Back to Journals » Journal of Pain Research » Volume 18
Ultrasound-Guided Sural Nerve and Tibial Nerve Block Provides Comparable Analgesia to Popliteal Sciatic Nerve Block Following Calcaneal Surgery: A Single Center Randomized Controlled Double-Blind Study
Authors Yao J, Cai J, Lu Q, Huang X
Received 12 November 2024
Accepted for publication 21 March 2025
Published 1 April 2025 Volume 2025:18 Pages 1765—1773
DOI https://doi.org/10.2147/JPR.S506049
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jinlei Li
Jun Yao,1,2,* Jialin Cai,2,* Qingwang Lu,2 Xiaojing Huang3
1Department of Anesthesiology, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Shanghai, 200233, People’s Republic of China; 2Department of Anesthesiology, Jinjiang Municipal Hospital (Shanghai Sixth People’s Hospital Fujian Campus), Shanghai, Fujian, 362200, People’s Republic of China; 3Department of Pain Medicine, Shanghai Geriatric Medical Center, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaojing Huang, Department of Pain Medicine, Shanghai Geriatric Medical Center, No. 2560 Chunshen Road, Minhang District, Shanghai, 201104, People’s Republic of China, Email [email protected]
Background: Popliteal sciatic nerve blocks have gained popularity as an anesthesia choice for calcaneal surgery. While the simpler technique of sural and tibial nerve blocks offers potential, its safety and efficacy require validation through a head-to-head clinical study. This study compared the efficacy of ultrasound-guided sural and tibial nerve blocks (ST) with popliteal sciatic nerve block (PS) for operative and postoperative analgesia.
Methods: A total of 80 patients (40 per group) undergoing calcaneal surgery were randomized to receive either ST or PS nerve blocks. Patients in both groups were provided with an intravenous patient-controlled analgesia (PCA) device containing flurbiprofen. Visual analogue scale (VAS) pain scores were recorded at awakening, 2, 6, 12, and 24 h postoperatively. In addition, block onset time, procedure duration, patient satisfaction, and application of postoperative analgesics were also recorded.
Results: VAS scores were comparable between groups throughout the 24-hour observation period (VAS range 0– 3, p > 0.05). ST blocks demonstrated faster onset (8.2 ± 1.5 vs 12.4 ± 2.1 minutes, p< 0.001) and shorter procedure time (11.5 ± 2.1 vs 16.8 ± 2.4 minutes, p< 0.001). Patient satisfaction scores were similar between groups (8.5 ± 0.8 vs 8.3 ± 0.9, p=0.31).
Conclusion: Ultrasound-guided sural and tibial nerve blocks provide effective operative and postoperative analgesia comparable to popliteal sciatic nerve block. The blocks are easy to perform, have a faster onset, and achieve high patient satisfaction, making them a valuable alternative for calcaneal surgery.
Keywords: calcaneal surgery, ultrasound-guided, popliteal sciatic nerve block, tibial nerve block, sural nerve block
Background
Calcaneal fractures are frequently encountered in clinical settings, often characterized by marked post-fracture displacement. Conservative management is often less effective, necessitating surgical intervention in many cases.1,2 The surgical procedure typically entails an extended “L”-shaped incision along the lateral aspect of the heel, subsequent fracture reduction, and internal fixation using a plate. Placing the plate on the lateral side of the calcaneus is conducive to restoring its anatomical integrity, resulting in precise therapeutic outcomes.3,4 After surgical treatment of calcaneus fractures, particularly high pain intensities are observed.5 This can be attributed to the rich innervation of the calcaneus and the extensive dissection involved in the surgical approach. Appropriate pain management protocols are essential following these procedures to enable early rehabilitation and return to function.
Historically, spinal anesthesia and endotracheal intubation general anesthesia were the preferred anesthetic techniques for this surgery. However, limitations such as specific patient conditions and anticoagulation therapy curtailed the use of these methods. Currently, a more comfortable anesthesia approach is often achieved using a combination of regional nerve blocks with general anesthesia. Consequently, popliteal sciatic nerve blocks have gradually become the preferred choice for anesthesia and analgesia in calcaneal surgery.6 While effective, conventional preoperative popliteal blocks require patient repositioning, causing discomfort and potential refusal. With ultrasound guidance, popliteal blocks can now be performed without repositioning, through precise nerve localization with the patient supine. This avoids the significant discomfort of traditional popliteal blocks requiring repositioning and better meets the demands for maximizing patient comfort in calcaneal surgery.7
The tibial nerve innervates the plantar heel, while the sural nerve supplies the lateral heel and ankle. Targeting these nerves allows precise pain control with minimal anesthesia in other areas, making them critical for effective analgesia in calcaneal surgery. We hypothesize that ultrasound-guided sural and tibial nerve blocks will provide comparable postoperative analgesia to popliteal sciatic nerve blocks while improving procedural efficiency and patient comfort.
Methods
The trial was designed as a single-center, randomized, double-blind, parallel two-arm controlled study. It received ethical approval from the Medical Ethics Committee of Jinjiang Municipal Hospital, Shanghai Sixth People’s Hospital Fujian Campus (Ethical approval number: jjsyy 2024–005-1.0). The study was registered at the Chinese Clinical Trial Registry (https://www.chictr.org.cn, ChiCTR2400081163). The prospective registration date was February 26, 2024. Between March 2024 and September 2024, a total of 80 patients with an American Society of Anesthesiologists physical status classification of I–II, who were scheduled for internal fixation surgery due to calcaneal fractures at the Fujian Campus of Shanghai Sixth People’s Hospital, were enrolled in this study. Eligible patients were informed about the study, and written informed consent was obtained from them. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Patients were randomly assigned into two groups using a random number table: the ultrasound-guided sural nerve combined with tibial nerve block group (ST group) and popliteal sciatic nerve block group using the conventional popliteal fossa approach (PS group), with 40 patients in each group. Patients meeting the following criteria were excluded from the study: 1) Allergic reactions to local anesthetics; 2) Infection at the puncture site; 3) Central nervous system diseases or peripheral neuropathies; 4) Severe cardiovascular or cerebrovascular diseases; 5) Coagulation disorders; 6) Inability to communicate due to language barriers; 7) Opioid analgesic addiction.
Prior to surgery, all patients underwent a comprehensive preoperative evaluation, including a detailed medical history, physical examination, and routine laboratory tests. Patients were instructed on the use of the visual analog scale (VAS) for pain assessment and the patient-controlled analgesia (PCA) device. Standard monitoring (ECG, noninvasive arterial blood pressure, and pulse oximetry) was established, and intravenous access was secured with a balanced crystalloid infusion (maximum 500 mL).
General anesthesia was induced using propofol (3 mg/kg) and sufentanil (5 μg) via intravenous administration. A laryngeal mask airway (LMA) was inserted, and anesthesia was maintained with sevoflurane throughout the surgical procedure. In cases where signs of pain stimulation were observed based on heart rate, blood pressure, end-tidal carbon dioxide levels, and respiratory rate, supplementary doses of sufentanil were administered. Ephedrine was used to manage cases of hypotension.
Upon awakening in the Post-Anesthesia Care Unit (PACU), patients were connected to an intravenous PCA pump delivering a solution consisting of 200 mg of flurbiprofen, with an infusion rate of 2 mL/hr, a bolus dose of 0.5 mL, and a 15-minute lockout time. Pain assessment using the VAS was initiated at various time points postoperatively. If a patient reported an increase in pain with a VAS score exceeding 4, a rescue analgesic intervention was administered via intravenous injection of 10 mg of flurbiprofen, and this intervention was documented.
Patients in the ST group were positioned in a standard supine position with their lower limbs extended. After routine skin disinfection and draping, a high-frequency ultrasound probe (m9cv, frequency 4–12 MHz, Mindray, China) was positioned approximately 4–6 cm above the ankle for scanning, with depth adjusted accordingly. The tibial nerve was identified between the medial malleolus and the Achilles tendon, positioned posterior to the posterior tibial artery. The sural nerve was located between the lateral malleolus and the Achilles tendon, often accompanied by small saphenous veins. Using an in-plane anterior-to-posterior needling technique, both nerves were separately blocked with a 22-gauge, 50-mm needle. A total of 15 mL of 0.35% ropivacaine was used (5 mL for the sural nerve and 10 mL for the tibial nerve).
Patients in the PS group were positioned in a lateral decubitus posture with the blocked side facing upward, and the hip and knee joints were slightly flexed. After skin disinfection and draping, a high-frequency ultrasound probe (similar to the ST group) was placed at the crease of the popliteal fossa. The depth was adjusted, and the probe was shifted proximally to identify the popliteal artery, gastrocnemius muscle, semimembranosus muscle, and sciatic nerve. When the sciatic nerve was bifurcated, the probe was moved proximally to a point above the bifurcation. An in-plane technique was employed for the sciatic nerve block,7 administering 15 mL of 0.35% ropivacaine.
For the tibial nerve block, the probe was placed approximately 4–6 cm above the ankle, identifying the nerve between the medial malleolus and the Achilles tendon, posterior to the posterior tibial artery (Figure 1). For the sural nerve block, the probe was positioned between the lateral malleolus and the Achilles tendon, often accompanied by small saphenous veins (Figure 2). During the procedure, the needle was visualized in real-time to ensure accurate placement of the local anesthetic.
To ensure comprehensive blockade, the traceback technique was used to visualize the peroneal and tibial components within the same paraneurium. This ensured that both nerve components were adequately covered by the local anesthetic, enhancing the effectiveness of the block. These procedures were performed by the same experienced Anesthesiologist in both block methods.
Various parameters were recorded in both groups, including the duration of the nerve block procedure, onset times of sensory blockade for the sural and tibial nerve regions, total intraoperative sufentanil usage, surgical duration, nerve block duration (from block completion to sensory recovery), VAS pain scores upon awakening in the PACU and at 2, 6, 12, and 24 hours postoperatively, the number of rescue flurbiprofen administrations within the first 24 hours, and patient satisfaction levels. The primary outcome was postoperative VAS pain scores at awakening, 2, 6, 12, and 24 hours. Secondary outcomes included comparisons of puncture time, nerve block onset time, satisfaction with pain management, and postoperative analgesic application. The nerve block procedure time was evaluated using a stopwatch, measuring from patient positioning to local anesthetic injection completion, ensuring accuracy and consistency.
The sample size was calculated using the comparison of means formula according to primary outcome measurement on pain scores recorded at awakening, 2, 6, 12 and 24 h time points postoperatively. The results of a previous pilot study showed that the means of the ST group and PS group were 3.89 and 3.01 respectively, with a standard deviation (SD) of 1.26 in both groups. Using a two-sided t-test, 66 patients were required to achieve a power of 80% with an α value of 0.05 for detecting the differences between them. Taking into consideration possible dropouts (20%), 80 patients (40 in each group) were enrolled in the study.
Statistical analysis was conducted using IBM SPSS for Windows® version 23.0 software (SPSS, Chicago, IL, USA). The Kolmogorov–Smirnov test was used to determine the normality of data distribution. Continuous data were presented as mean ± standard deviation ( ), and median (25th–75th percentiles), and categorical variables as counts (percentages). Comparisons of normally distributed continuous variables between the groups were performed using Student’s t-test, while non-normally distributed continuous variables between the groups were compared using the Mann–Whitney U-test. Categorical data were expressed as counts (percentage), and between-group comparisons were assessed using the chi-square test. A two-sided P value <0.05 was considered statistically significant.
), and median (25th–75th percentiles), and categorical variables as counts (percentages). Comparisons of normally distributed continuous variables between the groups were performed using Student’s t-test, while non-normally distributed continuous variables between the groups were compared using the Mann–Whitney U-test. Categorical data were expressed as counts (percentage), and between-group comparisons were assessed using the chi-square test. A two-sided P value <0.05 was considered statistically significant.
Results
Of the 87 patients that were screened, 7 (8%) were excluded, and 80 (92%) underwent randomization between March 9, 2024 and September 13, 2024. A total of 80 participants (40 patients in ST group and 40 patients PS group ultimately completed the study (Figure 3). The patients’ characteristics were presented in Table 1. There was no statistical difference in terms of sex ratio, age, weight, ASA class, and duration of surgery.
 |
Table 1 Patients’ Characteristics |
 |
Figure 3 Flow chart of the study. |
The pain VAS scores after surgery were shown in Figure 4. There was no difference in VAS at between ST group and PS group at postoperative awakening, 2, 6, 12, and 24 h. Pain scores were comparable between the two groups (VAS range 0–3, p > 0.05).
 |
Figure 4 VAS at awakening, 2, 6, 12, and 24 h after surgery. |
The onset time of nerve block in ST group was significantly shorter than in PS group, and this difference was statistically significant (P < 0.001). However, there was no statistically significant difference in the onset time of tibial nerve blockade between the both groups. And, there was no significant difference in the duration of nerve blockade between the two groups. The time required to complete the sural and tibial nerve blocks was significantly less than that required for the sciatic nerve block, with statistical significance (P< 0.001). While there were no statistically significant differences observed in intraoperative sufentanil dosage, the number of postoperative rescues flurbiprofen administrations within 24 hours, or satisfaction with pain management (Table 2).
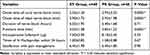 |
Table 2 Comparison of Different Variables for Two Groups |
Neither group of patients experienced adverse reactions such as vascular puncture, abnormal sensations during injection, or local anesthetic toxicity. Follow-up was conducted one week after discharge, during which no sensory or motor abnormalities or signs of nerve damage were observed.
Discussion
The study demonstrates that ultrasound-guided sural and tibial nerve blocks provide comparable postoperative analgesia to popliteal sciatic nerve blocks following calcaneal surgery. The findings align closely with our primary objective of evaluating the efficacy of selective nerve blocks and highlight their practical advantages, including reduced procedural time, quicker onset, and improved patient comfort. These results support the use of sural and tibial nerve blocks as a viable alternative to traditional sciatic nerve blocks, particularly in patients with mobility limitations.
Ultrasound-guided sciatic nerve block has multiple approaches, including the classical greater trochanter level, subgluteal, and popliteal fossa approaches, which are widely used in lower extremity surgery.8–10 Surgery for calcaneal fractures typically requires a lateral ankle incision, making sciatic nerve block the primary choice for both intraoperative anesthesia and postoperative analgesia. Although a new anterior thigh approach for sciatic nerve block has been proposed in recent years,11–13 studies and clinical practice have demonstrated that the popliteal fossa approach for sciatic nerve block is the simplest and most reliable technique.
The nerves involved in the calcaneus and its surrounding soft tissues include the saphenous nerve (from the femoral nerve), tibial nerve, and sural nerve.14–16 It has been found that the tibial nerve primarily controls the movement and sensation of the plantar region.17 Ultrasound-guided tibial nerve blocks have been used for procedures such as foreign object removal from the foot and treatment of frostbite injuries.18,19 Since calcaneal surgery often utilizes a lateral incision, the main nerves involved in the procedure are the tibial nerve and the sural nerve. Blocking these nerves above the ankle provides anesthesia coverage for the lateral aspect of the calcaneus and the skin of the sole, which aligns perfectly with the surgical site.
Previous research has demonstrated the effectiveness of combining the sural nerve block with the tibial nerve block for postoperative pain relief in calcaneal surgery.20 However, the use of combined ultrasound-guided sural and tibial nerve blocks above the ankle for anesthesia and pain management in calcaneal surgery, compared to the classical sciatic nerve block, remains unknown. This study aims to compare the operation time, onset time, analgesic effectiveness, and patient’s satisfaction with the classical popliteal sciatic nerve block, while also evaluating the feasibility of performing the nerve blocks without repositioning the patient.
In comparison to the classic popliteal sciatic nerve block, the sural nerve block and tibial nerve blocks had slightly shorter operation times, mainly due to the reduced repositioning time required for the conventional popliteal sciatic nerve block, particularly for patients with complex injuries who needed more time. The quicker onset of nerve block may be due to its status as a terminal branch of the sciatic nerve, with a smaller nerve diameter facilitating the rapid penetration of local anesthetic into nerve fiber components. Although there was a slight difference in block duration between the two groups, it was clinically insignificant. The duration of nerve block is influenced by various factors, including drug concentration and volume, the distance from the nerve, the degree of vascularization, and metabolism.21,22
During calcaneal surgery, opioid medications are used to control surgical stimuli, such as tourniquet placement, stimulation from the laryngeal mask, or internal fixation and reduction that may extend beyond the blockade area. When comparing popliteal sciatic nerve block with sural and tibial nerve blocks, both groups in this study had sufentanil dosages of less than 10 µg, and the clinical difference was negligible. Nerve blockade serves as the primary line of postoperative analgesia. In this study, the duration of blockade between the two techniques showed no significant difference and had no statistical significance. However, an important complication is rebound pain.23 Although the mechanism of rebound pain is currently a subject of debate, prolonged nerve blockade24 and the use of effective multimodal analgesia can help prevent it. The study utilized anti-inflammatory and analgesic drugs, combined with intravenous patient-controlled analgesia pumps and additional intravenous dosages, resulting in satisfactory pain relief in both groups. This multimodal analgesia approach significantly reduces the intraoperative use of opioid medications, with nerve blockade playing a major role in achieving this outcome.25,26
Compared to the popliteal approach for sciatic nerve blockade, selective blockade of the sural and tibial nerves provides comparable analgesia for calcaneal fracture repair while preserving ambulatory capability by sparing the common peroneal nerve. This allows patients to voluntarily mobilize and ambulate postoperatively, potentially mitigating risks of lower extremity deep vein thrombosis formation and subsequent pulmonary thromboembolism. Intact sensation also enables detection of impending compartment syndrome of the leg through pain and pressure, allowing timely medical intervention. Moreover, selective blockade greatly reduces the impact of nerve injury.27 Should minor nerve trauma occur, sensorimotor deficits would be confined to the corresponding distributions. Ultimately, selective blockade minimizes the extent of anesthesia to the surgical site, retaining autonomous mobility of the operative limb, averting restrictions from extensive blockade, and minimizing patient discomfort. In summary, compared to extensive sciatic nerve block, selective blockade of the sural and tibial nerves adequately fulfills the perioperative analgesic requirements for calcaneal fracture surgery while localizing the blockade, sparing uninvolved areas, preserving voluntary motor function, and reducing patient inconvenience.
This study has three primary limitations. First, there was no long-term postoperative assessment, as the evaluation period only extended to one week postoperatively, lacking an assessment of chronic complications. Second, the sample size in this study was quite small, so the results may require further validation through larger sample sizes. Third, only routine monitoring was applied, and bispectrality index (BIS) monitoring for anesthesia depth was not utilized. Future studies should consider longer-term follow-up to evaluate potential complications such as chronic pain or nerve injury. Additionally, larger multi-center trials are warranted to confirm the safety and long-term benefits of selective nerve blocks in diverse patient populations.
Conclusion
In conclusion, ultrasound-guided sural nerve and posterior tibial nerve blocks above the ankle provide satisfactory results for operative and postoperative analgesia in calcaneal surgery. The approach is as effective as the classic popliteal sciatic nerve block. It offers immediate postoperative limb mobility, and the potential for early postoperative mobilization. This approach is worthy of study and promotion by clinical practitioners.
Abbreviations
VAS, postoperative visual analog scales; PCA, patient-controlled analgesia; PACU, Post-Anesthesia Care Unit; LMA, laryngeal mask airway; BIS, bispectrality index.
Data Sharing Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This project was approved by Institutional Review Board of Jinjiang Municipal Hospital, Shanghai Sixth People’s Hospital Fujian Campus (Ethical approval number: jjsyy 2024-005-1.0). Written informed consent was obtained from participants.
Author Contributions
Jun Yao and Jialin Cai are co-first authors for this study. Jun Yao and Jialin Cai conceived and designed the study, participated in data acquisition and analysis, and drafted the manuscript. Qingwang Lu performed the statistical analysis and critically revised the manuscript for important intellectual content. Xiaojing Huang supervised the study, provided administrative support, and ensured the accuracy and integrity of the work. All authors made significant contributions to the conception, study design, execution, data acquisition, analysis, and interpretation. They all participated in drafting, revising, or critically reviewing the article, gave final approval of the version to be published, agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
This work was supported by the No funding was received for this study.
Disclosure
The authors declare that they have no competing interests in this work.
References
1. Wei N, Zhou Y, Chang W, Zhang Y, Chen W. Displaced intra-articular calcaneal fractures: classification and treatment. Orthopedics. 2017;40(6):e921–e929. doi:10.3928/01477447-20170907-02
2. Salameh M, Al-Hashki L, Al-Juboori S, Rayyan R, Hantouly A, Blankenhorn B. Management of displaced intra-articular calcaneal fractures; current concept review and treatment algorithm. Eur J Orthop Surg Traumatol. 2023;33(4):779–785. doi:10.1007/s00590-022-03264-5
3. Rammelt S, Swords MP. Calcaneal fractures-which approach for which fracture? Orthop Clin North Am. 2021;52(4):433–450. doi:10.1016/j.ocl.2021.05.012
4. Bajammal S, Tornetta P 3rd, Sanders D, Bhandari M. Displaced intra-articular calcaneal fractures. J Orthop Trauma. 2005;19(5):360–364.
5. Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934–944. doi:10.1097/ALN.0b013e31828866b3
6. Redborg KE, Sites BD, Chinn CD, et al. Ultrasound improves the success rate of a sural nerve block at the ankle. Reg Anesth Pain Med. 2009;34(1):24–28. doi:10.1097/AAP.0b013e3181933f09
7. Sepolvere G, Tedesco M, Cibelli M, et al. Technical report on the new ultrasound lateral mid-shaft approach to the sciatic nerve: a never-ending story. Medicina. 2025;61(1):100. doi:10.3390/medicina61010100
8. Li Y, Zhang Q, Wang Y, et al. Ultrasound-guided single popliteal sciatic nerve block is an effective postoperative analgesia strategy for calcaneal fracture: a randomized clinical trial. BMC Musculoskelet Disord. 2021;22(1):735. doi:10.1186/s12891-021-04619-5
9. Cataldo R, Carassiti M, Costa F, et al. Starting with ultrasonography decreases popliteal block performance time in inexperienced hands: a prospective randomized study. BMC Anesthesiol. 2012;12:33. doi:10.1186/1471-2253-12-33
10. Cooper J, Benirschke S, Sangeorzan B, Bernards C, Edwards W. Sciatic nerve blockade improves early postoperative analgesia after open repair of calcaneus fractures. J Orthop Trauma. 2004;18(4):197–201. doi:10.1097/00005131-200404000-00001
11. Pandin P, Vandesteene A, D’Hollander A. Sciatic nerve blockade in the supine position: a novel approach. Can J Anaesth. 2003;50(1):52–56. doi:10.1007/BF03020187
12. Wiegel M, Reske A, Hennebach R, et al. Anterior sciatic nerve block--new landmarks and clinical experience. Acta Anaesthesiol Scand. 2005;49(4):552–557. doi:10.1111/j.1399-6576.2005.00675.x
13. Wang L, Qu Y, Deng Y, Li J, Liu Y, Wu C. Evaluation of a new method of sciatic nerve block: a prospective pilot study. J Pain Res. 2023;16:2091–2099. doi:10.2147/JPR.S404489
14. Bianchi S, Droz L, Lups Deplaine C, Dubois-Ferriere V, Delmi M. Ultrasonography of the sural nerve: normal and pathologic appearances. J Ultrasound Med. 2018;37(5):1257–1265. doi:10.1002/jum.14444
15. Jackson LJ, Serhal M, Omar IM, Garg A, Michalek J, Serhal A. Sural nerve: imaging anatomy and pathology. Br J Radiol. 2023;96(1141):20220336. doi:10.1259/bjr.20220336
16. Riedl O, Frey M. Anatomy of the sural nerve: cadaver study and literature review. Plast Reconstr Surg. 2013;131(4):802–810. doi:10.1097/PRS.0b013e3182818cd4
17. Burl T, Latshaw P, Dreyfuss A. Ultrasound-guided posterior tibial nerve block for frostbite of the plantar surfaces: a case series. Clin Pract Cases Emerg Med. 2022;6(4):272–275. doi:10.5811/cpcem.2022.7.56727
18. Moake MM, Presley BC, Barnes RM. Ultrasound-guided posterior tibial nerve block for plantar foot foreign body removal. Pediatr Emerg Care. 2020;36(5):262–265. doi:10.1097/PEC.0000000000001897
19. Garcia Tomas V, DeLeon AM, Johnson PA, Vargas K, MacLyman S, Chung B. Proximal ultrasound-guided posterior tibial nerve block for the removal of calcaneal hardware. Cureus. 2023;15(6):e41047. doi:10.7759/cureus.41047
20. Farbood A, Asadi S, Amini A, et al. The effect of posterior tibial and sural nerve blocks on postoperative pain of patients following open reduction and internal fixation of calcaneal fractures. Foot Ankle Surg. 2022;28(7):858–862. doi:10.1016/j.fas.2021.11.009
21. Fournier R, Weber A, Gamulin Z. No differences between 20, 30, or 40 mL ropivacaine 0.5% in continuous lateral popliteal sciatic-nerve block. Reg Anesth Pain Med. 2006;31(5):455–459. doi:10.1016/j.rapm.2006.05.009
22. Migues A, Slullitel G, Vescovo A, Droblas F, Carrasco M, Perrin Turenne H. Peripheral foot blockade versus popliteal fossa nerve block: a prospective randomized trial in 51 patients. J Foot Ankle Surg. 2005;44(5):354–357. doi:10.1053/j.jfas.2005.07.005
23. Sort R, Brorson S, Gögenur I, Nielsen JK, Møller AM. Rebound pain following peripheral nerve block anaesthesia in acute ankle fracture surgery: an exploratory pilot study. Acta Anaesthesiol Scand. 2019;63(3):396–402. doi:10.1111/aas.13290
24. Hunt KJ, Higgins TF, Carlston CV, Swenson JR, McEachern JE, Beals TC. Continuous peripheral nerve blockade as postoperative analgesia for open treatment of calcaneal fractures. J Orthop Trauma. 2010;24(3):148–155. doi:10.1097/BOT.0b013e3181bfc9f7
25. O’Neill A, Lirk P. Multimodal Analgesia. Anesthesiol Clin. 2022;40(3):455–468. doi:10.1016/j.anclin.2022.04.002
26. Golembiewski J, Dasta J. Evolving role of local anesthetics in managing postsurgical analgesia. Clin Ther. 2015;37(6):1354–1371. doi:10.1016/j.clinthera.2015.03.017
27. Kahn RL, Ellis SJ, Cheng J, et al. The incidence of complications is low following foot and ankle surgery for which peripheral nerve blocks are used for postoperative pain management. HSS J. 2018;14(2):134–142. doi:10.1007/s11420-017-9588-y
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 4.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



