Back to Journals » Nature and Science of Sleep » Volume 16
Validation of the Athens Insomnia Scale Among Young Chinese Male Population in a High-Altitude Situation
Authors Tang X, Wang Q, Li S, Li X, Xin Q, Yang Y
Received 21 May 2024
Accepted for publication 11 September 2024
Published 17 September 2024 Volume 2024:16 Pages 1377—1386
DOI https://doi.org/10.2147/NSS.S475497
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sarah L Appleton
Xugang Tang,1 Qiang Wang,1 Shuang Li,1 Xiuchuan Li,1 Qian Xin,2 Yongjian Yang1
1Department of Cardiology, The General Hospital of Western Theater Command, Chengdu, Sichuan, People’s Republic of China; 2Department of Cardiology, The Sixth Medical Center of Chinese PLA General Hospital, Beijing, People’s Republic of China
Correspondence: Yongjian Yang, Department of Cardiology, The General Hospital of Western Theater Command, Chengdu, Sichuan, People’s Republic of China, Tel/Fax +86 28 8657 1255, Email [email protected]
Purpose: The Athens Insomnia Scale (AIS) is a widely used and authorized questionnaire for evaluating insomnia symptoms. However, its reliability and validity at high altitudes are uncertain. Therefore, this study aimed to confirm the validity and reliability of AIS during a 3658 m altitude exposure.
Patients and Methods: A total of 387 young Chinese males were enlisted in the acute high-altitude exposure group. They flew for about two hours, climbing from 400 m to 3658 m. The high-altitude-acclimated group consisted of 86 young Chinese men who had lived at least six months at 3658 m altitude. The sleep quality of the acute high-altitude exposure group was evaluated using the AIS before the ascent and after exposure to 3658 m for 24 hours, and one week. The sleep quality of the high-altitude-acclimated group was also assessed. The AIS’s internal consistency, reliability, and validity were evaluated.
Results: The respondents’ quality of sleep significantly decreased after being exposed to 3658 m as opposed to 400 m. Two factors comprised the AIS, according to an exploratory factor analysis: “sleep problem” (items 1– 5) and “daytime dysfunction” (items 6– 8). The Cronbach’s α internal consistency coefficients exceeded 0.8, and the corrected item-total correlations were all greater than 0.5 when the subjects were exposed to 3658 m. The model fit index was well within the criterion. The average variance extracted and composite reliability were all higher than 0.5 and 0.7, respectively. The interclass correlation coefficient was deemed “fair to good” at 0.482, which is greater than the 0.4 threshold. The AIS has satisfactory discriminant validity, as shown by the Fornell-Larcker criterion and cross-loading results. The daytime dysfunction R-square values (> 0.33) show that the frameworks have considerable predictive accuracy.
Conclusion: The AIS exhibits strong consistency, reliability, and validity. The AIS’s features and simplicity make it an essential psychometric tool for high-altitude sleep research.
Keywords: athens insomnia scale, high altitude, internal consistency, reliability, sleep, validity
Introduction
Ascending to altitudes above 2500 m can lead to acute mountain sickness (AMS), which is a common condition characterized by headaches, dizziness, gastrointestinal symptoms (eg, anorexia, nausea, or vomiting), weakness or fatigue, and sleep disturbance.1 Sleep disturbance is one of the most commonly reported symptoms of acclimatization to hypobaric hypoxia, and it is evaluated using the Lake Louise AMS scoring system. For the sleep quality item, subjects report whether they slept as well as usual (0 points), did not sleep as well as usual (1 point), woke up many times/had a poor night’s sleep (2 points), or could not sleep at all (3 points).1 Restful sleep is essential to perform work optimally the next day. However, sleep disturbance can worsen headaches and anxiety and cause daytime dysfunction after exposure to high altitudes.2 In addition to causing general discomfort, aggravating anxiety, despair, and other negative feelings, poor sleep quality can also accelerate the onset of AMS and impair cognitive function during the day.3 Low oxygen and low pressure-related sleep disturbances have become prevalent for those living at high altitudes, with detrimental effects on both physical and mental well-being.4,5 Research on sleep at high altitudes carries significant implications for enhancing the quality of life and sleep health of those who visit or live in high-altitude areas.6 Polysomnography is an effective method for diagnosing sleep disorders. Still, it is expensive and time-consuming, which limits its use in high-altitude environments.7 Several insomnia-related, self-rating scales are currently available for evaluating subjective sea-level sleep quality. The Pittsburgh Sleep Quality Index (PSQI),8–10 Insomnia Severity Index (ISI),11,12 and Athens Insomnia Scale (AIS)13–15 are commonly used and authorized insomnia symptom questionnaires. The AIS is considered a handy tool in clinical and research settings for clarifying the state of insomnia. It is more effective than the PSQI and the ISI in evaluating changes in sleep.16 The AIS has been translated into several languages, including English,17 French,18 Greek,19 Arabic,20 Japanese,21 and Spanish,22 and it is utilized by a variety of populations across the world. Additionally, the Chinese version of the AIS has been validated among both cancer patients23 and Chinese athletes.24 Several studies have used AIS to evaluate changes in sleep in subjects following high-altitude exposure,2,25,26 but more research is needed to determine the reliability and validity of the AIS for evaluating changes in sleep in subjects following high-altitude exposure.
Therefore, the current study aimed to validate the reliability and validity of the AIS for the assessment of altitude-related sleep disturbances in subjects following rapid exposure to 3658 m. Here we tested the hypothesis that the AIS is accurate enough to estimate sleep disturbances in a high-altitude setting.
Materials and Methods
Study Design
This research was conducted in May 2023, at two different altitudes in Southwest China: 400 m and 3658 m. The participants underwent baseline tests one week before starting their journey while they were at the 400 m altitude. A flight of almost two hours was needed to ascend from 400 m to 3658 m. After spending 24 hours and one week at the high-altitude location, high-altitude measurements were taken. In addition, another group of participants who had spent more than 6 months at 3658 m as a control group underwent the same test. All participants followed the same daily routine and avoided strenuous exercise during the journey. They also ate the same foods and stayed in the same barracks. The flowchart of the present study is presented in Figure 1.
 |
Figure 1 Flowchart. |
Subjects
We selected male lowlanders from locations below 500 meters who had not been exposed to high altitudes in the past six months, had no cardiovascular or respiratory problems, and did not use any prescription or non-prescription drugs. For the high-altitude acclimated group, volunteers had to meet the above-mentioned criteria, in addition to having stayed at high altitudes for at least six months. We excluded participants who had respiratory disease, cardiovascular or cerebrovascular disease, kidney or liver disease, or malignant tumors. All participants provided written consent and could withdraw from the study at any time. The study was conducted according to the Declaration of Helsinki and approved by the Ethics Committee of the General Hospital of Western Theater Command of the People’s Liberation Army (Approval identifier: 2022EC3-ky062).
We recruited a total of 419 young Chinese men, aged 18 to 37, at 400 m. At 3658 m, we recruited a total of 86 young Chinese men, aged 18 to 38, as part of the high-altitude-acclimated group. All participants were males, and a regular training component was in high altitudes. All participants were in good physical condition, as evidenced by chest X-ray, echocardiogram, and electrocardiogram tests.
Screening of the Study Subjects
The study conducted clinical investigations, such as resting heart rate (HR), blood pressure (BP), pulse oximeter saturation (SpO2), chest X-ray, echocardiography, and electrocardiogram, for one week before the trip. The purpose of these investigations was to eliminate patients with pulmonary and cardiovascular disorders from the study. Additionally, a questionnaire was used to gather demographic parameters, including age, weight, body mass index (BMI), and current drinking and smoking habits of the participating individuals.
Measurements of Physiological Parameters
After completing the questionnaires, we measured the participants’ resting HR (using OMRON HEM-6200; Omron Health Care, Inc., Bannockburn, IL, USA) and SpO2 (using Onyx 9500; Nonin Medical, Inc., Plymouth, MN, USA) three times consecutively, with approximately half-minute intervals between each measurement. We then calculated the mean of the three measurements and used it for our analysis.
Assessment of Sleep Quality Using the AIS
In this study, the AIS was used to assess the subjects’ sleep quality before and after exposure to high altitudes. The AIS consists of eight items that are rated on a 4-point scale ranging from 0 (no problem) to 3 (severe problem).17 The scale is designed to measure the subjective sleep quality of the participants over the past month. A higher score on the AIS indicates poorer sleep quality and a total score of 6 or more is considered insomnia. Studies have shown that using a score of 6 or more on the AIS as a threshold for insomnia diagnosis has a sensitivity of 92% and specificity of 66% at sea level.27 The reliability of the AIS was found to be very satisfactory at sea level, with Cronbach’s alpha of 0.89.17 To measure test-retest reliability, the subjects were assessed using the AIS three times a week apart, before and after being exposed to high altitudes.
Statistical Analysis
The data are presented as mean ± SD or n (%), as appropriate, and were analyzed using IBM SPSS22.0. The study used a significance level of p<0.05 for two-sided tests. The distribution of quantitative variables was tested for normality using the Kolmogorov–Smirnov test. Mean values were compared using a t-test, while the Pearson chi-squared test was used for comparing categorical variables.
The data analysis included exploratory factor analysis (EFA), confirmatory factor analysis (CFA), reliability analysis, and structural equation modeling (SEM). The AIS’s reliability and EFA were assessed using SPSS22.0, while CFA and SEM were performed using Mplus 8.3 and SmartPLS 4.1. The indirect impact test in SEM was conducted 5000 times using bootstrapping.
In the EFA study, the factors were extracted using principal component analysis and the maximum variance rotation approach, with components having eigenvalues greater than 1.0. If the explained variance of the first factor before rotation is <50%, it indicates no significant common method bias.28
We followed the guidelines provided by Hair et al17 for CFA and SEM analysis. To evaluate the model fit, we employed indices such as χ2/df <5, Root Mean Square Error of Approximation (RMSEA) <0.10, Standardized Root Mean Square Residual (SRMR) <0.05, Comparative Fit Index (CFI) >0.90, and the Tucker-Lewis Index (TLI) >0.90. To ensure the AIS’s convergent validity, Average Variance Extracted (AVE) (>0.5) and Construct Reliability (CR) (>0.7) were calculated using factor loadings. To determine the AIS’s discriminant validity, the Fornell-Larcker criterion and cross-loadings were used.
We used Cronbach’s α and corrected item-total correlations (CITC) in the AIS’s reliability analysis to determine the internal consistency coefficients, which had to be greater than 0.729 and 0.4,30 respectively. For the evaluation of the test-retest reliability of the AIS, we computed the interclass correlation coefficient (ICC) by comparing the item scores of the data from the AIS, which had to be greater than 0.4.31
Results
Clinical Characteristics
At 400 m, we signed up 419 young Chinese males as the acute high-altitude exposure group. However, incomplete data prevented 32 patients from participating in the data analysis. At 3658 m, we recruited a total of 86 young Chinese men as part of the high-altitude-acclimated group. Table 1 displays the clinical features of the sample. The BMI, drinking, and smoking patterns of the acute high-altitude exposure group and the high-altitude-acclimated group did not differ significantly, except in age.
 |
Table 1 Characteristics of the Sample |
HR and SpO2
In this study, we used participants’ heart rate and oxygen saturation to observe the trend of altitude adaptation, as these indicators were used to measure altitude acclimation.32 Table 2 shows that HR in the acute high-altitude exposure group increased considerably after exposure to 3658 m (p<0.01). The opposite pattern was observed for SpO2. The HR of the high-altitude-acclimated group was 79.8 ± 12.1 beats/min, substantially lower than that of the acute high-altitude exposure group (p<0.001). The high-altitude-acclimated group had a considerably higher SpO2 (91.2 ± 2.3%) than the acute high-altitude exposure group (p<0.05).
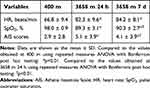 |
Table 2 Changes in HR, SpO2, and AIS Scores of the Acute High-Altitude Exposure Group After High-Altitude Exposure |
AIS Score
The acute high-altitude exposure group’s AIS scores significantly increased after exposure to 3658 m (p<0.01) (Table 2). After staying for 7 days at 3658 m, the AIS scores in the acute high-altitude exposure group decreased significantly as compared to the values obtained at 3658 m 24 h (p<0.01). The high-altitude-acclimated group had significantly higher AIS scores (5.9 ± 4.6) than the acute high-altitude exposure group remaining for 7 days at 3658 m (p<0.01) and insomnia prevalence (38/86 vs 121/387, p<0.05). Changes in each item of the AIS of the acute high-altitude exposure group after high-altitude exposure are presented in Table S1.
Measurement Model
The results of the EFA study indicate that the AIS is a valid instrument. The Kaiser-Meyer-Olkin measure value was 0.845 (p<0.001) for 400 m, 0.900 (p<0.001) for 3658 m 24 h, and 0.892 (p<0.001) for 3658 m 7 days, respectively. All values were greater than 0.7, which indicates that the instrument was suitable for factor analysis. Based on the eigenvalue criteria, the study identified two primary factors: Factor 1 (f1) = 3.339, which related to sleep issues (items 1–5), and Factor 2 (f2) = 1.022, which dealt with dysfunction throughout the day (items 6–8). The first factor explained 41.737% of the variance before rotation, suggesting no significant common method bias. The two factors combined explained 54.513% of the variance.
A study was conducted to evaluate the structural validity of the AIS using CFA. Table 3 shows the model fit index. The results indicated that the fit for the AIS items was acceptable. All standardized factor loadings were within a good range of 0.576–0.880 when the subjects were exposed to 3658 m (Figure 2), confirming the indicators’ reliability.
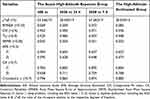 |
Table 3 The AIS’s Reliability and Validity Indices |
 |
Figure 2 Construct reliability and validity of the AIS. (A) 400 m altitude. (B) 3658 m 24 hours. (C) 3658 m 7-day. (D) 3658 m 6-month. |
The values of AVE of f1 and f2 were both higher than 0.5 when the subjects were exposed to 3658 m, confirming the convergent validity of the constructs. The CRs were all higher than 0.7 when the subjects were exposed to 3658 m, which approves the reliability of the constructs (Table 3).
The EFA study’s internal consistency coefficient test revealed the reliability of the AIS. Table 3 shows that all Cronbach’s α values for the AIS exceeded 0.7. The CITC were all greater than 0.5 when the subjects were exposed to 3658 m, demonstrating good internal consistency.
For the AIS total scores, the ICC value was 0.261 (subjects remaining at 400 m vs 3658 m for 24h, p<0.001) and 0.482 (subjects staying at 3658 m for 24 h vs 3658 m for 7 days, p<0.001), respectively. When the subjects were exposed to 3658 m, the ICC value (0.482, >0.4) was deemed “fair to good”,31 indicating acceptable test-retest reliability. Table S2 displays the ICCs for each item.
Convergent and Discriminant Validity
We used two methods, namely the Fornell-Larcker criterion, and cross-loadings, to evaluate the discriminant validity of the AIS. The Fornell-Larcker criterion states that the square root of AVE should be greater than the correlation to every other latent variable for each latent variable.29 On the other hand, cross-loadings require that each indicator’s loading should be greater than all its cross-loadings. The results of our analysis are presented in Table S3–10. Based on our findings, we conclude that the AIS has satisfactory convergent and discriminant validity and reliability.
The present study aimed to measure the variance inflation factor (VIF) values to identify any collinearity issues in the Framework. As per previous research,33 if the VIF value is <5, then the results are considered to be free of collinearity issues. The inner VIF values for all constructs ranged from 1.161 to 2.966. The results indicate that there are no collinearity issues with the data and that the survey findings are reliable and stable.
Predictive Accuracy
In this study, a bootstrapping technique was utilized to evaluate a hypothesis using 5000 samples.34 The structural model was assessed using the R-square, which is a measure of how well the model fits the data.35 According to Hair et al’s proposal, an R-square value above 0.33 is considered moderate. As shown in Table S11, the R-square values for daytime dysfunction (3658 m 24-hour), daytime dysfunction (3658 m 7-day), and daytime dysfunction (3658 m 6-month) were 41.3%, 42.2%, and 49.5%, respectively. These results indicate that the frameworks have moderate predictive accuracy.
The study found that sleep has a positive influence on daytime function when individuals are exposed to high altitudes, as hypothesized. The positive impact of sleep on daytime function was observed in subjects exposed to 3658 m (Table 4). These findings support the hypothesis.
 |
Table 4 Hypothesis Testing |
Discussion
To the best of our knowledge, this is the first study to examine the consistency, reliability, and validity of the AIS in a high-altitude situation. In this study, we validate the AIS using a large sample of young Chinese males. Our study found that participants exposed to 3658 m had Cronbach’s α values greater than 0.8 for AIS and 0.5 for CITC, respectively. The ICC results for AIS total scores indicated that the AIS had acceptable test-retest reliability. The Kaiser-Meyer-Olkin measure values were all greater than 0.8. The structural validity of the AIS was satisfactory (Table 3 and Table S3–10). The administration and evaluation of AIS in a high-altitude situation revealed that this scale is very dependable, practical, and simple to use. Furthermore, the AIS’s consistency, reliability, and validity were proven to be excellent in high-altitude conditions.
In the present study, we observed an increase in HR and a decrease in SpO2 when the subjects were rapidly exposed to 3658 m, consistent with the previous studies2,36 and the progress of acclimatization at high altitudes.32
High altitude conditions have a significant impact on sleep.37 Inadequate sleep can lead to high-altitude daytime dysfunction, emotional instability, and disrupted cognitive functioning.38 Despite the inherent limitations of subjective measures, questionnaires offer the benefit of being time and financially efficient. They also make it possible to gather large, longitudinal datasets within subjects, which can be used to investigate cause-and-effect relationships and the predictive power of various variables (eg, sleep quality and consequences linked to health). AIS was one of the questionnaires that was used to assess the change in high altitude-related sleep quality.2,25,26 In this study, we showed that a high-altitude environment affects participants’ subjective sleep quality over the short and long term (Table 2). Moreover, we examined the consistency, validity, and reliability of the AIS in a high-altitude environment.
Consistency of the AIS
Our study found that the AIS had very satisfactory internal consistency when subjects were exposed to 3658 m. Cronbach’s α values were good (Table 3). This indicates a high level of homogeneity of the AIS, which is further supported by the finding that Cronbach’s α remained very high among high-altitude-acclimated subjects (Cronbach’s α: 0.882). However, Cronbach’s α was slightly lower when subjects stayed at 400 m (Cronbach’s α: 0.796). One possible reason for this may be that smaller subjects staying at 400 m suffered from sleep disturbance. In previous research, non-patient controls had a lower Cronbach’s α of 0.75, while patients with primary insomnia and psychiatric patients had a higher Cronbach’s α of equal to or greater than 0.85.17 This may be because fewer subjects from the non-patient controls suffered from sleep disturbance compared to subjects from the primary patients with primary insomnia and psychiatric patients. Therefore, our results are supported by the research.
Moreover, when the subjects were exposed to 3658 m, all of the CITCs were larger than 0.5, further demonstrating the AIS’s good internal consistency.
Reliability of the AIS
For the AIS total scores, the ICC value was relatively low. However, the ICC value for the AIS total scores was significantly increased when the subjects were exposed to 3658 m for 7 d, which was greater than 0.4, as proposed by Fleiss et al.31 This may indicate that the effect of the high-altitude environment on sleep quality persists with prolonged altitude exposure, which is supported by that the insomnia prevalence in the high-altitude-acclimated group was higher than that in the acute high-altitude exposure group. The estimated test-retest reliability score for the AIS in clinical samples, according to a meta-analysis by Jahrami et al, is 0.84 at sea level,7 and 0.64 for another clinical study by Enomoto et al.39 Differences in the research contexts and samples may account for the discrepancy between Jahrami et al’s and Enomoto et al’s and our results. Therefore, we believe that the total score test-retest coefficient for the AIS may continue to rise as the duration of exposure to the plateau continues to increase and then maintain a stable level, which needs further study to verify.
Validity of the AIS
Our EFA investigation revealed two main components in the AIS: sleep problem (items 1–5) and daytime dysfunction (items 6–8), which is consistent with the other research.16,39,40 Furthermore, the current study’s eigenvalue values and factor loadings matched those reported by Sattler et al40 and Enomoto et al.39 The structures in the AIS were considered good as all the factor loadings of the items were above 0.5, the AVEs were greater than 0.5, and the CRs were above 0.7 when the subjects were at an altitude of 3658 m (Figure 2 and Table 3). The square root of the AVEs in the current study were all greater than the correlation to every other latent variable for each latent variable. Each item’s loading was greater than all of its cross-loadings, as determined by the Fornell-Larcker criterion and cross-loadings, which are used to assess the discriminant validity of the AIS (Table S3–10). In addition, our results (all the VIF <3) indicate that there are no collinearity issues with the data and that the survey findings are reliable and stable.
Lastly, the R-square values for daytime dysfunction at high altitudes were all greater than 0.33,35 which indicates that the frameworks have moderate predictive accuracy (Table S11). The hypothesis that sleep quality has a positive influence on daytime function when individuals are exposed to high altitudes was verified (Table 4).
In total, the findings of the present study suggested that the model of two factors with 8 items of the AIS showed a good fit and achieved construct validity in a high-altitude environment.
This study has several limitations that need to be considered. Firstly, the results are based on self-reported measures, which are prone to response and information bias, and therefore may not be entirely accurate. Secondly, due to limited existing research in the highlands, there is no gold standard for evaluating the AIS’s criterion validity. Finally, the sample used in this study only included young Chinese males, which means that females and older individuals were not represented, thus limiting the generalizability of the findings. These limitations should be taken into account when interpreting the results, and future studies should aim to address these issues.
Conclusion
In conclusion, the AIS is a scale that may be used in a wide range of clinical and research settings to quantify sleep difficulties. The AIS exhibits strong consistency, reliability, and validity. The AIS’s features and simplicity make it an essential psychometric tool in sleep research in high-altitude situations.
Data Sharing Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Acknowledgments
The authors would like to express their gratitude to all the subjects and investigators who participated in the research.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Major Military Logistics Research Projects (grant no. AWS21J004).
Disclosure
The study obtained written informed consent from all participants and was approved by the Ethics Committee of the General Hospital of Western Theater Command of People’s Liberation Army (Approval identifier: 2022EC3-ky062). The author(s) report no conflicts of interest in this work.
References
1. Roach RC, Bärtsch P, Hackett PH, et al. Hypoxia and molecular medicine. In: Sutton JR, Houston CS, Coates G, editors. The Lake Louise Acute Mountain Sickness Scoring System. Burlington, VT: Queen City Printers; 1993:272–274.
2. Tang XG, Li XC, Xin Q, Wang Q, Li S, Yang YJ. Anxiety as a risk factor for acute mountain sickness among young Chinese men after exposure at 3800 m: a cross-sectional study. Neuropsychiatr Dis Treat. 2023;19:2573–2583. doi:10.2147/NDT.S436438
3. de Aquino Lemos V, Antunes HK, Dos Santos RV, Lira FS, Tufik S, de Mello MT. High altitude exposure impairs sleep patterns, mood, and cognitive functions. Psychophysiology. 2012;49(9):1298–1306. doi:10.1111/j.1469-8986.2012.01411.x
4. Guan W, Ga Q, Li R, et al. Sleep disturbances in long-term immigrants with chronic mountain sickness: a comparison with healthy immigrants at high altitude. Respir Physiol Neurobiol. 2015;206:4–10. doi:10.1016/j.resp.2014.11.007
5. Li Q, Guo Z, Liu F, Liu Y, Bao D, Zhou J. The effects of altitude-related hypoxia exposure on the multiscale dynamics of blood pressure fluctuation during sleep: the observation from a pilot study. Nat Sci Sleep. 2021;13:1147–1155. doi:10.2147/NSS.S319031
6. Tan L, Li Y, Chen H, Lanzi G, Hu X. Sleep at high altitude: a bibliometric study and visualization analysis from 1992 to 2022. Heliyon. 2023;10(1):e23041. doi:10.1016/j.heliyon.2023.e23041
7. Nussbaumer-Ochsner Y, Schuepfer N, Siebenmann C, Maggiorini M, Bloch KE. High altitude sleep disturbances monitored by actigraphy and polysomnography. High Alt Med Biol. 2011;12(3):229–236. doi:10.1089/ham.2010.1073
8. Wang H, Li J, Liu Q, et al. Physical activity attenuates the association of long-term exposure to nitrogen dioxide with sleep quality and its dimensions in Chinese rural older adults. J Affect Disord. 2024;349:187–196. doi:10.1016/j.jad.2024.01.036
9. Benavides-Gelvez R, Rosa A, Hipolide D, Cespedes J, Ribeiro da Silva Vallim J. Assessing subjective sleep quality using the Pittsburgh sleep quality index among homeless individuals in São Paulo, Brazil. SLEEP MED. 2024;115:85. doi:10.1016/j.sleep.2023.11.263
10. Leng Y, Knutson K, Carnethon MR, Yaffe K. Association between sleep quantity and quality in early adulthood with cognitive function in midlife. Neurology. 2024;102(2):e208056. doi:10.1212/WNL.0000000000208056
11. Wang S, Jülich ST, Lei X. Latent profile of the insomnia severity index: a longitudinal study. SLEEP MED. 2024;115:202–209. doi:10.1016/j.sleep.2024.02.027
12. Tański W, Tomasiewicz A, Jankowska-Polańska B. Sleep disturbances as a consequence of long COVID-19: insights from actigraphy and clinimetric examinations-an uncontrolled prospective observational pilot study. J Clin Med. 2024;13(3):839. doi:10.3390/jcm13030839
13. Li H, Zhang Y, Chen Q, et al. Anxiety and depression among patients with insomnia during the first wave and the release of the COVID-19 in Northeast China: a cross-sectional survey. J Affect Disord. 2024;349:62–68. doi:10.1016/j.jad.2023.12.088
14. Nagasaki K, Kobayashi H, Nishizaki Y, et al. Association of sleep quality with duty hours, mental health, and medical errors among Japanese postgraduate residents: a cross-sectional study. Sci Rep. 2024;14(1):1481. doi:10.1038/s41598-024-51353-8
15. Zhu Y, Hu X, Zhu K, et al. Vaccination against SARS-CoV-2 contributed to reducing the prevalence of depression in Chinese adults - A cross-sectional study. J Affect Disord. 2024;349:407–413. doi:10.1016/j.jad.2024.01.035
16. Okajima I, Nakajima S, Kobayashi M, Inoue Y. Development and validation of the Japanese version of the Athens insomnia scale. Psychiatry Clin Neurosci. 2013;67(6):420–425. doi:10.1111/pcn.12073
17. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens insomnia scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48(6):555–560. doi:10.1016/S0022-3999(00)00095-7
18. Baize D, Meriaux-Scoffier S, Chrétien A, Hayotte M, Piponnier E, d’Arripe-Longueville F. Sleep assessment in competitive athletes: development and validation of French versions of the Athens insomnia scale and the athlete sleep behavior questionnaire. Sleep Sci. 2023;16(2):183–196. doi:10.1055/s-0043-1770803
19. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. The diagnostic validity of the Athens insomnia scale. J Psychosom Res. 2003;55(3):263–267. doi:10.1016/S0022-3999(02)00604-9
20. Hallit S, Haddad C, Hallit R, et al. Validation of selected sleeping disorders related scales in Arabic among the Lebanese population. Sleep Biol Rhythms. 2019;17(2):183–189. doi:10.1007/s41105-018-0196-0
21. Iwasa H, Takebayashi Y, Suzuki Y, et al. Psychometric evaluation of the simplified Japanese version of the Athens insomnia scale: the Fukushima health management survey. J Sleep Res. 2019;28(2):e12771. doi:10.1111/jsr.12771
22. Gómez-Benito J, Ruiz C, Guilera G. A Spanish version of the Athens insomnia scale. Qual Life Res. 2011;20(6):931–937. doi:10.1007/s11136-010-9827-x
23. Sun JL, Chiou JF, Lin CC. Validation of the Taiwanese version of the Athens insomnia scale and assessment of insomnia in Taiwanese cancer patients. J Pain Symptom Manage. 2011;41(5):904–914. doi:10.1016/j.jpainsymman.2010.07.021
24. Tan C, Wang J, Cao G, et al. Reliability and validity of the Chinese version of the Athens insomnia scale for non-clinical application in Chinese athletes. Front Psychol. 2023;14:1183919. doi:10.3389/fpsyg.2023.1183919
25. Szymczak RK, Sitek EJ, Sławek JW, Basiński A, Siemiński M, Wieczorek D. Subjective sleep quality alterations at high altitude. Wilderness Environ Med. 2009;20(4):305–310. doi:10.1580/1080-6032-020.004.0305
26. Guo WY, Bian SZ, Zhang JH, et al. Physiological and psychological factors associated with onset of high-altitude headache in Chinese men upon acute high-altitude exposure at 3700 m. Cephalalgia. 2016;37(4):336–347. doi:10.1177/0333102416646761
27. Lin CY, Cheng ASK, Nejati B, et al. A thorough psychometric comparison between Athens insomnia scale and insomnia severity index among patients with advanced cancer. J Sleep Res. 2020;29(1):e12891. doi:10.1111/jsr.12891
28. Hair JF, Black B, Babin BJ, Anderson R. Multivariate Data Analysis.
29. Fornell C, Larcker D. Evaluating structural equation models with unobservable variables and measurement error. J Marketing Res. 1981;18(1):39–50. doi:10.1177/002224378101800104
30. Han SW, Gregory W, Nylander D, et al. The SIBDQ: further validation in ulceratives colitis patients. Am J Gastroenterol. 2000;95(1):145–151. doi:10.1111/j.1572-0241.2000.01676.x
31. Fleiss J, Cohen J. The Design and Analysis of Clinical Experiments. New York, NY, USA: John Wiley & Sons; 1986.
32. Insalaco G, Romano S, Salvaggio A, Pomidori L, Mandolesi G, Cogo A. Periodic breathing, arterial oxyhemoglobin saturation, and heart rate during sleep at high altitude. High Alt Med Biol. 2012;13(4):258–262. doi:10.1089/ham.2012.1035
33. Sarstedt M, Ringle CM, Henseler J, Hair JF. On the emancipation of PLS-SEM: a commentary on Rigdon (2012). Long Range Planning. 2014;47(3):154–160. doi:10.1016/j.lrp.2014.02.007
34. Tenenhaus M, Vinzi V, Chatelin Y, Lauro C. PLS path modeling. Comput Stat Data Anal. 2005;48(1):159–205. doi:10.1016/j.csda.2004.03.005
35. Hair JFJ, Sarstedt M, Matthews LM, Ringle CM. Identifying and treating unobserved heterogeneity with FIMIX-PLS: part I–method. Eur Bus Rev. 2016;28(1):63–76. doi:10.1108/EBR-09-2015-0094
36. Tang XG, Wen J, Zhang XS, Jiang DC. Association between decreased osteopontin and acute mountain sickness upon rapid ascent to 3500 m among young Chinese men. J Travel Med. 2018;25(1). doi:10.1093/jtm/tay1075
37. West JB, Schoene RB, Milledge JS. Sleep. In: West JB, Schoene RB, Milledge JS, editors. High Altitude Medicine and Physiology.
38. West JB. Commuting to high altitude: value of oxygen enrichment of room air. High Alt Med Biol. 2002;3(2):223–235. doi:10.1089/15270290260131948
39. Enomoto K, Adachi T, Yamada K, et al. Reliability and validity of the Athens insomnia scale in chronic pain patients. J Pain Res. 2018;11:793–801. doi:10.2147/JPR.S154852
40. Sattler S, Seddig D, Zerbini G. Assessing sleep problems and daytime functioning: a translation, adaption, and validation of the Athens insomnia scale for non-clinical application (AIS-NCA). Psychol Health. 2021;38(8):1006–1031. doi:10.1080/08870446.2021.1998498
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, 3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

