Back to Journals » Journal of Pain Research » Volume 18
Trajectory of Self-Reported Pain and Association with Quality of Life in Patients with Perianal Abscesses After Surgery
Authors Gao Y, Zhang L, Qian Q, Zhang H , Yao Y
Received 18 October 2024
Accepted for publication 10 May 2025
Published 23 May 2025 Volume 2025:18 Pages 2615—2622
DOI https://doi.org/10.2147/JPR.S492923
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jonathan Greenberg
Yulei Gao,1 Li Zhang,1 Qiao Qian,1 Huachun Zhang,2 Yibo Yao1
1Department of Anorectal, Longhua Hospital Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 2Department of Nursing, Longhua Hospital Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China
Correspondence: Huachun Zhang, Department of Nursing, Longhua Hospital Shanghai University of Traditional Chinese Medicine, No. 725, Wanping South Road, Xuhui District, Shanghai, People’s Republic of China, Email [email protected] Yibo Yao, Department of Anorectal, Longhua Hospital Shanghai University of Traditional Chinese Medicine, No. 725, Wanping South Road, Xuhui District, Shanghai, People’s Republic of China, Email [email protected]
Background: Perianal abscesses are a common anorectal condition characterized by painful collections of pus near the anus and rectum. Surgical intervention is the standard treatment, yet postoperative pain can significantly impact patients’ quality of life (QoL). Understanding the variability in pain experiences and their association with QoL is crucial for improving postoperative outcomes.
Methods: This study included 575 patients who underwent surgical intervention for perianal abscesses between 2021 and 2023. Pain intensity was assessed using the Visual Analog Scale at multiple time points over a four-week follow-up period. QoL was measured using the Short Form-36 health Survey. Group-based trajectory modeling was employed to identify distinct pain trajectories. Multivariate linear regression analyses examined the association between pain trajectories and QoL, adjusting for demographic, lifestyle, and clinical covariates.
Results: Group-based trajectory modeling identified three distinct pain trajectories. Compared to participants in the fluctuating group, patients in trajectories characterized by gradual decline (β=5.17; 95% confidence interval: 2.44, 7.91) or rapid decline (β=5.19; 95% confidence interval: 2.48, 7.90) pain reported significantly higher QoL scores across SF-36 score at 4 weeks post-surgery.
Conclusion: The study highlights the heterogeneity in postoperative pain experiences among patients with perianal abscesses and underscores the importance of personalized pain management strategies. Early identification of patients at risk of poor pain outcomes can facilitate targeted interventions, ultimately improving long-term QoL.
Keywords: perianal abscesses, pain, trajectory, quality of life
Introduction
Perianal abscesses are a prevalent and distressing anorectal condition, characterized by localized collections of pus caused by an infection of the anal glands.1 These absences often present severe pain, swelling, and fever, significantly impacting patients’ quality of life (QoL) and daily functioning.2 The standard treatment for perianal absences is surgical intervention, typically involving incision and drainage to evacuate the pus and alleviate symptoms. While this procedure is generally effective in resolving acute infection, the postoperative period can be marked by varying degrees of pain and discomfort, which may persist for weeks to months.3
Pain management is a critical component of postoperative care for patients with perianal abscesses.4 Effective pain control not only enhances patient comfort but also facilitates early mobilization and recovery, reducing the risk of complications such as chronic pain and infection recurrence.5,6 Despite the importance of pain management, there is limited research on the trajectory of self-reported pain following surgery for perianal abscesses and its association with long-term QoL outcomes. Understanding these pain trajectories can provide valuable insights into patient recovery patterns and inform targeted interventions to improve postoperative outcomes.7,8
Group-based trajectory modeling is a statistical method that identifies distinct subgroups of individuals who follow similar progression paths over time.9 This approach allows for the characterization of heterogeneous pain experiences and the identification of factors associated with different pain trajectories. By applying group-based trajectory modeling to self-reported pain data, we can better understand the variability in pain experiences among patients with perianal abscesses and its impact on their QoL. Previous studies have successfully used group-based trajectory modeling to identify pain trajectories in various clinical populations, including patients with chronic pain, postoperative pain, and cancer-related pain.10,11 Understanding pain trajectories is crucial as it provides a framework for identifying variations in patient recovery patterns, uncovering potential risk factors associated with poor outcomes, and developing patient-centered postoperative care strategies, particularly in populations undergoing procedures with significant postoperative discomfort; such insights are vital in tailoring interventions to specific needs, optimizing resource allocation, and minimizing the overall burden of postoperative pain.
The primary aim of this study is to identify distinct pain trajectories in patients with perianal abscesses following surgical intervention and to examine the association between these trajectories and QoL. We hypothesize that there are multiple pain trajectories with differing impacts on QoL and that identifying these trajectories can help tailor postoperative pain management strategies to improve patient outcomes. Specifically, we aim to: (1) identify distinct trajectories of self-reported pain over a 4-week follow-up period; (2) examine the association between pain trajectories and QoL at 4 weeks.
Methods
Study Population
This study was conducted using data from patients who underwent surgical intervention for perianal abscesses at Longhua Hospital Shanghai University of Traditional Chinese Medicine, Shanghai Anorectal Department between 2021 and 2023. A total of 575 participants aged 18 years and older were included in the study. Inclusion criteria were: (1) diagnosis of perianal absence confirmed by clinical examination and imaging, (2) surgical intervention involving incision and drainage, and (3) availability of complete follow-up data for at least four weeks post-surgery. The abscess drainage procedures were performed using a standardized anesthesia protocol for all patients, specifically employing local anesthesia with sedation to ensure consistency across cases. This approach minimized variability and maintained procedural uniformity. Patient records were reviewed to confirm the consistent application of anesthesia techniques throughout the study period. Exclusion criteria included: (1) pre-existing chronic pain conditions unrelated to perianal abscess, (2) concurrent anorectal conditions requiring additional surgical intervention, and (3) inability to provide informed consent. This study complied with the Declaration of Helsinki, and was approved by the Ethics Committee of Longhua Hospital (NO. 2020LCSY032). All participants signed the informed agreement to participate.
Sample Size
The sample size of 575 participants was determined based on the expected prevalence of distinct pain trajectories and the need for sufficient statistical power to detect differences in QoL outcomes among these trajectories. Previous studies using group-based trajectory modeling have demonstrated the feasibility of identifying distinct pain trajectories with sample sizes ranging from 300 to 1000 participants.12,13
Assessment Tool
Pain Assessment
Self-reported pain was assessed using the Visual Analog Scale, a widely used and validated tool for measuring pain intensity. Participants were asked to rate their pain on a scale from 0 (no pain) to 100 (worst pain imaginable) at regular intervals post-surgery (eg, 1 week, 2 weeks, 3 weeks, 4 weeks). The Visual Analog Scale scores were used to construct pain trajectories over the 4-week follow-up period. All patients received a multimodal analgesia management, involving nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids as required, typically for less than 5 days. Antibiotics were routinely prescribed for 5–7 days to prevent secondary infections, consistent with surgical guidelines for perianal abscess management. Patients were also instructed to use adjunctive strategies, such as warm sitz baths, for additional symptom relief during recovery. In the follow-up period, pain management focused on a multimodal approach. Patients were regularly re-evaluated during outpatient visits to adjust the treatment plan based on their reported pain levels. NSAIDs remained the primary therapy, supplemented by opioids. Adjunctive therapies, such as warm sitz baths, were emphasized to promote local healing and alleviate discomfort. Education on medication adherence and lifestyle adjustments was also provided to optimize recovery outcomes.
Quality of Life Assessment
QoL was assessed using the Short Form-36 health Survey (SF-36), a validated instrument that measures eight domains of health-related quality of life: physical functioning, role limitations due to physical health problems, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health. The SF-36 was administered for 4 weeks post-surgery.
Covariates
Potential confounders were selected based on previous literature and their relevance to both pain and quality of life outcomes. These included:
Demographic factors: age (<60 years vs ≥60 years), gender (male vs female), education (primary and below vs secondary school vs college and above), marital status (married vs other), income (poor vs moderate vs better).
Lifestyle factors: smoking status (current, never), alcohol consumption (current, never).
Clinical factors: body mass index (<18.5 vs 18.5–23.9 vs ≥24 kg/m2), presence of comorbidities (none vs one vs at least one), duration of symptoms before surgery (< 1 week vs ≥1 weeks), surgical type (incision and drainage vs resection [excision of pathological tissue only]), and Parks typing (inter-sphincter type vs transsphincteric vs upper sphincter type).
Statistical Analysis
Group-based trajectory modeling was used to identify distinct pain trajectories over the 4-week follow-up period.14 The group-based trajectory modeling approach allows for the identification of subgroups of individuals who follow similar pain progression paths over time. The Bayesian Information Criterion (BIC) was used to determine the optimal number of trajectories. Models with one to four trajectories were compared, and the model with the lowest BIC value was selected as the best-fitting model. An average posterior probability of assigning individuals to a trajectory group up to 70% or higher was indicative of accurate classification. Chi-Square test was used to compare baseline characteristics between trajectory groups. A multiple linear regression analysis was conducted to examine the association between pain trajectory membership and quality of life outcomes at 4 weeks post-surgery. The SF-36 domain scores were used as the dependent variables, and pain trajectory membership was included as the main independent variable. We fitted three models: 1) crude model, ie, no adjustment; 2) adjusted for gender and age; and 3) adjusted for demographic, lifestyle, and clinical factors. SPSS 26.0 and Stata 17.0 statistical software were used to analyze the data in this study. All statistical tests were two-sided tests, and P<0.05 was taken as a statistically significant difference.
Results
Postoperative Self-Reported Pain Trajectory
After conducting multiple data processing sessions, we observed that among the models in groups 1–3, the absolute BIC values of the models in group 3 were lower than those of the other models, and the average posterior probability values were high, all exceeding 0.8. There were three distinct trajectory groups where the model achieved optimal values while maintaining clinical relevance (Figure 1). The first group comprised 17.9% of the population, characterized as “fluctuating”. The second cohort encompassed 39.2% of the population, classified as “gradual decline”. The third cohort included 42.8% of the population, categorized as “rapid decline”.
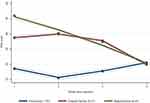 |
Figure 1 Postoperative self-reported pain trajectory. |
Characteristics of Participants
As shown in Table 1, the analysis revealed a significant association between age groups and the study groups (P = 0.018), with a higher proportion of participants aged <60 years in “fluctuating group” compared to “rapid decline group”. Gender distribution was balanced across all groups (P = 0.954). Baseline characteristics such as education level, BMI categories, marital status, symptom duration before surgery, and comorbidities were comparable among the groups (all P > 0.05). Notably, income levels differed significantly across groups (P = 0.042). Surgical type and Parks classification were evenly distributed across the groups (P > 0.05).
 |
Table 1 Patient Demographics and Baseline Characteristics |
Association Between Pain Trajectory with QoL
Results of multivariate linear regression analyses showed that after adjusting for demographic, lifestyle, and clinical factors, compared to the fluctuating group, participants in the gradual decline trajectory group had 5.17 (95% CI 2.44, 7.91) higher QoL scores, whereas participants in the rapid decline trajectory group had 5.19 (95% CI 2.48, 7.90) higher QoL scores (Table 2).
 |
Table 2 Results of Multiple Linear Regression Analysis |
Discussion
This study aimed to identify distinct pain trajectories in patients with perianal abscesses following surgical intervention and to examine the association between these trajectories and QoL. Using group-based trajectory modelling, we identified three distinct pain trajectories over the 4-week follow-up period. Our findings suggest that postoperative pain experiences are heterogeneous, with significant implications for patient management and outcomes.
The identification of multiple pain trajectories highlights the variability in postoperative pain experiences among patients with perianal abscesses. Consistent with previous research on postoperative pain, our study found that some patients experience a rapid decline in pain intensity, while others report persistent or fluctuating pain over time.7 The factors contributing to these different pain trajectories are likely multifactorial, including variations in surgical technique, individual pain thresholds, psychological factors, and the presence of comorbidities.15
Our analysis revealed a significant association between pain trajectory membership and QoL at 4 weeks post-surgery. Patients in trajectories characterized by gradual decline or rapid decline pain reported higher QoL scores across the SF-36. These findings are consistent with previous studies demonstrating the detrimental impact of postoperative pain on QoL.16,17 The strong association between pain and QoL underscores the importance of effective pain management strategies to improve long-term outcomes for patients with perianal abscesses. Redman et al3 reported declining VAS scores following abscess drainage, highlighting the acute nature of pain in the immediate postoperative period and its resolution with appropriate management. However, variations in results suggest a gap in standardized pain management protocols and their impact on pain trajectories, indicating a need for further research on personalized pain control strategies for perianal procedures.
The heterogeneity in pain trajectories suggests that a one-size-fits-all approach to pain management may be inadequate. Instead, personalized pain management strategies tailored to the specific needs of different patient subgroups are warranted.18 For example, patients in trajectories characterized by persistent pain may benefit from multimodal pain management approaches that combine pharmacological and non-pharmacological interventions, such as cognitive-behavioral therapy, transcutaneous electrical nerve stimulation, and acupuncture.19,20 Early identification of patients at risk of poor pain outcomes through baseline predictors, such as high levels of preoperative anxiety and depression, can facilitate timely interventions and potentially improve postoperative recovery.21,22
Future research should aim to validate our findings in larger, multicenter cohorts to enhance generalizability. Additionally, exploring the underlying mechanisms driving different pain trajectories, such as genetic, neurobiological, and psychosocial factors, could provide valuable insights for developing targeted interventions. Investigating the effectiveness of personalized pain management strategies in randomized controlled trials would further inform clinical practice and improve patient outcomes.23,24
One of the strengths of this study is the use of group-based trajectory modelling to identify distinct pain trajectories, which allows for a nuanced understanding of postoperative pain experiences. However, several limitations should be acknowledged. First, the inclusion of patients with perianal abscess from only one center and a poor sample size made the fitted change trajectory under representative; second, lifestyle, including physical activity level and dietary habits, is an important factor influencing postoperative pain, but we lacked the collection of this variable during follow-up; third, the group-based trajectory model is inherently flawed in that it ignores individual variability within the same trajectory, which may have weakened the trajectory of pain; fourth, because pain is based on self-reported scores, it may exaggerate an individual’s own self-perception. However, for the time being, the assessment of pain is based on scales; fifth, the present longitudinal study only followed pain reports for 4 weeks postoperatively, whereas, in fact, postoperative pain in patients with perianal abscesses may persist for a longer period of time. Future studies with extended follow-up are needed to assess these outcomes comprehensively; sixth, our single-center study lacks an external validation group, which may limit the generalizability of our findings. Future multicenter studies are recommended to externally validate our results and address potential geographic or institutional biases in the dataset.
Clinical Practice Implications
The identification and classification of pain trajectory groups provide a practical framework for implementing personalized postoperative care. Routine pain assessments at regular intervals (eg, weekly over the first month) allow for early detection of patients following moderate or fluctuating pain trajectories. This facilitates timely interventions such as multimodal analgesia or psychological support. Additionally, using pre-established classification criteria, such as pain intensity thresholds and trajectory trends, clinicians can predict recovery patterns and adjust treatment plans. This tailored approach improves pain control, enhances recovery, and promotes better long-term QoL outcomes for patients with perianal abscesses.
Conclusion
In conclusion, our study identified multiple distinct pain trajectories in patients with perianal abscesses following surgical intervention and demonstrated a significant association between pain trajectory membership and QoL. These findings underscore the importance of personalized pain management strategies to address the heterogeneous pain experiences and improve long-term outcomes for patients with perianal abscesses. Future research should focus on validating these findings in larger cohorts and exploring the underlying mechanisms to inform targeted interventions.
Data Sharing Statement
All data are available by contacting the corresponding author.
Ethics Approval
The study was approved by the Ethics Committee of Longhua Hospital (NO. 2020LCSY032).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by Shanghai Sinus Fistula Disease Research Center (2023ZZ02003).
Disclosure
The authors declare no competing interests in this work.
References
1. Sahnan K, Adegbola SO, Tozer PJ, Watfah J, Phillips RK. Perianal abscess. BMJ. 2017;356:j475. doi:10.1136/bmj.j475
2. Yamamoto T, Nakase H, Watanabe K, et al. Diagnosis and clinical features of perianal lesions in newly diagnosed Crohn’s disease: subgroup analysis from inception cohort registry study of patients with Crohn’s disease (iCREST-CD). J Crohn's Colitis. 2023;17:1193–1206. doi:10.1093/ecco-jcc/jjad038
3. Redman IA, Panahi P, Gill M, Drymousis P. Postoperative packing of perianal abscesses following incision and drainage. Br J Hosp Med. 2023;84:1–6. doi:10.12968/hmed.2023.0308
4. Wang G, Miao C. Chinese expert consensus on standardized treatment for presacral cysts. Gastroenterol Rep. 2023;11:goac079. doi:10.1093/gastro/goac079
5. Kehlet H, Dahl JB. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg. 1993;77:1048–1056. doi:10.1213/00000539-199311000-00030
6. van der Vijver RJ, van Laarhoven CJ, de Man BM, Lomme RM, Hendriks T. The effect of fibrin glue on the early healing phase of intestinal anastomoses in the rat. Int J Colorectal Dis. 2012;27:1101–1107. doi:10.1007/s00384-012-1435-5
7. Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention. Lancet. 2006;367:1618–1625. doi:10.1016/S0140-6736(06)68700-X
8. Macrae WA. Chronic pain after surgery. Br J Anaesth. 2001;87:88–98. doi:10.1093/bja/87.1.88
9. Liu L, Li X, Marshall IJ, Bhalla A, Wang Y, O’Connell MDL. Trajectories of depressive symptoms 10 years after stroke and associated risk factors: a prospective cohort study. Lancet. 2023;402 Suppl 1:S64. doi:10.1016/S0140-6736(23)02111-6
10. Dunn KM, Jordan K, Croft PR. Characterizing the course of low back pain: a latent class analysis. Am J Epidemiol. 2006;163:754–761. doi:10.1093/aje/kwj100
11. Nagin DS, Odgers CL. Group-based trajectory modeling (Nearly) two decades later. J Quant Criminol. 2010;26:445–453. doi:10.1007/s10940-010-9113-7
12. An R, Zhang S, Huang X, Lan Y, Cao T, Wan Q. Physical activity trajectories and their determinants in patients with chronic obstructive pulmonary disease: a cohort study. J Clin Nurs. 2023;32:5093–5102. doi:10.1111/jocn.16771
13. Jongen VW, Reyniers T, Schim van der Loeff M, et al. Trajectories of PrEP use among men who have sex with men: a pooled analysis of two prospective, observational cohort studies. J Int AIDS Soc. 2023;26:e26133. doi:10.1002/jia2.26133
14. Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–138. doi:10.1146/annurev.clinpsy.121208.131413
15. Katz J, Seltzer Z. Transition from acute to chronic postsurgical pain: risk factors and protective factors. Expert Rev Neurother. 2009;9:723–744. doi:10.1586/ern.09.20
16. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. doi:10.1016/j.ejpain.2005.06.009
17. Smith BH, Elliott AM, Chambers WA, Smith WC, Hannaford PC, Penny K. The impact of chronic pain in the community. Fam Pract. 2001;18:292–299. doi:10.1093/fampra/18.3.292
18. Rivadeneira DE, Ruffo B, Amrani S, Salinas C. Rectovaginal fistulas: current surgical management. Clin Colon Rectal Surg. 2007;20:96–101. doi:10.1055/s-2007-977487
19. Derry CJ, Derry S, McQuay HJ, Moore RA. Systematic review of systematic reviews of acupuncture published 1996-2005. Clin Med. 2006;6:381–386. doi:10.7861/clinmedicine.6-4-381
20. Eccleston C, Palermo TM, Williams AC, Lewandowski A, Morley S. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2009;CD003968. doi:10.1002/14651858.CD003968.pub2
21. Hinrichs-Rocker A, Schulz K, Jarvinen I, Lefering R, Simanski C, Neugebauer EA. Psychosocial predictors and correlates for chronic post-surgical pain (CPSP) - a systematic review. Eur J Pain. 2009;13:719–730. doi:10.1016/j.ejpain.2008.07.015
22. Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
23. Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc. 2010;85:S3–14. doi:10.4065/mcp.2009.0649
24. Turk DC, Wilson HD, Cahana A. Treatment of chronic non-cancer pain. Lancet. 2011;377:2226–2235. doi:10.1016/S0140-6736(11)60402-9
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
The Burden of Metastatic Cancer–Induced Bone Pain: A Narrative Review
Colosia A, Njue A, Bajwa Z, Dragon E, Robinson RL, Sheffield KM, Thakkar S, Richiemer SH
Journal of Pain Research 2022, 15:3399-3412
Published Date: 25 October 2022
The Efficacy of a Preoperative Occupational Therapy Educational Session for Saudi Patients Undergoing a Lower Extremity Joint Replacement
Al-Heizan MO, Shoman A, Tawffeq A, Banamah A, Balkhair F, Filimban S, Alsinan W, Batouk O, Turkistani T
Journal of Multidisciplinary Healthcare 2023, 16:31-38
Published Date: 10 January 2023
A Systematic Review and Meta-Analysis of the Effects of Rehabilitation Using Digital Healthcare on Musculoskeletal Pain and Quality of Life
Jang S, Lee B, Lee E, Kim J, Lee JI, Lim JY, Hwang JH, Jang S
Journal of Pain Research 2023, 16:1877-1894
Published Date: 31 May 2023
Physical Activity, Depression and Quality of Life in COPD – Results from the CLARA II Study
Horner A, Olschewski H, Hartl S, Valipour A, Funk GC, Studnicka M, Merkle M, Kaiser B, Wallner EM, Brecht S, Lamprecht B
International Journal of Chronic Obstructive Pulmonary Disease 2023, 18:2755-2767
Published Date: 29 November 2023
Associations Between Patterns of Daily Stepping Behavior, Health-Related Quality of Life, and Pain Symptoms Among Older Adults with Chronic Pain: A Secondary Analysis of Two Randomized Controlled Trials
Fanning J, Brooks AK, Irby MB, N'Dah KW, Rejeski WJ
Clinical Interventions in Aging 2024, 19:459-470
Published Date: 14 March 2024

