid function, the proportion of blood cells, and Hb in T2DM were intimately associated with facial and tongue features. The precise analysis of facial and tongue features through AI and advanced machine learning could be used to predict T2DM’s conditions and progression.
Keywords: type 2 diabetes, tongue imaging, face imaging, cardiovascular disease, machine learning
Introduction
In ancient Greek medicine and Chinese Traditional Medicine (TCM), physicians examined the tongue and face’s surface for various characteristic features, including color, hydration, coating, and texture, to obtain insight into a patient’s overall health.1–3 The tongue and face observation are critical components of the numerous tools for diagnosis.4,5 Tongue and face diagnosis, also referred to as tongue and face inspection, can provide valuable insights into the efficacy of treatment, the progression of the disease, and the overall health status of a patient.6 The tongue and face’s color can vary from colorless to dark red, suggesting a variety of pathologies, including blood deficiency and Qi deficiency. The tongue coating and texture also indicate conditions such as metabolic abnormalities in the internal environment, abnormal proliferation of gut microbiota, serum lipid imbalance, and microvascular damage.7–9
A global health concern, type 2 diabetes is a prevalent metabolic disorder that is distinguished by elevated blood glucose levels as a result of insulin resistance and insufficient insulin production.10 Although blood tests and clinical symptoms are the primary diagnostic tools, recent research and traditional medical practices have underscored the potential of tongue and face observations as non-invasive indicators of this condition.11–13 In TCM, DM was termed “XiaoKe”, or emaciation and thirst syndrome, in which the patient experiences weight loss and thirst secondary to the polyuria and hyperglycemia; XiaoKe could be traced to the TCM pathophysiology of lung dryness causing thirst, stomach heat causing hyperphagia and weight-loss, and renal asthenia causing polyuria and diabetes; therefore, the syndromes could be classified into lung-stomach dry-heat, spleen-stomach Qi asthenia, renal Yin-asthenia, Yin and Yang asthenia syndromes, which were accompanied by the distinct and specific tongue and facial signs. The TCM physicians could diagnose the DM patients with different signs according to the various manifestations of the tongue combined with other clinical symptoms and signs as well as pulse signs, acknowledge the condition or progress or treatment efficacies, and eventually administer respective medications (dialect therapy) and other therapies such as acupuncture. Thus, the facial and tongue signs are critical to diagnosing and treating DM by TCM physicians. For example, some TCM physicians could judge the patients with “spleen” (could be alternated to the modern medicine notion of pancreas) Qi asthenia by observing thick white tongue fur with other characteristics such as expanded tongue volume, slippery tongue, or scalloped tongue, indicating the accumulating of the dampness (a sign may be associated with incompetently handling the fluid transforming and transportation of the spleen caused by Qi asthenia), a classical sign in XiaoKe and obese patients, therefore alerting us if we should measure the pancreatic function and insulin resistance in these spleen Qi asthenia T2DM patients; another example would be the purple tongue or lips or even facial, suggesting stagnant of blood, a sign alert to exclude potential cerebrocardiovascular complications, or to implement respective preventive measures.
To validate and further explore the intimate metabolic relationships between the tongue and facial signs with T2DM via the modern medicine multiparameter assay, in this paper, we investigate the scientific foundation and clinical implications of observing the correlation between T2D and its manifestation through tongue and face characteristics. The incorporation of TCM and modern medicine would not only fill the gap between them, for instance, to promote the mutual understanding between them on the rationale or mechanism distinction of diagnosis and treatment, but also strengthen both of them, such as standardized and precise TCM diagnosis and treatment, or improve individualized therapy for the T2DM patients in modern medicine especially in chronic diabetic complications.
The use of image processing techniques to digitize and analyze tongue and face observation was becoming increasingly prevalent due to technological advancements.14–17 The precision and reproducibility of tongue and face diagnosis are enhanced by these techniques, which increases its accessibility to all physicians worldwide who are not familiar with Traditional Chinese Medicine (TCM). These technologies can potentially improve the efficacy and reliability of ancient diagnostic methods by integrating precise laboratory metabolic data with the ancient tongue and face diagnosis in T2DM patients. This paper examines the implications of tongue-and-face observation on the metabolic parameters of patients with T2DM.
Materials and Methods
Source of Patient Data
The study includes 269 adult T2DM patients admitted to the Department of Endocrinology at Shanghai Pudong Hospital between March and May 2024. They were selected in a randomized manner and fulfilled the diagnostic criteria for T2DM, as defined by the established World Health Organization (WHO) and American Diabetes Association (ADA) guidelines.18 Oral anti-diabetic medication, such as metformin, sulfonylurea, glinides, pioglitazone, sodium-glucose co-transporter inhibitors (SGLT-2i), α-glucosidase inhibitors, and dipeptidyl peptidase-IV inhibitors (DPP-IV inhibitors), as well as injectables, such as glucagon-like peptide-1 receptor agonists (GLP-1RA) and insulin (basal insulin or combined with prandial insulin or premixed insulin), were administered to patients in accordance with disease progression, glycemic control, and complications such as liver or kidney insufficiency. The selection criteria excluded other types of diabetes, such as T1DM, secondary DM, gestational DM, and other specific forms of DM. The study also excluded a few severe conditions, such as diabetic acidosis, hyperosmolar hyperglycemic state, lactic acidosis, shock, hypoperfusion of circulation, severe systemic disorders, stroke, asthma, uremia, intestinal obstruction, and severe sepsis.
Blood Sampling and Methods of Laboratory Assessment
The metabolic parameters were collected from patients on the day following their admission. These laboratory parameters include serum blood glucose, pancreatic islet function, hemoglobin A1C (HbA1C), thyroid function, hepatic and renal function, and whole blood cells. All biochemical indicators, including fasting blood glucose, hepatic function, and kidney function indicators, were analyzed using a full-automatic biochemical analyzer (ADVIA Chemistry XPT, SIEMENS, USA). The TOSOH G8 analyzer was used to determine the glycemic control level over the past three months. C-peptide and thyroid function indicators were processed using chemiluminescence methods in a full-automatic chemiluminescence immunoassay analyzer (ADIVA Centaur XPT, SIEMENS, USA).
Data Collection of Face and Tongue Color
Upon admission to the ward, the patients were arranged to receive the facial and tongue information sampling in an exclusive room with sufficient light and quietness. A prior request was made to the patient to clean their face and mouth. Subsequently, the tongue device was equipped with advanced AI ((XiMaLife, Sinology, China) and automatic machine learning to analyze the segmented features of the tongue and face by incorporating the fundamental information of each patient, and the based rationale of AI has been previously established.19–21 This analysis includes color correction (RGB value retraction, CIELab space analyzing based on machine learning, segmentation algorithm optimization utilizing ASPP module analyzing multiple alternative parameters), DetNet algorithm, a real-time Anchor-free model detection utilizing ATSS target-sampling and Generalized Focal Loss function to classification and boundary regression, the SegNet to improve the tongue segmentation analyses.
The face and tongue images of T2DM patients were subsequently acquired by the device equipped with a high-definition camera. Patients volunteered to receive the facial and tongue image sampling by the device at the standardized light source aligned to the CIELAB standards. The data were subsequently transferred to the private database of Shanghai Traditional Medicine University for backup. The technician subsequently retracted the backend information and privately transmitted it to the investigators of this study. Numerous previous studies have found this machine’s operating system information and detailed calculations and processes.
The categorical features for facial color are defined by machine calculation and include pale, normal, redness or yellow, and black. Lip color: red or dark red. Facial gloss: glossy or Dull. Tongue characteristics include pale white, light red, red, deep red, or dark red. Color of fur: yellow and white. Fur greasy: normal fur, oily fur, or lacking fur. Fur thickness: Thick or thin; Tongue lesion: normal or fission. Tongue volume: average or fat.
The face, lip, gloss, tongue, or fur color data were calculated using the Lab Color Space, also known as the CIELAB color space. This color-opponent space is based on the coordinates of the nonlinearly compressed CIE XYZ color space. It consists of three dimensions: L, a, and b, representing brightness, and two color-opponent dimensions, respectively. L (Lightness) refers to the pixel’s luminance, which ranges from pure black to pure white: 0–255. a (Red-Green): Indicates the range from red to green, with values ranging from approximately 0 (green) to 255 (red). b (Yellow-Blue): Indicates the spectrum from yellow to blue, with values ranging from approximately 0 (blue) to 255 (yellow). The discrete dimensional color parameter allows the machine to analyse the tongue and facial condition of individual T2DM patients. The sampling procedure is illustrated in Figure 1.
 |
Figure 1 The tongue imaging device discern the different pathological features of tongue displayed as normal color (A), coating (B) tongue lesion (C), and both (D). |
Statistical Analyses
The statistical analyses were conducted using Prism (GraphPad, version 10.0) and SPSS (IBM, version 26.0). We utilized Spearman correlational analysis, a nonparametric analysis, to establish correlational relationships between facial and tongue imaging features and dimensional parameters with glucose metabolic, hepatic, renal function, cardiac injury, tumor, thyroid function, and blood cell indicators. We screened the p-coefficient with values below 0.05 as two parameters significantly correlated. A multilinear regression analysis was employed to determine the independent facial and tongue imaging features associated with significant indicators. Multiple receiver operating characteristic curves (ROCs) were drawn to assess the predictive value of significant facial and tongue imaging parameters for metabolic parameters. p < 0.05 was established as the significance threshold for all statistical analyses. Data were presented as the mean ± standard error of the mean (SEM).
Results
The Characteristics of Patients with T2DM
Our study included T2DM patients for facial and tongue feature analyses. Table 1 displays the demographic characteristics, glucose metabolic status, lipid profile, and serum uric acid level.
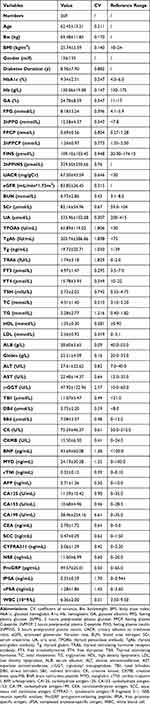 |
Table 1 The Demographic Characteristics of Included T2DM Patients |
The Relationship Between the Facial and Tongue Features and Parameter of Glucose Metabolic State
We analyzed the correlational relationships between the facial and tongue features with dimensional color parameters and glucose metabolic status represented by HbA1c, GA, C-peptide, and insulin levels. The significant results are shown in Tables 2 and 3.
 |
Table 2 The Correlational Relationship Between Significant Facial and Tongue Feature with the Glucose Metabolic Status |
 |
Table 3 The Correlational Relationship Between the Significant Dimensional Parameters of Facial and Tongue Colors and Glucose Metabolic Status |
The Relationship Between the Tongue Color and Parameters of Hepatic and Renal Function
We analyzed the correlational relationships between the facial and tongue features with dimensional color parameters and hepatic and renal function. The significant results are shown in Tables 4 and 5.
 |
Table 4 The Correlational Relationship Between the Significant Facial and Tongue Feature and Critical Hepatic and Renal Function Indicators |
 |
Table 5 The Correlational Relationship Between the Significant Dimensional Facial and Tongue Colors and the Critical Hepatic and Renal Function Indicators |
The Relationship Between the Facial and Tongue Imaging Feature and the Cardiac Injury Markers
We analyzed the correlational relationships between the facial and tongue features with dimensional color parameters and cardiac injury markers. The significant results are shown in Table 6.
 |
Table 6 The Correlational Relationship Between the Significant Facial and Tongue Imaging Feature and Dimensional Color with the Cardiac Injury Markers |
The Relationship Between the Facial and Tongue Imaging and the Tumor Markers in T2DM
We analyzed the correlational relationships between the facial and tongue features with dimensional color parameters and tumor markers. The significant results are shown in Tables 7 and 8.
 |
Table 7 The Correlational Relationship Between the Significant Facial and Tongue Imaging Feature with the Tumor Markers in T2DM |
 |
Table 8 The Correlational Relationship Between the Significant Facial and Tongue Imaging Dimensional Color with the Tumor Marker in T2DM |
The Relationship Between the Facial and Tongue Imaging with the Thyroid Function, Hemoglobin, White Blood Cell, and Palate in T2D
We analyzed the correlational relationships between the facial and tongue features with dimensional color parameters and thyroid function, blood cells. The significant results are shown in Tables 9 and 10.
 |
Table 9 The Correlational Relationship Between the Significant Facial and Tongue Feature and Dimensional Color with the Thyroid Function, Hb, WBC, and Plt |
 |
Table 10 The Correlational Relationship Between the Dimensional Color of Facial and Tongue Imaging and Thyroid Function, Hb, WBC, and Plt |
The Multilinear Regression Analyses Use Parameters of Facial and Tongue Imaging as the Independent Determinators for the Significant Metabolic Indicators
We performed the regression analyses to determine the facial and tongue features with dimensional color parameters to the aforementioned significant metabolic parameters. The significant determinants are displayed in Table 11.
 |
Table 11 The Multilinear Regression Models of Variables to the Significant Metabolic Parameters’ Changes |
The Predictive Value of the Significant Facial and Tongue Imaging Parameters in Glucose Metabolism, Renal Function, Cardiac Injury, Tumor Markers, Thyroid Function and Blood Cells via ROC
Finally, we created the receiver operating characteristic curve (ROC) to assess the predictive value of significant facial and tongue imaging parameters for glucose metabolism (Figure 2), eGFR (Figure 3), cardiac injury (Figure 4), tumor markers (Figure 5), thyroid function and blood cells (Figure 6).
Discussion
TCM is a comprehensive system of diagnosis and treatment that is predicated on an understanding of the internal equilibrium and harmony of the human body.22 The four diagnostic procedures in Traditional Chinese Medicine are inspection, inquiry, sensing and listening, and palpation. Inspection diagnosis, particularly tongue observation, is considered the most fundamental and initial stage of these, as it provides an insight into the patient’s internal state. The tongue is regarded as the external entrance of the heart in Traditional Chinese Medicine (TCM), and it is responsible for the cardiovascular system’s condition. In recent decades, emerging consensus on the tongue pattern as the diagnostic tool in multiple diseases has provoked scientists and clinicians to develop instruments for observing the condition of the tongue in order to assist therapy of both local and systemic diseases,23,24 and even advanced the predictive or diagnostic tools in diabetes with minimal or non-invasive paradigms.11,25
In the present research, we discovered that the metabolic status and related organic laboratory parameters, including hepatic and renal function, cardiac injury markers, tumor markers, thyroid function, and blood cell count, were correlated with the facial, tongue, lip, fur, and other features, as well as dimensional color parameters. This suggests that there is a close correlation between the facial, tongue, and color characteristics and the metabolic status of T2DM patients, as evidenced by the precise analysis. The predictive value of these indicators was evaluated for the laboratory markers that were evaluated in the present study using the ROC assay. Consequently, we could combine these features with other clinical parameters to create a more comprehensive model for predicting the condition and progression of T2DM in patients. This model would be particularly useful for assisting physicians in evaluating the risks of microvascular and macrovascular complications and the therapeutic effects of these patients in future clinical practices.
Additionally, there is an increasing practice of incorporating tongue and facial diagnosis from Traditional Chinese Medicine (TCM) into Western medical practices. Numerous medical professionals, such as physicians, nurses, and therapists, realize the importance of integrating traditional Chinese diagnostic methods into their clinical practices.26,27 This integration enables a more comprehensive approach to patient care by integrating the strengths of both traditional and modern medical systems.28,29 It is imperative to conduct ongoing research on tongue diagnosis in order to enhance its scientific foundation and clinical application. In order to improve the scientific foundation and clinical application of tongue and face diagnosis, it is essential to conduct supplementary research, such as the current study. The efficacy of this diagnostic instrument could be enhanced by conducting research and AI deep learning on the correlations between tongue manifestations and specific biomarkers, pathological changes, and genetic factors.30–32 Furthermore, it is imperative that the next generation of healthcare professionals be provided with a thorough comprehension of this valuable diagnostic technique through educational programs and initiatives that are designed to enhance TCM knowledge and skills, such as tongue observation.
In resource-limited environments where advanced diagnostic instruments are not readily accessible, the integration of tongue and face observations into routine assessments can offer valuable insights into a patient’s overall health status. This is particularly true in clinical settings. Nevertheless, it is imperative to underscore that these observations should be employed as supplementary tools rather than as independent diagnostic criteria.
Limitations
We did not conduct risk comparisons between individuals with T2DM and those who are not. Additionally, future predictive models must incorporate additional tongue and facial features, laboratory data, and imaging data, including CT, coronary arterial imaging, cranial MRI, and MRA, to evaluate the severity and risks of macrovascular complications. It is also necessary to quantitatively evaluate the TCM syndromes in order to identify and reconstruct the relationships with the condition of T2DM in modern medicine practice. This will enable us to provide more precise and personalized treatment.
Conclusion
In conclusion, tongue and face observation is a critical element of clinical diagnosis in TCM, as it assists to inform treatment decisions, prognosis, and diagnosis by providing a glimpse into the patient’s internal state. The integration of modern technologies, such as AI deep learning and digitization, has enhanced its accuracy, reproducibility, and accessibility. Tongue and face diagnosis remain a valuable instrument for the promotion of comprehensive wellness. Although these observations offer a non-invasive, cost-effective approach to obtaining insight into a patient’s health status, they require further scientific investigation to verify their diagnostic accuracy. Modern medical research and traditional wisdom can be combined to create a more comprehensive diagnostic and management strategy, thereby improving our understanding of T2DM.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethical Statement
The study, including sampling, examinations, and access or utilization of the raw data for this study, obtained ethical approval from the Shanghai Pudong Hospital (WZ-010.). Study participants provided informed consent before the study. The guidelines and procedures were outlined in accordance with the Declaration of Helsinki. All data utilized in this investigation were anonymized prior to their utilization.
Acknowledgments
We would like to send our sincere gratitude to all the patients for whom we may actively participate in this study and to all staff, especially the nursing team in the Department of Endocrinology from Shanghai Pudong Hospital, for whom we have made significant contributions to this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by Integrated Traditional Chinese and Western Medicine (YC-2023-0404), Fudan Zhangjiang Clinical Medicine Innovation Fund Project (KP0202118), Fudan Good Practice Program of Teaching and Learning (FD2023A227), Project of Key Medical Discipline of Pudong Hospital of Fudan University (Zdxk2020-11), Project of Key Medical Specialty and Treatment Center of Pudong Hospital of Fudan University (Zdzk2020-24), Integrative Medicine special fund of Shanghai Municipal Health Planning Committee (ZHYY- ZXYJHZX-2-201712), Special Department Fund of the Pudong New Area Health Planning Commission (PWZzk2017-03), Outstanding Leaders Training Program of Pudong Health Bureau of Shanghai (PWR12014-06), Pudong New Area Clinical Plateau Discipline Project (PWYgy-2021-03), the Natural Science Foundation of China (21675034), National Natural Science Foundation of China (81370932), Shanghai Natural Science Foundation (19ZR1447500), Pudong New Area Clinical Characteristic Discipline Project (PWYts2021-11), Pudong New Area Clinical Characteristic Discipline Project (PWYts2021-01), Wenzhou Medical University Education Grant (JG2021197).
Disclosure
The authors declare that there is no potential conflict of interest.
References
1. Chen ZL. Brief history of tongue inspection. Chinese Med J. 1987;100(1):38–44.
2. Dickinson WH. The lumleian lectures on the tongue as an indication of disease. Br Med J. 1888;1(1421):625–632. doi:10.1136/bmj.1.1421.625
3. Edwards M. Put out your tongue! The role of clinical insight in the study of the history of medicine. Med History. 2011;55(3):301–306. doi:10.1017/S0025727300005305
4. Holroyde-Downing N. Tongues on fire: on the origins and transmission of a system of tongue diagnosis. Electronic Thesis Dissert. 2017;2017:1.
5. Lin Y, Bin W, Jiatuo XU, Liping TU. Facial color classification of traditional Chinese medicine inspection based on fusion of facial image features. J Clin Med Pract. 2020;24(14):1–5.
6. Lu LM, Chen X, Xu JT. [Determination methods for inspection of the complexion in traditional Chinese medicine: a review]. Zhong xi yi jie he xue bao. 2009;7(8):701–705. doi:10.3736/jcim20090801
7. Seerangaiyan K, Jüch F, Winkel EG. Tongue coating: its characteristics and role in intra-oral halitosis and general health-a review. J Breath Res. 2018;12(3):034001. doi:10.1088/1752-7163/aaa3a1
8. Chen H, Li Q, Li M, et al. Microbial characteristics across different tongue coating types in a healthy population. J Oral Microbiol. 2021;13(1):1946316. doi:10.1080/20002297.2021.1946316
9. Van Tornout M, Dadamio J, Coucke W, Quirynen M. Tongue coating: related factors. J Clin Periodontol. 2013;40(2):180–185. doi:10.1111/jcpe.12031
10. Abel ED, Gloyn AL, Evans-Molina C, et al. Diabetes mellitus-Progress and opportunities in the evolving epidemic. Cell. 2024;187(15):3789–3820. doi:10.1016/j.cell.2024.06.029
11. Wziątek-Kuczmik D, Świątkowski A, Cholewka A, Mrowiec A, Niedzielska I, Stanek A. Thermal imaging of the tongue surface as a predictive method in the diagnosis of type 2 diabetes mellitus. Sensors. 2024;24(8):2447. doi:10.3390/s24082447
12. Tian Z, Fan Y, Sun X, et al. Predictive value of TCM clinical index for diabetic peripheral neuropathy among the type 2 diabetes mellitus population: a new observation and insight. Heliyon. 2023;9(6):e17339. doi:10.1016/j.heliyon.2023.e17339
13. Deng H, Hu P, Li H, et al. Novel lipid indicators and the risk of type 2 diabetes mellitus among Chinese hypertensive patients: findings from the Guangzhou Heart Study. Cardiovasc Diabetol. 2022;21(1):212. doi:10.1186/s12933-022-01660-z
14. Zhang N, Jiang Z, Li J, Zhang D. Multiple color representation and fusion for diabetes mellitus diagnosis based on back tongue images. Comput Biol Med. 2023;155:106652. doi:10.1016/j.compbiomed.2023.106652
15. Zhang B, Kumar BV, Zhang D. Detecting diabetes mellitus and nonproliferative diabetic retinopathy using tongue color, texture, and geometry features. IEEE Transact Bio-Medical Engin. 2014;61(2):491–501. doi:10.1109/TBME.2013.2282625
16. Li J, Huang J, Jiang T, et al. A multi-step approach for tongue image classification in patients with diabetes. Comput Biol Med. 2022;149:105935. doi:10.1016/j.compbiomed.2022.105935
17. Mathew JK, Sathyalakshmi S. ExpACVO-Hybrid Deep learning: exponential Anti Corona Virus Optimization enabled Hybrid Deep learning for tongue image segmentation towards diabetes mellitus detection. Biomed Signal Process Control. 2023;83:104635. doi:10.1016/j.bspc.2023.104635
18. ElSayed NA, Aleppo G, Bannuru RR. 2. Diagnosis and classification of diabetes: standards of care in Diabetes—2024. Diabetes Care. 2024;47(Suppl 1):S20–s42. doi:10.2337/dc24-S002
19. Shi MJ, Li GZ, Li FF, Xu C. Computerized tongue image segmentation via the double geo-vector flow. ChinMed. 2014;9(1):7. doi:10.1186/1749-8546-9-7
20. Zhao C, Li GZ, Li F, Wang Z, Liu C. Qualitative and quantitative analysis for facial complexion in traditional Chinese medicine. Biomed Res Int. 2014;2014:207589. doi:10.1155/2014/207589
21. Li FF, Zhou R, Li GZ, Zhao RW. Classification of facial diagnosis gloss in Chinese medicine based on different algorithms. Chin J Integr Med. 2016. doi:10.1007/s11655-016-2492-3
22. Tang JL, Liu BY, Ma KW. Traditional Chinese medicine. Lancet. 2008;372(9654):1938–1940. doi:10.1016/S0140-6736(08)61354-9
23. Wziątek-Kuczmik D, Niedzielska I, Mrowiec A, et al. Thermal imaging of tongue surface as a prognostic method in the diagnosis of general diseases-preliminary study. J Clin Med. 2023;12(21). doi:10.3390/jcm12216860
24. Nicolas-Rodriguez E, Pons-Fuster E, López-Jornet P. Diagnostic infrared thermography of the tongue and taste perception in patients with oral lichen planus: case-control study. J Clin Med. 2024;13(2):435. doi:10.3390/jcm13020435
25. Thirunavukkarasu U, Umapathy S, Ravi V, Alahmadi TJ. Tongue image fusion and analysis of thermal and visible images in diabetes mellitus using machine learning techniques. Sci Rep. 2024;14(1):14571. doi:10.1038/s41598-024-64150-0
26. Lu SM, Yang B, Tan ZB, et al. TaoHe ChengQi decoction ameliorates sepsis-induced cardiac dysfunction through anti-ferroptosis via the Nrf2 pathway. Phytomedicine. 2024;129:155597. doi:10.1016/j.phymed.2024.155597
27. Tian D, Chen W, Xu D, et al. A review of traditional Chinese medicine diagnosis using machine learning: inspection, auscultation-olfaction, inquiry, and palpation. Comput Biol Med. 2024;170:108074. doi:10.1016/j.compbiomed.2024.108074
28. Qiao C, Gu C, Wen S, et al. The integrated bioinformatic assay of genetic expression features and analyses of traditional Chinese medicine specific constitution reveal metabolic characteristics and targets in steatosis of nonalcoholic fatty liver disease. Hepatic Med. 2023;15:165–183. doi:10.2147/HMER.S428161
29. Tian X, Wang H, Chen L, Yuan H, Peng C, Wang W. Distinct changes in metabolic profile and sensory quality with different varieties of chrysanthemum (Juhua) Tea Measured by LC-MS-based untargeted metabolomics and electronic tongue. Foods. 2024;13(7):1080. doi:10.3390/foods13071080
30. Yang G, Zhou S, He H, et al. Exploring the ”gene-protein-metabolite” network of coronary heart disease with phlegm and blood stasis syndrome by integrated multi-omics strategy. Front Pharmacol. 2022;13:1022627. doi:10.3389/fphar.2022.1022627
31. Liu M, Wang X, Wu F, et al. Variations of oral microbiome in chronic insomnia patients with different tongue features. Am J Chin Med. 2020;48(4):923–944. doi:10.1142/S0192415X20500445
32. Wang XH, Yang YN, Li YH, et al. Oral bacteriome and mycobiome of patients with idiopathic membranous nephropathy with different tongue coatings treated with a Chinese herbal formula. J Ethnopharmacol. 2024;331:118233. doi:10.1016/j.jep.2024.118233
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.






