Back to Journals » Nature and Science of Sleep » Volume 17
The Relationship Between Education Level and the Prevalence and Medical Behavior of Sleep-Disordered Breathing: A Population-Based Cross-Sectional Study
Authors Zheng G, Ou Q, Shan G , Hu Y, Lao M, Tan J, Feng T, Zhan W, Zhou R, Zhang R, Wu S
Received 30 December 2024
Accepted for publication 7 April 2025
Published 1 May 2025 Volume 2025:17 Pages 749—761
DOI https://doi.org/10.2147/NSS.S511510
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Gaihong Zheng,1 Qiong Ou,2,3 Guangliang Shan,4 Yaoda Hu,4 Miaochan Lao,3 Jiaoying Tan,3 Tong Feng,3 Weixin Zhan,3 Ruohan Zhou,3 Ranxu Zhang,3 Shuhe Wu1
1Guangdong Cardiovascular Institute, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangzhou, Guangdong, 510080, People’s Republic of China; 2Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Guangdong Cardiovascular Institute, Guangzhou, Guangdong, 510080, People’s Republic of China; 3Sleep Center, Department of Respiratory and Critical Care Medicine, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, Guangdong, 510080, People’s Republic of China; 4Department of Epidemiology & Biostatistics, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences/School of Basic Medicine, Peking Union Medical College, Beijing, 100000, People’s Republic of China
Correspondence: Qiong Ou, Guangdong Cardiovascular Institute, Guangdong Provincial People’s Hospital Guangdong Academy of Medical Sciences, No. 106 Zhongshan Road, Yuexiu District, Guangzhou City, Guangdong Province, People’s Republic of China, Tel +86-13609717251, Email [email protected]
Objective: Sleep-disordered breathing (SDB) poses a substantial health burden. It is often marked by patients’ low awareness and poor treatment-seeking. While age, obesity, and genetics are known risk factors, limited studies suggest that socioeconomic status, including educational level, may also affect its prevalence. However, the exact relationship remains unclear. This study aims to explore the link between educational level and SDB prevalence in Chinese community-dwelling individuals and its impact on medical behavior.
Patients and Methods: This cross - sectional study analyzed data from 3,717 residents in the Guangdong cohort. Binary logistic regression was used for multivariable analysis. The product - of - coefficients method was applied to analyze potential mediating effects of education level on SDB through lifestyle and BMI.
Results: The prevalence of SDB was 29.7%, 33%, 29.2%, 30.5% and 31.5% in the illiterate, primary school, junior high school, high school and university or above education groups, respectively, with no significant difference (P=0.580).After further adjustment for age, gender, and marital status, the results showed that education level had no significant impact on the risk of SDB in the population (P> 0.05). Mediation analysis showed that education level had an indirect effect on SDB through BMI and smoking(P< 0.0001). The rates of SDB consultation among the five groups with different education levels were 2.8%, 4.4%, 3.7%, 3.7%, and 3.9%, respectively, with no significant difference (P=0.981).
Conclusion: In Chinese community - dwelling individuals, SDB is present across all education levels. BMI and smoking may influence this. SDB patients overall have low consultation rates. As medical behavior for SDB does not differ much across education levels, disease education and intervention for SDB should target all education groups.
Keywords: educational attainment, factor, consultation rates, mediation
Introduction
Sleep Disordered Breathing (SDB) is a chronic condition that affects people’s health, and in addition to this, it can cause economic and transportation safety losses and hazards.1 Its primary etiology is the recurrent episodes of partial or complete obstruction of the upper airway during sleep, leading to intermittent hypoxia and structural fragmentation of sleep.2 This causes multi-system damage to the individual, for example SDB has been shown to be associated with the development of certain heart diseases, secondary hypertension.2,3
The prevalence of SDB in the overall population is high, ranging from about 10 to 40%. In some older age groups, the prevalence is even as high as 75% or more.4 In the United States, about 25% of adults have SDB.5 The burden of SDB disease is heavy. The primary risk factors for SDB are obesity and advanced age,1,6 and risk factors for SDB also include gender, neck circumference, race, family history, and structural abnormalities of the face and skull.6–9 In addition to these well-known risk factors, SDB has been linked to socioeconomic status in several previous studies.10–14 Numerous chronic diseases can be influenced by socioeconomic status(SES), mainly due to the biological behavioral social model.15 Previous studies have used a single variable or several of them (such as income, occupation, education level) to represent an individual’s SES at the level of society.16,17 In this study, the single variable of “education level” is mainly used to represent an individual’s level of SES. In recent years, many relevant studies have been done on the impact of education level on heart diseases, diabetes, chronic kidney disease and other diseases.15,18–20 However, there is not much research on the relationship between education level and SDB disease, especially whether education level affects the medical behavior of patients with this disease. Education level has become a strong determinant of health disparities, such as coronary heart disease.15 In recent years, low education level has been considered a risk factor for SDB,10–12 however there is controversy. Some studies have suggested that low education level is associated with an increased prevalence of SDB, while others have found no significant association or even a protective effect.13,14,21–23
Therefore, studying the association between education level and SDB diseases in Chinese individuals is the purpose of this study. Although previous studies have provided preliminary exploration, the current study needs to be conducted with a larger sample, community-based population, and a cross-sectional study method. There are almost no studies on the impact of education level on SDB patient seeking behavior. We assume that the incidence of SDB is higher in the low education group than in the high education group, and the visit rate of SDB patients is lower.
Materials and Methods
Research Subject
This study is a cross-sectional study. The participants were selected from the Guangdong cohort of the Chinese Academy of Medical Sciences’ Whole Life Cycle Cohort Study and Information Construction in 2021. The cohort was established using a multi-stage, stratified cluster sampling design to select a representative population. In the initial phase, Guangdong Province was selected, with Shantou City (Chenghai District, Jinping District, Nan’ao County) and Meizhou City (Meijiang District, Jiaoling County) designated as the sampling areas. Subsequently, in the second phase, specific districts within these cities and villages within the counties were chosen. Ultimately, with the backing of the local government, residents from the selected villages and communities were invited to take part in the study.
Participants who were willing to monitor their sleep at home and had a report of sleep monitoring were selected (n=3830). After excluding participants with missing data on education level (n=113), 3717 participants were finally included in the study. Detailed overview of the study process in the study is depicted in Figure 1 of the research report. We used information such as questionnaire results, sleep monitoring results, and physical examination results. The study was approved by the Ethics Committee of Guangdong Provincial People’s Hospital (GDREC2020221H), and all participants provided written informed consent.
 |
Figure 1 Flowchart of participant selection. |
Questionnaire Administration
Baseline data were collected by trained personnel according to standard operating procedures. Unified questionnaires were used throughout the survey. A face-to-face questionnaire was used to collect information on socio-demographics, personal medical histories, lifestyle factors, and sleep-related symptoms and habits. Each questionnaire was checked for completeness and accuracy by an epidemiologist through a face-to-face examination of the subjects.
Measures
Education Level
The highest level of education obtained was questionnaire collected and further categorized into five categories: illiterate, primary school, junior high school, high school, university and above.
Sleep-Disordered Breathing
In this study, a type IV Wearable intelligent sleep monitor (WISM) developed by Chengdu Yunweikang Healthcare Co., Ltd. was used to monitor sleep at night. The WISM is a type IV sleep monitoring device that uses photoelectric sensors to monitor blood oxygen saturation signals. The device is small and easy to wear, which greatly improves the cooperation of the participants. The recommended monitoring site is the thenar region of the palm, and veins, scars, spots and hairy areas should be avoided. We set 7 consecutive hours from 23:00 each night to 6:00 the next morning as the monitoring time. The monitoring parameters mainly included the Oxygen desaturation index (ODI), which was the total number of times that the blood oxygen saturation decreased by ≥3% divided by the effective monitoring time in hours. In a comparative study of type IV WISM and PSG in a sleep center, our research group used a type IV WISM ODI of 7.0 events/hour as the threshold for screening for the presence or absence of SDB, which was misdiagnosed in only 2 cases (0.1%), and it had the best sensitivity, specificity, and accuracy for predicting SDB, with 86%, 91%, and 95%, respectively.24 Therefore, in this study, ODI≥7.0 events/hour was defined as SDB.
Other Factors
Based on standard practices, clinical expertise, and references from published literature, the following variables were selected as covariates in accordance with the aforementioned principles: For sociodemographic factors, these included age, sex, and marital status (categorized as unmarried, married, divorced, or widowed).The lifestyle included smoking, drinking, drinking tea, physical exercise, and occupational labor. Smoking status was categorized as current smokers and current nonsmokers, with the latter including former smokers. Alcohol consumption status was divided into current drinkers and current nondrinkers, with the latter including former drinkers. The status of tea drinking was divided into current tea drinkers and current non-tea drinkers, the latter included former tea drinkers. Physical exercise was classified as rarely or never: less than 1 time/week, occasional exercise: 1–2 times/week, and regular exercise: more than 2 times/week. Occupational labor is divided into light: mainly sitting at the desk, or moving less work, such as office staff, sales staff, housework, etc; Middle: such as motor vehicle driving, electrician installation, lathe operation, assembly line assembly, etc; Heavy: such as manual agricultural labor, steel-making, dance, sports, handling, etc. Other factors included BMI, neck circumference, waist circumference, family monthly income level (divided into less than 3000 yuan, 3000–4999 yuan, 5000–9999 yuan, 10000 yuan or more), history of disease (hypertension, diabetes, dyslipidemia), snoring, insomnia, disease awareness (awareness of snoring as a disease), and health seeking behavior (Visited a doctor for sleep breathing problems such as snoring).
Sample Size Calculation
We assumed that the prevalence of SDB in the general population was 38%,25 the odds ratio (OR) of the education level between university and above and illiterate was about 1.5, with an a of 0.05, 3474 participants would have 80% power to detect this effect size.
Statistical Analysis
Measurement data with normal distribution were represented as mean ± SD, and analysis of variance was used to compare means among three or more independent samples. The count data were expressed as percentage (%), the ordered classified data were analyzed by nonparametric test, and the unordered classified data were analyzed by chi-square test. Binary logistic regression were used for multivariate analysis, and the results were expressed as odds ratio (OR) and 95% confidence interval, respectively. To explore the potential mediating factors that may influence the relationship between education level and SDB, we conducted a mediation analysis using the product of coefficients method. This method allows us to estimate the indirect effect of education level on SDB mediated through lifestyle factors and BMI. Interaction and stratified analyses were conducted according to age (<60 and ≥ 60 years) and sex (male and female). All of the analyses were performed with SPSS25.0 software, the statistical software packages R (http://www.R-project.org, The R Foundation) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc., Boston, MA). P < 0.05 was considered to indicate statistical significance.
Results
Basic Information of the Subjects
The subjects we actually analyzed in this study were 3717, and the details of the subjects are shown in Table 1. Among them, 2573 (69.2%) were in the non-SDB group and 1144 (30.8%) were in the SDB group.
Association Between Educational Level and Prevalence of SDB
The prevalence of SDB was 29.7%, 33.0%, 29.2%, 30.5% and 31.5% in the illiterate, primary school, junior high school, high school and college or above education groups, respectively. Chi-square test showed that there was no significant difference in the prevalence of SDB among the five groups (P=0.580) (Table 1). After adjusting for age, gender and marital status, the results showed that there was no significant difference in the risk of SDB among different education levels (Table 2).
 |
Table 1 Baseline Characteristics of Community Populations Grouped Based on Educational Level |
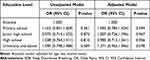 |
Table 2 Correlation Between Education Level and Risk of SDB Prevalence |
Although the overall relationship between education level and SDB was not significant, we explored the potential mediating effects of lifestyle and BMI. The results of the mediation analysis are presented in Table 3. The mediation analysis revealed several key findings. Firstly, regarding BMI, the direct effect of education level on SDB was significant (P=0.004). Moreover, the indirect effect of BMI was also significant (P<0.0001), accounting for −88.81% of the total effect. This suggests that BMI plays a crucial role in the relationship between education level and SDB. Secondly, in terms of smoking, the indirect effect was significant (P<0.0001), accounting for 26.25% of the total effect. This indicates that smoking also has an important impact on this relationship. Lastly, for other mediators including drinking, drinking tea, occupational labor, and physical exercise, no significant indirect effects were observed. In summary, while the overall relationship between education level and SDB was not significant, the mediation analysis highlighted the significant roles of BMI and smoking in this relationship.
 |
Table 3 Mediation Analysis of the Association Between Education Level and the Risk of SDB Prevalence |
Stratified Analysis by Gender and Age
As shown in the Figure 2, the P-values for all interaction terms were not statistically significant (P > 0.1). This indicates that age and gender do not have an interactive effect on the association between education level and SDB in our study.
To further explore the relationship between education level and the risk of SDB across different age groups and sexes, we conducted subgroup analyses, and the results are presented in the forest plot (Figure 2). These findings indicate that there was no significant difference in the risk of SDB among different education levels across different age groups and sexes.
Although the overall association between education level and SDB was not significant across different sexes, we investigated the potential mediating effects of BMI and smoking. The mediation analysis yielded some intriguing insights regarding the mediating roles of BMI and smoking.
In females, the indirect effect of BMI was significant (P<0.0001), accounting for −138% of the total effect. This suggests that BMI plays a crucial role in the relationship between education level and SDB in females. The indirect effect of smoking was not significant (P=0.082) (Table 4).
 |
Table 4 Mediation Analysis of the Association Between Education Level and the Risk of SDB Prevalence in Female Participants |
In males, the indirect effect of smoking was significant (P=0.008), accounting for 18.85% of the total effect. This indicates that smoking plays an important role in the relationship between education level and SDB in males. The indirect effect of BMI was not significant (P=0.928) (Table 5).
 |
Table 5 Mediation Analysis of the Association Between Education Level and the Risk of SDB Prevalence in Male Participants |
Relationship Between Education Level and Medical Behaviors of SDB Patients
A total of 1144 SDB patients were included in this study as subjects. Among them, 44 (3.8%) had the behavior of attending the clinic. The rates of SDB visits in the five groups with different levels of education were 2.8%, 4.4%, 3.7%, 3.7%, 3.9%, and the chi-square test showed that the difference in the rate of visits among the five groups was not significant (P=0.981) (Table 6).
 |
Table 6 Sleep, Disease Awareness, and Health Seeking Behavior in SDB Patients with Different Levels of Education |
Discussion
Studying the association between education level and SDB prevalence was the purpose of this study so that an individual’s likelihood of developing SDB could be predicted based on education level. SDB prevalence among community residents did not appear to be significantly correlated with education level. Individuals’ education level cannot be used to predict the risk of SDB prevalence.
A cross-sectional study of a randomly selected population over the age of 18 years living in an Iranian city with 3529 individuals filling out the Berlin questionnaire to investigate the risk of SDB. Education level was not found to be associated with SDB prevalence.13
A Korean population-based cross-sectional study with 7955 subjects using the Berlin Questionnaire (K-BQ) to assess the risk of SDB found that education level and occupation were not associated with the prevalence of SDB, and high education level was not a protective factor for SDB.14
Another cross-sectional study of 715 hospital staff who completed the Berlin questionnaire in 2012 found education level not associated with SDB prevalence.21
A study in Tehran, Iran, included 4021 participants who filled out the STOP-BANG questionnaire to measure the risk of SDB. The higher education group did not differ from the lower education group in STOP-BANG scores, and education level did not have any significant effect on those at high risk of SDB.22
An observational Swedish study of 10336 men and 2602 women with a first hospital admission for SDB in adults over 35 years of age showed that educational level was not associated with SDB in women.23
Other studies have shown that low SES is not associated with apnea-hypopnea index, indicating that SES is not associated with SDB.26
These studies all showed no effect of education level on SDB prevalence.
The low SES of men may be protective against SDB, according to other studies.27
All of these studies support the idea that education level is not a protective factor for the prevalence of SDB, which is different from our perceptions regarding the effect of education on chronic diseases. In people’s perception, higher levels of education should reduce the prevalence and mortality of some chronic diseases, including hypertension, diabetes, and heart disease. However, this paper observes that education level does not affect the risk of SDB.
While many studies have examined the link between education level and SDB, most have used questionnaires. This study innovatively applies objective diagnostic criteria to assess SDB prevalence, offering a more precise evaluation and deepening our understanding of their relationship.
It should be stressed that although some prior studies used objective diagnostic criteria, they mostly focused on specific groups like hospitalised patients or occupational cohorts. In contrast, this study targets a healthy community - based Chinese population. This difference is crucial as SDB varies among ethnicities, and community residents’ health and lifestyle may differ from those in clinical settings, impacting SDB prevalence and characteristics.
Moreover, this study not only establishes the association between education level and SDB prevalence but also delves into the underlying mechanisms. This exploration informs targeted interventions and policies, contributing to reducing SDB prevalence.
Although the overall relationship between education level and SDB was not significant, the mediation analysis provided valuable insights into the potential mechanisms underlying this relationship. The most notable finding was the significant indirect effect of BMI, which accounted for −88.81% of the total effect. This suggests that BMI may play a crucial role in the relationship between education level and SDB. Similar conclusions were reached in the study by Petrovic D et al.12
The present study also observed that the higher the BMI, the higher the risk of SDB prevalenceD (Table S1). Many previous studies have also yielded similar results.25,28,29 The mechanism of action of which has also been studied more clearly. One, it may be that fat deposition in or around the upper airway increases the collapsibility of the upper airway; two, it may be that it reduces circulatory latency, leading to shorter times and thus more events per hour;30,31 and three, it may be that it increases the arousal threshold.30
Previous studies have found a negative association between socioeconomic status and BMI in high- and middle-income countries,32–35 and our study found similar results (Table S2).The main reason for this social disparity is that people with higher SES are more likely to have more healthy behaviors, including healthier diets, more physical activity, and more hours of sleep, as well as higher awareness, literacy, and easier access to resources for health compared to those with lower SES.34–37
In conclusion, BMI may act as a negative regulatory mediator. Individuals with lower education levels tend to have higher BMIs, which in turn leads to a higher risk of SDB. Therefore, we should encourage universal weight loss, which can better prevent SDB.
Smoking also showed a significant indirect effect, accounting for 26.25% of the total effect. This finding suggests that smoking cessation programs targeted at individuals could be an effective strategy for reducing the risk of SDB.
The results of the stratified analysis by sex revealed that education level was not strongly associated with SDB prevalence in either males or females. However, the mediation analysis highlighted some interesting differences in the potential mediating roles of BMI and smoking between the two sexes.
In females, the significant indirect effect of BMI suggests that women with higher education levels may have lower BMI, which in turn reduces their risk of SDB. This finding is consistent with previous research indicating that women with higher education levels are more likely to have healthier lifestyles and higher levels of health literacy.38 They may be more concerned about their weight and engage in behaviors that help maintain a healthy BMI. In contrast, the indirect effect of BMI was not significant in males. This may be due to differences in lifestyle behaviors and health literacy between men and women. Men with higher education levels may not show the same level of concern about their weight or engage in the same healthy behaviors as women.39
Regarding smoking, the significant indirect effect in males suggests that smoking plays a more important role in the relationship between education level and SDB in men. This finding highlights the need for targeted smoking cessation programs for men.
Many people with SDB usually do not seek medical attention after the onset of symptoms, resulting in a high prevalence of undiagnosed SDB.
The visit behavior of SDB patients is influenced by multiple factors at multiple levels. However, there is a paucity of research on influencing visit behavior.40 The purpose of this study was to investigate the current status of SDB patients’ access to medical care and to determine whether education level influences patient access. In our study, only 3.8% of SDB patients had sought medical attention. This shows that it is very common in China for SDB patients not to seek medical attention. One study has shown that SDB is not considered to be a disease, but rather a normal physiological phenomenon, which may be related to natural aging, or due to some behaviors at bedtime. As long as these behaviors are corrected, SDB can be alleviated or “disappear” without the need to go to the hospital,41 which may be one of the reasons why people do not go to the hospital. And this study showed that education level did not affect SDB patients’ attendance and had little relationship with SDB patients’ attendance. A similar conclusion was reached in a study by Hui Zhang et al.40
In our study, as educational level increased, there were no significant differences in insomnia rates among the five groups. However, higher education levels were associated with increased snoring rates and greater awareness of snoring as a disease, yet no significant differences in medical consultation rates were observed (Table 6).To analyze the possible reasons, first, although the public believes that snoring is a problem, they think that there is no good solution to snoring and it is useless to seek medical treatment; second, some people think that snoring is a shameful thing and do not want other people to know about it, and they do not want to go to the doctor because of snoring.42 Third, although the public realizes that snoring is a problem, they think that snoring will not have serious consequences for them, so they do not go to the doctor. Further analysis of the underlying reasons is mainly due to the general public’s superficial knowledge of SDB and the low level of importance attached to it, which has also been found by many surveys.43,44
Our study finds that disease awareness, comorbid diabetes, and comorbid insomnia act as protective factors regarding the medical behavior of SDB patients (Tables S3 and S4). Further analysis suggests that education is a key motivator for SDB patients to seek medical care. Therefore, the state and society should vigorously pursue programs and measures to disseminate knowledge about SDB.
In exploring whether the allocation of time resources for SDB education can be based on the level of education as an objective factor, this study found that there is no difference in the risk of SDB disease between different levels of education, and that the level of education has little relationship with the consultation behavior of SDB patients, and that the level of education does not affect the consultation behavior of SDB patients. It suggests that the knowledge of SDB should be educated in the whole population, and the same SDB education should be carried out in the population with different education levels. This study also provides some reference value in the design of intervention programs for early identification of people at risk for SDB and increased patient attendance at the clinic.
Strengths of this study: Firstly, relying on a large cohort study, this study is the first large-sample cross-sectional study to examine the association between education level and the prevalence of SDB in a community-based population in China, and explores the potential mechanisms of this association, providing a scientific basis for the prevention of SDB in China. Secondly, there is a problem of low diagnosis rate of SDB. PSG is the gold standard for SDB diagnosis, but it is time-consuming, laborious, and requires expensive equipment, and it is unrealistic to conduct a large-scale population study in a community where it is generally difficult to have multiple pieces of equipment at the same time. In this case, type IV sleep testing equipment shows its unique advantages, which is easy and fast to operate and suitable for large-scale population studies; it is also a way to apply type IV sleep monitoring equipment to large-scale population studies in China, and to accumulate experience for the application of type IV sleep monitoring equipment in population studies. Thirdly, this study incorporated rich demographic characteristics, lifestyle and other indicators.
The current study has some limitations. First, the study population consisted of ethnic Chinese individuals, and the manifestation of SDB can vary among different ethnicities. This may affect the generalizability of our findings to other ethnic populations. We acknowledge that SDB symptoms and their impact on health may differ across ethnic groups due to variations in anatomical features, lifestyle factors, and genetic predispositions. Therefore, the results of this study may not be directly applicable to other ethnic populations. Multi-ethnic studies are needed to explore the cross-cultural applicability of our results and develop more inclusive diagnostic and treatment methods. Second, the potential selection bias caused by voluntary participation in sleep monitoring might influence the results. To minimize this, we used regression adjustment and stratified analysis, but it remains a limitation. We propose that future studies adopt more comprehensive recruitment strategies or advanced statistical methods to better control for this bias. Third, the level of education was collected through a questionnaire and the objectivity could be improved. Fourth, the cross-sectional nature of the study limits our ability to establish causality. Future longitudinal studies are needed to better understand the temporal relationships between these variables. Fifth, while we have adjusted for several key confounding factors, including age, sex, and marital status, and considered lifestyle and BMI as mediators, there may be other unmeasured confounding factors that could influence the relationship between education level and SDB. For example, race, family history and structural abnormalities of the face and skull could also play a role. Future studies should consider including these factors to provide a more comprehensive understanding of the relationship. Sixth, we acknowledge that socioeconomic factors such as income and occupation may significantly influence the relationship between education level and SDB. While our study focuses on education level as a key indicator of SES, we recognize that a more comprehensive assessment of SES, including income and occupation, would provide a deeper understanding of this relationship. Therefore, we emphasize that future studies should incorporate a broader range of SES measures, such as income and occupation, to more robustly explore the association between education level and SDB. This approach will help to clarify the complex interplay of socioeconomic factors and their impact on health outcomes like SDB. Seventh, SDB was diagnosed with a type IV sleep apnea monitoring device, not with a polysomnography device, which led to a decrease in the reliability of the diagnosis of SDB,45,46 but there are now some studies that support the use of a type IV device for screening in a population.23,47 This demonstrates the reliability of our use of type IV devices to screen for SDB in the population. Eighth, the prevalence of SDB is associated with a variety of factors, and the interrelationships and effects of numerous factors have not been adequately demonstrated.
Conclusion
Our study shows that in Chinese community - dwelling individuals, SDB is present across all education levels. BMI and smoking may influence this, with gender differences. These findings provide valuable insights into the potential mechanisms underlying the relationship between education level and SDB and suggest that interventions should be tailored to the specific needs of each sex. SDB patients overall have low consultation rates. As medical behavior for SDB does not differ much across education levels, disease education and intervention for SDB should target all education groups.
Data Sharing Statement
The datasets used or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Ethics Committee of Guangdong Provincial people’s Hospital (GDREC2020221H), obtained the informed consent of all participants. The study was conducted in accordance with the principles outlined in the Declaration of Helsinki.
Author Contributions
All authors made significant contributions to the research, encompassing the study’s conceptualization, design, implementation, data collection, analysis, and interpretation. They participated in manuscript drafting, revising, and critical reviewing. Each author approved the final version for publication, agreed on the submission journal, and takes responsibility for the article’s content. The individual contributions of the authors, based on the CRediT taxonomy, are as follows: Gaihong Zheng: Conceptualization, Formal analysis, Writing - original draft. Qiong Ou: Methodology, Supervision, Project administration, Writing - review & editing. Guangliang Shan: Supervision, Project administration, Writing - review & editing. Yaoda Hu: Supervision, Project administration, Writing-review & editing. Miaochan Lao: Data curation, Validation, Writing - review & editing. Jiaoying Tan: Investigation, Methodology, Writing - review & editing. Tong Feng: Software, Visualization, Writing - review & editing. Weixin Zhan: Data curation, Formal analysis, Writing - review & editing. Ruohan Zhou: Data curation, Formal analysis, Writing - review & editing. Ranxu Zhang: Data curation, Formal analysis, Writing - review & editing. Shuhe Wu: Data curation, Formal analysis, Writing - review & editing.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82170098) and Remote interactive demonstration application of regional data of national health and basic physiological parameters (Grant No. 2022FY100803) to Qiong Ou and CAMS Innovation Fund for Medical Sciences (CIFMS, Grant No. 2020-I2M-2-009) to Guangliang Shan.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lyons MM, Bhatt NY, Pack AI, Magalang UJ. Global burden of sleep-disordered breathing and its implications. Respirology. 2020;25(7):690–702. doi:10.1111/resp.13838
2. Huang B, Liu H, Scherlag BJ, et al. Atrial fibrillation in obstructive sleep apnea: neural mechanisms and emerging therapies. Trends Cardiovasc Med. 2021;31(2):127–132. doi:10.1016/j.tcm.2020.01.006
3. Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;144(3):e56–e67. doi:10.1161/CIR.0000000000000988
4. Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi:10.1016/j.smrv.2016.07.002
5. Gottlieb DJ, Punjabi NM. Diagnosis and management of obstructive sleep apnea: a review. JAMA. 2020;323(14):1389–1400. doi:10.1001/jama.2020.3514
6. Tamanyan K, Walter LM, Davey MJ, Nixon GM, Horne RS, Biggs SN. Risk factors for obstructive sleep apnoea in Australian children. J Paediatr Child Health. 2016;52(5):512–517. doi:10.1111/jpc.13120
7. Bonsignore MR, Saaresranta T, Riha RL. Sex differences in obstructive sleep apnoea. Eur Respir Rev. 2019;28(154):190030. doi:10.1183/16000617.0030-2019
8. Dudley KA, Patel SR. Disparities and genetic risk factors in obstructive sleep apnea. Sleep Med. 2016;18:96–102. doi:10.1016/j.sleep.2015.01.015
9. Rundo JV. Obstructive sleep apnea basics. Cleve Clin J Med. 2019;86(9 Suppl 1):2–9. doi:10.3949/ccjm.86.s1.02
10. Adams RJ, Piantadosi C, Appleton SL, et al. Investigating obstructive sleep apnea: will the health system have the capacity to cope? A population study. Aust Health Rev. 2012;36(4):424–429.
11. Mokarami H, Gharibi V, Kalteh HO, Faraji Kujerdi M, Kazemi R. Multiple environmental and psychosocial work risk factors and sleep disturbances. Aust Int Arch Occup Environ Health. 2020;93(5):623–633. doi:10.1007/s00420-020-01515-8
12. Petrovic D, Haba-Rubio J, Carmeli C, Vollenweider P, Heinzer R, Stringhini S. Stringhini S.Social inequalities in sleep-disordered breathing: evidence from the CoLaus|HypnoLaus study. J Sleep Res. 2019;28(5):e12799. doi:10.1111/jsr.12799
13. Amra B, Farajzadegan Z, Golshan M, Fietze I, Penzel T. Penzel T.Prevalence of sleep apnea-related symptoms in a Persian population. Sleep Breath. 2011;15(3):425–429. doi:10.1007/s11325-010-0353-4
14. Kang K, Seo JG, Seo SH, Park KS, Lee HW. Prevalence and related factors for high-risk of obstructive sleep apnea in a large Korean population: results of a questionnaire-based study. J Clin Neurol. 2014;10(1):42–49. doi:10.3988/jcn.2014.10.1.42
15. Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137(20):2166–2178. doi:10.1161/CIRCULATIONAHA.117.029652
16. Zhang YB, Chen C, Pan XF, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604. doi:10.1136/bmj.n604
17. Petrovic D, de Mestral C, Bochud M, et al. The contribution of health behaviors to socioeconomic inequalities in health: a systematic review. Prev Med. 2018;113:15–31. doi:10.1016/j.ypmed.2018.05.003
18. Zhang J, Chen Z, Pärna K, et al. Mediators of the association between educational attainment and type 2 diabetes mellitus: a two-step multivariable Mendelian randomisation study. Diabetologia. 2022;65(8):1364–1374. doi:10.1007/s00125-022-05705-6
19. Liang J, Cai H, Liang G, et al. Educational attainment protects against type 2 diabetes independently of cognitive performance: a Mendelian randomization study. Acta Diabetol. 2021;58(5):567–574. doi:10.1007/s00592-020-01647-w
20. Winitzki D, Zacharias HU, Nadal J, et al. Educational attainment is associated with kidney and cardiovascular outcomes in the German CKD (GCKD) Cohort. Kidney Int Rep. 2022;7(5):1004–1015. doi:10.1016/j.ekir.2022.02.001
21. Seyedmehdi SM, Rahnama N, Yazdanparast T, Jamaati H, Attarchi M, Adimi Naghan P. Hassani S.Prevalence of snoring and the risk of sleep apnea in hospital staff. Work. 2016;55(4):765–772. doi:10.3233/WOR-162460
22. Foroughi M, Malekmohammad M, Sharafkhaneh A, Emami H, Adimi P, Khoundabi B. Prevalence of obstructive sleep apnea in a high-risk population using the stop-bang questionnaire in Tehran, Iran. Tanaffos. 2017;16(3):217–224.
23. Li X, Sundquist K, Sundquist J. Socioeconomic status and occupation as risk factors for obstructive sleep apnea in Sweden: a population-based study. Sleep Med. 2008;9(2):129–136. doi:10.1016/j.sleep.2007.02.003
24. Xu Y, Ou Q, Cheng Y, et al. Comparative study of a wearable intelligent sleep monitor and polysomnography monitor for the diagnosis of obstructive sleep apnea. Sleep Breath. 2023;27(1):205–212. doi:10.1007/s11325-022-02599-x
25. Tufik S, Santos-Silva R, Taddei JA, Bittencourt LR. Obstructive sleep apnea syndrome in the Sao Paulo epidemiologic sleep study. Sleep Med. 2010;11(5):441–446. doi:10.1016/j.sleep.2009.10.005
26. Reddy EV, Kadhiravan T, Mishra HK, et al. Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: a community-based study. Sleep Med. 2009;10(10(8):p.913–8):913–918. doi:10.1016/j.sleep.2008.08.011
27. Rezaie L, Maazinezhad S, Fogelberg DJ, et al. Compared to individuals with mild to moderate obstructive sleep apnea (OSA), individuals with severe OSA had higher BMI and respiratory-disturbance scores. Life. 2021;11(5):368. doi:10.3390/life11050368
28. Li Y, Miao Y, Tan J, Zhang Q. Association of modifiable risk factors with obstructive sleep apnea: a Mendelian randomization study. Aging. 2023;15(23):14039–14065. doi:10.18632/aging.205288
29. de Araujo Dantas AB, Gonçalves FM, Martins AA, et al. Worldwide prevalence and associated risk factors of obstructive sleep apnea: a meta-analysis and meta-regression. Sleep Breath. 2023;27(6):2083–2109. doi:10.1007/s11325-023-02810-7
30. Nokes B, Orr JE, White S, et al. Effect of obesity on sleep apnea pathogenesis differs in women versus men: multiple mediation analyses in the retrospective SNOOzzzE cohort. J Appl Physiol. 2024;136(6):1516–1525. doi:10.1152/japplphysiol.00925.2023
31. Leppänen T, Kulkas A, Mervaala E, Töyräs J. Increase in body mass index decreases duration of apneas and hypopneas in obstructive sleep apnea. Respir Care. 2019;64(1):77–84. doi:10.4187/respcare.06297
32. Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev. 2012;13(11):1067–1079. doi:10.1111/j.1467-789X.2012.01017.x
33. Vazquez CE, Cubbin C. Socioeconomic status and childhood obesity: a review of literature from the past decade to inform intervention research. Curr Obes Rep. 2020;9(4):562–570. doi:10.1007/s13679-020-00400-2
34. Wang Y, Lim H. The global childhood obesity epidemic and the association between socio-economic status and childhood obesity. Int Rev Psychiatry. 2012;24(3):176–188. doi:10.3109/09540261.2012.688195
35. Pampel FC, Denney JT, Krueger PM. Obesity SES, and economic development: a test of the reversal hypothesis. Soc Sci Med. 2012;74(7):1073–1081. doi:10.1016/j.socscimed.2011.12.028
36. Krueger PM, Reither EN. Mind the gap: race/ethnic and socioeconomic disparities in obesity. Curr Diab Rep. 2015;15(11):95. doi:10.1007/s11892-015-0666-6
37. Pigeyre M, Rousseaux J, Trouiller P, et al. How obesity relates to socio-economic status: identification of eating behavior mediators. Int J Obes Lond. 2016;40(11):1794–1801. doi:10.1038/ijo.2016.109
38. Newton S, Braithwaite D, Akinyemiju TF. Socio-economic status over the life course and obesity: systematic review and meta-analysis. PLoS One. 2017;12(5):e0177151. doi:10.1371/journal.pone.0177151
39. Stringhini S, Spencer B, Marques-Vidal P, et al. Age and gender differences in the social patterning of cardiovascular risk factors in Switzerland: the CoLaus study. PLoS One. 2012;7(11):e49443. doi:10.1371/journal.pone.0049443
40. Zhang H, Liang C, Zhang X, et al. Factors influencing patient delay in individuals with obstructive sleep apnoea: a study based on an integrated model. Ann Med. 2022;54(1):2828–2840. doi:10.1080/07853890.2022.2132417
41. Shaw R, McKenzie S, Taylor T, et al. Beliefs and attitudes toward obstructive sleep apnea evaluation and treatment among blacks. J Natl Med Assoc. 2012;104(11–12):510–519. doi:10.1016/s0027-9684(15)30217-0
42. Williams SJ, Seale C, Boden S, et al. Medicalization and beyond: the social construction of insomnia and snoring in the news. Health. 2008;12(2):251–268. doi:10.1177/1363459307086846
43. Eseverri MV, Noya Pdel V, Mac Lean B, Cipriani SA, Remedi Adel R. Ronquido primario y síntomas asociados a apneas obstructivas de la infancia: prevalencia, pesquisa y actitud familiar [Primary snoring and obstructive apnea of childhood associated symptoms: prevalence, screening and familiar attitude]. Arch Argent Pediatr. 2008;106(3):231–235. doi:10.1590/S0325-00752008000300008
44. Grivell N, Haycock J, Redman A, et al. Assessment, referral and management of obstructive sleep apnea by Australian general practitioners: a qualitative ana-lysis. BMC Health Serv Res. 2021;21(1):1248. doi:10.1186/s12913-021-07274-7
45. Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of sleep medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. doi:10.5664/jcsm.6506
46. Abrahamyan L, Sahakyan Y, Chung S, et al.Diagnostic accuracy of level IV portable sleep monitors versus polysomnography for obstructive sleep apnea: a systematic review and meta-analysis. Sleep Breath. 2018;22(3):593–611. doi:10.1007/s11325-017-1615-1
47. Pei G, Ou Q, Shan G, et al. Screening practices for obstructive sleep apnea in healthy community people: a Chinese community-based study. J Thorac Dis. 2023;15(9):5134–5149. doi:10.21037/jtd-22-1538
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


