Back to Journals » Cancer Management and Research » Volume 17
Tumor-Educated Platelets lncRNA-STARD4-AS1 and ELOA-AS1 as Potential Novel Biomarkers for the Early Diagnosis of Non-Small Cell Lung Cancer
Authors Luo C, Lin Z, Huang F, Ning L, Yuan Y
Received 29 September 2024
Accepted for publication 14 December 2024
Published 3 January 2025 Volume 2025:17 Pages 1—9
DOI https://doi.org/10.2147/CMAR.S498516
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
ChangLiang Luo, Zhongyuan Lin, Fangfang Huang, Leping Ning, Yulin Yuan
Department of Clinical Laboratory, The People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, Guangxi, 530021, People’s Republic of China
Correspondence: Leping Ning; Yulin Yuan, Department of Clinical Laboratory, The People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, 530021, People’s Republic of China, Email [email protected]; [email protected]
Purpose: (Tumor-educated platelets) TEPs have emerged as active players in all steps of tumorigenesis, confrontation of platelets with tumor cells via transfer of tumor-associated biomolecules and results in the sequestration of such biomolecules. The current study was aimed to examine whether TEPs lncRNA-STARD4-AS1 and ELOA-AS1 might be potential biomarkers for NSCLC.
Materials and Methods: TEPs were obtained by low-speed centrifugation. Quantitative real-time PCR was used to determine the expression level of TEPs-STARD4-AS1, ELOA-AS1 in the training cohort and the validation cohort. ROC curve was generated to evaluate their diagnostic value. Correlations between TEPs-STARD4-AS1, ELOA-AS1 and clinical parameters were further analyzed.
Results: Our results showed that the level of TEPs-STARD4-AS1 and ELOA-AS1 significantly upregulated in patients with NSCLC compared with healthy controls in the two cohorts. By ROC analysis, we found that TEPs-STARD4-AS1, ELOA-AS1 could offer valuable diagnostic performance for NSCLC patients (AUCSTARD4-AS1 = 0.800/0.774, and AUCELOA-AS1 = 0.754/0.718 for diagnosing adenocarcinoma and squamous cell carcinoma cases from controls, respectively). The combination of TEP-STARD4-AS1 and ELOA-AS1 improved the diagnostic efficiency of NSCLC. Clinicopathological analysis further revealed that TEPs-STARD4-AS1 level significantly correlated with tumor-node-metastasis (TNM) stage (p = 0.011), while TEPs-ELOA-AS1 expression significantly correlated with tumor-node-metastasis (TNM) stage and (p = 0.019) distant metastasis (p = 0.004).
Conclusion: Our data suggested that TEPs-STARD4-AS1 and ELOA-AS1 are promising non-invasive circulating diagnostic markers for NSCLC.
Keywords: tumor-educated platelets, STARD4-AS1, ELOA-AS1, diagnosis, NSCLC
Introduction
Non-small cell lung cancer (NSCLC), mainly divided into adenocarcinoma (LUAD) and squamous cell carcinoma (SCC), accounts for more than 80% of all lung cancers,1 has the highest incidence and ranks first in cancer-related mortality worldwide.2 Despite significant progress has been made in the treatment of lung cancer in recent years, the 5-year survival rate for NSCLC patients is only 5–20%,3,4 mainly due to the lack of effective early diagnostic methods. At present, the gold standard for tumor diagnosis is still tissue biopsy and pathologic diagnosis, but it has limitations in the assessment of cancer development, genotyping and prognosis, due to tumor evolution and heterogeneity.5 And it has been found that many patients refuse to undergo puncture surgery, considering its invasive procedure. Therefore, there is an urgent need to discover sensitive, specific, especially noninvasive biomarkers for early detection of NSCLC. In recent years, many clinicians and scientists have tried to use blood-based liquid biopsies as a potential alternative diagnostic method for NSCLC.
Liquid biopsies, including tumor-educated blood platelets (TEPs), exosomes, circulating cell-free tumor DNA, and circulating tumor cells, might offer earlier and more convenient diagnosis for patients with cancer.6,7 Additionally, these techniques are less invasive and might provide a more comprehensive characterization for cancer.
Platelets, as a type of abundant blood cells, are circulating anucleated cell fragments that originate from megakaryocytes in bone marrow and are traditionally known for their role in hemostasis and initiation of wound healing.8 More recently, TEPs have emerged as active players in all steps of tumorigenesis including tumor growth, tumor cell extravasation, and metastasis, confrontation of platelets with tumor cells via transfer of tumor-associated biomolecules including RNA transcripts and proteins, as well as altering their spliced RNA profiles and results in the sequestration of such biomolecules.9,10 Additionally, it has been reported that biomolecules in TEPs might be more stable and could offer high sensitivity for the detection of cancer, while tumor-associated biomolecules released into the plasma are susceptible to degradation.11 Therefore, TEPs have emerged as a promising source of biomarkers for liquid biopsy.12–14 Numerous studies have indicated that the transcriptomic and proteomic profile of platelets undergo alterations in response to the presence of cancer, emphasizing their potential utility as a biomarker for the diagnosis and prognosis of tumor.15–18
Long non-coding RNA (LncRNA) is a group of RNA molecules with a transcript length of more than 200 nucleotides that widely exists in eukaryotic cells, but it does not encode protein itself. The mechanism of action of lncRNA is diverse, it regulates the expression level of genes through epigenetic regulation, splicing, imprinting, transcriptional regulation, and subcellular transport, and it plays important roles in tumorigenesis and tumor progression, virus replication, inflammatory injury, and other pathological processes.19,20 For example, Ji et al first discovered and reported MALAT1 in 2003, it is closely related to early metastasis and prognosis of lung adenocarcinoma,21 and acts as an inflammatory regulator, modulating the expression of inflammatory mediators such as TNF-α and IL-6 in endothelial cells;22 Yi Liao et al also found that lncRNAs such as MALAT1 and NEAT1 posse a high accuracy in the diagnosis of sepsis and the determination of 28-day mortality in patients with sepsis.23 Yongdong Wang et al found that lncRNAs such as H19, APOA1-AS, IFNG-AS1, RMRP, and Lnc-EGFR exhibit considerable sensitivity and specificity in diagnosing MS but also in forecasting its progression and assessing disease severity.24 Additionally, Ping Lin et al showed that lncRNAs, especially lncRNA H19, FAM201A and HOTAIR, can induce cancer radio resistance by regulating cell death-related signaling pathways, which could be considered as a predictive theragnostic biomarker to evaluate radiotherapy response.25 These data indicated that lncRNAs play important roles in cancer pathogenesis, which could provide new insight into the biology of this disease.
In the present study, 2 lncRNAs were selected based on p <0.0001 and log 2 (fold change) >14.8 from the result of Illumina high-throughput RNA sequencing between 1 LUAD sample and 1 healthy sample. Next, we investigated the expression pattern and diagnostic value of 2 lncRNAs from platelets in patients with NSCLC to explore whether TEPs could enable NSCLC diagnostic and identify NSCLC types.
Materials and Methods
Illumina High-Throughput RNA Sequencing
One early-stage LUAD sample and 1 healthy sample were obtained from The People’s Hospital of Guangxi Zhuang Autonomous Region. The samples were proceeded for Illumina high-throughput RNA sequencing in the company of Novogene. Upregulated LncRNAs (STARD4-AS1, ELOA-AS1) were selected based on p <0.001 and log 2 (fold change) >14.8.
Sample Collection and Platelet Isolation
Whole blood samples of NSCLC patients and healthy controls, which then were divided into the training cohort (20 LUAD,15 SCC and 15 healthy controls) and the validation cohort (81 LUAD,59 SCC and 45 healthy controls), obtained from The People’s Hospital of Guangxi Zhuang Autonomous Region from 2022 to 2024. Platelets were isolated using low-speed centrifugation as previously described.9,10 Plasma samples were collected and then centrifuged for 20 min at 120 g to remove cells and debris. The platelet-rich plasma was centrifuged at 360 g for 20 min to pellet platelets, which then collected in 300 ul DEPC and stored at −80°C. The study complied with the Declaration of Helsinki and was approved by the Ethics Committee of The People’s Hospital of Guangxi Zhuang Autonomous Region (No: KY-KJT-2021-79 and KY-KJT-2022-100). Informed consent was obtained from all individual participants included in the study.
RT-qPCR for lncRNAs
RT-qPCR was determined on the Bio-Rad CFX96 (Bio-Rad Laboratories, Inc, Hercules, CA, USA) using TB Green Premix EX TaqTM Fast qPCR (CN830S, Takara, Japan) after platelets RNA was isolated using a Liquid Total RNA Isolation Kit (RP4002, BioTeke, China) and reverse transcribed to cDNA using PrimeScriptTM Fast RT reagent Kit with gDNA Erase (RR092s, Takara, Japan). The GAPDH was used as the endogenous control and was amplified simultaneously with target genes. The synthesized RT-qPCR primers were listed in Table 1. The relative gene expression level was calculated using the comparative Ct (Cycle threshold) method formula 2−ΔCt,while CT value is the number of cycles when the fluorescence signal in each reaction tube reaches a set threshold and ΔCT = CT lncRNA–CT GAPDH.
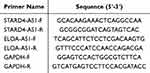 |
Table 1 Primers Used for RT-qPCR |
Statistical Analysis
Statistical analyses were performed using SPSS version 23.0 (SPSS, Chicago, IL, USA) or Prism7 (GraphPad software, La Jolla, CA). The Shapiro–Wilk test was carried out to check the normality of the distribution. The non-normally distributed variable was analyzed by Mann–Whitney test. Chi-square test was used to analyze the categorical variables. Statistical differences were set at *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. p < 0.05 was considered statistically significant. ROC curve analysis was used to estimate the diagnostic value of the lncRNAs.
Results
Establishment the Detection Method of TEPs-LncRNAs
A total of 1457 upregulated and 1004 downregulated LncRNAs were screened according to the result of Illumina high-throughput RNA sequencing, we finally selected upregulated LncRNA-STARD4-AS1, ELOA-AS1 based on p <0.001 and log 2 (fold change) >14.8 (Figure 1A). Next, we evaluated the TEPs that isolated from the certain volume of plasma are suitable for the detection of STARD4-AS1 and ELOA-AS1, our data showed that the abundances of 2 lncRNAs were proportionally increased as the volume of collected plasma increased (Figure 1B). Finally, we found TEPs, which are isolated from 600 μL volume of plasma is enough for the detection. The amplification Curve (Figure 1C) of TEPs-LncRNAs isolated from 600 μL plasma showed that the 600 μL plasma is enough for TEPs isolation and 2 lncRNAs detection, the Melt Curve (Figure 1D) of 2 lncRNAs isolated from 600 μL volume showed that the specificity of Primer is also good.
Upregulated of NSCLC TEPs-LncRNAs in Two Different Cohorts
The training cohort consisted of small samples including 20 LUAD patients, 15 SCC patients and 15 healthy controls. We initially explored the expression level of TEPs-TARD4-AS1 and ELOA-AS1 in the training cohort after the detection method establishment. As shown in Figure 2A and B, compared with healthy controls, TEPs-STARD4-AS1 and ELOA-AS1 notably upregulated in both LUAD and SCC patients. In order to confirm the expression level of 2 lncRNAs, we collected more samples including 81 LUAD patients, 59 SCC patients and 45 healthy controls as the validation cohort considering the small samples in the training cohort. In our validation cohort, the data show that the expression of 2 lncRNAs was highly consistent with the data of the training cohort (Figure 2C and D), which indicated the potential of TEPs-STARD4-AS1 and ELOA-AS1 as non-invasive circulating diagnostic markers for NSCLC.
Diagnostic Value of TEPs-LncRNAs Analysis in NSCLC
ROC curve analysis was used to evaluate the diagnosis value of TEPs-lncRNAs for NSCLC. ROC was constructed 3 models just using the data of validation cohort: LUAD vs controls, SCC vs controls, NSCLC vs controls. The AUC of TEP-STARD4-AS1 was 0.800 with 72.8% sensitivity and 71.1%specificity in LUAD, 0.774 with 89.8% sensitivity and 51.1%specificity in SCC, 0.789 with 70.1% sensitivity and 71.1% specificity in NSCLC (Figure 3A). The AUC of TEP- ELOA-AS1 was 0.754 with 77.8% sensitivity and 64.4%specificity in LUAD, 0.718 with 72.8% sensitivity and 64.3%specificity in SCC, 0.739 with 75.7% sensitivity and 64.5% specificity in NSCLC (Figure 3B). ROC curves revealed that the TEP-STARD4-AS1 and ELOA-AS1 expression was both able to discriminate NSCLC patients from healthy controls; however, TEP-STARD4-AS1 showed better AUC, moderate sensitivity and specificity. Next, we proceed a combined diagnosis of the 2 lncRNAs, 0.869 with 65.4% sensitivity and 95.6%specificity in LUAD, 0.825 with 78.0% sensitivity and 75.5% specificity in SCC, 0.851 with 60.7% sensitivity and 95.6% specificity in NSCLC (Figure 3C), the combined diagnosis for NSCLC show better AUC than that for STARD4-AS1 and ELOA-AS1 alone though the sensitivity was lower. More importantly, the combination of 2 lncRNAs improved the specificity to 95.6%, which provided compelling evidences that combination of 2 lncRNAs acted as relatively high diagnostic value for NSCLC. All AUCs are shown in Table 2.
 |
Table 2 AUC of TEPs-STARD4-AS1 and ELOA-AS1 in All Subgroups |
Correlation Between the Expression Level of TEPs-LncRNAs and Clinical Parameters of NSCLC
According to the median value of relative TEPs-lncRNAs expression in the validation cohort, 140 NSCLC patients were correspondently classified into two groups; relative high group: expression ratio ≥ median, relative low group: expression ratio < median. As presented in Table 3 and Figure 3D–F, the result show that the TEPs-STARD4-AS1 expression significantly correlated with tumor-node-metastasis (TNM) stage (p = 0.011), the TEPs-ELOA-AS1 expression significantly correlated with tumor-node-metastasis (TNM) stage (p = 0.019) and distant metastasis (p = 0.004), while there were no significant correlations between TEP lncRNAs and other parameters.
 |
Table 3 Correlation Between TEPs-lncRNAs Level and Clinical Parameters of NSCLC |
Discussion
Over the past decade, systematic empirical research specific on NSCLC have identified several biomarkers and prognostic factors.26 However, the prognosis of NSCLC remains quite poor and the 5-year survival rate for NSCLC patients is still low, since most of the patients are diagnosed at a late stage of the disease. Recently, TEPs, as a promising source of biomarkers for liquid biopsy, is progressively proving a pivotal tool for screening and early detection of cancer.27–29
LncRNAs are a heterogeneous group of noncoding transcripts widely found in body fluids including TEPs. In recent years, aberrant TEPs lncRNA expression has been found to participate in NSCLC development and metastasis. For example, Xiaohan Dong et al found that downregulated TEPs SNORD55 possessed an AUC of 0.803 for NSCLC and an AUC of 0.803 for early NSCLC, they validated that it had the ability of acting as a promising biomarker for NSCLC.30 Additionally, Xinyi Li et al found that downregulated TEP linc–GTF2H2-1, RP3-466P17.2 and upregulated lnc-ST8SIA4-12 in patients with lung cancer possessed AUCs of 0.781, 0.788, 0.725, which suggested that lncRNAs sequestered in TEPs enabled blood-based lung cancer diagnosis and progression prediction.31 However, there is few rearches on STARD4-AS1 or ELOA-AS1 in NSCLC.
In this study, we examined the potential of TEPs-STARD4-AS1 and ELOA-AS1 might as non-invasive circulating diagnostic markers for NSCLC. Firstly, upregulated LncRNA-STARD4-AS1 and ELOA-AS1 were selected based on log 2 (fold change) >14.8 according to the result of Illumina high-throughput RNA sequencing. Meanwhile, we found TEPs, which isolated from 600 μL volume of plasma, are enough for the detection of 2 lncRNAs; this suggests that only 2 mL of blood is needed for each patient and greatly facilitating clinical blood collection. Next, we explored the expression level of 2 lncRNAs in the training cohort and confirmed it in the validation cohort after the detection method establishment. The results show that TEPs-TARD4-AS1 and ELOA-AS1 were upregulated in the two cohorts, which is consistent with the data of Illumina high-throughput RNA sequencing. For STARD4-AS1, there are reports suggesting its upregulation might regulate the process of ferroptosis and could be used as a novel biomarker of oral squamous cell carcinoma,32,33 but the research in TEPs from NSCLC is rarely reported just like ELOA-AS1. It is the first time that TEPs-STARD4-AS1 and ELOA-AS1 were found to upregulate in NSCLC. We then evaluate the diagnosis value of 2 lncRNAs, we found they could offer valuable diagnostics information for NSCLC, both TEPs-STARD4-AS1 (AUC 0.800 in LUAD and AUC 0.774 in SCC) and TEPs-STARD4-AS1 (AUC 0.754 in LUAD and AUC 0.718 in SCC). Of course, combination of 2 lncRNAs possessed a better ability to discriminate between NSCLC and controls (AUC 0.869 in LUAD and AUC 0.825 in SCC). More importantly, the combination of 2 lncRNAs improved the specificity to 95.6%, which indicated the potential as non-invasive circulating diagnostic markers for NSCLC. We also analyzed the correlation between the 2 lncRNAs level and the clinicopathological characteristics of the 140 NSCLC patients in the validation cohort, we found that the expression level of TEPs-STARD4-AS1 was positively correlated with TNM stage, while TEPs-ELOA-AS1 expression significantly correlated with TNM stage and distant metastasis, this might suggest they play a role similar to oncogene in the development and malignancy of NSCLC.
Despite the role of STARD4-AS1 and ELOA-AS1, we found in TEPs from NSCLC, and few studies have previously discussed. Nevertheless, there are several limitations in the present study, which should be carefully considered. First, our research included 175 NSCLC patients, and the total sample size was relatively small. Second, most of the subjects included in the study recruit in one hospital and are local residents, which may affect the accuracy of the conclusion. A previous study has already highlighted that differences in RNA expression in LUAD across races and differences in protein expression across race,34 which demonstrated that enough research subjects from different district, country or race would provide compelling result. Last, we did not proceed ROC curve analysis, which combined TEPs-lncRNAs with a standard screening test marker such as CEA because of the data missing in some subjects.
Conclusion
Our data suggested that TEPs-STARD4-AS1 and ELOA-AS1 are promising non-invasive circulating diagnostic markers for NSCLC.
Funding
This research was supported by Guangxi Natural Science Foundation under Grant No. 2022GXNSFBA035515 and Self-funded research project of The Health Committee of Guangxi Zhuang Autonomous Region under Grant No.Z-A20220100.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Siegel RL, Miller KD. Cancer statistics. CA. 2023;73(1):17–48. doi:10.3322/caac.21763
2. Adjei AA. Lung cancer worldwide. J Thorac Oncol. 2019;14(6):956. doi:10.1016/j.jtho.2019.04.001
3. Ellis PM, Vandermeer R. Delays in the diagnosis of lung cancer. J Thorac Dis. 2011;3(3):183–188. doi:10.3978/j.issn.2072-1439.2011.01.01
4. Walters S, Maringe C, Coleman MP, et al. Lung cancer survival and stage at diagnosis in Australia, Canada, Denmark, Norway, Sweden and the UK: a population-based study, 2004–2007. Thorax. 2013;68(6):551–564. doi:10.1136/thoraxjnl-2012-202297
5. Crowley E, Di Nicolantonio F, Loupakis F, Bardelli A. Liquid biopsy: monitoring cancer-genetics in the blood. Nat Rev Clin Oncol. 2013;10(8):472–484. doi:10.1038/nrclinonc.2013.110
6. Visser E, Genet S, De Kock R, et al. Liquid biopsy-based decision support algorithms for diagnosis and subtyping of lung cancer. Lung Cancer. 2023;178:28–36. doi:10.1016/j.lungcan.2023.01.014
7. Wang L, Zhao S, Mingxin YU. LncRNA NR2F1-AS1 is involved in the progression of endometrial cancer by sponging miR-363 to target SOX4. Pharmazie. 2019;74(5):295–300. doi:10.1691/ph.2019.8905
8. Leslie M. Cell biology. Beyond clotting: the powers of platelets. Science. 2010;328(5978):562–564. doi:10.1126/science.328.5978.562
9. Best MG, Sol N, Kooi I, et al. RNA-seq of tumor-educated platelets enables blood-based pan-cancer, multiclass, and molecular pathway cancer diagnostics. Cancer Cell. 2015;28(5):666–676. doi:10.1016/j.ccell.2015.09.018
10. Best MG, Wesseling P, Wurdinger T. Tumor-educated platelets as a noninvasive biomarker source for cancer detection and progression monitoring. Cancer Res. 2018;78(13):3407–3412. doi:10.1158/0008-5472.can-18-0887
11. Nilsson RJ, Karachaliou N, Berenguer J, et al. Rearranged EML4-ALK fusion transcripts sequester in circulating blood platelets and enable blood-based crizotinib response monitoring in non-small-cell lung cancer. Oncotarget. 2016;7(1):1066–1075. doi:10.18632/oncotarget.6279
12. Antunes-Ferreira M, Koppers-Lalic D, Würdinger T. Circulating platelets as liquid biopsy sources for cancer detection. Mol Oncol. 2021;15(6):1727–1743. doi:10.1002/1878-0261.12859
13. D’ambrosi S, Nilsson RJ, Wurdinger T. Platelets and tumor-associated RNA transfer. Blood. 2021;137(23):3181–3191. doi:10.1182/blood.2019003978
14. Zhang Q, Liu H, Zhu Q, et al. Patterns and functional implications of platelets upon tumor “education”. Int J Biochem Cell Biol. 2017;90:68–80. doi:10.1016/j.biocel.2017.07.018
15. Campolo F, Sesti F, Feola T, et al. Platelet-derived circRNAs signature in patients with gastroenteropancreatic neuroendocrine tumors. J Transl Med. 2023;21(1):548. doi:10.1186/s12967-023-04417-8
16. Gao Y, Liu CJ, Li HY, et al. Platelet RNA enables accurate detection of ovarian cancer: an intercontinental, biomarker identification study. Protein Cell. 2023;14(6):579–590. doi:10.1093/procel/pwac056
17. Liefaard MC, Moore KS. Tumour-educated platelets for breast cancer detection: biological and technical insights. Br J Cancer. 2023;128(8):1572–1581. doi:10.1038/s41416-023-02174-5
18. Luo CL, Xu ZG, Chen H, et al. LncRNAs and EGFRvIII sequestered in TEPs enable blood-based NSCLC diagnosis. Cancer Manag Res. 2018;10:1449–1459. doi:10.2147/cmar.s164227
19. Schmitz SU, Grote P, Herrmann BG. Mechanisms of long noncoding RNA function in development and disease. Cell Mol Life Sci. 2016;73(13):2491–2509. doi:10.1007/s00018-016-2174-5
20. Spizzo R, Almeida MI, Colombatti A, Calin GA. Long non-coding RNAs and cancer: a new frontier of translational research? Oncogene. 2012;31(43):4577–4587. doi:10.1038/onc.2011.621
21. Gutschner T, Hämmerle M, Eissmann M, et al. The noncoding RNA MALAT1 is a critical regulator of the metastasis phenotype of lung cancer cells. Cancer Res. 2013;73(3):1180–1189. doi:10.1158/0008-5472.can-12-2850
22. Zhuang YT, Xu DY, Wang GY, Sun JL, Huang Y, Wang SZ. IL-6 induced lncRNA MALAT1 enhances TNF-α expression in LPS-induced septic cardiomyocytes via activation of SAA3. Eur Rev Med Pharmacol Sci. 2017;21(2):302–309.
23. Liao Y, Wang R, Wen F. Diagnostic and prognostic value of long noncoding RNAs in sepsis: a systematic review and meta-analysis. Expert Rev Mol Diagn. 2022;22(8):821–831. doi:10.1080/14737159.2022.2125801
24. Wang Y, Wang J, Zhang X, Xia C, Wang Z. Diagnostic efficacy of long non-coding RNAs in multiple sclerosis: a systematic review and meta-analysis. Front Genet. 2024;15:1400387. doi:10.3389/fgene.2024.1400387
25. Lin P, Xing W, Ren Q, Wang Q, Yan J, Mao G. LncRNAs as theragnostic biomarkers for predicting radioresistance in cancer: a systematic review and meta-analysis. Front Oncol. 2022;12:767750. doi:10.3389/fonc.2022.767750
26. Wang LP, Niu H, Xia YF, et al. Prognostic significance of serum sMICA levels in non-small cell lung cancer. Eur Rev Med Pharmacol Sci. 2015;19(12):2226–2230.
27. Schlesinger M. Role of platelets and platelet receptors in cancer metastasis. J Hematol Oncol. 2018;11(1):125. doi:10.1186/s13045-018-0669-2
28. Sheng M, Dong Z, Xie Y. Identification of tumor-educated platelet biomarkers of non-small-cell lung cancer. Onco Targets Ther. 2018;11:8143–8151. doi:10.2147/ott.s177384
29. Wang Y, Dong A. TEP RNA: a new frontier for early diagnosis of NSCLC. J Cancer Res Clin Oncol. 2024;150(2):97. doi:10.1007/s00432-024-05620-w
30. Dong X, Song X, Ding S, et al. Tumor-educated platelet SNORD55 as a potential biomarker for the early diagnosis of non-small cell lung cancer. Thorac Cancer. 2021;12(5):659–666. doi:10.1111/1759-7714.13823
31. Li X, Liu L, Song X, et al. TEP linc-GTF2H2-1, RP3-466P17.2, and lnc-ST8SIA4-12 as novel biomarkers for lung cancer diagnosis and progression prediction. J Cancer Res Clin Oncol. 2021;147(6):1609–1622. doi:10.1007/s00432-020-03502-5
32. Ji L, Liang S, Cheng Y, et al. Identification of a novel necroptosis-related LncRNA signature for prognostic prediction and immune response in oral squamous cell carcinoma. Cancer Biomark. 2024;40(3–4):319–342. doi:10.3233/cbm-230407
33. Li J, Qiao Z, Li Y, Lu X, Shao T, Lv X. Bioinformatic analysis indicated that STARD4-AS1 might be a novel ferroptosis-related biomarker of oral squamous cell carcinoma. Heliyon. 2024;10(12):e33193. doi:10.1016/j.heliyon.2024.e33193
34. Liu Y, Li Z, Meng Q, et al. Identification of the consistently differential expressed hub mRNAs and proteins in lung adenocarcinoma and construction of the prognostic signature: a multidimensional analysis. Int J Surg. 2024;110(2):1052–1067. doi:10.1097/js9.0000000000000943
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




