Back to Journals » Patient Related Outcome Measures » Volume 15
The Role of Medical Helicopter and Ground Medical Crews in Polytrauma Management: An Evaluative Perspective
Authors Anghele M, Marina V , Anghele AD, Moscu CA, Dragomir L
Received 27 August 2024
Accepted for publication 21 November 2024
Published 24 December 2024 Volume 2024:15 Pages 315—328
DOI https://doi.org/10.2147/PROM.S486167
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Mihaela Anghele,1 Virginia Marina,2 Aurelian-Dumitrache Anghele,3 Cosmina-Alina Moscu,3 Liliana Dragomir1
1Clinical-Medical Department, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University, Galati, Romania; 2Medical Department of Occupational Health, Faculty of Medicine and Pharmacy, “Dunărea de Jos” University, Galati, Romania; 3Doctoral School, Dunărea de Jos” University, Galati, Romania
Correspondence: Virginia Marina, Email [email protected]
Introduction: Polytrauma remains a major global health challenge, with rapid intervention being critical for survival, especially during the “Golden Hour”. This study examines the impact of Helicopter Emergency Medical Services (HEMS) on procedural care during the transfer of polytraumatized patients to urban hospitals in Romania.
Methods: A retrospective cohort study was conducted at the County Emergency Hospital “St. Ap. Andrei” in Galați, covering January 2020 to October 2021. The study analyzed data from 89 patients transported by the Romania’s Mobile Emergency Service for Resuscitation and Extrication (SMURD) Galați air unit. Key parameters included demographics, injury mechanism, vital statistics, and prehospital interventions. Statistical analyses were performed using SPSS, with significance set at p < 0.05.
Results: Out of 89 patients (mean age 21.6 years, 80.3% male), trauma causes were primarily traffic accidents (34.8%) and falls (33.7%). A Glasgow Coma Scale (GCS) score ≤ 8 was noted in 28.1% of cases, with head trauma observed in 51.6% of patients. HEMS interventions frequently involved oxygen therapy (89.5%) and patient stabilization maneuvers, leading to a mortality rate of 6.7%. Notably, helicopter transport enabled efficient transfer and improved survival outcomes in this cohort.
Discussion: HEMS demonstrated benefits in reducing intervention times and enhancing prehospital care quality for polytrauma patients, especially in hard-to-reach areas. The study aligns with global data on HEMS’s role in trauma systems, underlining the importance of multidisciplinary collaboration and rapid transport.
Conclusion: HEMS plays a crucial role in improving survival rates for severely injured patients through timely interventions and specialized care. Further research comparing HEMS and ground services could refine trauma management protocols in similar settings.
Keywords: severely injured, air rescue crew, polytrauma management, multidisciplinary approach, patient transport
Introduction
Trauma remains a global health concern, contributing to over 8% of annual deaths worldwide (GBD 2019).1 Young people are especially vulnerable, as road injuries, self-harm, and violence rank among the top causes of mortality and disability.2 Rapid intervention within the critical “Golden Hour” is essential for improving trauma outcomes, underscoring the need for timely, efficient transport to specialized care facilities.3
The primary goal of trauma transport is to minimize morbidity and mortality by transferring patients quickly to the appropriate hospital level. Transport methods vary by health system, ranging from ground ambulances to air services like helicopters, each demanding robust infrastructure, reliable communications, and well-equipped vehicles.4,5 However, transporting critical patients (injury severity score > 16) carries risks and requires a trained medical team skilled in advanced life support.5
Air transport, although costly and resource-intensive, offers key advantages: reduced time to hospital, high-quality prehospital care, and access to remote trauma centers.4–6 Nevertheless, the impact of helicopter transport on survival remains unclear, influenced by factors such as injury severity, transport protocols, and access to trauma centers.5–7 Patient movement during transport can cause hemodynamic, respiratory, and neurological issues, making continuous monitoring of vital signs essential, particularly for severely injured patients with thoracic, abdominal, or extremity injuries.3–5
Romania’s Mobile Emergency Service for Resuscitation and Extrication (SMURD) has been conducting helicopter medical interventions since 2003, aiming to swiftly rescue critically injured patients. Regulated under Government Ordinance no. 126/20038 and the Methodological Norms approved by the Order of the Ministry of Administration and Interior and the Minister of Health no. 277/777/2004,9 this public service operates Eurocopter EC 135 helicopters supplied by the Ministry of Health and managed by the Special Aviation Unit of the Ministry of Internal Affairs. Although SMURD provides essential air transport services, comprehensive guidelines to determine the most suitable mode of transport and to avoid over-triage for interclinic transfers are still lacking.10
The aim of this study is to evaluate prehospital intervention times and systematically analyze the maneuvers used to stabilize and diagnose polytrauma patients, based on a retrospective cohort study of SMURD interventions in Galați County. Through this analysis, the research seeks to provide a detailed understanding of the variables that may influence the management of polytrauma patients in the prehospital context, including interventions by air and ground teams. A case study has been selected for illustrative purposes.
Materials and Methods
The study was conducted at the County Emergency Hospital “St. Ap. Andrei” in Galaţi between January 2020 and October 2021, involving 89 patients including children, teenagers, and young adults up to 45 years of age. The study database consisted of data collected through observation sheets of polytrauma patients who required intervention from the SMURD Galaţi air unit for transport to the nearest hospital/trauma center for further investigations and specialized treatment. Data regarding vital parameters, diagnostics, mechanism of injury, and primary evaluation and patient stabilization steps were considered study variables.
Statistical analysis was performed using SPSS v26 software and Microsoft Excel version 2019. Significance was considered at the P < 0.05 level with a confidence interval of 95%. Continuous values were presented as mean and standard deviation, while categorical variables were presented as percentages. The study was conducted in accordance with the Helsinki Declaration of the World Medical Association, following a protocol approved by the local Bioethics committee and obtaining approval from the hospital administration.
Results
The distribution of patients within the group was evaluated based on socio-demographic characteristics such as sex, living area, and age. Following frequency analysis conducted on these variables, a higher prevalence was found among males (80.3%, 61 patients), while females represented only 19.7% (15 patients). In terms of living area, a nearly equal distribution between rural and urban areas was observed, with a slightly higher prevalence in rural areas (57.9%, 44 patients), compared to urban areas (42.1%, 32 patients) (Table 1).
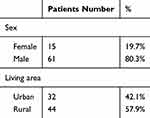 |
Table 1 Prevalence of Polytrauma Patients Within the Group by Gender and Living Area |
The average age of the cohort was 21.6 years, with a standard deviation of 22.089. The minimum age within the group was 0 (representing infants), and the maximum was 45 years. The skewness index had a value of 0.157, indicating that the distribution of the group was positively skewed. This can also be seen in the histogram, with the peak subtly shifted to the left. However, the distribution within this group closely resembled a Gaussian normal distribution (see Figure 1).
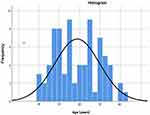 |
Figure 1 Histogram for depicting the age distribution of the group. |
The etiology of trauma was related to traffic-related causes in 31 (34.8%) cases, falls in 30 (33.7%), and aggressions in 6 (6.7%) patients. The prevalence of other identified trauma-producing mechanisms is indicated in Figure 2.
 |
Figure 2 The prevalence of other identified trauma-producing mechanisms. |
Table 2 summarizes descriptive statistics for vital parameters and other measured parameters, such as GCS score, blood pressure, oxygen saturation, pulse rate, respiratory rate, blood sugar, and temperature. A total of 25 patients, representing 28.1%, had a GCS value of 8 or less.
 |
Table 2 Descriptive Statistics of Study Group by Key Parameters |
Descriptive statistics were calculated for the key parameters selected within the study group.
In terms of the patients’ diagnoses, with a few exceptions (2 cases of hanging, psychomotor agitation due to ethanol abuse, and 2 cases of drowning), the patients in the study group presented complex polytrauma affecting multiple body regions: cranial and craniofacial traumas, thoracic traumas, abdominal and pelvic, spinal injuries, limb traumas (Figure 3).
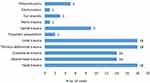 |
Figure 3 The distribution of the types of trauma within the study group. |
The presence of traumatic head injuries was higher among patients in the group (51.6% of cases). Data analysis indicates that most patients presented with cranial traumas of varying severity (36%) or craniofacial trauma (15.7%), often associated with thoraco-abdominal or limb injuries. Thoraco-abdominal trauma ranks second in the studied group (20.2% of total cases), mostly associated with limb trauma. Spinal trauma was diagnoses in 10.1% of cases.
Among the most frequent complications of polytrauma within the patients in the study group were: coma with GCS<8 (14.6% of cases), cardiorespiratory arrest (11.2%), hypovolemic hemorrhagic or traumatic shock, hematoma, hemopneumothorax, burns, spleen or kidney traumatic injury, respiratory distress syndrome (Figure 4). Ethanol intoxication was identified in 12 cases (13.4%). Six patients (6.7%) died during the intervention.
 |
Figure 4 The frequency of polytrauma complications in the study group. |
The specific characteristics of the interventions carried out in pre-hospital care were evaluated to identify the types of missions and specific trauma management approaches, such as extrication, immobilization, and stabilization of the patient. The group’s most frequent types of interventions were primary (89.5%, 68 patients). One search and rescue mission was recorded, and three (3.9%) extrication missions were recorded. Table 3 displays a summary of the mission types and on-scene treatment.
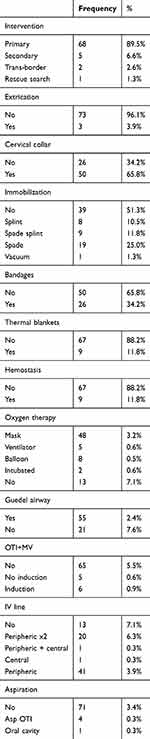 |
Table 3 Mission Types and Specific Management and Stabilization Maneuvers for Polytrauma Patients |
Stabilizing the patient involves a series of complex interventions aimed at increasing the patient’s stability for transport and reducing the immediate risk of death. Pre-hospital management of polytrauma includes immobilizing and stabilizing the patient before and during transport to a specialized hospital unit.11 Cervical immobilization is required in cases of cranio-cerebral trauma to preserve the integrity of the spinal cord. In this study group, cervical immobilization using a cervical collar was utilized for the majority of 50 subjects (65.8%,), while 26 subjects (34.2%) did not require this type of immobilization.
Within this study group, 51.3% of subjects did not require complete immobilization. Splints, primarily used for complex limb injuries, were employed in 10.5% of cases. Scoop stretcher immobilization was applied in 36.8% (n=28) of cases, while a vacuum splint was used in only one case (1.3%).
Bandages were applied in 34.5% of cases due to hemorrhagic wounds, with complex hemostasis necessary in only 11.8% of cases. Considering the complex pathophysiology of trauma, thermal risk is a critical factor. A spontaneous drop in core body temperature post-trauma is correlated with poor prognosis.12 Consequently, thermal blankets were used for all patients with massive hemorrhages.
Oxygen therapy was administered as a first-line treatment for signs of hypoxia, using either non-invasive methods (mask or AMBU bag) or invasive methods [orotracheal intubation (OTI), mechanical ventilation (MV)]. An oxygen mask was used for most subjects (63.2%); eight subjects (10.5%) were ventilated using an AMBU bag, and 6.6% required mechanical ventilation. Two subjects (2.6%) required orotracheal intubation. Additionally, 14.5% required both OTI and MV, with 6.6% not requiring induction, while 7.9% required drug induction. Aspiration through the intubation tube was necessary for 5.3% of subjects.
Intravenous access for medication administration was critical for patient stabilization. In this study group, 13 subjects (17.1%) had an intravenous line inserted. Most subjects (53.9%) had a peripheral line, while two were inserted for 26.3%. One patient (1.3%) had a central line inserted, and one had both central intravenous and peripheral lines.
Intervention times for polytrauma cases were also evaluated. Four distinct times were identified, each representing a specific phase of the intervention: T1 – time from the call to patient pickup; T2 – transport time until patient handover to the specialized ground crew; T3 – time from patient handover to refueling (optional based on intervention distances); and T4 – return time to the Galaţi Aeromedical Operation Point.
The average intervention time for T1 was 24.30 minutes (standard deviation 11.66), with a minimum of 6 minutes and a maximum of 70 minutes. The average intervention time for T2 was 23.09 minutes (standard deviation 9.8), with a minimum of 5 minutes and a maximum of 58 minutes.
Discussions
In this study, we found that primary interventions were frequently used as the initial response for events causing polytrauma. The average response time was approximately 24 minutes from the initial call to patient pickup, and the transport and handover to the ground emergency team had a similar average duration. This highlights the efficiency of helicopter services; especially over medium and long distances where rapid transport is essential. Literature indicates that the total response time for helicopter emergency medical services (HEMS), from the initial call to hospital arrival, varies between 20 and 30 minutes for distances up to 80 km and between 30 and 60 minutes for longer distances.13
Managing polytraumatized patients is one of the greatest challenges in trauma care, and optimizing these interventions remains a major goal in clinical research. Trauma-related deaths are most common within the first hour after an accident, also known as the “golden hour of trauma.” Therefore, effective interventions during this period are essential for survival and recovery.13,14 In air ambulance interventions, the treatments applied on-site and during transport must focus on life-saving procedures that do not delay rapid transfer to specialized treatment centers.13
Our study showed that the emergency helicopter responded to numerous patients with severe polytrauma, with injuries to the head, chest, limbs, spine, abdomen, or pelvis. The average Glasgow Coma Scale (GCS) score of patients was 11, with a minimum of 3 and a maximum of 15; in 46 cases, the GCS score was below 8 (51.6%), indicating severe brain injuries. Recorded complications included hemorrhagic shock, hypovolemic shock, pneumothorax, open fractures, traumatic amputations, respiratory failure, cardiac arrest, and coma—each presenting significant threats to patients’ lives.
Rapid interventions and effective collaboration with ground emergency teams saved lives in most cases. Out of a total of 89 patients, six deaths were recorded (6.7%). The air medical team conducted primary evaluations, administered oxygen (in 89.5% of cases), controlled bleeding, immobilized fractures, performed cardiac massage (in 12 cases of cardiac arrest, representing 13.5% of patients), and provided thermal protection. Central or peripheral venous lines were also placed, essential for the rapid administration of fluids and medications.
Consistent with recent literature, our study highlights the benefits of air medical transport for critically injured patients, including advanced intervention teams, fast transport times, and access to remote areas. A large study in the US involving 258,827 trauma patients transported either by helicopter (16%) or ground ambulance (84%) showed a 22% reduction in mortality for those transported by helicopter, independent of the patient’s age or trauma mechanism.15 Another recent study, based on data from the Trauma Register DGU, Germany (2013–2017), indicated a 50% reduction in adjusted mortality risk for pediatric polytrauma patients transported by helicopter.10
In recent years, the number of specialized hospitals—including trauma centers, spinal care, pediatric care, burn treatment, stroke management, cardiology, and advanced resuscitation services—has increased in our country.16
Rapid transport to these facilities is essential for optimal care. The following case study illustrates the critical role of air medical services, ground medical teams, and multidisciplinary hospital teams in the survival and management of severe polytrauma cases.
We included the case study with the intention of providing a concrete example of how HEMS (Helicopter Emergency Medical Services) can facilitate rapid and coordinated pre-hospital care in cases of severe trauma. The case study highlights the specifics of air emergency interventions and emphasizes HEMS’s role in optimizing medical response by ensuring quick access to patients in hard-to-reach areas and efficient transport to specialized trauma centers. This section is intended to complement the statistical data in the study with a practical description, underlining the utility of HEMS in a real context.
Case Presentation
We present the case of a 44-year-old man who survived a railway accident due to the prompt intervention of the air rescue team’s medical crew from the Galaţi Aeromedical Operation Point in Romania and the comprehensive multidisciplinary management provided upon his admission to the Intensive Care Unit. The patient was the driver of a car struck by a train near a rural village, 85 km from the nearest multidisciplinary hospital. The helicopter emergency medical service was alerted, departing and arriving at the scene within 17 minutes. Concurrently, a ground paramedic crew from the local territory arrived at the accident scene (Figures 5 and 6). The paramedics identified the patient as a victim of a road-rail collision.
 |
Figure 5 The intervention of ground medical crews played a crucial role in managing the polytrauma of the patient. |
 |
Figure 6 The intervention of medical helicopter crew played a crucial role in managing the polytrauma of the patient. |
The patient was conscious but agitated and confused, with a Glasgow Coma Scale (GCS) score 12. He had normal, reactive pupils bilaterally, periorbital and right palpebral hematomas, and bilateral anterior epistaxis. His airway was open and clear, respirations were normal at a rate of 16 breaths per minute, and he had a present and rhythmic peripheral pulse. Cardiac assessment showed a sinus rhythm with a narrow QRS complex, ventricular rate of 125 beats per minute, rhythmic heart sounds, and a blood pressure of 120/70 mmHg. There were no focal neurological deficits observed. Vesicular breath sounds were present bilaterally, though diminished in the right pulmonary area, with an oxygen saturation of 75%. The patient’s skin was warm, dry, and cyanotic, and his abdomen was normal. The Revised Trauma Score was 11.
After the primary assessment, advanced airway management was performed through orotracheal intubation with pharmacological induction using atropine, midazolam, etomidate, fentanyl, succinylcholine (Lysthenon), and rocuronium (Esmeron), followed by controlled mechanical ventilation. Cervical spine immobilization was achieved using a cervical collar, and total spinal immobilization was performed using a rigid spine stretcher with lateral head stabilizers and front as well as chin restraints. Peripheral venous access was established with two 14-gauge lines for administering anti-inflammatory corticosteroids (methylprednisolone sodium succinate) and maintenance of anesthesia (etomidate, midazolam, rocuronium).
The patient arrived at the hospital within 90 minutes and was received by a multidisciplinary team. Upon admission to the Emergency Department, the patient had a GCS score of 3 due to a pharmacologically induced coma, was mechanically ventilated, and hemodynamically stable. Imaging investigations were promptly performed, revealing the following:
A cervical spine CT scan showed a right transverse process of C2 fracture with transverse involvement. The cervical lines were normally aligned. Right lateral cervical subcutaneous emphysema and a small pneumorrhachis.
A Non-enhanced head CT scan (the gold standard for investigating head trauma).17 (Figures 7–11) revealed a right frontoparietal epicranial hematoma with an underlying fracture. Right frontoparietal biconvex hyperdense extra-axial well-defined collection-epidural hematoma (11 mm thickness).18 Bilateral cerebral subarachnoid hemorrhage; supra- and infra-tentorial pneumocephalus. No midline shift and no herniation were present. Right lateral and medial orbital wall fractures. Fractures of the anterior and posterior walls of the right frontal sinus, with hemosinus. Bilateral maxillary and sphenoid sinus fractures with hemosinus. Right temporal and zygomatic processes of the temporal bone fractures. The hyperdense content of the left mastoid cells is indicative of a left mastoid fracture.
 |
Figure 9 Non-enhanced head CT scan. Axial brain window. Bilateral linear hyper densities between parietal gyri-subarachnoid hemorrhage (black arrowheads). Pneumocephalus (black solid arrow). |
 |
Figure 10 Non-enhanced head CT scan. Axial brain window. Hyperdense content of the right maxillary sinus-hemosinus (black solid arrow). |
 |
Figure 11 Chest CT scan-axial lung window. Deep lateral-thoracic emphysema (black solid arrow). Right pneumothorax (black arrowheads). |
Contrast-enhanced CT scan of the chest, abdomen, and pelvis revealed the following (Figures 11 and 12):
- Right hemopneumothorax (15 mm thick hemothorax). Partially collapsed right lung with right lower lobe passive atelectasis. Small ground-glass opacities in the right upper lobe and left lower lobe. Hyperdense non-enhancing collection in the anterosuperior mediastinum with air inclusion suggests a hematoma. Deep lateral-thoracic emphysema. Manubrial fracture and fractures of the right third, fourth, and fifth lateral costal arches.
- No traumatic lesions of the liver, spleen, pancreas, or kidneys. There were no free intraperitoneal fluid or fractures.
 |
Figure 12 Chest CT scan-axial lung window. Partially collapsed right lung with right lower lobe passive atelectasis (solid black arrow). Small anterior pneumomediastinum (black arrowhead). |
The right pneumothorax was surgically drained in the Emergency Department, with radiological confirmation of right lung re-expansion. After stabilization, the patient was admitted to the Neurosurgery Intensive Care Unit.
Due to the active bleeding described after the initial imaging, a 24-hour follow-up non-enhanced head CT scan was performed. The right frontotemporal epidural hematoma (10 mm thickness in the frontal area and 8 mm in the anterior temporal region) did not reach the size for which surgery needed to be performed. Bilateral temporal-parietal subarachnoid hemorrhage. No midline shift and no herniation were present. There were no other notable changes compared to the previous CT scan.
After receiving conservative treatment for 20 days, the patient’s condition progressively improved, restoring consciousness and pulmonary functions to physiological limits.
The goals of pharmacotherapy are to reduce morbidity and prevent complications.19
The behavior of patients who try to hide their conditions can represent an important lesson for clinical practice.20
People with polytrauma must receive ongoing assistance and care to handle the long-term repercussions of their injuries on their mental health.21
Instability or neuroticism, as a personality feature, amplifies the occurrence of burnout syndrome.22
The increase in burnout among medical staff of Emergency Department is directly proportional to the nature of the work.23
Neurological examination showed no abnormalities and psychiatric assessment did not reveal any cognitive disorders. As a result, the patient was discharged.
Conclusions
This study affirms the beneficial role of helicopter emergency medical services (HEMS) in the pre-hospital management of polytrauma patients, highlighting the importance of high-level treatment protocols and the expertise of the rescue team in enhancing patient survival. While we do not claim that HEMS saves more lives than other transport methods, our findings emphasize its effectiveness in rapid response and specialized care, especially in scenarios where time and access are critical factors.
The successful pre-hospital management in our study was largely based on patient stabilization and immobilization, involving specific interventions to prevent hypoxia, hemorrhagic shock, and hypothermia. Equipment such as cervical collars, vacuum splints, and isothermal foil played an essential role in this process, while both air and ground teams collaborated to deliver timely and coordinated care, which positively influenced patient outcomes.
Moreover, this study underscores the need for a collaborative approach in trauma care, involving advanced airway management, imaging, surgical interventions, and intensive care. Imaging, in particular, proved critical in complex trauma cases, providing essential insights that guide diagnosis, clinical decisions, and ongoing monitoring.
Our study’s findings reveal that early intervention, coordinated transport, and a multidisciplinary approach are critical in improving outcomes for trauma patients. However, further research comparing HEMS outcomes with other transport methods and exploring specific factors contributing to its effectiveness could provide additional insights and refine pre-hospital care strategies for trauma patients.
Abbreviation
CT, computer tomography; GCS, Glasgow Coma Scale; HEMS, Helicopter Emergency Medical Services; No, number; MV, mechanical ventilation; OTI, orotracheal intubation; SMURD, Romania’s Mobile Emergency Service for Resuscitation and Extrication.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of Clinical Emergency Hospital, Galati, Romania. (Project identification code: 974/04/2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Informed consent was obtained from the case subject for publication of the case details and accompanying images. The Hospital Ethics Committee approved this study. In addition, consent was obtained from the study participants, and for those that were minors, legal guardians provided consent. Subsequent research was carried out under the conditions agreed upon in this informed consent, which was drawn up in accordance with the current legislation of the World Health Organization and the European Union on research on human subjects in the field of medicine, considering the latest version of the Declaration of Human Rights in Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas, took part in drafting, revising, or critically reviewing the article, gave final approval of the version to be published, agreed on the journal to which the article has been submitted, and agreed to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors declare that they have no competing interests.
References
1. GBD 2019. Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222. doi:10.1016/S0140-6736(20)30925-9
2. Murray CJ. Findings from the Global Burden of Disease Study 2021. Lancet. 2024;403(10440):2259–2262. doi:10.1016/S0140-6736(24)00769-4
3. Michaels D, Pham H, Puckett Y, Dissanaike S. Helicopter versus ground ambulance: review of national database for outcomes in survival in transferred trauma patients in the USA. Trauma Surg Acute Care Open. 2019;4(1):e000211. doi:10.1136/tsaco-2018-000211
4. Spoelder EJ, Slagt C, Scheffer GJ, van Geffen GJ. Transport of the patient with trauma: a narrative review. Anaesthesia. 2022;77(11):1281–1287. doi:10.1111/anae.15812
5. Khan SM, Lance MD, Elobied MAK. Transport of critically Ill patients – a review of early interventions, protocols, and recommendations. Int J Health Sci Res. 2021;11(4):133–143. doi:10.52403/ijhsr.20210418
6. Chesters A, Grieve PH, Hodgetts TJ. A 26-year comparative review of United Kingdom helicopter emergency medical services crashes and serious incidents. J Trauma Acute Care Surg. 2014;76(4):1055–1060. doi:10.1097/TA.0000000000000170
7. Galvagno SM Jr, Sikorski R, Hirshon JM, et al. Helicopter emergency medical services for adults with major trauma. Cochrane Database Syst Rev. 2015;2015(12). doi:10.1002/14651858.CD009228.pub3
8. Emergency Ordinance no. 126 of December 18, 2003 regarding the operation, functioning and financing of the emergency assistance provided with the helicopters purchased by the Ministry of Health and assigned to the medical operators of the Fundeni Clinical Institute and the Târgu Mureş County Emergency Clinical Hospital. Available from: https://legislatie.just.ro/Public/DetaliiDocument/48613.
9. Order no. 777 of June 17, 2004 for the approval of the Methodological Norms for the application of the Government Emergency Ordinance no. 126/2003 regarding the operation, functioning and financing of emergency assistance provided by helicopters purchased by the Ministry of Health and assigned to the medical operators of the Fundeni Clinical Institute and the Târgu Mureş County Emergency Clinical Hospital. Available from: http://www.legex.ro/Ordin-777-2004-45695.aspx.
10. Bläsius FM, Horst K, Brokmann JC, et al. Helicopter emergency medical service and hospital treatment levels affect survival in pediatric trauma patients. J Clin Med. 2021;10(4):837. doi:10.3390/jcm10040837
11. Overview | Major Trauma: assessment and Initial Management | guidance | NICE Available from: https://www.nice.org.uk/guidance/ng39.
12. Pape H-C, Moore EE, Mckinley T, Sauaia A. Pathophysiology in patients with polytrauma. Injury. 2022;53(7):2400–2412. doi:10.1016/j.injury.2022.04.009
13. Fulton M II, Schwartfeger S. EMS Tactical Damage Control Resuscitation Protocol. StatPearls; 2024.
14. Marsden NJ, Tuma F. Polytraumatized Patient. Treasure Island (FL): StatPearls Publishing; 2024.
15. Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69(5):1030–1034. doi:10.1097/TA.0b013e3181f6f450
16. State of health in the EU. Romania - Country Health Profile; 2023. Available from: https://health.ec.europa.eu/system/files/2023-12/2023_chp_ro_english.pdf.
17. Popescu C-M, Marina V, Avram G, Cristescu Budala CL. Spectrum of magnetic resonance imaging findings in acute pediatric traumatic brain injury - a pictorial essay. J Multidiscip Healthc. 2024;17:2921–2934.PMID: 38911614. doi:10.2147/JMDH.S466044
18. Popescu CM, Marina V, Munteanu A, Popescu F. Acute computer tomography findings in pediatric accidental head trauma-review. Pediatric Health Med Ther. 2024;15:231–241.PMID: 38882239. doi:10.2147/PHMT.S461121
19. Dragomir L, Marina V, Anghele M, Anghele AD. Clinical or imaging diagnosis of the current medical practice for superior vena cava syndrome? Diagnostics. 2021;11(11):2058. doi:10.3390/diagnostics11112058
20. Dragomir L, Marina V, Moscu CA, Anghele M. The patient hides the truth, but the computer tomography examination restores it! Diagnostics. 2022;12:876. doi:10.3390/diagnostics12040876
21. Anghele M, Marina V, Moscu CA, Dragomir L, Anghele AD, Lescai AM. Emotional distress in a patients following polytrauma. J Multidiscip Healthc. 2023;1161–1170. doi:10.2147/JMDH.S405904
22. Moscu CA, Marina V, Anghele M, Anghele AD, Dragomir L. Did personality type influence burn out syndrome manifestations during covid-19 pandemic ? Int J Gen Med. 2022;15:5487–5498. doi:10.2147/IJGM.S353405
23. Moscu C-A, Marina V, Dragomir L, Anghele A-D, Anghele M. The impact of burnout syndrome on job satisfaction among emergency department nurses of emergency clinical county hospital “Sfântul Apostol Andrei” of Galati, Romania. Medicina. 1516;2022:58.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



