Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 20
Validation of an AI-Powered Smart Dry Powder Inhaler (RS01X) for Asthma and COPD in a Clinical Setting
Authors Chamaon D , Sportel E , Elferink ECM, van der Palen J
Received 24 September 2024
Accepted for publication 1 February 2025
Published 25 March 2025 Volume 2025:20 Pages 811—819
DOI https://doi.org/10.2147/COPD.S490684
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jill Ohar
Dumiana Chamaon,1,* Esther Sportel,2,* Emma CM Elferink,1,3 Job van der Palen4,5
1Department of Pulmonary Medicine, Medisch Spectrum Twente, Enschede, the Netherlands; 2Department of Clinical Pharmacy, Medisch Spectrum Twente, Enschede, the Netherlands; 3Faculty of Medicine, Radboud Universiteit, Nijmegen, the Netherlands; 4Department of Epidemiology, Medisch Spectrum Twente, Enschede, the Netherlands; 5Section Cognition, Data and Education, University of Twente, Enschede, the Netherlands
*These authors contributed equally to this work
Correspondence: Dumiana Chamaon, Email [email protected]
Introduction: The main treatment for patients with chronic obstructive pulmonary disease (COPD) or asthma is inhalation medication. Treatment efficacy is often suboptimal due to poor therapy adherence and errors in inhalation technique. The RS01XTM (RS01X) is a smart, single dose dry powder inhaler (smart DPI) that monitors therapy adherence and inhalation technique via inhalation profiles, consisting of duration, volume and peak inspiratory flow (PIF). The objective was to validate the smart DPI compared to an external inhalation profile recorder (IPR).
Methods: This monocenter cross-sectional study with 97 participants comprises patients with COPD, asthma and healthy participants. Participants performed three inhalations with the smart DPI. The inhalations differed in duration, volume and PIF, and orientation of the inhaler (horizontal (correct) and at a 45-degree angle (incorrect)). A paired sample t-test was performed to test for differences in the mean values between the smart DPI and the IPR. Also, the intraclass correlation coefficient (ICC) was calculated.
Results: The correlation between the smart DPI and the IPR shows for all the inhalation parameters an ICC > 0.95 (all p < 0.001). Analyses for healthy subjects, and patients with COPD and asthma show no relevant differences between the groups (all ICC > 0.93, all P < 0.001). Inhalations with the inhaler in an incorrect 45-degree angle show negligible but statistically significant differences on the parameters volume (0.44 milliliters) and PIF (1.5L/min) between IPR and smart DPI (P < 0.05).
Discussion: The smart DPI is a valid instrument for measuring inhalation parameters to improve therapy adherence and inhalation techniques in patients with asthma and COPD.
Keywords: dry powder inhaler, DPI, inhalation parameters, inhalation technique, single dose, smart inhaler, validation
Introduction
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death and the seventh leading cause of poor health globally. Additionally, asthma claimed the lives of 455,000 and affected an estimated 262 million people in 2019.1,2
The main treatment for patients with COPD or asthma is inhalation medication. The advantage lies in the direct delivery of the drug to the airways.3–5
Despite effective inhalation medication, treatment effect is often suboptimal due to poor therapy adherence and errors in inhalation technique.6,7 Effectiveness heavily relies on the correct administration technique. Errors related to inhalation maneuvers and device handling are frequently observed in both COPD and asthma patients when using inhalers.8,9
Consequences of these errors and lack of therapy adherence are an increase in exacerbations for both asthma and COPD patients and subsequently an increase in health care utilisation and costs.6 One way to correct these errors and adherence is via digital monitoring of the inhaler use and providing feedback.10,11
Smart-inhalers have the ability to record the time and date, and failure rate (eg, device malfunction) of every inhalation more accurately compared to measurement from patients, or using pharmacy records.12 Additionally, certain smart-inhalers have the possibility to measure air flow.13 Different studies have been performed with smart inhalers and its effect on therapy adherence; in these studies the use of a smart device increased therapy adherence.14,15
The RS01X (Berry Healthcare, Osnago; Amiko Digital Health, Milan) is a smart single dose dry powder inhaler (smart DPI) that can monitor therapy adherence and inhalation technique via inhalation profiles. Inhalation profiles consist of duration, volume, and peak inspiratory flow (PIF).16
This device has undergone a technical validation using Amiko employees, however, a validation in a clinical setting with patients with asthma or COPD is still missing and necessary before it can be integrated in respiratory patient care.
The objective of the present study is to validate the smart DPI compared to an external Inhalation Profile Recorder (IPR) in a real-life population of asthma and COPD patients and healthy volunteers in a clinical setting.
Patients and Methods
Study Design
A monocenter cross-sectional study was performed at Medisch Spectrum Twente (MST) in Enschede, the Netherlands from October 2023 till the end of December 2023. For this study 90 participants comprised of healthy volunteers, COPD patients, and asthma patients were required, all participants had to perform three inhalations on the smart DPI.
Study Population
The population in the study consisted of three groups: group 1 were asthma patients, group 2 COPD patients and group 3 healthy volunteers. Participants were eligible based on the following in- and exclusion criteria:
Inclusion Criteria
- Written informed consent
- ≥ 18 years of age
- Group 1: Clinically diagnosed asthma patients3
- Group 2: Clinically diagnosed COPD II–IV patients according to the Gold criteria; a forced expiratory volume within 80% of the reference value (FEV1 <80%)4
Exclusion criteria
- Low cognitive function
- Group 3: presence of any chronic pulmonary disease
Study Procedure / Setting
After informed consent was obtained, participants from all three groups were instructed on how to use the smart DPI. Then, they had to perform at least 3 successful inhalations through the smart DPI with empty capsules.
The three inhalations differed from one another. Initially, while maintaining the inhalator in the correct horizontal orientation – considered as 0-degrees – and executing a standard inhalation (measurement 1), subsequently, holding the inhalator horizontally and inhaling with greater force compared to the first inhalation (measurement 2), and lastly, adopting an incorrect 45-degree angle with the inhalator while engaging in a standard inhalation (measurement 3).
An external inhalation profile recorder (IPR) was attached to the smart DPI to validate the measurements of the smart inhaler. The IPR contains a differential pressure sensor (Honeywell – SSCDRNN005PD2A5). A digital auto-zero calibration is performed at the start of each recording to further correct output error including offset error, thermal effect on offset and offset drift. The data collected by the pressure sensor is converted to airflow data using the formula presented by Clark and Hollingsworth.17
Inhalation Parameters
The inhalation parameters used were the inhalation duration in seconds, the inhalation volume in liters, and the peak inspiratory flow (PIF) in liters/minute (L/min).
An inhalation was deemed “successful” when a minimum peak inspiratory flow of 15 L/min and a maximum of 120 L/min was reached; there was a minimum inhalation time of 0.5 seconds and a maximum of 4 seconds; the capsule spun as per the intended use of capsule based inhalers.
Primary Outcome
Determine the accuracy of the smart DPI by comparing the measurements to the IPR.
Secondary Outcome
Determine the accuracy of the smart DPI for healthy volunteers, the asthma patients and the COPD patients separately.
The study was conducted according to the Declaration of Helsinki, and the study was approved by the institutional review board at MST (approval number: K23-36).
Data Analysis
Descriptive Statistics
Information regarding age, sex, and health status (categorized as healthy or afflicted by a medical condition) of all participants was collected.
Statistical Analysis
Statistical analysis have been performed in IBM SPSS Statistics 2818 and R version 4.2.1.19 P-values <0.05 were deemed statistically significant. The required sample size was determined by an anticipated intraclass correlation coefficient (ICC) of 0.9, with a minimal acceptable ICC of 0.75, with an alpha of 5% and a power of 90%. A minimum of 26 participants per group were needed. Additionally, in order to assess the variations in measurements within each group, a minimum of 30 subjects per group was needed.
The data analysis was conducted on continuous non-clustered data. Data was deemed non-clustered due to per-protocol variations in inhalations within each patient. Consequently, each inhalation was individually analyzed. Continuous data was visually assessed to determine its normality. A paired samples t-test was performed to compare the means between the measurements obtained with the smart DPI and IPR. To quantify the level of agreement between two simultaneously measured values (smart DPI and IPR) on a continuous scale, a scatterplot was constructed and the ICC was calculated. A Bland Altman plot was employed to assess the consistency of the measurements across the range of values for PIF, volume, and duration of the inhalations.
Results
A total of 97 participants were included. The population (N = 97) consisted of three groups: asthma patients (N = 32), COPD patients (N = 30), and healthy volunteers with no lung diseases (N = 35). The mean ages in years were 54.6, 68.3 and 42.4 (Table 1).
 |
Table 1 Population Characteristics |
The mean inhalation duration was 2.3 seconds, mean volume was 1.7 liters, and mean PIF 62 L/min.
Only the third inhalation, with the inhaler in a 45-degree angle, as seen in Table 2, shows statistically significant differences on the parameters volume and PIF (P < 0.05).
 |
Table 2 Difference in Inhalation Parameter of the Smart DPI Versus the IPR |
Scatterplots were made for each inhalation parameter, to visualize the agreement between the smart DPI and the IPR (Figure 1).
 |
Figure 1 Scatterplots for the different inhalation parameters (duration in seconds, volume in liters, PIF in liters/minute). |
The correlation between the smart DPI and the IPR shows for all the inhalation parameters an ICC > 0.95 (all p < 0.001) (Table 3).
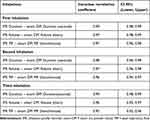 |
Table 3 Intraclass Correlation Coefficient of the Smart DPI Versus the IPR |
When performing the analyses with the data clustered for the three inhalations (N= 291 inhalations), the results showed that for the parameters Volume and PIF statistically significant differences in the mean were observed (Appendix Table 1, Appendix Figure 1). However, all ICC were 0.99 for all inhalation parameters (Table 4).
 |
Table 4 Intraclass Correlation Coefficient |
Sensitivity analyses were performed to assess consistency and systematic bias. The Bland Altman plots for volume and PIF show a few outliers, but no systematic biases (Figure 2).
The plot for inhalation duration seems to show a negative systematic deviation if duration > 4 seconds.
Separate analyses were performed for healthy subjects, and patients with COPD and asthma. Scatterplots were evaluated and ICC was calculated for all groups, showing no relevant differences between the groups. (all ICC > 0.93, all P < 0.001) (Appendix Table 2, Appendix Figure 2).
Discussion
The clustered and non-clustered data showed that the smart DPI can measure inhalation parameters very accurately, when compared to an inhalation profile recorder.
In the inhalation at an incorrect angle, the parameters volume and PIF showed very small, but statistically significant differences between the smart DPI and IPR. Participants performed the third inhalation whilst holding the inhaler at a 45-degree angle, which deviates from the standard inhalation protocol.20 The differences are so small, that they are inconsequential.
The participants with COPD where older and had a larger male population compared to the healthy and asthma population of the study. Since the prevalence of COPD is higher for males and those of older age,21 these participant characteristics correspond to their respective population.
The research protocol stated that the duration of a successful inhalation was between 0.5 and 4 seconds. However, during the measurements some participants inhaled longer than 4 seconds. Since both the smart DPI and the IPR recorded for more than 4 seconds, and longer inhalations is something that can occur in real life practice the definition of a successful inhalation was changed to: duration between 0.5 and 5 seconds. Therefore, more participants were able to remain in the analyses and it would better represent a real-life situation measurement. It is important to note that the Bland Altman plot seemed to show a negative systematic bias if duration was >4 seconds, but ICC values are high. This can be explained because the smart DPI was trained with inhalations according to protocol, so up to 4 seconds. This should be tested on more participants to see if this continues to occur. If so, the smart inhaler might need alterations in the software.
The data was considered non-clustered because participants received specific instruction for all the three inhalations.
Additionally, the software in the smart DPI is programmed to measure inhalation profiles based on how an empty capsule spins in the smart inhaler. If it is implemented in regular care the capsules will contain medication. This changes the conditions of the measurements and can potentially alter the results provided by this smart inhaler. To see if it makes a difference in the accuracy of the inhalation profiles measured by the smart DPI, this should be assessed in future research with patients inhaling their medication, to verify whether it influences the accuracy of the smart DPI inhalation profile measurements, compared to the IPR.
To the best of the researcher’s knowledge, this is the first study about the smart DPI smart inhaler, including patients with asthma or COPD. However, the possibility and the potential of smart inhalers to improve adherence has been shown in multiple studies.11,13
The RS01X is an upgrade from the RS01 inhaler. The RS01X compared to the RS01 has a built in sensor and digital capabilities with the performance of the RS01.22,23
Besides from build-in smart-inhalers (eg, RS01X), there are different electronic monitoring devices (EMD), such as digital inhaler add-ons.24 Current EMD’s can monitor adherence due to their ability to record when an inhaler is used and can notify when patients need to take their next dose, while some can also register inhalation parameters (eg, inspiratory flow).13,24,25 However, what sets the smart DPI (RS01X) apart from many digital inhalers is not only its ability to notify patients when to take medication, it also provides real time feedback to patients on whether an inhalation is performed successfully based on the measured parameters. Additionally, apart from EMD add-ons ability to improve adherence based on records on when to use the inhaler, if the add-on is too complicated to attach or use this will actually effect adherence negatively.24
Conclusion
There is a strong correlation between the measurements of the smart DPI and the IPR.
The smart DPI is a valid instrument for measuring inhalation parameters duration, volume, and peak inspiratory flow in a real-life population of asthma and COPD patients, if used according to protocol. The clinical validation of the Smart DPI device and the accurate measurement of inhalation parameters, could aid in the assessment of therapy adherence and inhalation technique by physicians prior to upscaling the therapy. This is conform GINA/ GOLD guidelines.
Data Sharing Statement
The data that support the findings of this work are available from the corresponding author upon request. All data provided will be anonymized and terms for usage will be agreed in advance.
Acknowledgments
The smart DPI (RS01XTM) device was provided by Berry Healthcare.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that there are no relevant material or financial interests that relate to the described research and the finding in this work.
References
1. WHO. Chronic obstructive pulmonary disease (COPD). Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd). (2023).
2. Organization WH. Asthma. 2024. Available from: https://www.who.int/news-room/fact-sheets/detail/asthma#:~:text=Asthma%20affected%20an%20estimated%20262,and%20caused%20455%20000%20deaths.
3. GINA. Global Strategy for Asthma Management and Prevention, 2022. Available from: www.ginasthma.org2022.
4. Disease GIfCOL. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2023). Available from: www.goldcopd.org2023.
5. Gregoriano C, Dieterle T, Breitenstein AL, et al. Use and inhalation technique of inhaled medication in patients with asthma and COPD: data from a randomized controlled trial. Respir Res. 2018;19(1):237. doi:10.1186/s12931-018-0936-3
6. Usmani OS, Lavorini F, Marshall J, et al. Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res. 2018;19(1):10. doi:10.1186/s12931-017-0710-y
7. Kocks JWH, Chrystyn H, van der Palen J, et al. Systematic review of association between critical errors in inhalation and health outcomes in asthma and COPD. NPJ Prim Care Respir Med. 2018;28(1):43. doi:10.1038/s41533-018-0110-x
8. George M. Adherence in Asthma and COPD: new Strategies for an Old Problem. Respir Care. 2018;63(6):818–831. doi:10.4187/respcare.05905
9. Chrystyn H, van der Palen J, Sharma R, et al. Device errors in asthma and COPD: systematic literature review and meta-analysis. NPJ Prim Care Respir Med. 2017;27(1):22. doi:10.1038/s41533-017-0016-z
10. Dekhuijzen R, Lavorini F, Usmani OS, van Boven JFM. Addressing the impact and unmet needs of nonadherence in asthma and chronic obstructive pulmonary disease: where do we go from here? J Allergy Clin Immunol Pract. 2018;6(3):785–793. doi:10.1016/j.jaip.2017.11.027
11. Bosnic-Anticevich S, Bakerly ND, Chrystyn H, Hew M, van der Palen J. Advancing digital solutions to overcome longstanding barriers in asthma and COPD management. Patient Prefer Adherence. 2023;17:259–272. doi:10.2147/PPA.S385857
12. Chan AH, Reddel HK, Apter A, Eakin M, Riekert K, Foster JM. Adherence monitoring and e-health: how clinicians and researchers can use technology to promote inhaler adherence for asthma. J Allergy Clin Immunol Pract. 2013;1(5):446–454. doi:10.1016/j.jaip.2013.06.015
13. Chan AHY, Pleasants RA, Dhand R, et al. Digital inhalers for asthma or chronic o bstructive pulmonary disease: a scientific perspective. Pulmonary Ther. 2021;7(2):345–376. doi:10.1007/s41030-021-00167-4
14. Moore A, Preece A, Sharma R, et al. A randomised controlled trial of the effect of a connected inhaler system on medication adherence in uncontrolled asthmatic patients. Eur Respir J. 2021;57(6):2003103. doi:10.1183/13993003.03103-2020
15. Sulaiman I, Greene G, MacHale E, et al. A randomised clinical trial of feedback on inhaler adherence and technique in patients with severe uncontrolled asthma. Eur Respir J. 2018;51(1):1701126. doi:10.1183/13993003.01126-2017
16. RS01X. Connected and intelligent single-dose dry powder inhaler. Available from: https://rs01x.com/.
17. Clark AR, Hollingworth AM. The relationship between powder inhaler resistance and peak inspiratory conditions in healthy volunteers--implications for in vitro testing. J Aerosol Med. 1993;6(2):99–110. doi:10.1089/jam.1993.6.99
18. Corp I. IBM SPSS Statistics for Windows.
19. Team RC. R: A Language and Environment for Statistical Computing.
20. Salbutamol. Cyclohaler. 2024. Available from: https://inhalatorgebruik.nl/nl/inhalator/cyclohaler/144/salbutamol--cyclohalercyclohaler.
21. GOLD. GLOBAL STRATEGY FOR PREVENTION, DIAGNOSIS AND MANAGEMENT OF COPD: 2024 Report. Global Initiative for Chronic Obstructive Lung Disease – GOLD. 2024; 18: 0–10.
22. BERRY. RS01-X digital capsule based DPI. Available from: https://www.berryglobal.com/en/product/product-item/rs01x-digital-capsule-based-dpi-13207315.
23. BERRY. Berry global’s leading single-dose DPI goes digital. 2020.Available from: https://www.berryglobal.com/en/news/articles/berry-globals-leading-single-dose-dpi-goes-digital.
24. van de Hei SJ, Stoker N, Flokstra-de Blok BMJ, et al. Anticipated barriers and facilitators for implementing smart inhalers in asthma medication adherence management. Npj Primary Care Respiratory Medicine. 2023;33(1):22. doi:10.1038/s41533-023-00343-w
25. Zabczyk C, Blakey J. The effect of connected “smart” inhalers on medication adherence. Front Med Technol. 2021;3. doi:10.3389/fmedt.2021.657321
 © 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2025 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


